Abstract
Mycoplasma pneumoniae pneumonia (MPP) often overlaps with the clinical manifestations and chest imaging manifestations of other types of community-acquired pneumonia (CAP). We retrospectively analyzed the clinical and imaging data of a group of patients with CAP, summarized their clinical and imaging characteristics, and discussed the diagnostic significance of their certain HRCT findings. The HRCT findings of CAP researched in our study included tree-in-bud sign (TIB), ground-glass opacity (GGO), tree fog sign (TIB + GGO), bronchial wall thickening, air-bronchogram, pleural effusion and cavity. The HRCT findings of all cases were analyzed. Among the 200 cases of MPP, 174 cases showed the TIB, 193 showed the GGO, 175 showed the tree fog sign, 181 lacked air-bronchogram. In case taking the tree fog sign and lack of air-bronchogram simultaneously as an index to distinguish MPP from OCAP, the sensitivity was 87.5%, the specificity was 97.5%, the accuracy was 92.5%. This study showed that that specific HRCT findings could be used to distinguish MPP from OCAP. The combined HRCT findings including the tree fog sign and lacked air-bronchogram simultaneously would contribute to a more accurate diagnosis of MPP.
Similar content being viewed by others
Introduction
Mycoplasma pneumoniae pneumonia (MPP) is a respiratory tract infectious disease caused by Mycoplasma pneumoniae. Mycoplasma pneumoniae was a common cause of respiratory tract infections before the COVID-19 pandemic, with worldwide incidence of 8.61% from 2017 to 2020, measured by direct test methods. However, non-pharmaceutical interventions (NPIs) against COVID-19 drastically lowered the transmission of M pneumoniae. In the short term, the incidence was down to 1.69% world-widely between 2020 and 2021, but the specific epidemiology varies by region1. Mycoplasma pneumoniae is now still considered a common cause of community-acquired pneumonia and estimates show that around 1% of the population of the United States is infected annually2. In China, Streptococcus pneumoniae, Mycoplasma pneumoniae and Klebsiella pneumoniae are the three leading bacterial pathogens (29.9%, 18.6% and 15.8%) of acute respiratory infections3. Because MP infection often overlaps with the clinical manifestations and chest imaging manifestations of other types of CAP, an early diagnosis or exclusion of MPP can result in more accurate treatment for CAP patients. However, mycoplasma pneumoniae cannot be detected by Gram staining or routine bacterial culture. Moreover, there is currently no rapid serological test with sufficient performance to detect mycoplasma pneumoniae, and a rapid antigen test has demonstrated poor sensitivity4,5. Therefore, the diagnosis of MPP requires elevated serum antibody levels, and therefore, it can take 2 or more weeks to obtain definitive results. MPP is an acute lung infection mainly with interstitial lesions. Due to the significant differences in clinical manifestations between MPP and pneumonia caused by common bacteria such as Streptococcus pneumoniae, and the treatment with antibiotics such as β-lactams and sulfonamide drugs is ineffective, early identification of MPP is crucial for the initial treatment of CAP6,7,8,9,10. For the early diagnosis of MPP, medical imaging is a powerful supplement to etiological examination. In earlier study, medical imaging has been used to determine the etiology of pneumonia11. Some studies using chest roentgenogram or computed tomography (CT) described central zone predominance of abnormalities observed in MPP12,13. Characteristic high-resolution CT (HRCT) findings in MPP were also reported14,15. However, only a few reports, with a relatively small number of patients, described the differences in HRCT findings between MPP and other CAP (OCAPs) 16,17. This study retrospectively analyzed the clinical and imaging data of a group of patients with CAP, summarized their clinical and imaging characteristics, and discussed the diagnostic significance of their certain HRCT findings, including "Tree-in-Bud Sign(TIB)", "Ground-glass opacity (GGO)", "Tree Fog Sign (TIB + GGO)", "Bronchial wall thickening", "Air-bronchogram", “Pleural effusion" and "Cavity".
