Abstract
The use of a large femoral head in total hip arthroplasty (THA) to stabilize and reduce the incidence of dislocation is on the increase, but concerns arise when combining them with small acetabular components due to potential mechanical failures in thin polyethylene (PE) liners. A single-institution, retrospective cohort study was conducted on 116 patients with minimum 2-year follow-up who received 36-mm femoral heads and acetabular components ≤ 52 mm, using either remelted highly cross-linked polyethylene (remelted HXLPE) or vitamin E-infused HXLPE (VEPE). Osteolysis and implant loosening were not observed in either group. Although a fracture of the PE liner was observed in each group (1.7%), the clinical outcomes were excellent, as the mean modified Harris Hip Score (mHHS) at the last follow-up was 93.5. Moreover, the mean linear wear rates measured by digital imaging software in both groups were low, with 0.035 mm/y in remelted HXLPE and 0.030 mm/y in VEPE. In conclusion, The use of a large femoral head on a thin PE liner can be a viable treatment option in patients who need to prioritize stability; however, careful attention should be paid to mechanical fractures of the PE liner.
Similar content being viewed by others
Introduction
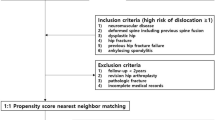
Recently, there has been an increasing trend of using a large femoral head (≥ 36 mm) in total hip arthroplasty (THA) with ceramic on ceramic, metal on metal, and ceramic or metal on polyethylene (PE)1. It can provide improved stability and range of motion, which reduces the impingement of implants and the risk of dislocation after THA2,3. However, theoretically, a larger femoral head can be related to a higher rate of polyethylene liner wear with an increased articular surface. Although highly cross-linked polyethylene (HXLPE) reduces PE wear and allows the use of larger femoral heads, several studies have reported that there are concerns about an increased risk of mechanical failures, including fracture of HXLPE liners due to oxidation on the rim4,5,6,7,8. Additionally, a thinner liner should be used for a large femoral head in a small acetabulum. This has raised concerns regarding the risk of wear and fracture of thin HXLPE liners. Currently, it has been known that residual free radicals generated during the cross-linking process of first-generation HXLPE make it more brittle, and the second-generation HXLPE was introduced to provide oxidative stability and retain the superior mechanical properties through several methods, including mechanical deformation and annealing, sequential annealing, incorporation of antioxidant-containing materials, high-pressure crystallization after melting HXLPE, and polyethylene surface-grafting with a biocompatible polymer8,9,10,11,12. It is expected to yield favorable results related to wear rate and PE liner fracture when using a relatively small acetabular component with a large femoral head; however, few studies have been conducted on this topic13.The aim of this study was to evaluate the radiologic outcomes (including osteolysis and loosening of implants), wear rates, cumulative reoperation, complications, and clinical outcomes using the modified Harris Hip Score (mHHS) at the last follow-up in patients who underwent THAs with 36-mm femoral heads and acetabular components ≤ 52 mm with HXLPE liners. We also compared differences in outcomes between first-generation remelted highly cross-linked polyethylene (remelted HXLPE) and second-generation vitamin-E-infused highly cross-linked polyethylene (VEPE). We used the antioxidant, specifically vitamin E, containing HXLPE liner among the second generation HXLPE liners.
