Abstract
Chemotherapy is a powerful means of cancer treatment but its efficacy is compromised by the emergence of multidrug resistance (MDR), mainly linked to the efflux transporter ABCB1/P-glycoprotein (P-gp). Based on the chemical structure of betulin, identified in our previous work as an effective modulator of the P-gp function, a series of analogs were designed, synthesized and evaluated as a source of novel inhibitors. Compounds 6g and 6i inhibited rhodamine 123 efflux in the P-gp overexpressed leukemia cells, K562/Dox, at concentrations of 0.19 µM and 0.39 µM, respectively, and increased the intracellular accumulation of doxorubicin at the submicromolar concentration of 0.098 µM. Compounds 6g and 6i were able to restore the sensitivity of K562/Dox to Dox at 0.024 µM and 0.19 µM, respectively. Structure–activity relationship analysis and molecular modeling revealed important information about the structural features conferring activity. All the active compounds fitted in a specific region involving mainly transmembrane helices (TMH) 4–6 from one homologous half and TMH 7 and 12 from the other, also showing close contacts with TMH 6 and 12. Compounds that bound preferentially to another region were inactive, regardless of their free energy of binding. It should be noted that compounds 6g and 6i were devoid of toxic effects against peripheral blood mononuclear normal cells and erythrocytes. The data obtained indicates that both compounds might be proposed as scaffolds for obtaining promising P-gp inhibitors for overcoming MDR.
Similar content being viewed by others
Introduction
In recent decades, chemotherapy has emerged as the hope for improving the outcome of cancer1,2. While many of the chemotherapeutic and targeted therapy drugs show early clinical benefits with improved overall survival, a large number of patients develop resistance3,4. As a result, cells have become less sensitive to the therapeutic effects of a broad array of agents, which is known as multidrug resistance (MDR), and poses a formidable challenge in clinical anticancer practices5,6, including first-line treatments of leukemia7,8.
Chronic myelogenous leukemia (CML) is a malignant myeloproliferative disorder9 which is successfully treated with tyrosine kinase inhibitors10,11. However, the effectiveness of these drugs and of doxorubicin (Dox) is altered by the development of MDR, conferred through different molecular mechanisms and pathways11,12,13. Among the factors involved in the genesis of this phenomenon, the outward transport of anticancer drugs mediated by transmembrane transporters plays a key role14,15. Efflux proteins belonging to the ATP binding-cassette (ABC) family which have been recognized in humans are classified in 7 subfamilies namely ABCA to ABCG14,16. Among these, ABCB subfamily is composed by more than 10 transporters involved in the efflux of drugs, peptides and ions18,19. One of the most significant efflux protein is ABCB1/P-glycoprotein (P-gp)15,17, an ATP-active transporter able to extrude structurally different drugs, which limits their intracellular availability and hampers their therapeutic effect20,21. ABCB1/P-gp, thereafter P-gp, is composed of two transmembrane domains (TMD), each with six transmembrane α-helices (TMH) and a nucleotide binding domain (NBD)22,23. ATP-hydrolysis represents the driving force for the TMD to switch between the inward- and the outward-facing conformations, which leads to the removal of the chemotherapeutic agents23.
Although diverse chemical entities grouped in three generations of inhibitors have been submitted to clinical trials, none of them has been successful. The first-generation of inhibitors such as verapamil or cyclosporine A with phenylethylamine and cyclic undecapeptide scaffolds, respectively, were ineffective or showed side effects associated with their pharmacological uses24,25. The second-generation of P-gp inhibitors such as the cyclosporine D analogue, PSC833, showed improved effectiveness and selectivity, however these entities exhibited undesired drug-drug interactions23,25,26 while the third-generation of modulators such as tariquidar, revealed more affinity to P-gp and low pharmacokinetic interactions, but their cytotoxicity led to therapeutic failures23,25,26. These major drawbacks, make the development of suitable novel agents capable of circumventing MDR/P-gp an urgent necessity.
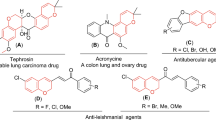
There is ample evidence that plant-derived substances exhibit privileged chemical structures plausible for obtaining novel derivatives27,28. Many of these, including some obtained from Argentinian plants, have improved the efficacy of anticancer drugs by inhibiting the P-gp transporter function29,30,31,32.
In a previous work, we found that betulin (1) was a potent compound capable of modulate P-gp32, which established its chemical structure as a promising scaffold to obtain derivatives with improved activity. In other publication, we observed that the increasing number of methoxy substituents as well as the presence of a flexible linker, such as the –NHCH2– group, favored the P-gp inhibitory effect33. In addition, known first and third generation of P-gp inhibitors including verapamil, tariquidar and elacridar, bear OCH3 groups on their aromatic moieties34,35. Based on this data and considering pentacyclic triterpenes as an encouraging chemical skeleton, a series of novel compound 1 derivatives were designed and synthesized. For comparison purposes, the work includes also the synthesis of a derivative from the inactive compound betulinic acid (2)32. The chemical entities obtained were then evaluated in order to find the best candidates for P-gp inhibition.
Results and discussion
Synthetic chemistry
As previously described, compound 1, bearing a primary alcohol at position C-28, was shown to be a promising MDR reversal agent due to the inhibition on P-gp, while betulinic acid (2), containing a C-28 carboxyl group, completely lacked this property32. Based on these findings, taking into consideration the information regarding the pharmacophores and the contacts favoring anti-P-gp activity33 and the fact that the O-methylation of polyphenolic rings, which leads to increased lipophilicity, seems to be a key modification to obtain effective P-gp modulators36,37,38,39, a library of betulin derivatives was prepared. Modifications of the position C-28 to yield esters, an amide, and carbamates suitable for structure–activity relationship studies (SARs), were the key changes performed in this series of compounds. The fact that carbamates exhibit proteolytic stability in combination with their ability to penetrate cell membranes40 makes this functionality a valuable option to include in novel compounds.
The derivatives were designed to be suitable to (a) compare the effect of the C-28 bonding functional group (ester or carbamate), (b) confirm the influence of the number of methoxy substituents in the aromatic ring as well as the presence of other rings, and (c) study the length of the saturated or unsaturated carbon chain connecting the C-28 of compound 1 and the aromatic ring counterpart. Finally, the replacement of the methoxy-substituted aromatic ring by other heterocycles, such as substituted piperazines or tetrahydroquinoline, enriched the library and the expected SAR study.
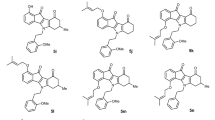
The synthesis of esters 3a-e starts with a Steglich esterification of compound 1 with mono-, di- and tri-methoxy substituted aromatic acids, providing moderate to high yields of the corresponding esters (Fig. 1). In addition, treatment of compound 2 using the N,N΄-dicyclohexylcarbodiimide/hydroxybenzotriazole (DCC/HOBt) system led to the intermediate reactive ester, which provided the amide 4 upon reaction with 3,4,5-trimethoxybenzylamine (Fig. 1).
Synthesis of betulin esters 3a-e and of the betulinic acid amide 4; Reagents and conditions: (i) corresponding acid, DCC, 4-dimethylaminopyridine (DMAP), dichloromethane (DCM)/tetrahydrofuran (THF) (3:2), 0 °C to rt, overnight, 47–98%; (ii) HOBt, DCC, THF, 0 °C to rt, 15 h, 88%; (iii) 3,4,5-trimethoxybenzylamine, THF, 0 °C to rt, 16 h, 50%.
To prepare the proposed derivatives 6a-j, 6l and 6m, compound 1 was activated to the p-nitrophenyl carbonate 5, which upon treatment with the corresponding amines in presence of N,N΄-diisopropylehtylamine (DIPEA) gave the expected carbamates in 42–75% yields (Fig. 2). Trifluoroacetic acid (TFA)-mediated Boc-group removal from compound 6j afforded the corresponding carbamate 6k.
Cytotoxic activity of the compounds in sensitive and resistant leukemia cells
To determine the effect of the proposed library on proliferation and to establish the appropriate concentrations to be used in the P-gp modulatory assays, the colorimetric MTT experiment was performed on resistant (K562/Dox) and sensitive (K562) CML cell lines.
As observed in Table 1, compounds 3a-e, 6a-g, 6j and 6m displayed no inhibition on proliferation of K562/Dox and K562 at the highest concentration assayed of 50 μM. Since compounds 4, 6h, 6i, 6k, and 6l produced more than 55% toxicity at this concentration in both cell lines, their half-maximal inhibitory concentration (IC50) values were obtained, and were 19.7, 4.6, 19.1, 9.4, and 8.0 μM, respectively, in K562 cells. These results indicated that compounds 6h, 6k, and 6l were toxic to this cell line, according to the upper limit of toxicity of 10 μM proposed by US National Cancer Institute (NCI)41. By contrast, compounds 4, 6h, 6i, 6k, and 6l showed no cytotoxicity toward K562/Dox, with IC50 values ranging from 12.5 to 34.4 μM. Regarding verapamil and the third-generation reference P-gp blocker, tariquidar42, the first was not toxic at 50 μM, while the latter exhibited cytotoxicity on K562/Dox and K562 cells with IC50 values of 2.2 and 2.4 μM, respectively. These results suggest that the derivatives 3b, 4 and 6a-6g, 6i-6m are safer candidates for P-gp/MDR reversal agents than tariquidar.
