Abstract
Bone resection is highly valued in total knee arthroplasty (TKA), but how to determine the amount of distal femur resection is still controversial. The purpose of this study was to explore how to use lateral condyle as a reference for distal femoral osteotomy in TKA. Magnetic resonance imaging (MRI) and Radiographic images from 118 nonarthritic subjects and 123 osteoarthritis (OA) subjects were used to assess the cartilage wear pattern of the distal femur in varus knees. Measurements were performed on three-dimensional reconstruction after virtual bone cutting. The difference between the resection amount of distal (0°) and posterior (90°) was calculated when the medial condyle was used as a reference in OA patients. The osteotomy amount on lateral was calculated in nonarthritic subjects when the medial condylar osteotomy was consistent with the thickness of the implants. In 43% of OA patients, there was > 1 mm difference between the 0° and 90° in medial condyle cartilage, and no difference was observed in lateral. When using medial condyle as a reference for osteotomy, there was a difference of 1.3 ± 0.56 mm between the resection amount of 0° and 90°, and the difference was 0.24 ± 0.27 mm when using lateral condyle. Statistical analysis showed that there was a linear correlation between the resection amount of lateral condyle and mechanical lateral distal femoral angle (mLDFA) in nonarthritic subjects (r = 0.845, p < 0.001). Lateral distal femoral condyle has more uniform cartilage wear in varus knee osteoarthritis. Using the lateral condyle as the reference for distal femoral osteotomy is more suitable for the cartilage wear pattern of the varus knee. The position of cutting guide can be adjusted by preoperative measurements of mLDFA.
Similar content being viewed by others
Introduction
Total knee arthroplasty (TKA) is one of the most common and cost-effective operations for end-stage knee osteoarthritis (OA). However, the satisfaction rate of patients with TKA has only been 75 to 80%, mainly due to persistent pain and poor function1. The balance of soft tissue in TKA is affected by many factors, consisting of the looseness of surrounding soft tissue, the variation of bone geometry and the amount of bone cut. In Kinematic Alignment (KA) the thickness of bone cut should be the same as the implant to attain balanced soft tissue2,3.
Cartilage wear patterns were strongly influenced by limb alignment, the varus knees showing more loss in early flexion with thinner cartilage in medial compartments. When the knee joint is fully extended, the line parallel to the longitudinal axis of the femur intersects the best-fit circle on the peripheral boundary of the subchondral bone at 0°. Ninety-two percent of knees with varus deformity had > 1 mm cartilage wear at 0°on the medial femoral condyle and lateral femoral condyle had minor degeneration. The axis of motion of the knee joint crosses the center point of the medial and lateral condyles of the femur, Howell et al. found the subchondral bone of the medial and lateral femoral condyles has the same single radius of curvature4,5. In arthritic knees with varus alignment, the lateral femoral condyle had more native morphotype4,5,6,7. The lateral condyle of the distal femur has less cartilage and bone wear due to the pattern of cartilage wear in patients with varus knees. However, no study has investigated the possible effect of using the lateral condyle as a reference for distal femoral osteotomy.
This was a retrospective study conducted to provide anthropometric data by measuring the parameters of virtually resected distal femurs undergoing TKA using a 3D reconstruction process. The hypothesis of this study was that the lateral condyle of femur had more consistent cartilage wear at 0° and 90°. Osteotomy of the distal femur with the lateral condyle as a reference might reduce the cartilage thickness and lead to the difference in excision volume between the distal femur and the posterior condyle of femur.