Materials and methods
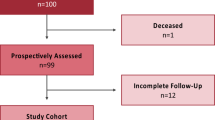
This study followed the World Medical Association Declaration of Helsinki and strengthened the reporting of observational studies in epidemiology (STROBE) guidelines for cohort studies. All procedures performed in studies involving human participants were in accordance with ethical standards. The patient information was reviewed by the University Human Subjects Committee, and an informed consent exemption was obtained from the institutional review board (IRB) of our affiliated institutions (Pusan National University Yangsan Hospital, Approval No. 05-2022-174). All experimental protocols were approved by our institutional committee (Pusan National University Yangsan Hospital, Approval No. 05-2022-174). Following institutional review board approval (IRB), a single-institution, retrospective cohort study was conducted on patients who underwent primary THAs with 36-mm femoral heads and acetabular components ≤ 52 mm with HXLPE liners from July 2012 to December 2020 with a minimum 2-year follow-up period. We identified 122 patients from the electronic medical records. Of these, five patients who were lost to follow-up and one who died from a cause that was not associated with our surgery were excluded. The electronic medical records of 116 patients were reviewed (Fig. 1). The mean follow-up period was 3.6 years (range, 2.1–9.2 years), and the mean age at the time of operation was 61.5 years (range, 31–85 years). There were 89 male patients (77%) and 27 female patients (23%). The mean body mass index (BMI) was 24.5 kg/m2, and the mean bone marrow density (BMD) was − 1.2. The causes of THA were osteonecrosis in 66 cases (56%), osteoarthritis in 36 cases (31%), femoral neck fracture in 10 cases (9%), acetabular fracture in two cases (2%), femoral head insufficiency fracture in one case (1%), and pigmented villonodular synovitis (PVNS) in one case (1%) (Table 1).
All operations were performed by an experienced arthroplasty surgeon using a posterolateral approach with transosseous reinsertion of short external rotators. Even if the acetabular size was small, if patients with at least one risk factor for dislocation, such as neuromuscular disease, we considered using a 36-mm femoral head. The final decision was made through an intraoperative stability test using the trial components. The acetabular components used were Trilogy (Zimmer Biomet, Warsaw, IN, USA) in 47 cases (41%) and G7 (Zimmer Biomet) in 69 cases (59%). The size of the acetabular components was 52 mm in 111 cases (96%) and 50 mm in five cases (4%). The femoral components used were the Versys Fiber Metal Taper (Zimmer Biomet) in 45 cases (39%), Wagner SL Revision (Zimmer Biomet) in one case (1%), Heritage (Zimmer Biomet) in one case (1%), and Microplasty (Zimmer Biomet) in 69 cases (59%). Longevity (Zimmer Biomet) in 47 cases (41%) and E1 (Zimmer Biomet) in 69 cases (59%) were utilized as HXLPE liners. The mean 45 mid-arc PE liner thickness was 5.5 mm. Trilogy was always used with Longevity, and G7 was always paired with E1. The thickness of each PE liner was 5.8 mm (at the 45 mid-arc for 50-mm Trilogy with Logevity), 5.8 mm (at the 45 mid-arc for 52-mm Trilogy with Logevity), 4.3 mm(at the 45 mid-arc for 50-mm G7 with E1), and 5.3 mm(at the 45 mid-arc for 52-mm G7 with E1), respectively. The femoral heads used were cobalt-chromium in four cases (3%) and ceramic (Biolox delta, Ceram Tec, Germany) in 112 cases (97%). The femoral head was 36 mm in size in all cases. The numbers of trans-acetabular screws were no screw in 11 cases (9%), one screw in 97 cases (84%), and two screws in eight cases (7%). The mean neck length was − 1.0 mm (Table 2).
Patients were followed up at 6 weeks, 3 months, 6 months, and 12 months postoperatively, and annually thereafter. We obtained radiographs and evaluated mHHS scores at each visit. Standard radiographs, including anteroposterior radiographs and cross-table lateral images of the hip, were used for radiographic evaluation. We compared the images obtained immediately postoperatively with those taken at the last follow-up to assess osteolysis and implant loosening. We defined radiolucent lesions of > 2 mm around the prosthetic components that were not present immediately after surgery as osteolysis14. Changes in inclination of > 5° and vertical or horizontal migration of the acetabular component of > 2 mm were defined as acetabular component loosening15.
Digital imaging software (PolyWare; Draftware Developers Inc., Vevay, IN, USA) was used to measure anteversion and inclination of the acetabular cup16,17. The software also calculated the linear and volumetric wear rates. To evaluate the intra- and extra-observer reliability of the estimated linear and volumetric wear rates, one observer investigated it twice at intervals of 2 weeks, and three observers investigated it. All clinical information regarding the patients and the results of the other observers were concealed.