Materials and methods
Materials
We retrospectively enrolled 400 patients who had community acquired pneumonia (CAP) with a confirmed etiology and underwent HRCT between January 2021 and January 2022. As mentioned in recent similar studies12,13,14,15,16,17,18, it was estimated that the incidence of certain imaging features such as “Bronchial wall thickening”, “Intralobular or lobular GGO” in MPP exceeded 70–90%, while the incidence in OCAP was 35–60%. According to these studies, using PASS 15 software, we calculated the sample size based on a 1:1 ratio for two groups, with a sample size of approximately 200 cases per group. Therefore, our study selected 200 clinically confirmed cases of MPP and 200 cases of OCAP as a control. The study was approved by the Ethics Committee of the second hospital of Shandong university (Approval number: KYLL-2022LW132, provided in the supplementary file). All procedures were carried out in accordance with the principles of the Helsinki Declaration. The informed consent was obtained from all subjects and/or their legal guardians.
Inclusion criteria:
All cases met the diagnostic criteria of community-acquired pneumonia: A. Onset in community. B. Relevant clinical manifestations of pneumonia: (1) New onset of cough or expectoration, or aggravation of existing symptoms of respiratory tract diseases, with or without purulent sputum, chest pain, dyspnea, or hemoptysis; (2) Fever; (3) Signs of pulmonary consolidation and/or moist rales; (4) Peripheral white blood cell count (WBC) > 10 × 109/L or < 4 × 109/L, with or without a left shift. C. Chest radiograph showing new patchy infiltrates, lobar or segmental consolidation, ground-glass opacities, or interstitial changes, with or without pleural effusion. Clinical diagnosis can be established if a patient satisfies Criterion A, Criterion C and any one condition of Criterion B and meanwhile, tuberculosis, pulmonary tumour, noninfectious interstitial lung disease, pulmonary edema, atelectasis, pulmonary embolism, pulmonary eosinophilia and pulmonary vasculitis are all excluded19,20. The HRCT image was the initial image scanned by the patient at the first visit without treatment. Sputum examination, urinary antigen testing for Streptococcus pneumoniae, and serology for Mycoplasma pneumoniae were performed. A blood culture was also performed for suspected bacteremia. Sputum was obtained by spontaneous expectoration or with the aid of nebulized saline and was examined by Gram and Ziehl–Neelsen staining and used to culture for bacteria and acid-fast bacilli. There are many laboratory testing methods for mycoplasma pneumoniae. During recent years, various new techniques have been adapted for the diagnosis of mycoplasma pneumoniae infection, notably in the field of molecular biology. Standard polymerase chain reaction (PCR) is currently the method of choice for direct pathogen detection. Serology, which is the basic strategy for mycoplasma diagnosis in routine clinical practice, has been improved by the widespread availability of sensitive assays for separate detection of different antibody classes. For the diagnosis of mycoplasma pneumonia, serology and direct pathogen detection should be combined21,22,23. In this study, according to currently universally acknowledged standards, those who met the diagnostic criteria for CAP and serologically positive were diagnosed with MPP. Serologically positive identification of mycoplasma pneumoniae based on a positive immunoglobulin M (IgM) result or a fourfold increase in immunoglobulin G (IgG) levels in convalescent versus initial blood samples by chemiluminescence immunoassay21,22,23. Other etiologies including Coxiella burnetii, Legionella pneumophila, Chlamydophila psittaci, and Chlamydophila pneumoniae were examined, as deemed necessary by the attending physicians.
Exclusion criteria:
A. Poor CT image quality. B. Patients who had an unclear etiology. C. Patients with underlying pulmonary diseases, aspiration pneumonia, malignant diseases, connective tissue diseases or immunocompromised status were also excluded.
Methods
Study design
The clinical characteristics and chest HRCT images of 400 patients were analyzed retrospectively. The clinical characteristics included gender, age, height, weight, body mass index (BMI), smoking history, maximum body temperature and one or more accompanying systemic symptoms (headache, muscle soreness, fatigue, anorexia, etc.). The HRCT findings of CAP researched in our study included tree-in-bud sign (TIB), ground-glass opacity (GGO), tree fog sign (TIB + GGO), bronchial wall thickening, air-bronchogram, pleural effusion and cavity.
Radiologic data
We have provided partial raw data in the supplementary file, and some certain data cannot be provided to protect the patients’ privacy. The datasets used and/or analysed during the current study available from the corresponding author on reasonable request. The image data of this study were read by two senior radiologists and one chief physician of respiratory medicine. The HRCT findings of all cases were analyzed. In case of disagreement or dispute, a third senior radiologist was asked for consultation and discussion.