Method
A total of 123 knees from 112 OA patients undergoing TKA and 118 knees from 108 nonarthritic participants were included in the study between April 2020 and June 2021. All included subjects had varus knees. Lower limb alignment was assessed by the mechanical axes of the femur and tibia on full-length lower limb slices in the standing position. The inclusion criteria of arthritic group were: primary, degenerative and non-inflammatory knee OA with moderate to severe pain and failure of conservative treatment. The exclusion criteria are (1) previous knee surgery; (2) knee joint infection; (3) stiffness or ankylosis of hip joint; (4) bone loss or nerve function defect; (5) the need of highly restrictive prostheses; (6) severe knee joint deformity: knee joint flexion < 90°, flexion contracture > 20°, varus or valgus deformity > 10°. Patients in nonarthritic group consulted the orthopedic surgeon for a complaint unrelated to the cartilage wear, such as a slight soft-tissue injury or avulsion fracture. The nonarthritic subjects with cartilage wear were excluded by magnetic resonance imaging (MRI). The present study was approved by our Institutional Review Board, and informed consent was acquired from all subjects. All methods were performed in accordance with the relevant guidelines and regulations.
MRI and Radiographic parameters
All subjects of the study underwent full weight-bearing long-leg standing radiographs and lateral knee radiographs according to a standardized protocol to avoid bias. The MRI used for this study were obtained with a 1.5 T MRI (Sonata Magnetom, Siemens Medical Solutions, Erlagen, Germany) with the knee in or near full extension. Cartilage thickness was measured by applying the best-fit circle on the peripheral boundary of the subchondral bone. The thickness of the cartilage of each condyle was measured at 0° and 90°5 (Fig. 1). On MRI, we used previously described methods to determine the radius of a condyle and the thickness of the cartilage. The radius of a condyle was determined by drawing the best-fit circle of the subchondral cancellous bone interface of the femoral condyle in the sagittal image. In the sagittal plane, a clear boundary between the subchondral bone and the cartilage can be seen.
The method for measuring and computing cartilage thickness on the medial and lateral femoral condyle. (A) Medial condyle. (B) Lateral condyle. α is a line parallel to the longitudinal axis of the femur, and β is a line perpendicular to α. α and β are equally divided the best-fit circle on the peripheral boundary of the subchondral bone. The red lines are cartilage in contact with alpha and beta, representing 0° and 90° cartilage thickness, respectively.
Computed tomography (CT) scans of the knees were obtained by a Philips CT (Philips Medical Systems, The Netherlands) and the acquired imagines were stored by the Picture Archiving and Communication System (PACS). RadiAnt-DICOM software (Medixant Ltd., Poznań, Poland), which has a mouse cursor that can automatically manifest distance and angle, was used to complete the measurements on the CT scans. To reduce the measurement error, two independent experienced orthopedic surgeons checked all of the images and measured relevant parameters in the case of double-blind.
The following variables were measured8,9 and these were illustrated in Fig. 2.
Radiographic measurements of coronal parameters. (A) Hip-knee-ankle angle (HKA) is angle between the line from the center of hip joint to the center of knee joint and the line from the center of knee joint to the center of ankle joint; Valgus correction angle (VCA) is the angle between the mechanical and anatomical axes of the femur. (B) Mechanical lateral distal femoral angle (mLDFA) is the lateral distal femoral angle between the femoral mechanical axis and the line tangential to the femoral condyles. (C) Medial proximal tibial angle (MPTA) is the medial angle between the tibial mechanical axis and the proximal tibial joint line connecting the distalmost points on the concavity of the subchondral bone of the medial and lateral tibial plateaus.
-
I)
HKA: Hip-knee-ankle angle. The angle between the line from the center of hip joint to the center of knee joint and the line from the center of knee joint to the center of ankle joint;
-
II)
MPTA: Medial proximal tibial angle. The medial angle between the tibial mechanical axis and the proximal tibial joint line connecting the most distal points on the concavity of the subchondral bone of the medial and lateral tibial plateaus;
-
III)
mLDFA: Mechanical lateral distal femoral angle. The lateral distal femoral angle between the femoral mechanical axis and the line tangential to the femoral condyles;
-
IV)
VCA: Valgus correction angle. The angle between the mechanical and anatomical axes of the femur.
3D reconstruction and simulated osteotomy
Mimics 21.0 (Materialise, Leuven, Belgium) software was used for 3D reconstruction based on CT scans. Regional growth was performed to segment the femur, and each model was examined and corrected by a senior surgeon prior to measurement. The 3D model files were imported into 3-matic 13.0 (Materialise) for analysis.