Electronic medical records were reviewed to confirm re-operation and complications, including dislocation, periprosthetic fracture, PE liner fracture, heterotopic ossification, and deep joint infection. We used either remelted HXLPE (Longevity) or VEPE (E1) as liners. The outcomes of each group were compared and analyzed.
Statistical analysis
Patient characteristics are presented as means and standard deviations (SDs) for continuous variables or as frequencies and percentages for categorical variables. Continuous variables were analyzed using independent t-tests. Categorical variables were analyzed using the chi-squared test or Fisher's exact test. Intra- and interobserver reliabilities were evaluated using intraclass correlation coefficients (ICCs) with 95% confidence intervals (CI). An ICC of one means perfect reliability, and an ICC of zero means the opposite. Statistical analysis was performed using SPSS version 25.0 (SPSS Inc., Chicago, IL, USA), and statistical significance was set at p < 0.05.
Results
We compared groups divided according to the type of polyethylene liner used (remelted HXLPE or VEPE). The characteristics of the two groups, including age, sex, BMI, BMD, laterality, and surgical approach, were not significantly different. For causes of THAs, the number of femoral neck fractures was nine in the remelted HXLPE group and one in the VEPE group (p = 0.001). The other causes were not significantly different (Table 1). Operative data involving trans-acetabular screws, cup anteversion, cup inclination, cup size, 45 mid-arc PE liner thickness, and prosthetic femoral head were not significantly different between the two groups (Table 2).
Osteolysis and implant loosening were not observed in either of the groups. The mean linear wear rates were 0.035 mm/y and 0.030 mm/y in the remelted HXLPE and VEPE groups, respectively, which were not statistically different. The mean volumetric wear rate was 13.052 mm3/y in the remelted HXLPE group and 12.954 mm3/y in the VEPE group, respectively, which was not statistically different. All measurements showed a high ICC value (> 90), indicating excellent intra- and interobserver reliability. Re-operations occurred in two cases (4.3%) in the remelted HXLPE group and in one case (1.5%) in the VEPE group, but the difference was not statistically significant. Regarding complications, dislocations in three cases (6.4%), periprosthetic fracture in one case (2.1%), PE liner fracture in one case (2.1%) (Fig. 2), and heterotopic ossification in three cases (6.4%) were observed in the remelted HXLPE group. PE liner fracture in one case (1.5%) and heterotopic ossification in one case (1.5%) were observed in the VEPE group. The periprosthetic fracture that occurred in the remelted HXLPE was a Vancouver-type B1 fracture. It was treated with open reduction and internal fixation (ORIF) using a periprosthetic plate. All PE liner fractures occurred in cases using a 52 mm acetabular component. The PE liner fracture in the remelted HXLPE group occurred 3 years postoperatively, and we conducted an isolated liner exchange. The PE liner fracture in the VEPE group occurred 2.5 years postoperatively, the cause of which was not detected. We converted this to a dual-mobility THA. Total postoperative dislocation occurred in three cases (2.6%), and no further dislocation occurred after closed reduction. The incidence of dislocation was statistically different between the two groups (p = 0.033). The mean mHHS of all the patients at the last follow-up was 93.5. The mean mHHS was 92.5 in the remelted HXLPE group and 94.1 in the VEPE group, which was not significantly different (p = 0.245) (Table 3).
Discussion
The use of large femoral heads for stability and reduction of the incidence of dislocation is increasing1. However, when using a small acetabular component in small patients, a thin PE liner should be used along with a large femoral head. In particular, compared to Westerners, Asians frequently have to use relatively small acetabular components in THAs because of their small acetabular size18. HXLPE has enhanced wear resistance, and the introduction of HXLPE has provided us with the opportunity of considering the use of a large femoral head with a thin PE liner. However, there are still concerns that the use of thin PE liners with larger femoral heads carries the risk of liner fracture and increased wear, leading to osteolysis4,5,6,7,8,19. Second-generation HXLPE liners have been developed to improve wear resistance while preserving their mechanical properties. It is expected to provide good results when using relatively small acetabular components with large femoral heads, but few studies have been conducted on this topic13. In this study, we aimed to determine whether it is safe to use large femoral heads on thin PE liners and compare the remelted HXLPE group with the VEPE group.