Modulating effects of the candidates on P-gp by the rhodamine 123 and doxorubicin intracellular accumulation assays
The need for new entities with novel scaffolds to overcome MDR drives efforts to test compounds prepared in accordance with encouraging data previously obtained32,33. Compounds derived from the isolated plant-derived molecules 1 and 2, at sub-cytotoxic doses, were subjected to the rhodamine 123 (Rho123) intracellular accumulation assay to determine their capacity as P-gp inhibitors. The absence of significant changes in cell shape, which is proportional to cell size, as measured by forward-scattered light (FSC) and cell granularity (side-scattered light, SSC)43, indicated that the target compounds did not induce signs of cytotoxicity at the assayed concentrations in either cell line (data not shown).
As observed in Table 2, derivatives 3a, 3c, 3d, 3e, and 6h did not induce statistically significant Rho123 accumulation (p > 0.05) at the highest concentrations tested (50 or 6.25 µM). However, compounds 3b, 6a-6g, 6j, and 6m at 50 μM significantly increased Rho123 retention in K562/Dox (p < 0.001–0.05), with fluorescence activity ratio (FAR) values ranging from 1.1 to 4.0 (Table 2). Compounds 4, 6i, and 6k efficiently enhanced the intracellular accumulation of the dye (p < 0.01–0.05) at 25 µM with FAR values of 1.3–3.0, while compound 6l did the same (p < 0.01) at 12.50 µM. The most effective compounds 6k, 6d, 6i and 6g were able to modulate P-gp with FAR values ranging from 2.1 to 3.1 even at 12.50 µM. In view of these results, the active candidates were subsequently tested at successive two-fold dilutions to establish their minimum effective concentrations (MECs). Derivatives 3b, 6b, and 6e were weakly active at 50 μM, while compounds 4, 6j, and 6l showed weak inhibition of the Rho123 efflux (p < 0.01–0.05) at 25, 12.50 and 6.25 µM, respectively (Table 2). Although compound 4 showed itself weakly active, its reversal activity was greater than that observed for its lead compound 2, which was inactive at 50 µM32. The latter result matched that described by Delou et al. 200944 who found compound 2 not to alter Rho123 accumulation in MA-104 cells when applied at 22 µM. The rest of the derivatives exhibited very low MEC values (p < 0.01–0.05, Table 2). Compounds 6c and 6m presented MECs of 3.12 µM, which is higher than that observed for compound 1 (MEC = 1.56 µM)32. Compounds 6a, 6f and 6k inhibited the outward transport of Rho123 (Table 2) at the same level as compound 132. Surprisingly, derivatives 6d and particularly compounds 6g and 6i, with MECs of 0.78, 0.19 and 0.39 μM, respectively, exceeded the activity of compound 1, verapamil and tariquidar, the latter two with MEC values of 0.39 and 0.78 μM, respectively. No statistical differences were observed (p > 0.05) when compounds 6g and 6i were compared to verapamil at the same concentration of 0.39 μM, or when compounds 6g and 6i at 0.78 μM were compared with tariquidar at the same concentration (p > 0.05). Derivatives 6g and 6i showed dose-dependent behavior (b = 64.49 p < 0.01; 95% CI 36.12 to 92.87, and b = 40.14 p < 0.01; CI 25.02 to 55.26, respectively, Figs. 3 and 4A). The complete panel of active compounds caused no significant accumulation of Rho123 in K562 at the maximum concentration assayed (Table 2 and Fig. 4B). These concentrations were equal to or higher than the effective concentrations observed in K562/Dox (Table 2), confirming that the main mechanism by which the compounds increased the concentration of the dye was by inhibition of the P-gp pump.
Representative histograms of the fluorescence intensity of cells treated with rhodamine 123 (Rho123, blue) or with Rho123 and compounds 6 g (A) or 6i (B) (green) at (A.1) 50 µM, (A.2) 0.19 µM, (B.1) 25 µM and (B.2) 0.39 µM in K562/Dox cell line. The increase in Rho123-associated mean fluorescence intensity (MFI) could be observed in K562/Dox cells treated with compounds 6g (A3) and 6i (B3), respectively.
In the rhodamine 123 (Rho123) accumulation assay, the intracellular accumulation of the dye was significantly augmented by treatment with different concentrations of compounds 6g and 6i in K562/Dox cells (A). In K562 cells (B), the respective compounds did not increase Rho123 accumulation. Significant differences from the negative control were determined using the one-tailed paired Student's t-test (***p < 0.001, **p < 0.01, *p < 0.05).
Since compounds 6g and 6i appeared as the most promising candidates, their anti-P-gp activity and mechanisms of inhibition were further investigated. To verify whether the blocking effect of both compounds on P-gp also applies to other substrates of the transporter, flow cytometry was conducted using the fluorescent drug, Dox45. Dox accumulation was substantially increased (p < 0.0001–0.05) in K562/Dox cells treated with 50 and 25 µM of compounds 6g and 6i, respectively (Fig. 5A), with FAR values of 1.26 ± 0.02 and 1.27 ± 0.03, respectively. Both compounds still caused a statistically significant retention (p < 0.01–0.05) of Dox when applied at the submicromolar concentration of 0.098 µM (Fig. 5A). This result shows compounds 6g and 6i to have higher activity than tariquidar, which displayed a MEC value of 0.39 µM. Comparing this reference compound at its MEC value with the same concentration of compounds 6g and 6i, no statistical differences were observed (p > 0.05). As seen in Fig. 5B, a similar Dox-accumulation (p > 0.05) was observed between K562 cells treated with compounds 6g and 6i and the negative control group, suggesting that a selective modulatory effect on P-gp led to the increase in Dox accumulation.
In the doxorubicin (Dox) accumulation assay, the intracellular accumulation of the dye was significantly augmented by treatment with different concentrations of compounds 6g and 6i in K562/Dox cells (A). In K562 cells (B), the respective compounds did not increase Dox accumulation. Significant differences from negative controls were determined using the one-tailed paired Student's t-test (****p < 0.0001, ***p < 0.001, **p < 0.01, *p < 0.05).
The inhibition of the efflux function of P-gp is consistent with previous studies reporting this property in other pentacyclic triterpenes, including glycyrrhizin, momilin, hederagenin and others, in most cases with active concentrations ranging from 5 to 500 µM30,46,47. This inhibitory effect was also observed in treatments with the structurally closely related lupane representative, lupeol, which proved effective at 100 µM47. The level of activity observed with compounds 6a, 6f, and 6k is similar to that observed with the oleanane triterpene, oleanolic acid, showing effectiveness at 2 µM48.
Doxorubicin resistance reversal assay
As determined, the inhibition of P-gp function by the most active novel derivatives, 6g and 6i, led to a significant intracellular increase of Dox in the resistant cell derivative. This intracellular availability allows this drug to reach the nucleus, where it induces its cytotoxic effect49,50. To demonstrate this, the effect of compounds 6g and 6i on the reversal of Dox resistance in K562/Dox was evaluated by co-administration of the drug with each derivative. Consistently, 6g and 6i at 1.56 µM managed to decrease the IC50 of Dox (Fig. 6), with FR values of 5.37 ± 1.36 (p < 0.05) and 2.69 ± 0.39 (p < 0.01), respectively. These results revealed that enhancing the intracellular drug concentration led to increased sensitivity to Dox. The Dox-reversal activity of compounds 6g and 6i was similar to (p > 0.05) and lower (p < 0.05) than that of verapamil, respectively. The latter was also applied at 1.56 µM (FR = 6.81 ± 1.20). Compound 6g at 0.78 and at 0.39 µM (FR values of 3.98 ± 0.71 and 2.09 ± 0.34, respectively) achieved the same potency as that of verapamil (p > 0.05). The derivative 6g was still active at 0.024 µM, with an FR value of 1.17 ± 0.05, showing a stronger activity (p < 0.01) than that of verapamil with a MEC of 0.098 µM and a FR value of 1.20 ± 0.05. Similarly, compound 6g was 16 times more potent for restoring the cytotoxicity of Dox than the lead molecule 1, which still chemosensitized K562/Dox at 0.39 µM. A dose-dependent activity was observed (b = − 36.87 p < 0.01; 95% CI − 55.16 to − 18.58) (Fig. 6). Compound 6i at 0.78 and 0.39 µM displayed FR values of 1.63 ± 0.06 and 1.22 ± 0.10, respectively and, at the MEC value of 0.19 µM, the FR value corresponded to 1.39 ± 0.07 (Fig. 6), achieving the same reversal effect to verapamil (p > 0.05) at the same concentration. Like compound 6g, this compound enhanced Dox cytotoxicity in a dose-dependent manner (b = − 31.88 p < 0.01; 95% CI − 46, 9 to − 16.87) and displayed nearly twice the chemosensitizer potency as that of compound 1.
Dose–response curves for the ability of compounds 6g (A) and 6i (B) to sensitize K562/Dox cells to doxorubicin (Dox). This effect was significantly increased in the presence of 6g and 6i starting at 0.024 µM (p < 0.01) and 0.19 µM (p < 0.05), respectively. Assays performed on K562 discarded changes in Dox cytotoxicity by a mechanism other than the influence on P-gp. Values are expressed as mean ± SE of at least three independent experiments.