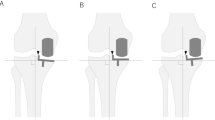
A sphere was fitted to the surface of the femoral head, and the geometric center point of the sphere was defined as the center of the hip joint. The knee joint was centered at the midpoint of the femoral intercondylar fossa. The femoral mechanical axis was defined as a line connecting the center of the hip and the center of the knee10. The distal femoral and proximal tibial cuts were perpendicular to the mechanical axis. The thickness of distal femur resection was set to be consistent with the implant size of 8 mm, including the thickness of cartilage and bone (Fig. 3)11. Cartilage thickness was set to be consistent with the MRI date. When the lateral condyle was used as the reference, setting the resection depth at 8 mm from the distal lateral condyle. When the medial condyle was used as the reference, setting the resection depth at 8 mm from the distal medial condyle12.
Statistical analysis
SPSS Statistics Package 21.0 (IBM, Armonk, New York, USA) was used to analyze data and p < 0.05 was defined as statistically significant. Scatterplots for each population were created to demonstrate alignment distributions for healthy and arthritic groups. The data were statistically analyzed by two researchers and all the measured variables and data are described as mean ± standard deviation. The paired-samples t-test was used to analyze the differences between measurement data and Levene's test was used to examine the homogeneity of the data. A linear regression test was performed to evaluate the correlation. The intra-class correlation values (ICC) were calculated to determine the reliability of inter-observer and intra-observer measurements.
Ethical approval and consent to participate
The present study was approved by the Academic Ethics Committee of the Third Hospital of Hebei Medical University, and all patients provided their informed consent for participation and publication. All of the data and materials are available.
Results
The demographic data of all patients, including gender, age, body mass index (BMI) and side, were collected before the operation and shown in Table 1. The ICC values of all measurement parameters were good to excellent, with the intra-observer ICCs and the interobserver ICCs ranging from 0.836 to 0.995 (Table 2).
For varus arthritic knees, there was a difference in cartilage thickness between the distal and posterior condyles on the medial femoral condyle (p < 0.05). In the medial condyle, the cartilage thickness was 0.17 ± 0.31 mm at 0° and 1.08 ± 0.5 mm at 90°. No difference of cartilage thickness was observed in the lateral condyle between 0° and 90°. In the lateral condyle, the cartilage thickness was 1.23 ± 0.43 mm at 0° and 1.48 ± 0.47 mm at 90°. There was no specificity in the distribution of femoral cartilage in the medial and lateral femoral condyles in nonarthritic knees (Table 3).
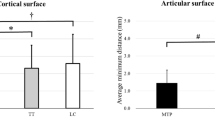
Three-dimensional reconstruction was used to simulate the osteotomy of osteoarthritis subjects perpendicular to the mechanical axis of the femur. When the medial condyle was used as the reference for distal femoral osteotomy, there was a difference of 1.3 ± 0.56 mm between the distal femoral end and posterior femoral condyle, and 43% of patients had a difference of more than 1 mm. When the lateral condyle was used as the reference for distal femoral osteotomy, the difference between distal femoral and posterior femoral condyle resection was 0.24 ± 0.27 mm (Table 4).
The simulated osteotomy of nonarthritic subjects showed that when the resection amount of the medial distal femoral condyle was set to 8 mm, the resection amount of the lateral distal femoral condyle was 4.81 ± 1.76 mm. There was a linear correlation between the osteotomy thickness of the lateral condyle and LDFA (r = 0.845, p < 0.001, Table 5). The resection amount of the lateral distal femoral condyle be predicted from the equation: Osteotomy thickness = − 49.237 + 0.625 * mLDFA (R2 = 0.715).
Discussion
In this study, it was found that Lateral distal femoral condyle has more uniform cartilage wear in varus knee osteoarthritis. Based on this, using the lateral femoral condyle as the reference for distal femoral osteotomy can make the bone resection in the distal femur and the posterior femoral condyle more consistent. For the unworn knee, it was found that there was a correlation between mLDFA and osteotomy thickness of the lateral condyle, using the medial condyle as a reference. The surgeon can adjust the cutting guide according to the preoperative measured mLDFA and the thickness of the lateral condyle to obtain a more consistent resection of the distal femur and posterior femoral condyle.