Several studies have demonstrated that large femoral heads with thin PE liners are safe. Baker et al. investigated 882 primary THAs cases over a mean follow-up period of 4 years. They reported a mean linear PE wear rate of 0.042 mm/yr. Evidence of osteolysis or component loosening was not observed at long-term follow-up, which is consistent with our outcome. There were no liner fractures or dissociations, and the cumulative incidences of dislocation, any revision, and any reoperation were low at mid-term. The 10-year cumulative dislocation, revision, and reoperation incidences were 3.2%, 5.6%, and 9.3%, respectively20. Jauregui et al. conducted a matched-paired analysis of thin PE and conventional-thickness PE liners with 241 THAs. No significant differences were observed between the liner wear rates of the two groups, and no cases of PE fractures were observed in either cohort21. Hagman et al. evaluated the clinical and radiographic results of large femoral heads against thin PE liners with a minimum 5-year follow-up period. They demonstrated that patients reporting outcomes showed excellent results at an average follow-up duration of 8.5 years, with no cases of liner fracture22.
In this study, there was no osteolysis or implant loosening at the last follow-up in either group. The mean PE linear wear rates in both groups were 0.035 and 0.030 mm/y, respectively, which are below the theoretical threshold of 0.100 mm/year for osteolysis23. The mean linear and volumetric wear rates in the remelted HXLPE group were higher than those in the VEPE group; however, the differences between the two groups were insignificant. Both groups showed extremely low wear rates, even though it is difficult to compare their superiority owing to the relatively short follow-up period, including the bedding-in period. The clinical outcomes were excellent, as the mean mHHS at the last follow-up was 93.5. The total reoperation rate was low (2.6%). However, PE liner fractures were observed in two cases (1.7%), which occurred on the rim of the PE liner and required re-operation. This result differs from those of previous studies in terms of the use of large femoral heads on thin PE liners20,21,22. In previous studies, PE liner fractures were not observed. Thermal stabilization, such as remelting or annealing to reduce the residual free radicals generated during the cross-linking process, can reduce the mechanical properties of the liners5,8. Second-generation HXLPE liners have been developed by several methods to preserve their mechanical properties. Second-generation HXLPE liners have better wear resistance than previous generations of PE liners24,25. However, several cases of second-generation HXLPE failure have still been reported due to unidentified causes26,27,28. We also observed PE liner fractures in two cases in this study. Although we could not detect the causes of PE liner fractures, the possibility of these in both groups was demonstrated in this study. Considering this possibility, caution should be exercised when using a large femoral head on a thin PE liner.
This study has some limitations. First, this was a single-center retrospective cohort study, despite accounting for all postoperative clinical outcomes in consecutive patients. Second, the sample size was not large, and the follow-up period was relatively short. However, there are few studies on the safety of using a large femoral head on a thin PE liner, and this study provides significant evidence for the consideration of this option. Although several studies have demonstrated that there is no significant difference in femoral head penetration between conventional HXLPE and VEPE29,30, to the best of our knowledge, no study has compared their use with thin PE liners when considering the use of large femoral heads. In addition, unlike previous studies, the possibility of PE liner fractures in both groups was demonstrated in the present study. Third, as Asians usually have a small acetabulum, when considering the minimum acetabular cup size for the use of a large head, it seems that more male patients were included in this study. This may cause a probable selection bias that could impact the results. Fourth, owing to compatibility, there was a pairing to choose acetabular components and PE liners. Trilogy was used with remelted HXLPE, and G7 was used with VEPE. These limitations are an obvious obstacle to the generalization of our results, and further multicenter prospective studies are needed to verify their authenticity; we would also continue further follow-up in these patients. Especially, this study showed no osteolysis and excellent wear rates measured by digital imaging software. We believe these results are meaningful, and we will continue to monitor long-term survival outcomes, including osteolysis, in the future.