While compound 6g at 1.56 µM produced a slight increase in Dox toxicity in the parental K562 cell line by some non-P-gp mediated mechanism, this was not observed when it was tested at 0.39 µM (FR of 1.10 ± 0.07; p > 0.05). Compound 6i did not show a reversal effect on this cell line at 1.56 µM (Fig. 6), suggesting a selective effect on P-gp at all assayed concentrations.
Structure–activity relationships
In this study, we aimed to compare two different types of bonding, ester and carbamate, between the betulin core and the pharmacophore counterpart. The ester derivatives 3a-3e were found to be inactive opposite to compound 1, but most of the carbamates, 6a, 6d, 6f, 6g, 6i and 6k, exhibited equal or better anti-P-gp activity than the lead compound 1. On the other hand, the betulinic acid amide 4 was found to be 32-fold less active against P-gp than the corresponding betulin carbamate 6d (MEC values of 25 μΜ and 0.78 μΜ, respectively, see Table 2).
Another SAR objective was to study the influence on activity of the substituents on the aromatic ring of the pharmacophore counterpart. Previous studies demonstrated that an increased number of methoxy substituents favored anti-P-gp activity23,33,36. Our results confirmed these findings, since the P-gp inhibitory activity of betulin carbamates was favored with the increasing number of methoxy groups on the phenyl moiety of the conjugates, as evidenced by the MEC values of compounds 6b, 6c and 6d (MEC = 50, 3.12 and 0.78 µM, respectively). The same was observed by comparing the MEC values of compounds 6e (MEC = 50 µM), 6f (MEC = 1.56 µM) and 6g (MEC = 0.19 µM) with one, two and three –OCH3 groups, respectively. Further studies regarding the carbamates and, more specifically, the replacement of the methoxy-substituted aromatic ring by substituted piperazines and a tetrahydroquinoline (derivatives 6h-6m), showed that less potent inhibitors were obtained, except for the carbamate 6i, which was found to be the second most active derivative after compound 6g (MEC = 0.39 and 0.19 µM, respectively). Likewise, when the length of the carbon chain connecting the C-28 of compound 1 and the aromatic ring increased, more potent derivatives were obtained. As observed in Table 2, compound 6a (MEC = 1.56 µM) was less effective than compound 6d and both showed weaker reversal activity than compound 6g, all of them bearing three O-methyl groups. Similarly, compound 6c was less effective than compound 6f, both bearing two OCH3 substituents (MEC = 3.12 and 1.56 µM, respectively). The length of the chain did not alter the moderate effectiveness (MEC = 50 µM) of compounds 6b and 6e with only one O-methyl group. A summary of these findings is shown in Fig. 7.
Taking into consideration the SAR studies so far, the best candidates should contain the betulin core connected to a pharmacophore through a carbamate bonding. Regarding the structural elements in the pharmacophore counterpart, the increased number of -OMe groups on the phenyl ring and the length of the carbon chain folding both moieties of the molecules led to increased activity. These findings could be used to rationally guide the design and synthesis of new lead compounds with improved tumor P-gp inhibitory activity.
Inhibitor binding and structural determinants by molecular modeling
The protocol used for molecular dynamics (MD) analysis has been recently tested thoroughly with other families of P-gp inhibitors32,33. In these studies, Dox was taken as the reference substrate and verapamil and tariquidar as known modulators. The antitumoral agent paclitaxel (Taxol) has been taken as the crystallographic reference, as it was co-crystallized in the experimental structure 6QEX, and re-docked to validate the docking protocol33,51. In the current work, the chemotherapeutic drug vincristine, co-crystallized into the structure 7A6952, was also included as a reference substrate.
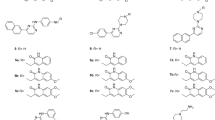
To obtain the initial structures for the MD simulations, the docking protocol was used to scan inside the whole transmembrane region, making no assumptions about the localization of a particular binding site. The main binding sites were determined for the working substrate Rho123, for vincristine and compared to that previously obtained for Dox, verapamil and tariquidar33. Next up, target compounds were included, thus covering the whole range of experimental activities, from those completely inactive to those most powerful. A set of molecular MD simulations on these compounds was intended to reveal in detail the binding dynamics and the structural factors that determine their activity. As a first, gross observation, it should be noted that the compounds clearly distribute between two different sites as shown in Figs. 8A,B, which shows a superimposed and aligned representative snapshot of the most populated cluster of one trajectory for each compound. Amide 4 and carbamates of series 6 fell in the apex of the inverted “V” formed by TMH 4–6 from one homologous half and TMH 7 and 12 from the other; this pocket was labeled as site I. The compounds mentioned accommodate in two general modes with minor differences: (i) a distorted U, with the carbamate or the carbamate linked to the alkyl chain as the camber connecting the triterpene, and the aromatic moieties as the branches of the “U” (Fig. 8A1 and C with compound 6g as example) or (ii) a V-shape with the piperazine or tetrahydroquinoline burying a bit deeper into the right side as observed in Fig. 8A2 (Fig. 8D showing compound 6i, as representative). Both modes of binding shown in Fig. 8C and D fully overlap with that of vincristine and this, in turn, with that of Rho123 and what had been previously observed for Dox33 (see also Supplementary Material Figs. S1 and S2). In both cases, the triterpene moiety arranged practically in the same way into the hydrophobic cavity shaped by specific residues of TMH 4–7 and 12 (details below). On the other hand, compounds from series 3 went to a different site, hereinafter referred as site II, involving different regions of TMH 4, 5 and 12 and TMH 8 and 11 (Fig. 8B and E featuring 3a as example).
Superimposition of the aligned snapshots of the most populated clusters after a cluster analysis over the last 50 ns of each simulation for compounds binding to site I (A) and to site II (B). The poses of compounds representative of each pattern are superimposed on the one obtained for the simulation of Rho123 shown as a translucent yellow surface: (C) 6g; (D) 6i and (E) 3a. The cartoon representation of the protein is colored in (C–E) according to the amino acid sequence, from red to blue.
A summary of the calculated free energies of binding (ΔG°b) from these simulations is shown in Table 3. The compounds interacting with the residues of site I showed a good correlation with the experimental MEC values for the Rho123 intracellular accumulation assay, as shown in Fig. 9. In sharp contrast, compounds of series 3, which interact with site II, did not modulate the activity of P-gp, regardless of their binding energies. This preference for what we describe as site I is remarkable, besides the evident overlap with Rho123 and even with the bulkier chemotherapeutics substrates, Dox and vincristine (Supplementary Material Fig. S3). Indeed, these findings reinforce the relevance of the residues involved in binding site I, as was previously discussed in studies from our group32,33 and in the literature cited therein. The results obtained highlight not only the identity of these residues, but also the mandatory requisite for tightly contacting both halves of the transporter at once, especially TMH 6 and 12, which connect the TMHs and the NBDs.
Correlation between the logarithms of the minimum effective concentrations (MEC) (Table 2) and the ΔG°b, calculated from the MD simulations.
A closer look at the binding modes of the most powerful inhibitors 6g and 6i is shown in two representative snapshots of the most populated cluster for each trajectory in Fig. 10, which can be taken as illustrative for the two variants of binding in this site for the amide- or carbamate-alkyl-bridged series. The triterpene moiety fits in the cavity shaped by the hydrophobic residues Trp232 from TMH 4, Phe303, Ile306, Tyr307 and Tyr310 from TMH 5, Phe336, Leu339, Ile340 and Phe343 from TMH 6, Phe728 from TMH 7, Phe983, Met986, Ala987, the alkyl chain of Gln990 and Val991 from TMH 12 (images of 6g and 6i on the hydrophobicity-colored surface available in Supplementary Material, Fig. S4). The interaction with the 3-OH of the steroid moiety and the π system of Phe303 is present in all cases, as an anchor in the limit of the hydrophobic pocket; to the left (Fig. 10), some polar residues appear, Gln725 and Gln828. The methoxy-substituted ring of 6g (and similarly, though with weaker interactions for 6a-f) interacts with Trp232, Gln347 (hydrophobic or H-bound, depending upon the substitution of their phenyl rings), Phe343 and Ser 344. The aliphatic or carbamate-alkyl “bridges” of compound 4 and of series 6 contact mainly Ile340, Met876, Met986 and Glu990 and, more importantly, contribute to the flexibility that enables the twisting shape (Fig. 10A,B). The main difference between 6g and 6i is the strong electrostatic contact of the latter with Glu875 and the contacts with Leu65 and Gln946, as observed in the right side of Fig. 10.
These features are absent in compounds 3a, 3c, 3d and 3a, which were found to be not flexible enough for arranging in this mode and therefore fell to site II. The ester function itself does not appear as a drawback, as the NH of the amide present in the carbamates 6 or in the amine of 4 is not generally involved in strong H-bond interactions. The absence of sp3-hybridized atoms between the carbonyl and the aromatic moiety seems to favor more extended conformations, as previously observed for quinolinone-pyrimidine hybrids, for which the conjugated carbonyl-vinyl bridge conferred rigidity and decreased or prevented the activity of these species33.
Besides the above features described in Fig. 10, deeper analyses were obtained by energy decomposition to quantify the contribution of each residue averaged over the time of the simulation. Figure 11A–D compares the patterns obtained for Rho123, vincristine, 6g, and 6i. Both target compounds had prominent peaks (denoting persistent interactions) for the same residues as Rho123 and vincristine. These peaks also match those obtained for Dox and tariquidar, for which the free energy contribution per residue is reproduced from previous calculations33 (Supplementary Material Fig. S5).