Statistical analysis
The enumeration data were expressed by frequency or rate (%), and chi-square test was used for comparison between groups. The measurement data were expressed by means ± standard deviation (x ± sd), and ANOVA (analysis of variance) was used for comparison between groups. All tests were two-tailed and a P value < 0.05 was considered significant.
Ethics approval
The study was approved by the Ethics Committee of the second hospital of Shandong university (No. KYLL-2022LW132, provided in the supplementary file). All procedures were carried out in accordance with the principles of the Helsinki Declaration. The informed consent was obtained from all subjects and/or their legal guardians.
Results
Enrolled patients
Clinical parameters are presented in Table 1. In this study, none patient was complicated with other basic diseases. Most patients came to the hospital due to cough, expectoration and fever, without dyspnea or respiratory failure. The differences in clinical characteristics, including gender, age, height, weight, body mass index (BMI), smoking history, maximum body temperature and accompanying systemic symptoms (headache, muscle soreness, fatigue, anorexia, etc.), were not statistically significant between MPP group and OCAP group (P > 0.05).
Results of the analysis of HRCT findings
Tree-in-bud sign (TIB)
Among the 200 cases of MPP, 174 cases showed the tree-in-bud sign (TIB) (Fig. 1, red arrow), accounting for 87%, compared with 62% in OCAP (124/200). The tree-in-bud sign (TIB) was often observed in MPP patients, and was also observed in some bronchiolitis patients. In case taking the tree-in-bud sign (TIB) as an index to distinguish MPP from OCAP, the sensitivity was 88%, the specificity was 38%, the accuracy was 63%, the odds ratio was 4.2, and chi-square test p = 0.01 (Table 2).
Ground-glass opacity (GGO)
Among the 200 cases of MPP, 193 cases showed the ground-glass opacity (GGO) (Fig. 1, yellow arrow), accounting for 96.5%, compared with 50.5% in OCAP (101/200). The ground-glass opacity (GGO) was often observed in MPP patients, and was also observed in some OBP patients. In case taking the ground-glass opacity (GGO) as an index to distinguish MPP from OCAP, the sensitivity was 98%, the specificity was 50%, the accuracy was 74%, the odds ratio was 39, and chi-square test p < 0.001 (Table 2).
Tree fog sign (TIB + GGO)
The tree fog sign, which means that both tree-in-bud sign and ground-glass opacity exist simultaneously, indicates that the edges of the tree-in-bud are not clear and there is exudative change. Only when the GGO surrounds the TIB can be determined "tree fog sign", and when they are simultaneously displayed but separately distributed, they could not be determined "tree fog sign". Among the 200 cases of MPP, 174 cases showed the tree fog sign (TIB + GGO) (Fig. 1, blue arrow), accounting for 87%, compared with 38% in OCAP (76/200). The tree fog sign (TIB + GGO) was often observed in MPP patients, and was also observed in some OBP patients. In case taking the tree fog sign (TIB + GGO) as an index to distinguish MPP from OCAP, the sensitivity was 88%, the specificity was 63%, the accuracy was 75%, the odds ratio was 11.67, and chi-square test p < 0.001 (Table 2).
Air-bronchogram
Among the 200 cases of MPP, 181 lacked air-bronchogram (Fig. 2, the red arrow showed the air-bronchogram), accounting for 90.5%, compared with 40% in OCAP (80/200). Air-bronchogram was often observed in some OCAP patients (Fig. 2B, the red arrow showed the air-bronchogram) but was rarely observed in MPP patients (Fig. 2A). In case taking lack of air-bronchogram as an index to distinguish MPP from OCAP, the sensitivity was 93%, the specificity was 60%, the accuracy was 76%, the odds ratio was 18.5, and chi-square test p < 0.001 (Table 2).
Tree fog sign (TIB + GGO) + lack of air-bronchogram
Among the 200 cases of mycoplasma pneumonia, 175 cases had the tree fog sign and lacked air-bronchogram simultaneously, accounting for 87.5%, compared with 2.5% in OCAP (5/200). In case taking the tree fog sign (TIB + GGO) and lack of air-bronchogram simultaneously as an index to distinguish MPP from OCAP, the sensitivity was 87.5%, the specificity was 97.5%, the accuracy was 92.5%, the odds ratio was 273, and chi-square test p < 0.001 (Table 3).