Conclusion
A large femoral head with a small acetabular component has some advantages in terms of stability and prevention of dislocation. Although second-generation HXLPE liners have been developed, there are still concerns regarding the mechanical failure of thin PE liners. In this study, there was no osteolysis or loosening of implants. Although a fracture of the PE liner was observed in each group (1.7%), the clinical outcomes were excellent, as the mean mHHS at the last follow-up was 93.5. Moreover, the mean linear and volumetric wear rates in both groups were low, and there was no significant difference between both groups. Using a large femoral head on a thin PE liner may be a viable treatment option for patients in whom stability should be prioritized; however, close attention should be paid to mechanical fractures of the PE liner.
Data availability
All data generated and analyzed during the current study are included in the published article.
References
Tsikandylakis, G. et al. Head size in primary total hip arthroplasty. EFORT Open Rev. 3, 225–231 (2018).
Howie, D. W., Holubowycz, O. T. & Middleton, R. Large Articulation Study Group. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: A randomized controlled trial. J. Bone Joint Surg. Am. 94, 1095–1102 (2012).
Jameson, S. S. et al. Lower rates of dislocation with increased femoral head size after primary total hip replacement: A five-year analysis of NHS patients in England. J. Bone Joint Surg. Br. 93, 876–880 (2011).
Currier, B. H. et al. Evaluation of oxidation and fatigue damage of retrieved crossfire polyethylene acetabular cups. J. Bone Joint Surg. Am. 89, 2023–2029 (2007).
Tower, S. S. et al. Rim cracking of the cross-linked longevity polyethylene acetabular liner after total hip arthroplasty. J. Bone Joint Surg. Am. 89, 2212–2217 (2007).
Furmanski, J. et al. Clinical fracture of cross-linked UHMWPE acetabular liners. Biomaterials 30, 5572–5582 (2009).
Furmanski, J., Kraay, M. J. & Rimnac, C. M. Crack initiation in retrieved cross-linked highly cross-linked ultrahigh-molecular-weight polyethylene acetabular liners: An investigation of 9 cases. J. Arthroplasty 26, 796–801 (2011).
Singh, G. et al. Manufacturing, oxidation, mechanical properties and clinical performance of highly cross-linked polyethylene in total hip arthroplasty. Hip Int. 28, 573–583 (2018).
Samujh, C., Bhimani, S., Smith, L. & Malkani, A. L. Wear analysis of second-generation highly cross-linked polyethylene in primary total hip arthroplasty. Orthopedics 39, e1178–e1182 (2016).
Oral, E., Wannomae, K. K., Hawkins, N., Harris, W. H. & Muratoglu, O. K. Alpha-tocopherol-doped irradiated UHMWPE for high fatigue resistance and low wear. Biomaterials 25, 5515–5522 (2004).
Oral, E. & Muratoglu, O. K. Vitamin E diffused, highly crosslinked UHMWPE: A review. Int. Orthop. 35, 215–223 (2011).
Parekh, A. et al. Second-generation highly cross-linked polyethylene in total hip arthroplasty. JBJS Rev. 9, e20.00065 (2021).
Callary, S. A., Sharma, D. K., D’Apollonio, T. M. & Campbell, D. G. Large articulations do not increase wear rates of thin second-generation highly cross-linked polyethylene liners at ten years. Bone Jt. Open. 6, 839–845 (2023).
Joshi, R. P., Eftekhar, N. S., McMahon, D. J. & Nercessian, O. A. Osteolysis after Charnley primary low-friction arthroplasty. A comparison of two matched paired groups. J. Bone Joint Surg. Br. 80, 585–590 (1998).
Cruz-Pardos, A., García-Rey, E. & García-Cimbrelo, E. Total hip arthroplasty with use of the cementless Zweymüller alloclassic system: A concise follow-up, at a minimum of 25 years, of a previous report. J. Bone Joint Surg. Am. 99, 1927–1931 (2017).