Free energy decomposition in terms of per residue contribution obtained for rhodamine 123 (A); vincristine (B); compound 6g (C); and compound 6i (D). (E) The profiles obtained for vincristine (blue) and compound 6f (green) are superimposed on those calculated for 3a (red) and 3d (orange). The labels correspond to the residues of the latter.
The patterns obtained for compounds 3a and 3c are superimposed in Fig. 11E on those of vincristine and compound 6f (less powerful than compound 6g but still overlapping the peaks of the substrates). As can be observed, almost all peaks of both derivatives, 3a and 3c, corresponded to different residues than that observed for the substrates or the series 6 partners (for example, note the lack of any interaction with TMH 6).
Selective toxicity of compounds 6g and 6i over mammalian cells
Derivative 6g did not reveal cytotoxicity on PBMC by means of the MTT assay at 50 µM, while the same concentration of compound 6i slightly affected cell viability (64%). The IC50 value of 26.37 ± 2.88 µM suggests that the latter molecule could not be considered as cytotoxic, based on the 10 µM value established by the US National Cancer Institute41. Neither compound induced erythrocyte hemolysis at the maximum tested concentration of 50 µM.
Conclusions
In our ongoing search for novel P-gp inhibitors, a panel of new betulin derivatives was designed on the basis of the structural requirements previously determined as important for P-gp interaction. Among the series of derivatives obtained, compounds 6g and 6i proved to be the most potent and efficacious for blocking the P-gp-mediated efflux of Rho123. Further study of the pharmacological profile of both entities revealed that they increased the intracellular accumulation of Dox, rendering K562/Dox cells sensitive to its cytotoxic effect. The large amount of data obtained herein and the negligible cytotoxicity of compounds 6g and 6i lay the groundwork for a second step involving further in vitro studies and in vivo studies.
The activity was positively potentiated by the number of aromatic ring methoxy substituents and the length and flexibility of the chain linking both parts of the molecule, which provided an appropriate fit into a specific region of the large TMD. Such a preference is not trivial for a multispecific and substrate-promiscuous transporter like P-gp and was already observed for other families of potential inhibitors32,33. This mechanism of inhibition certainly deserves further investigation. However, at this point it reveals very useful clues for the rational design of new inhibitors by finding: (I) molecular shapes designed to arrange within the hydrophobic cavity described as part of site I (compound 1 scaffold appeared to do it very well as previously observed32; (II) appropriate linkers and methoxylated aromatics or piperazine derivatives allowing tight contact with TMH 6 and 12 simultaneously.
The data obtained establish the basis for developing compounds which, administered in combination with chemotherapeutic agents transported by P-gp, could restore the efficacy of these in P-gp/MDR cancer cells.
Materials and methods
Chemistry
All solvents were dried and purified prior to use according to standard procedures. When required, reactions were performed under inert atmosphere (Ar) in preflamed glassware. Anhydrous Na2SO4 was used for drying solutions, and the solvents were then routinely removed at ca. 40 °C under reduced pressure using a rotary vacuum evaporator. All reagents employed in the present work were commercially available and used without further purification. Among all the amines employed in the synthesis of the betulin carbamates, 6a-m and tert-butyl-4-(2-aminoethyl) piperazine-1-carboxylate, used for the synthesis of 6j, were prepared according to a previously published protocol53. 2-(3,4-dimethoxyphenyl)ethan-1-amine and 2-(3,4,5-trimethoxyphenyl)ethan-1-amine employed in the synthesis of 6f and 6g, respectively, were synthesized and characterized according to the procedures described in Supplementary Material. Flash column chromatography (FCC) was performed on silica gel (70–230 and 230–400 mesh, Merck, Germany) and analytical thin layer chromatography (TLC) on silica 60gel-F254 precoated aluminum foils (0.2 mm film, Merck, Germany). Spots on the TLC plates were visualized with UV light at 254 nm and using anisaldehyde solution. 1H NMR spectra were recorded in CDCl3 at 600.13 MHz and 13C spectra at 150.9 MHz on a Bruker AVANCEIII HD spectrometer. Chemical shifts (δ) are indicated in parts per million downfield from TMS. Coupling constants (J) are reported in Hertz. HR mass spectra were performed using an ESI-LTQ-ORBITRAP XL unit (Thermo Scientific, Bremen, Germany). The Orbitrap Unit was operated in positive mode, with a spray voltage of 3.2 kV, while the sheath gas flow rate and auxiliary gas flow rate were adjusted to 12 and 2 arbitrary units, respectively. The capillary voltage and the tube lens voltage were set to 10 and 110 V, respectively. The scan ranged from m/z 150 up to 2000. The purity of the tested compounds was determined by reversed phase high performance liquid chromatography (HPLC) (Jasco LC-NetII/ADC series) equipped with a Phenomenex Gemini-NX RP-C18 150 × 4.6 mm, 5 μm particle size column and a MD-4010 PDA Detector and monitored at 254 and 280 nm. Linear gradients of A and B were used where A = 0.1% TFA in H2O and B = 0.1% TFA in CH3CN, at a flow rate of 0.8 mL/min. The purity of the tested compounds, which corresponded to > 95% (see the Supplementary Material), was evaluated as a percentage ratio between the areas of the main peak and of possible impurities.
General procedure for the synthesis
General procedure for the synthesis of betulin esters 3a-e
To a stirring solution of compound 1 in dry DCM/THF (3:2 v/v, 0.05 M), under Ar atmosphere, the aromatic acid (1.5 eq) and 4-dimethylaminopyridine (1.75 eq) were added, and the suspension was cooled to 0 °C. Subsequently DCC (1.75 eq) was added, and the reaction mixture was stirred for 5 min at 0 °C and then at ambient temperature overnight. Upon consumption of the starting material, dicyclohexylurea (DCU) was filtered under vacuum and washed in the filtration funnel with ethyl acetate (AcOEt). After evaporation of the solvent to dryness under reduced pressure, the residue was subjected to FCC, affording the pure betulin esters 3a-e as colorless oils.