Precise TKA surgical planning should take into account the pattern of cartilage wear in arthritic patients with varus knees. Residual cartilage in patients with osteoarthritis may affect the accuracy of the osteotomy. Nam et al. proposed surgical planning for TKA based on CT does not consider articular cartilage and could lead to external malrotation of the femoral implant13.
The femoral cartilage wear is strongly associated with lower extremity mechanical alignment. MRI measurements of the knee in arthritic patients with varus knees showed that there were 43% of patients with cartilage thickness differences > 1 mm between 0° and 90° of medial femoral condyles, consistent with previous reports. The progression of arthritis is accompanied by the wear of femoral cartilage. Johnson et al. found the wear of femoral cartilage is affected by the lower limb alignment through femorotibial cartilage maps and joint kinematics. Cartilage wear of varus knee is mainly concentrated in the medial compartment of early flexion, while valgus knee has more cartilage wear in the posterolateral femoral condyle during deep flexion4. Denis et al. found that 92% of OA patients with varus knee had cartilage wear of more than 1 mm at 0° flexion, while the lateral femoral condyle had minor cartilage degeneration. Morphological studies found the subchondral bone of the medial and lateral femoral condyles has the same single radius of curvature and a single transverse axis5,7,14. There was greater cartilage wear on the medial condyle of the distal femur and more asymmetry wear between 0° and 90° than the lateral. Therefore, we recommend using the lateral femoral condyle as a reference for distal femoral osteotomy.
Cartilage thickness in the medial condyle of 0° was found to be significantly less than that on 90° in OA patients with varus knees (Table 3), using the medial condyle as a reference resulted in an increase in the radius of curvature in extension. 11% to 26% revision TKAs were performed for instability while part of them had mid-flexion instability15. Clary et al. identify the sudden reduction in the radii-of-curvature of femoral condyle as a potential cause of clinically observed paradoxical anterior femoral translation in mid-flexion16.
Different femoral sagittal design in TKA were based on different theories. Multi-radius (MR) design was based on the theory of knee rotation center which was first proposed by Frankel et al. in 1971. It reported that knee flexion occurs around a varying transverse axis, the flexion axis varies in a helical fashion during the flexion process, and the instantaneous rotation center of the femoral posterior condyle forms a “J curve17,18’’. Single-radius (SR) design had a uniform radius of curvature. It designed based on the principle that superficial medial collateral ligament is isometric throughout its range of movement. SR regards the femoral condyle as a spherical sphere with a single radius19. SR had theoretical advantages, and it provided a more posterior flexion axis and a longer extensor moment arm and maintained stabilization during movement, especially in mid-flexion20. SR design required the radius of curvature in the sagittal plane. No difference in cartilage wear was observed between the distal and posterior condyles of the lateral femoral condyle. Using the lateral femoral condyle as the reference for distal femoral osteotomy has the advantage of keeping the radius of curvature consistent when applying the SR design implants.
When the lateral condyle was used as a reference, the resection amount of the distal femur was affected by the geometric shape of the femur, and the position of the osteotomy line of the distal femur should be adjusted by morphological measurement of the femur. In this study, multiple linear regression analysis was performed on the resection amount measured by simulated osteotomy in nonarthritic subjects. mLDFA was linearly correlated with the resection amount differences between the medial and lateral condyles at 0° (r = 0.845, p < 0.001), and a 0.85 mm increment of osteotomy thickness on lateral condyle was observed with every 1° mLDFA increment when the osteotomy of the medial condyle was set at 8 mm (Fig. 4). Using Fig. 4 and the equation: Osteotomy thickness = − 49.237 + 0.625 * mLDFA, the surgeon can predict the resection thickness of lateral condyle by measuring mLDFA preoperatively and use this information intra-operatively. The amount of osteotomy may not affect limb alignment but has important implications for ligament tension, tissue balance and clinical outcome16. Many scholars attributed the unsatisfactory results after TKA to the inability of knee prosthesis to simulate physiological and natural knee motion and suggested to amend the surgical strategy20,21. Severe deformities lead to elevated joint lines. The least worn part of the joint was often used as a reference for bone cuts, and the wear of bone and cartilage in the medial condyle might result in over-resection22. Mullaji et al. proposed that the thickness of distal femoral resection should be determined according to the degree of bone defect in the medial femoral condyle23. Denis et al. suggested referencing guide should be adjusted to compensate for the mean 1.9 mm cartilage wear at the distal medial condyle5. Yue et al. proposed the intercondylar notch ceiling could be used as an accurate landmark to determine the proper distal femoral resection level during TKA10.