Shin, W. C. et al. The reliability and accuracy of measuring anteversion of the acetabular component on plain anteroposterior and lateral radiographs after total hip arthroplasty. Bone Joint J. 97, 611–616 (2015).
Shim, B. J., Park, S. J. & Park, C. H. The wear rate and survivorship in total hip arthroplasty using a third-generation ceramic head on a conventional polyethylene liner: A minimum of 15-year follow-up. Hip Pelvis 34, 115–121 (2022).
Hoaglund, F. T. & Low, W. D. Anatomy of the femoral neck and head, with comparative data from Caucasians and Hong Kong Chinese. Clin. Orthop. Relat. Res. 152, 10–16 (1980).
Pijls, B. G., Van der Linden-Van der Zwaag, H. M. & Nelissen, R. G. Polyethylene thickness is a risk factor for wear necessitating insert exchange. Int. Orthop. 36, 1175–1180 (2012).
Baker, C. E., Bukowski, B. R., Abdel, M. P. & Trousdale, R. T. The Lawrence D. Dorr surgical techniques & technologies award: Using big heads and small acetabular components with highly cross-linked polyethylene in total hip arthroplasty: Is it safe?. J. Arthroplasty 36, S11–S17 (2021).
Jauregui, J. J. et al. Is the use of thin, highly cross-linked polyethylene liners safe in total hip arthroplasty?. Int. Orthop. 40, 681–686 (2016).
Hagman, D. S. et al. Primary THA using thin polyethylene liners and large femoral heads: A minimum 5-year follow-up. J. Arthroplasty 37, S588–S591 (2022).
Dowd, J. E., Sychterz, C. J., Young, A. M. & Engh, C. A. Characterization of long-term femoral-head-penetration rates. Association with and prediction of osteolysis. J. Bone Joint Surg. Am. 82, 1102–1107 (2000).
Sax, O. C. et al. Low wear at 10-year follow-up of a second-generation highly cross-linked polyethylene in total hip arthroplasty. J. Arthroplasty 37, S592–S597 (2022).
Shareghi, B., Johanson, P. E. & Kärrholm, J. Wear of vitamin E-infused highly cross-linked polyethylene at five years. J. Bone Joint Surg. Am. 99, 1447–1452 (2017).
Bates, M. D. & Mauerhan, D. R. Early fracture of a vitamin-E-infused, highly cross-linked polyethylene liner after total hip arthroplasty: A case report. JBJS Case Connect 5, e65 (2015).
Brazier, B. G. & Mesko, J. W. Superior rim fracture of a vitamin E-infused highly cross-linked polyethylene (HXLPE) liner leading to total hip arthroplasty revision. Arthroplasty Today 4, 287–290 (2018).
Kim, K. B., Lee, S. M., Moon, N. H., Do, M. U. & Shin, W. C. Early unexpected failure of a vitamin E-infused highly cross-linked polyethylene liner: A case report. Medicine 100(41), e27454 (2021).
Kjærgaard, K. et al. Vitamin E-doped total hip arthroplasty liners show similar head penetration to highly cross-linked polyethylene at five years: A multi-arm randomized controlled trial. Bone Joint J. 102, 1303–1310 (2020).
Nielson, T. et al. Large femoral heads in total hip arthroplasty with vitamin E highly cross-linked polyethylene: Head penetration rates compared to highly cross-linked polyethylene. J. Arthroplasty 37, S685–S691 (2022).
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
W.C.S. and K.T.S. designed the research. M.U.D., J.S.K. and S.M.L. conducted the search. W.C.S., M.U.D. and N.H.M. had full access to the study data and carried out all analysis. M.U.D. wrote the draft of this paper. W.C.S. and S.M.L. revised the article critically.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Do, M.U., Moon, N.H., Suh, K.T. et al. Safety of using a large femoral head on thin polyethylene for total hip arthroplasty based on different types of polyethylene. Sci Rep 13, 22769 (2023). https://doi.org/10.1038/s41598-023-50217-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-50217-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.