3a: compound 1 was reacted with 4-methoxybenzoic acid according to the general procedure. Yield = 98%; Colorless oil; Rf (PhMe/EtOAc 95:5) = 0.27; 1H NMR (600 MHz, CDCl3) δ 8.01 (br s, 1 H), 7.99 (br s, 1 H), 6.93 (br s, 1 H), 6.91 (br s, 1 H), 4.72 (d, J = 2.5 Hz, 1 H), 4.60 (t, J = 1.4 Hz, 1 H), 4.48 (dd, J = 11.1, 2.1 Hz, 1 H), 4.06 (dd, J = 11.0, 1.4 Hz, 1 H), 3.86 (s, 3 H), 3.18 (dd, J = 11.5, 4.8 Hz, 1 H), 2.52 (td, J = 11.3, 5.9 Hz, 1 H), 2.06–1.95 (m, 2 H), 1.91 (ddd, J = 12.4, 8.4, 1.2 Hz, 1 H), 1.80–1.73 (m, 2 H), 1.70 (s, 3 H), 1.68–1.21 (m, 16 H), 1.18–1.08 (m, 2 H), 1.06 (s, 3 H), 1.0 (s, 3 H), 0.97 (s, 3 H), 0.91 (td, J = 14.1, 4.4 Hz, 1 H), 0.83 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 9.5 Hz,1 H); 13C NMR (151 MHz, CDCl3) δ 166.7, 163.3, 150.2, 131.5, 122.9, 113.6, 109.8, 79.0, 62.9, 55.4, 55.3, 50.4, 48.9, 47.8, 46.7, 42.8, 40.9, 38.9, 38.7, 37.6, 37.2, 34.7, 34.2, 30.0, 29.7, 28.0, 27.4, 27.2, 25.2, 20.8, 19.2, 18.3, 16.1, 16.1, 15.3, 14.8; HR-ESI (m/z) [2 M + H+] calculated for C38H57O4 1153.8438. Found: 1153.8428; HPLC analysis: peak area 99.5%, tR = 14.30 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
3b: compound 1 was reacted with 3,4,5-trimethoxybenzoic acid according to the general procedure. Yield = 71%; Colorless oil; Rf (PhMe/EtOAc 9:1) = 0.24; 1H NMR (600 MHz, CDCl3) δ 7.31 (s, 2 H), 4.72 (d, J = 2.6 Hz, 1 H), 4.61 (t, J = 1.5 Hz, 1 H), 4.53 (dd, J = 11.1, 1.9 Hz, 1 H), 4.08 (d, J = 11.1 Hz, 1 H), 3.91 (s, 9 H), 3.19 (dd, J = 11.6, 4.8 Hz, 1 H), 2.54 (td, J = 11.1, 5.8 Hz, 1 H), 2.08–2.00 (m, 1 H), 1.95–1.86 (m, 2 H), 1.81–1.72 (m, 2 H), 1.71 (s, 3 H), 1.69–1.65 (m, 2 H), 1.64–1.14 (m, 16 H), 1.07 (s, 3 H), 1.00 (s, 3 H), 0.97 (s, 3 H), 0.91 (td, J = 13.4, 4.4 Hz, 1 H), 0.83 (s, 3 H), 0.76 (s, 3 H), 0.69 (d, J = 9.4 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 166.5, 152.9, 150.1, 125.5, 110.0, 106.8, 79.0, 63.5, 60.9, 56.3, 55.3, 50.4, 48.8, 47.8, 46.8, 42.8, 40.9, 38.9, 38.7, 37.7, 37.2, 34.8, 34.2, 30.1, 29.7, 28.0, 27.4, 27.2, 25.2, 20.8, 19.1, 18.3, 16.1, 16.0, 15.3, 14.8; HR-ESI (m/z) [2 M + H+] calculated for C40H61O6 1273.8860. Found: 1273.8845; HPLC analysis: peak area 99.3%, tR = 12.90 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
3c: compound 1 was reacted with trans-2,4-dimethoxycinnamic acid according to the general procedure. Yield = 95%; Colorless oil; Rf (PhMe/EtOAc 9:1) = 0.4; 1H NMR (600 MHz, CDCl3) δ 7.92 (d, J = 16.2 Hz, 1 H), 7.45 (d, J = 8.6 Hz, 1 H), 6.50 (dd, J = 8.5, 2.4 Hz, 1 H), 6.45–6.42 (m, 2 H), 4.71 (d, J = 2.5 Hz, 1 H), 4.60 (t, J = 1.5 Hz, 1 H), 4.39 (dd, J = 11.1, 2.0 Hz, 1 H), 3.97 (d, J = 11.1 Hz, 1 H), 3.87 (s, 3 H), 3.84 (s, 3 H), 3.18 (dd, J = 11.4, 4.8 Hz, 1 H), 2.50 (td, J = 11.2, 5.9 Hz, 1 H), 2.05–1.98 (m, 1 H), 1.93 (m, 1 H), 1.89–1.84 (m, 1 H), 1.79–1.71 (m, 2 H), 1.69 (s, 3 H), 1.68–1.39 (m, 13 H), 1.30–1.23 (m, 3 H), 1.22–1.08 (m, 2 H), 1.06 (s, 3 H), 0.99 (s, 3 H), 0.97 (s, 3 H), 0.90 (td, J = 12.6, 4.0 Hz, 1 H), 0.83 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 9.6 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 168.4, 162.7, 159.8, 150.3, 140.0, 130.4, 116.7, 116.1, 109.8, 105.2, 98.4, 79.0, 62.5, 55.4, 55.3, 50.4, 48.9, 47.7, 46.6, 42.7, 40.9, 38.9, 38.7, 37.6, 37.2, 34.7, 34.2, 29.9, 29.7, 28.0, 27.4, 27.2, 25.2, 20.8, 19.2, 18.3, 16.1, 16.0, 15.3, 14.8; HR-ESI (m/z) [M + H+] calculated for C41H61O5 633.4519. Found: 633.4516; HPLC analysis: peak area 94.8%, tR = 13.20 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
3d: compound 1 was reacted with 3,4,5-trimethoxycinnamic acid according to the general procedure. Yield = 64%; Colorless oil; Rf (PhMe/EtOAc 9:1) = 0.29; 1H NMR (600 MHz, CDCl3) δ 7.59 (d, J = 15.6 Hz, 1 H), 6.75 (s, 2 H), 6.36 (d, J = 15.6 Hz, 1 H), 4.71 (d, J = 2.5 Hz, 1 H), 4.60 (t, J = 1.5 Hz, 1 H), 4.40 (dd, J = 11.4, 2.0 Hz, 1 H), 4.00 (d, J = 11.4 Hz, 1 H), 3.89 (s, 6 H), 3.88 (s, 3 H), 3.18 (dd, J = 11.4, 4.8 Hz, 1 H), 2.50 (td, J = 11.1, 5.6 Hz, 1 H), 2.05–1.97 (m, 1 H), 1.96–1.91 (m, 1 H), 1.89–1.83 (m, 1 H), 1.78–1.71 (m, 2 H), 1.70 (s, 3 H), 1.65–1.24 (m, 18 H), 1.06 (s, 3 H), 1.00 (s, 3 H), 0.97 (s, 3 H), 0.91 (td, J = 13.1, 4.2 Hz, 1 H), 0.83 (s, 3 H), 0.76 (s, 3 H), 0.69 (d, J = 11.2 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 167.4, 153.4, 150.1, 144.6, 140.1, 129.9, 129.0, 128.2, 117.5, 109.9, 105.2, 79.0, 62.9, 61.0, 56.2, 55.3, 50.4, 48.9, 47.7, 46.6, 42.7, 40.9, 38.9, 38.7, 37.6, 37.2, 34.7, 34.2, 29.9, 29.6, 28.0, 27.4, 27.1, 25.2, 20.8, 19.1, 18.3, 16.1, 16.0, 15.3, 15.2, 14.8; HR-ESI (m/z) [M + H+] calculated for C42H63O6 663.4624. Found: 633.4570; HPLC analysis: peak area 99.1%, tR = 12.60 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
3e: compound 1 was reacted with 2,4,5-trimethoxycinnamic acid according to the general procedure. Yield = 47%; Colorless oil; Rf (PhMe/EtOAc 9:1) = 0.16; 1H NMR (600 MHz, CDCl3) δ 7.98 (d, J = 16.2 Hz, 1 H), 7.02 (s, 1 H), 6.50 (s, 1 H), 6.38 (d, J = 16.2 Hz, 1 H), 4.71–4.70 (m, 1 H), 4.60 (t, J = 1.6 Hz, 1 H), 4.40 (dd, J = 11.2, 1.9 Hz, 1 H), 3.98 (d, J = 11.4 Hz, 1 H), 3.93 (s, 3 H), 3.87 (s, 3 H), 3.86 (s, 3 H), 3.19 (dd, J = 11.4, 4.8 Hz, 1 H), 2.51 (td, J = 11.1, 5.7 Hz, 1 H), 2.07–1.98 (m, 1 H), 1.96–1.91 (m, 1 H), 1.89–1.85 (m, 1 H), 1.80–1.71 (m, 2 H), 1.70 (s, 3 H), 1.66–1.11 (m, 18 H), 1.06 (s, 3 H), 0.99 (s, 3 H), 0.97 (s, 3 H), 0.91–0.86 (m, 1 H), 0.83 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 9.5 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 168.2, 153.9, 152.1, 150.3, 143.3, 139.5, 129.0, 125.3, 115.8, 115.1, 110.9, 109.8, 96.9, 79.0, 62.5, 56.5, 56.0, 55.3, 50.4, 48.9, 47.7, 46.6, 42.7, 40.9, 38.9, 38.7, 37.6, 37.2, 34.7, 34.2, 29.9, 29.7, 28.0, 27.4, 27.2, 25.2, 20.8, 19.1, 18.3, 16.1, 16.0, 15.3, 14.8; HR-ESI (m/z) [M + H+] calculated for C42H63O6 663.4624. Found: 633.4619; HPLC analysis: peak area 98.1%, tR = 11.33 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
General procedure for the synthesis of amide 4
To an ice-cold stirring solution of compound 2 (20 mg, 0.044 mmol) in dry THF, HOBt (8 mg, 0.06 mmol) and DCC (10 mg, 0.05 mmol) were added, and the solution was stirred at room temperature for 15 h. After completion of the reaction, the mixture was diluted in 1,2-dichloroethane (DCE) and washed sequentially with 5% aqueous ice-cold NaHCO3, water and brine. Then it was dried over anhydrous Na2SO4, filtered and concentrated to dryness, to provide the corresponding active ester as a white solid (22 mg, 88% yield); 1H NMR (600 MHz, CDCl3) δ 8.08 (d, J = 8.4 Hz, 1 H), 7.56 (ddd, J = 7.2, 1.2, 0.6 Hz, 1 H), 7.43 (ddd, J = 7.2, 1.2, 0.6 Hz, 1 H), 7.36 (d, J = 8.2 Hz, 1 H), 4.73 (d, J = 2.3 Hz, 1 H), 4.63 (t, J = 1.7 Hz, 1 H), 4.17 (d, J = 8.4 Hz, 1 H), 3.51–3.43 (m, 1 H), 3.21–3.15 (m, 2 H), 2.95 (td, J = 11.2, 5.0 Hz, 1 H), 2.65–2.61 (m, 1 H), 2.41 (dd, J = 13.0, 8.1 Hz, 1 H), 2.21 (td, J = 12.6, 3.7 Hz, 1 H), 2.12–2.04 (m, 1 H), 1.71 (s, 3 H), 1.61–1.51 (m, 7 H), 1.47–1.40 (m, 4 H), 1.35–1.25 (m, 6 H), 1.18–1.24 (m, 2 H), 1.08–1.10 (m, 1 H), 1.04 (s, 3 H), 0.98 (s, 3 H), 0.97 (s, 3 H), 0.90 (td, J = 13.6, 4.1 Hz, 1 H), 0.81 (s, 3 H), 0.76 (s, 3 H), 0.69–0.72 (m, 1 H); 13C NMR (151 MHz, CDCl3) δ 171.8, 157.1, 149.2, 143.6, 128.9, 128.7, 124.7, 120.6, 110.4, 107.9, 78.9, 57.0, 55.8, 55.4, 50.5, 49.9, 49.1, 46.6, 42.5, 40.8, 38.9, 38.7, 38.45, 37.2, 36.8, 34.9, 34.4, 33.9, 31.4, 30.3, 30.1, 28.0, 27.4, 25.6, 25.4, 24.9, 20.8, 19.4, 18.3, 16.1, 15.4, 14.8.