Other HRCT findings
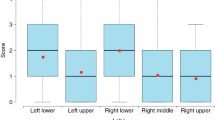
It has been reported that the bronchial wall thickening was a more specific sign of MPP23 while our study found that the specificity was weak (Fig. 3, yellow arrow). The other HRCT findings, including the distribution of lesions, pleural effusion and cavity (Fig. 4, the red arrow showed the cavity, the yellow arrow showed the pleural effusion), were not statistically significant between MPP group and OCAP group (p > 0.05) (Table 2).
Discussion
This study showed that that specific HRCT findings could be used to distinguish MPP from OCAP. The tree-in-bud sign (TIB), the ground-glass opacity (GGO), the tree fog sign (TIB + GGO) and the lack of air-bronchogram were significant findings in MPP.
As previously reported, bronchial wall thickening was characteristic findings of MPP on HRCT14,15 while our study found that the specificity was weak. As known, the cause of bronchial wall thickening is bronchial inflammation. We determined that a considerable number of OCAPs might also invade the bronchus and cause bronchitis or bronchiolitis which induced the bronchial wall thickening as a HRCT finding.
Centrilobular nodules on CT correspond pathologically to cellular infiltration in bronchioles with exudates or granulation tissue in bronchiolar lumens. This HRCT finding was generally named the tree-in-bud sign (TIB). A previous study showed the microbiological features of CAP patients with a TIB pattern share similarities with those of pneumonia in the general population24. In another study, Mycoplasma pneumoniae infection was frequently associated with a TIB pattern25. Mycoplasma pneumoniae has an affinity for airway cilia and bronchioles and causes peribronchial and perivascular infiltration of mononuclear cells and edematous and ulcerative lesions in bronchial walls26. In the present study, 87% of MPP cases had TIB pattern, compared with 62% in OCAP. The ground-glass opacity (GGO) indicates inflammatory exudation. Among the 200 cases of MPP, 193 cases showed the ground-glass opacity (GGO), accounting for 96.5%, compared with 50.5% in OCAP. In this study, the HRCT findings of GGO combined with TIB, defined as the tree fog sign, appeared in 174 MPP cases, accounting for 87%, compared with 38% in OCAP (76/200). The above results showed that the tree-in-bud sign (TIB), the ground-glass opacity (GGO) and the tree fog sign (TIB + GGO) were relatively specific HRCT characters of MPPs, but still part of OCAPs also had the above findings.
It is well known that Mycoplasma pneumoniae infection often involves bronchioles. HRCT findings of diffusely narrowed air bronchograms and volume loss of the involved lobe have been reported in MPP14. The bronchial lumen infected by Mycoplasma pneumoniae could be narrowed and obstructed by the thickened bronchial wall and mucus production. Therefore, in MPP, the air-bronchogram on HRCT could be narrowed or absent and lead to volume loss in the infiltrated area due to decreased air or subsequent atelectasis. In our study, among the 200 cases of MPP, 181 lacked air-bronchogram, accounting for 90.5%, compared with 40% in OCAP (80/200). Air-bronchogram was often observed in some OCAP patients but was rarely observed in MPP patients. Therefore, the lack of air-bronchogram was a significant finding in MPP. However, this pathologic change can also occur during other infections27. With many other causative bacteria of pneumonia, such as streptococcus pneumoniae, the areas primarily affected are the alveoli. Radiologically, air space consolidation by streptococcus pneumoniae typically abuts the surrounding visceral pleura and is likely to form air bronchograms in consolidation28. Additionally, a few studies have reported that such findings in MPP are attributable to organizing pneumonia29.