There were some limitations in this study. First, the nonarthritic group for the image analysis was selected for patients with slight soft-tissue injury or avulsion fracture rather than patients without knee joint disease. The nonarthritic subjects with cartilage wear were excluded by MRI, but there may be potential effects. Second, a relatively small sample size for each subject group, this was due mainly to the relatively lengthy segmentation process. Third, it was a retrospective study with non-randomized design, which had inherent drawbacks.
Conclusion
With the wear patterns of cartilage in varus osteoarthritic knees treated with TKA, it showed significantly more wear at 0° in the medial compartment than at 90°. Distal femoral resection using medial condyle as reference resulted in > 1 mm difference of resection between 0° and 90°of flexion. The lateral femoral condyle has more consistent cartilage wear. Orthopedic surgeons can adjust the reference position according to the preoperative measured mLDFA and the measured thickness of the lateral condyle to obtain a more balanced resection in the distal femur and posterior femoral condyle.
Data availability
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TKA:
-
Total knee arthroplasty
- OA:
-
Osteoarthritis
- mLDFA:
-
Mechanical lateral distal femoral angle
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computed tomography
- ICC:
-
Intra-class correlation values
- BMI:
-
Body mass index
- MR:
-
Multi-radius
- SR:
-
Single-radius
References
Carr, A. J. et al. Knee replacement. Lancet Lond. Eng. 379(9823), 1331–1340 (2012).
Hohman, D. W. Jr., Nodzo, S. R., Phillips, M. & Fitz, W. The implications of mechanical alignment on soft tissue balancing in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 23(12), 3632–3636 (2015).
Rivière, C. et al. Alignment options for total knee arthroplasty: A systematic review. Orthop. Traumatol. Surg. Research OTSR 103(7), 1047–1056 (2017).
Michael Johnson, J. & Mahfouz, M. R. Cartilage loss patterns within femorotibial contact regions during deep knee bend. J. Biomech. 49(9), 1794–1801 (2016).
Howell, S. M., Howell, S. J. & Hull, M. L. Assessment of the radii of the medial and lateral femoral condyles in varus and valgus knees with osteoarthritis. J. Bone Jt .Surg. Am. 92(1), 98–104 (2010).
Nam, D., Lin, K. M., Howell, S. M. & Hull, M. L. Femoral bone and cartilage wear is predictable at 0° and 90° in the osteoarthritic knee treated with total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 22(12), 2975–2981 (2014).
Faschingbauer, M. et al. Cartilage survival of the knee strongly depends on malalignment: a survival analysis from the Osteoarthritis Initiative (OAI). Knee Surg. Sports Traumatol. Arthrosc. Off. J ESSKA 28(5), 1346–1355 (2020).
Sappey-Marinier, E. et al. Primary osteoarthritic knees have more varus coronal alignment of the femur compared to young non-arthritic knees in a large cohort study. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 30(2), 428–436 (2022).
Choi, Y. S. et al. Asymmetric transepicondylar axis between varus and valgus osteoarthritic knees in windswept deformity can be predicted by hip-knee-ankle angle difference. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 30(9), 3024–3031 (2022).
Yue, B. et al. The intercondylar notch ceiling: An accurate reference for distal femoral resection in total knee arthroplasty for severely degenerated varus knees. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 25(9), 2818–2824 (2017).