To a solution of the above active ester (22 mg, 0.04 mmol) in dry THF (50 μL) under Ar atmosphere and stirring at 0 °C, 3,4,5-trimethoxybenzylamine (12 μL, 0.067 mmol) was added and the reaction mixture was stirred for another 16 h at ambient temperature. After completion of the reaction, the mixture was diluted in ethyl acetate and washed sequentially with 5% aqueous ice-cold citric acid, water, and brine. The organic layer was dried over anhydrous Na2SO4, filtered, and concentrated to dryness. The residue obtained was subjected to FCC using PhMe/EtOAc 9:1 as eluent, affording the corresponding amide 4 in 50% yield; White solid; m.p.: 99.7–100.5 °C; Rf (PhMe/EtOAc 95:5) = 0.08; 1H NMR (600 MHz, CDCl3) δ 6.49 (s, 2 H), 5.94–5.89 (m, 1 H), 4.74 (d, J = 2.9 Hz, 1 H), 4.60 (t, J = 2.2 Hz, 1 H), 4.40 (dd, J = 14.4, 5.8 Hz, 1 H), 4.34 (dd, J = 14.8 Hz, 5.8 Hz, 1 H), 3.84 (d, J = 1.2 Hz, 6 H), 3.83 (d, J = 0.6 Hz, 3 H), 3.19–3.12 (m, 2 H), 2.52 (td, J = 13.0, 3.7 Hz, 1 H), 1.97–1.90 (m, 2 H), 1.78 (dd, J = 12.3, 7.6 Hz, 1 H), 1.73–1.71 (m, 1 H), 1.69 (s, 3 H), 1.66–1.64 (m, 1H), 1.62–1.52 (m, 5 H), 1.58–1.33 (m, 9 H), 1.30–1.23 (m, 3 H), 1.14 (dt, J = 13.3, 3.0 Hz, 1 H), 0.97 (s, 3 H), 0.96 (s, 3 H), 0.95–0.92 (m, 1 H), 0.90 (s, 3 H), 0.81 (s, 3 H), 0.75 (s, 3 H), 0.68–0.65 (m, 1 H); 13C NMR (151 MHz, CDCl3) δ 175.9, 153.4, 150.8, 137.1, 135.0, 129.0, 128.2, 109.5, 104.6, 79.0, 60.8, 56.0, 55.7, 55.4, 50.6, 50.1, 46.7, 43.3, 42.5, 40.7, 38.8, 38.7, 38.4, 37.6, 37.2, 34.4, 33.7, 30.9, 29.4, 28.0, 27.4, 25.6, 24.9, 20.9, 19.5, 18.3, 16.2, 16.1, 15.3, 14.6; HR-ESI (m/z) [M + H+] calculated for C40H61NO5 635.4550. Found: 635.4573; HPLC analysis: analysis: peak area 98.9%, tR = 6.02 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
General procedure for the synthesis of betulin p-nitrophenylcarbonate ester 5
To a stirring solution of compound 1 (200 mg, 0.45 mmol) in dry THF (10 mL), under Ar atmosphere, pyridine (36 μL, 0.45 mmol) was added, and the mixture was cooled to 0 °C. p-nitrophenylchloroformate (94.3 mg, 0.47 mmol) was added in 3 portions and the reaction mixture was stirred for 24 h at ambient temperature. Consequently, the mixture was concentrated under reduced pressure to dryness. The solid residue obtained was diluted in DCM and washed sequentially with 5% aqueous ice-cold citric acid, water, and brine, dried over anhydrous Na2SO4, filtered and concentrated to dryness. The desired product was afforded as a white foam (227 mg) after FCC purification using PhMe/EtOAc 95:5 as eluent. Yield = 83%; White foam; Rf (PhMe/EtOAc 95:5) = 0.14; 1H NMR (600 MHz, CDCl3) δ 8.29 (s, 1 H), 8.28 (s, 1 H), 7.41 (s, 1 H), 7.39 (s, 1 H), 4.71 (br s, 1 H), 4.61 (t, J = 1.7 Hz, 1 H), 4.51 (dd, J = 10.8 Hz, 2.0 Hz, 1 H), 4.08 (d, J = 10.7 Hz, 1 H), 3.19 (dd, J = 11.4, 4.8 Hz, 1 H), 2.45 (td, J = 10.8, 5.4 Hz, 1 H), 2.03 (dtd, J = 14.2, 10.5, 4.9 Hz, 1 H), 1.95–1.84 (m, 2 H), 1.75 (td, J = 13.9, 4.7 Hz, 1 H), 1.70 (s, 3 H), 1.68–1.08 (m, 19 H), 1.05 (s, 3 H), 1.00 (s, 3 H), 0.97 (s, 3 H), 0.91 (td, J = 12.5, 3.7 Hz, 1 H), 0.83 (s, 3 H), 0.76 (s, 3 H), 0.69 (d, J = 11.2 Hz, 1 H);. 13C NMR (151 MHz, CDCl3) δ 155.6, 153.0, 149.7, 145.3, 125.3, 121.8, 78.9, 68.3, 55.3, 50.3, 48.8, 47.7, 46.7, 42.7, 40.9, 38.9, 38.7, 37.7, 37.1, 34.4, 34.2, 29.6, 29.5, 28.0, 27.4, 27.0, 25.2, 20.7, 18.3, 16.1, 16.0, 15.3, 14.8.
General procedure for the synthesis of betulin carbamates 6a-m
To a stirring solution of carbonate ester 5 (0.16 mmol) in dry THF (0.2 M), under Ar atmosphere, the corresponding amine (appropriate equivalents for each case, see below) and DIPEA (1 eq) were added, and the reaction mixture was stirred at ambient temperature or heated at 50–60 °C. After completion of the reaction the mixture was diluted in EtOAc and washed sequentially with 5% aqueous ice-cold citric acid, water, and brine, dried over anhydrous Na2SO4, filtered, and concentrated to dryness. The residue thus obtained was purified by FCC to provide, upon solvent removal, the corresponding carbamates 6a-m.
6a: compound 6a was prepared using 3 equivalents of 3,4,5-trimethoxyaniline and overnight heating. Yield = 45%; Colorless oil; Rf (PhMe/EtOAc 9:1) = 0.11; 1H NMR (600 MHz, CDCl3) δ 6.69 (s, 1 H), 6.58 (s, 1 H), 4.70 (d, J = 2.5 Hz, 1 H), 4.60 (t, J = 1.7 Hz, 1 H), 4.34 (d, J = 10.7 Hz, 1 H), 4.07 (t, J = 6.8 Hz, 1 H), 3.98 (d, J = 10.1 Hz, 1 H), 3.85 (s, 6 H), 3.81 (s, 3 H), 3.19 (dd, J = 11.5, 4.7 Hz, 1 H), 2.47 (td, J = 11.1, 5.7 Hz, 1 H), 2.02–1.98 (m, 1 H), 1.91–1.71 (m, 4 H), 1.70 (s, 3 H), 1.66–1.51 (m, 5 H), 1.45–1.37 (m, 6 H), 1.30–1.25 (m, 2 H), 1.22 (dd, J = 12.8, 4.7 Hz, 1 H), 1.12–1.07 (m, 2 H), 1.06 (s, 3 H), 1.04–1.00 (m, 1 H), 0.99 (s, 3 H), 0.98 (s, 3 H), 0.95–0.92 (m, 1 H), 0.91–0.88 (m, 1 H), 0.83 (s, 3 H), 0.77 (s, 3 H), 0.69 (d, J = 9.5 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 153.4, 150.1, 134.0, 125.3, 121.8, 109.9, 79.0, 64.4, 61.0, 56.1, 55.3, 50.4, 48.8, 47.7, 46.5, 42.7, 40.9, 38.9, 38.7, 37.6, 37.1, 34.5, 34.2, 29.8, 29.6, 28.0, 27.4, 27.1, 25.2, 20.8, 18.3, 16.1, 15.3, 14.8, 13.7; HR-ESI (m/z) [M + H+] calculated for C40H62NO6 652.4509. Found: 652.4557; HPLC analysis: peak area 96.2%, tR = 9.59 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