In our study, the differences in clinical characteristics, including gender, age, height, weight, body mass index (BMI), smoking history, maximum body temperature and accompanying systemic symptoms (headache, muscle soreness, fatigue, anorexia, etc.), were not statistically significant between MPP group and OCAP group. Therefore, it is not accurate to distinguish MPP from OCAP only by clinical characteristics. The detection of pathogenic microorganisms is the gold standard for the diagnosis of MPP. Identification of Mycoplasma pneumoniae based on a positive immunoglobulin M (IgM) result or a fourfold increase in immunoglobulin G (IgG) levels in convalescent versus initial blood samples by chemiluminescence immunoassay or positivity for mycoplasma pneumoniae in a sputum by polymerase chain reaction (PCR)23. HRCT is not considered the gold standard for diagnosing MPP. It may be difficult to distinguish MPP from OBP completely using HRCT, and the interpretations of HRCT findings lack the objectivity of a quantitative analysis. However, HRCT is an important supplementary method for the diagnosis of MPP. We researched some relatively specific HRCT findings of MPP, including tree-in-bud sign (TIB), ground-glass opacity (GGO), tree fog sign (TIB + GGO), bronchial wall thickening, air-bronchogram, pleural effusion and cavity. Similar results could be seen from the study by Nakanishi et al., which considered that HRCT had considerable ability to detect a lateral bronchial abnormality and to diagnose or rule out MPP based on the distribution of affected areas, abnormalities in lateral bronchial lesions, and the degree of air bronchogram in the infiltrates18. However, the diagnosis of MPP by these methods was not simple30. We therefore considered that the combined HRCT findings would contribute to a more accurate diagnosis of MPP. That was, community-acquired pneumonia (CAP) with the following HRCT features including the tree fog sign (TIB + GGO) and lacked air-bronchogram simultaneously indicated mycoplasma pneumoniae infection closely.
There were several limitations in this study. Firstly, our study was a single-center study. Secondly, the number of cases involved were limited. Thirdly, current diagnostic PCR or serology cannot discriminate between mycoplasma pneumoniae infection and carriage. Therefore, the diagnostic criteria for MPP needs further optimization.
Conclusions
This study showed that specific HRCT findings could be used to distinguish MPP from OCAP. The combined HRCT findings including the tree fog sign (TIB + GGO) and lacked air-bronchogram simultaneously would contribute to a more accurate diagnosis of MPP.
Data availability
We have provided partial raw data in the supplementary file, and some certain data cannot be provided to protect the patients’ privacy. The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Meyer Sauteur, P. M. & Beeton, M. L. Mycoplasma pneumoniae: gone forever?. Lancet Microbe 4(10), e763 (2023).
Abdulhadi, B. & Kiel, J. Mycoplasma Pneumonia. StatPearls. Treasure Island (FL) Ineligible Companies. Disclosure: John Kiel Declares No Relevant Financial Relationships with Ineligible Companies (StatPearls Publishing, 2023).
Li, Z. J. et al. Etiological and epidemiological features of acute respiratory infections in China. Nat. Commun. 12(1), 5026 (2021).
Beersma, M. F. et al. Evaluation of 12 commercial tests and the complement fixation test for Mycoplasma pneumoniae-specific immunoglobulin G (IgG) and IgM antibodies, with PCR used as the “gold standard”. J. Clin. Microbiol. 43(5), 2277–2285 (2005).
Miyashita, N. et al. Diagnostic sensitivity of a rapid antigen test for the detection of Mycoplasma pneumoniae: Comparison with real-time PCR. J. Infect. Chemother. 21(6), 473–475 (2015).
Álvaro Varela, A. I., Aguinaga Pérez, A., Navascués Ortega, A., Castilla, J. & Ezpeleta, B. C. Clinical characteristics of patients with Mycoplasma pneumoniae infection. Enferm. Infecc. Microbiol. Clin. (Engl. Ed.) 40(8), 449–452 (2022).
Han, M. S. et al. Contribution of co-detected respiratory viruses and patient age to the clinical manifestations of mycoplasma pneumoniae pneumonia in children. Pediatr. Infect. Dis. J. 37(6), 531–536 (2018).
Nir-Paz, R., Saraya, T., Shimizu, T., Van Rossum, A. & Bébéar, C. Editorial: Mycoplasma pneumoniae clinical manifestations, microbiology, and immunology. Front. Microbiol. 8, 1916 (2017).
Poddighe, D., Demirkaya, E., Sazonov, V. & Romano, M. Mycoplasma pneumoniae infections and primary immune deficiencies. Int. J. Clin. Pract. 2022, 6343818 (2022).
Atkinson, T. P., Balish, M. F. & Waites, K. B. Epidemiology, clinical manifestations, pathogenesis and laboratory detection of Mycoplasma pneumoniae infections. FEMS Microbiol. Rev. 32(6), 956–973 (2008).
Franquet, T. Imaging of pneumonia: trends and algorithms. Eur. Respir. J. 18(1), 196–208 (2001).
Hsieh, S. C. et al. Mycoplasma pneumonia: Clinical and radiographic features in 39 children. Pediatr. Int. 49(3), 363–367 (2007).