Minoda, Y. et al. Posterior reference guides do not always maintain the size of posterior femoral condyles in TKA. Knee Surg. Sports Traumatol. Arthrosc. 24, 2489–95 (2016).
Blakeney, W., Beaulieu, Y., Puliero, B., Kiss, M. O. & Vendittoli, P. A. Bone resection for mechanically aligned total knee arthroplasty creates frequent gap modifications and imbalances. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 28(5), 1532–1541 (2020).
Nam, J. H., Koh, Y. G., Kim, P. S., Park, J. H. & Kang, K. T. Effect of the presence of the articular cartilage on the femoral component rotation in total knee arthroplasty in female and varus osteoarthritis knees. J. Orthop. Surg. Res. 15(1), 499 (2020).
Churchill, D. L., Incavo, S. J., Johnson, C. C. & Beynnon, B. D. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin. Orthop. Relat. Res. 356, 111–118 (1998).
Mehta, N. et al. Mid-flexion instability after total knee arthroplasty: diagnosis, implant design, and outcomes. Orthopedics 5, 1–7 (2022).
Clary, C. W., Fitzpatrick, C. K., Maletsky, L. P. & Rullkoetter, P. J. The influence of total knee arthroplasty geometry on mid-flexion stability: An experimental and finite element study. J. Biomech. 46(7), 1351–1357 (2013).
Frankel, V. H., Burstein, A. H. & Brooks, D. B. Biomechanics of internal derangement of the knee. Pathomechanics as determined by analysis of the instant centers of motion. J. Bone Jt. Surg. Am. 53(5), 945–962 (1971).
Ng, J. W. G., Bloch, B. V. & James, P. J. Sagittal radius of curvature, trochlea design and ultracongruent insert in total knee arthroplasty. EFORT Open Rev. 4(8), 519–524 (2019).
Hollister, A. M., Jatana, S., Singh, A. K., Sullivan, W. W. & Lupichuk, A. G. The axes of rotation of the knee. Clin. Orthop. Relat. Res. 290, 259–268 (1993).
Luo, Z., Zhou, K., Wang, H., Pei, F. & Zhou, Z. Comparison between mid-term results of total knee arthroplasty with single-radius versus multiple-radii posterior-stabilized prostheses. J. Knee Surg. 35(2), 204–214 (2022).
Jenny, J. Y. et al. Single-radius, multidirectional total knee replacement. Knee Surg Sports Traumatol Arthrosc. Off. J. ESSKA 21(12), 2764–2769 (2013).
Babazadeh, S., Dowsey, M. M., Swan, J. D., Stoney, J. D. & Choong, P. F. Joint line position correlates with function after primary total knee replacement: A randomised controlled trial comparing conventional and computer-assisted surgery. J. Bone Jt. Surg. Brit. 93(9), 1223–1231 (2011).
Mullaji, A. B., Padmanabhan, V. & Jindal, G. Total knee arthroplasty for profound varus deformity: technique and radiological results in 173 knees with varus of more than 20 degrees. J. Arthroplast. 20(5), 550–561 (2005).
Acknowledgements
We would like to express our thanks to all of the people who have participated in this research. Thanks for the technical support from the Department of Imaging of the Third Hospital of Hebei Medical University.
Funding
Funded by The National Natural Science Foundation of China (Grant No.81873983).
Author information
Authors and Affiliations
Contributions
F.W. supervised, coordinated and provided further advice on revisions; M.W. conceived of the manuscript, and participated in its design, drafted and wrote the manuscript; K.H. conceived of the manuscript, and participated in its design; H.K. conceived of data collection and data analysis; L.K. conceived of literature search and analysis. The first draft of the manuscript was written by M.W. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wei, M., Hao, K., Kang, H. et al. Lateral distal femoral condyle has more uniform cartilage wear in varus knee osteoarthritis. Sci Rep 14, 86 (2024). https://doi.org/10.1038/s41598-023-50168-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-50168-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.