6b: compound 6b was prepared using 1.1 equivalents of 4-methoxybenzylamine at room temperature for 24 h. Yield = 60%; Colorless oil; Rf (PhMe/EtOAc 9:1) = 0.15; 1H NMR (600 MHz, CDCl3) δ 7.24–7.20 (m, 2 H), 6.88–6.84 (m, 2 H), 4.89 (br s, 1 H), 4.68 (d, J = 2.5 Hz, 1 H), 4.58 (t, J = 1.5 Hz, 1 H), 4.34–4.25 (m, 3 H), 3.88 (d, J = 10.6 Hz, 1 H), 3.80 (s, 3 H), 3.18 (dd, J = 11.5, 4.7 Hz, 1 H), 2.45 (tt, J = 10.8, 5 Hz, 1 H), 1.99 (h, J = 9.9 Hz, 2 H), 1.81 (d, J = 13.0 Hz, 1 H), 1.79–1.72 (m, 2 H), 1.71–1.69 (m, 1 H), 1.68 (s, 3 H), 1.62–1.50 (m, 9 H), 1.43–1.35 (m, 5 H), 1.26 (s, 3 H), 1.21 (dd, J = 13.2, 4.9 Hz, 2 H), 1.11 (s, 1 H), 1.04 (s, 3 H), 0.97 (s, 3 H), 0.93–0.86 (m, 1 H), 0.83 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 9.4 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 129.0, 128.2, 114.1, 109.8, 79.0, 55.3, 50.4, 48.8, 47.7, 46.6, 42.7, 40.9, 38.9, 38.7, 37.5, 37.1, 34.2, 29.7, 28.0, 27.4, 27.1, 25.2, 20.8, 18.3, 16.1, 16.1, 15.3, 14.7; HR-ESI (m/z) [M + H+] calculated for C39H60NO4 606.4522. Found: 606.4520; HPLC analysis: peak area 100%, tR = 8.72 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
6c: compound 6c was prepared using 1.1 equivalents of 3,4-dimethoxybenzylamine at room temperature for 1 h. Yield = 66%; Colorless oil; Rf (PhMe/EtOAc 9:1) = 0.09; 1H NMR (600 MHz, CDCl3) δ 6.84 (s, 1 H), 6.82 (s, 2 H), 4.92 (s, 1 H), 4.69 (d, J = 2.5 Hz, 1 H), 4.58 (t, J = 1.5 Hz, 1 H), 4.31 (s, 2 H), 4.29 (s, 1 H), 3.87 (s, 3 H), 3.87 (s, 3 H), 3.18 (dd, J = 11.4, 4.8 Hz, 1 H), 2.45 (td, J = 11.1, 5.7 Hz, 1 H), 1.99 (qui, J = 9.9 Hz, 1 H), 1.82 (d, J = 13.7 Hz, 1 H), 1.79–1.72 (m, 3 H), 1.68 (s, 3 H), 1.66–1.11 (m, 19 H), 1.04 (s, 3 H), 0.97 (s, 6 H), 0.92–0.86 (m, 1 H), 0.82 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 8.4 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 149.2, 137.9, 129.0, 128.2, 125.3, 111.2, 111.0, 109.8, 79.0, 56.0, 55.9, 55.3, 50.4, 48.8, 47.7, 46.6, 42.7, 40.9, 38.8, 38.7, 37.5, 34.5, 34.2, 29.8, 29.6, 28.0, 27.4, 27.1, 25.2, 21.4, 20.8, 19.1, 18.3, 16.1, 16.0, 15.3, 14.8; HR-ESI (m/z) [M + H+] calculated for C40H62NO5 636.4628. Found: 636.4631; HPLC analysis: peak area 95.1%, tR = 8.56 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
6d: compound 6d was prepared using 1.1 equivalents of 3,4,5-trimethoxybenzylamine at room temperature for 1.5 h. Yield = 62%; White solid; m.p.: 153.154.5 °C; Rf (PhMe/EtOAc 9:1) = 0.14; 1H NMR (600 MHz, CDCl3) δ 6.52 (s, 2 H), 4.96 (s, 1 H), 4.69 (d, J = 2.3 Hz, 1 H), 4.59 (t, J = 1.5 Hz, 1 H), 4.33 (s, 1 H), 4.31 (s, 2 H), 3.90 (d, J = 11.4 Hz, 1 H), 3.85 (s, 6 H), 3.83 (s, 3 H), 3.18 (dd, J = 11.4, 4.7 Hz, 1 H), 2.45 (td, J = 11.1, 5.8 Hz, 1 H), 2.04–1.94 (m, 1 H), 1.82 (d, J = 14.0 Hz, 1 H), 1.79–1.72 (m, 3 H), 1.68 (s, 3 H), 1.61–1.47 (m, 9 H), 1.44–1.34 (m, 5 H), 1.29–1.18 (m, 4 H), 1.05 (s, 3 H), 0.97 (s, 6 H), 0.90 (dd, J = 12.7, 3.7 Hz, 1 H), 0.82 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 9.2 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 153.4, 134.3, 109.8, 104.6, 79.0, 60.8, 56.1, 55.3, 50.4, 48.8, 47.7, 46.6, 42.7, 40.9, 38.9, 38.7, 37.5, 37.1, 34.5, 34.2, 29.8, 29.6, 28.0, 27.4, 27.1, 25.2, 20.8, 19.1, 18.3, 16.1, 16.0, 15.3, 14.8; HR-ESI (m/z) [M + H+] calculated for C41H64NO6 666.4733. Found: 666.4730; HPLC analysis: peak area 95.0%, tR = 8.49 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
6e: compound 6e was prepared using 1.1 equivalents of 4-methoxyphenylethylamine at room temperature for 24 h. Yield = 55%; Colorless oil; Rf (PhMe/EtOAc 95:5) = 0.1; 1H NMR (600 MHz, CDCl3) δ 7.10 (d, J = 8.5 Hz, 2 H), 6.84 (d, J = 8.5 Hz, 2 H), 4.69 (d, J = 2.3 Hz, 1 H), 4.65 (br s, 1 H), 4.58 (t, J = 1.7 Hz, 1 H), 4.25 (dd, J = 10.9, 1.9 Hz, 1 H), 3.83 (d, J = 11.6 Hz, 1 H), 3.79 (s, 3 H), 3.45–3.37 (m, 2 H), 3.18 (dd, J = 11.5, 4.8 Hz, 1 H), 2.76 (t, J = 6.8 Hz, 2 H), 2.54–2.37 (m, 1 H), 1.97 (m, 1 H), 1.88–1.70 (m, 3 H), 1.68 (s, 3 H), 1.66–1.48 (m, 7 H), 1.44–1.35 (m, 5 H), 1.29–1.77 (m, 5 H), 1.11 (s, 1 H), 1.04 (s, 3 H), 1.02 (s, 1 H), 0.97 (m, 6 H), 0.91 (dd, J = 12.9, 3.7 Hz, 1 H), 0.82 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 9.6 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 158.3, 157.0, 150.5, 150.3, 129.7, 129.0, 128.2, 125.3, 114.0, 109.7, 79.0, 63.0, 60.5, 55.3, 50.4, 48.8, 47.8, 47.7, 46.6, 42.7, 40.9, 38.9, 38.7, 37.5, 37.1, 34.2, 29.7, 29.2, 28.0, 27.4, 27.1, 25.2, 21.4, 20.8, 19.1, 18.3, 16.1, 16.0, 15.3, 14.7; HR-ESI (m/z) [M + H+] calculated for C40H62NO4 620.4679. Found: 620.4676; HPLC analysis: peak area 98.0%, tR = 9.32 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
6f: compound 6f was prepared using 1.1 equivalents of 3,4-dimethoxyphenylethylamine at room temperature for 72 h. Yield = 50%; Colorless oil; Rf (PhMe/EtOAc 9:1) = 0.10; 1H NMR (600 MHz, CDCl3) δ 6.81 (d, J = 8.1 Hz, 1 H), 6.74–6.69 (m, 2 H), 4.68 (d, J = 2.6 Hz, 1 H), 4.67–4.64 (m, 1 H), 4.58 (t, J = 1.7 Hz, 1 H), 4.26 (d, J = 12.4 Hz, 1 H), 3.87 (s, 3 H), 3.86 (s, 3 H), 3.84–3.81 (m, 1 H), 3.47–3.36 (m, 2 H), 3.18 (dd, J = 11.4, 4.7 Hz, 1 H), 2.76 (t, J = 6.9 Hz, 2 H), 2.44 (td, J = 10.7, 5.7 Hz, 1 H), 1.98 (qui, J = 9.1 Hz, 1 H), 1.81–1.69 (m, 3 H), 1.67 (s, 3 H), 1.65–1.48 (m, 7 H), 1.39 (m, 6 H), 1.30–1.18 (m, 5 H), 1.04 (s, 3 H), 1.02–0.99 (m, 1 H), 0.96 (s, 6 H), 0.89 (td, J = 12.9, 4.0 Hz, 1 H), 0.82 (s, 3 H), 0.76 (s, 3 H), 0.67 (d, J = 9.4 Hz, 1 H) 13C NMR (151 MHz, CDCl3) δ 158.4, 157.0, 149.0, 147.7, 120.7, 118.8, 112.0, 111.4, 109.8, 79.0, 55.9, 55.8, 55.3, 50.4, 48.8, 47.7, 46.6, 42.7, 42.3, 40.9, 38.9, 38.7, 37.5, 37.1, 35.7, 34.2, 29.6, 28.0, 27.4, 27.1, 25.2, 20.8, 19.1, 18.3, 16.1, 16.0, 15.3, 14.7; HR-ESI (m/z) [2 M + H+] calculated for [C41H63NO5] 1299.9492. Found: 1299.9467. HPLC analysis: peak area 96.4%, tR = 8.35 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