Tanaka, N. et al. High resolution CT findings in community-acquired pneumonia. J. Comput. Assist. Tomogr. 20(4), 600–608 (1996).
Lee, I., Kim, T. S. & Yoon, H. K. Mycoplasma pneumoniae pneumonia: CT features in 16 patients. Eur. Radiol. 16(3), 719–725 (2006).
Reittner, P. et al. Mycoplasma pneumoniae pneumonia: Radiographic and high-resolution CT features in 28 patients. AJR Am. J. Roentgenol. 174(1), 37–41 (2000).
Reittner, P., Ward, S., Heyneman, L., Johkoh, T. & Müller, N. L. Pneumonia: High-resolution CT findings in 114 patients. Eur. Radiol. 13(3), 515–521 (2003).
Ito, I. et al. Differentiation of bacterial and non-bacterial community-acquired pneumonia by thin-section computed tomography. Eur. J. Radiol. 72(3), 388–395 (2009).
Nakanishi, M. et al. Ability of high-resolution computed tomography to distinguish Mycoplasma pneumoniae pneumonia from other bacterial pneumonia: Significance of lateral bronchial lesions, less air bronchogram, and no peripheral predominance. Respir. Investig. 58(3), 169–176 (2020).
Cao, B. et al. Diagnosis and treatment of community-acquired pneumonia in adults: 2016 clinical practice guidelines by the Chinese Thoracic Society, Chinese Medical Association. Clin. Respir. J. 12(4), 1320–1360 (2018).
Metlay, J. P. et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am. J. Respir. Crit. Care Med. 200(7), e45–e67 (2019).
Daxboeck, F., Krause, R. & Wenisch, C. Laboratory diagnosis of Mycoplasma pneumoniae infection. Clin. Microbiol. Infect. 9(4), 263–273 (2003).
Medjo, B. et al. Mycoplasma pneumoniae as a causative agent of community-acquired pneumonia in children: Clinical features and laboratory diagnosis. Ital. J. Pediatr. 40, 104 (2014).
Kim, N. H. et al. Comparison of polymerase chain reaction and the indirect particle agglutination antibody test for the diagnosis of Mycoplasma pneumoniae pneumonia in children during two outbreaks. Pediatr. Infect. Dis. J. 26(10), 897–903 (2007).
Shimon, G., Yonit, W. W., Gabriel, I., Naama, B. R. & Nissim, A. The, “tree-in-bud” pattern on chest CT: Radiologic and microbiologic correlation. Lung 193(5), 823–829 (2015).
Cha, S. I. et al. Mycoplasma pneumoniae bronchiolitis in adults: Clinicoradiologic features and clinical course. Scand. J. Infect. Dis. 41(6–7), 515–519 (2009).
Tanaka, H. Correlation between radiological and pathological findings in patients with Mycoplasma pneumoniae pneumonia. Front. Microbiol. 7, 695 (2016).
Maldonado, F., Daniels, C. E., Hoffman, E. A., Yi, E. S. & Ryu, J. H. Focal organizing pneumonia on surgical lung biopsy: Causes, clinicoradiologic features, and outcomes. Chest 132(5), 1579–1583 (2007).
Kantor, H. G. The many radiologic facies of pneumococcal pneumonia. AJR Am. J. Roentgenol. 137(6), 1213–1220 (1981).
Llibre, J. M., Urban, A., Garcia, E., Carrasco, M. A. & Murcia, C. Bronchiolitis obliterans organizing pneumonia associated with acute Mycoplasma pneumoniae infection. Clin. Infect. Dis. 25(6), 1340–1342 (1997).
Wang, K. et al. Clinical symptoms and signs for the diagnosis of Mycoplasma pneumoniae in children and adolescents with community-acquired pneumonia. Cochrane Datab. Syst. Rev. 10(10), Cd009175 (2012).
Acknowledgements
This work was supported by the Natural Science Foundation of Shandong Province (ZR2021MH181).
Author information
Authors and Affiliations
Contributions
D.S., S.X. and N.F. were in charge of experimental design and article writing, H.M. and C.W. were in charge of data statistics, and H.S. was in charge of data collection. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sui, Dx., Ma, Hc., Wang, Cc. et al. Diagnostic significance of HRCT imaging features in adult mycoplasma pneumonia: a retrospective study. Sci Rep 14, 153 (2024). https://doi.org/10.1038/s41598-023-50702-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-50702-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.