6g: compound 6g was prepared using 1.1 equivalents of 3,4,5-trimethoxyphenylethylamine at room temperature for 72 h. Yield = 55%; Colorless oil; Rf (PhMe/EtOAc 9:1) = 0.25; 1H NMR (600 MHz, CDCl3) δ 6.40 (s, 2 H), 4.71–4.69 (m, 1 H), 4.69 (d, J = 2.5 Hz, 1 H), 4.58 (t, J = 1.9 Hz, 1 H), 4.27 (d, J = 10.9 Hz, 1 H), 3.88–3.86 (m, 1 H), 3.85 (s, 6 H), 3.83 (s, 3 H), 3.44 (qui, J = 6.4 Hz, 2 H), 3.18 (dd, J = 11.4, 4.8 Hz, 1 H), 2.76 (t, J = 7.2 Hz, 2 H), 2.49–2.39 (m, 1 H), 1.99 (qui, J = 9.2 Hz, 1 H), 1.82–1.71 (m, 3 H), 1.68 (s, 3 H), 1.65–1.48 (m, 8 H), 1.39 (m, 6 H), 1.29–1.17 (m, 4 H), 1.04 (s, 3 H), 1.03–1.00 (m, 1 H), 0.97 (s, 6 H), 0.90 (td, J = 12.9, 4.0 Hz, 1 H), 0.82 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 9.4 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 157.0, 153.3, 150.2 137.9, 129.0, 128.2, 125.3, 109.8, 105.7, 79.0, 63.0, 60.8, 56.1, 55.3, 50.4, 48.8, 47.7, 46.6, 42.7, 42.2, 40.9, 38.8, 38.7, 37.5, 37.1, 36.6, 34.5, 34.2, 29.8, 29.6, 28.0, 27.4, 27.1, 25.2, 21.4, 20.8, 19.1, 18.3, 16.1, 16.0, 15.3, 14.8; HR-ESI (m/z) [M + H+] calculated for C42H66NO6 680.4890. Found: 680.4791; HPLC analysis: peak area 95.2%, tR = 8.99 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
6h: compound 6h was prepared using 20 equivalents of piperazine at room temperature for 18 h. Yield = 75%; Colorless oil; Rf (DCE/MeOH 9:1) = 0.36; 1H NMR (600 MHz, CDCl3) δ 4.68 (d, J = 2.6 Hz, 1 H), 4.58 (t, J = 1.7 Hz, 1 H), 4.27 (d, J = 10.7 Hz, 1 H), 3.86 (d, J = 10.8 Hz, 1 H), 3.72 (s, 1 H), 3.51 (br s, 4 H), 3.17 (dd, J = 11.4, 4.8 Hz, 1 H), 2.89 (br s, 4 H), 2.80–2.62 (m, 2 H), 2.45 (td, J = 11.1, 5.0 Hz, 1 H), 2.03–1.93 (m, 1 H), 1.83–1.79 (m, 1 H), 1.78–1.69 (m, 3 H), 1.67 (s, 3 H), 1.66–1.48 (m, 5 H), 1.43–1.33 (m, 5 H), 1.31–1.15 (m, 4 H), 1.10–1.04 (m, 2 H), 1.03 (s, 3 H), 0.97 (s, 3 H), 0.96 (s, 3 H), 0.89 (td, J = 12.9, 4.2 Hz, 1 H), 0.81 (s, 3 H), 0.75 (s, 3 H), 0.67 (d, J = 9.3 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 155.8, 150.2, 129.0, 128.2, 109.8, 78.9, 63.9, 55.3, 50.4, 48.8, 47.7, 46.6, 45.3, 43.4, 42.7, 40.9, 38.8, 38.7, 37.5, 37.1, 34.6, 34.2, 30.0, 29.6, 28.0, 27.4, 27.1, 25.2, 20.8, 19.1, 18.3, 16.1, 16.1, 15.4, 14.8; HR-ESI (m/z) [M + H+] calculated for C35H59N2O3 555.4457. Found 555.4487; HPLC analysis: peak area 98.2%, tR = 12.34 min, gradient: 45% (3 min to 45%) to 100% B over 20 min.
6i: compound 6i was prepared using 1.1 equivalents of N-methylpiperazine without DIPEA at room temperature for 15 h. Yield = 68%; White solid; m.p.: 189–190 °C; Rf (PhMe/EtOAc 1:9) = 0.13; 1H NMR (600 MHz, CDCl3) δ 4.69 (d, J = 2.5 Hz, 1 H), 4.59 (t, J = 1.7 Hz, 1 H), 4.29 (d, J = 9.3 Hz, 1 H), 3.88 (d, J = 10.9 Hz, 1 H), 3.68 (br s, 4 H), 3.18 (dd, J = 11.6, 4.8 Hz, 1 H), 2.78–2.48 (m, 4 H), 2.47–2.39 (m, 1 H), 2.02–1.94 (m, 1 H), 1.83–1.69 (m, 4 H), 1.68 (s, 3 H), 1.66–1.47 (m, 6 H), 1.43–1.36 (m, 5 H), 1.30–1.15 (m, 7 H), 1.11–1.05 (m, 2 H), 1.04 (s, 3 H), 0.98 (s, 3 H), 0.97 (s, 3 H), 0.93–0.85 (m, 2 H), 0.82 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 9.6 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 155.6, 150.1, 129.0, 128.2, 125.3, 109.9, 91.5, 79.0, 64.2, 55.3, 54.2, 50.4, 48.8, 47.7, 46.6, 42.7, 40.9, 38.9, 38.7, 37.5, 37.1, 34.6, 34.2, 30.0, 29.6, 28.0, 27.4, 27.1, 25.2, 20.8, 19.1, 18.3, 16.1, 16.1, 15.3, 14.8; HR-ESI (m/z) [M + H+] calculated for C36H61N2O3 569.4682. Found: 569.4669; HPLC analysis: peak area 98.0%, tR = 9.65 min, gradient: 25% (3 min to 25%) to 75% B over 20 min.
6j: compound 6j was prepared using 1.1 equivalents of tert-butyl-4-(2-aminoethyl) piperazine-1-carboxylate at room temperature for 20 h. Yield = 70%; Colorless oil; Rf (EtOAc) = 0.4; 1H NMR (600 MHz, CDCl3) δ 5.08 (s, 1 H), 4.68 (d, J = 2.6 Hz, 1 H), 4.58 (t, J = 2.0 Hz, 1 H), 4.30–4.24 (m, 2 H), 3.85 (d, J = 11.1 Hz, 1 H), 3.71 (td, J = 5.8, 1.7 Hz, 2 H), 3.42 (br s, 4 H), 3.30 (br s, 1 H), 3.18 (dd, J = 11.6, 4.8 Hz, 1 H), 2.50–2.47 (m, 1 H), 2.39 (br s, 4 H), 2.02–1.95 (m, 1 H), 1.85 (d, J = 12.9 Hz, 1 H), 1.79 (dd, J = 12.4, 7.3 Hz, 1 H), 1.74 (d, J = 12.5 Hz, 1 H), 1.68 (s, 3 H), 1.65–1.48 (m, 9 H), 1.46 (s, 9 H), 1.43–1.35 (m, 5 H), 1.31–1.22 (m, 5 H), 1.04 (s, 3 H), 0.97 (s, 3 H), 0.96 (s, 3 H), 0.92–0.85 (m, 1 H), 0.82 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 9.3 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 171.1, 157.1, 154.7, 150.3, 129.0, 128.2, 125.3, 109.8, 79.7, 79.0, 64.3, 63.1, 57.2, 55.3, 52.7, 50.4, 48.8, 47.7, 46.6, 42.7, 40.9, 38.9, 38.7, 37.5, 37.1, 34.6, 34.2, 30.6, 29.7, 28.4, 28.0, 27.4, 27.1, 25.2, 20.8, 19.1, 18.3, 16.1, 16.0, 15.3, 14.8, 13.7; HR-ESI (m/z) [M + H+] calculated for C42H72N3O5 698.5472. Found: 698.5447; HPLC analysis: peak area 98.7%, tR = 8.27 min, gradient: 25% (3 min to 25%) to 75% B over 20 min.
6l: compound 6l was prepared using 1.1 equivalents of 4-(4-Methylpiperazino) benzylamine at room temperature for 24 h. Yield = 42%; White solid; m.p.: 151–152 °C; Rf (EtOAc/Et3N 10:0.1) = 0.33; 1H NMR (600 MHz, CDCl3) δ 7.21–7.17 (m, 2 H), 6.90 (s, 1 H), 6.88 (s, 1 H), 4.88 (br s, 1 H), 4.68 (d, J = 2.5 Hz, 1 H), 4.58 (t, J = 1.9 Hz, 1 H), 4.30–4.24 (m, 3 H), 3.87 (d, J = 11.2 Hz, 1 H), 3.29 (br s, 4 H), 3.18 (d, J = 11.1 Hz, 1 H), 2.72 (br s, 4 H), 2.48–2.41 (m, 4 H), 2.01–1.94 (m, 1 H), 1.84–1.72 (m, 3 H), 1.67 (s, 3 H), 1.63–1.48 (m, 6 H), 1.44–1.34 (m, 5 H), 1.29–1.17 (m, 6 H), 1.04 (s, 3 H), 1.02–0.99 (m, 1 H), 0.96 (s, 6 H), 0.89 (td, J = 13.1, 4.4 Hz, 2 H), 0.82 (s, 3 H), 0.76 (s, 3 H), 0.67 (d, J = 9.5 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 171.1, 157.0, 150.3, 129.0, 128.8, 128.2, 116.4, 109.7, 79.0, 63.2, 60.4, 55.3, 54.7, 50.4, 48.8, 48.6, 47.7, 46.6, 44.6, 42.7, 40.9, 38.9, 38.7, 37.5, 37.1, 34.5, 34.2, 29.8, 29.7, 28.0, 27.4, 27.1, 25.2, 21.0, 20.8, 19.1, 18.3, 16.1, 16.1, 15.3, 14.7, 14.2; HR-ESI (m/z) [M + H+] calculated for C43H68N3O3 674.5260. Found: 674.5258; HPLC analysis: peak area 96.4%, tR = 11.5 min, gradient: 50% (3 min to 50%) to 100% B over 20 min.
6m: compound 6m was prepared using 1.1 equivalents of 6,7-dimethoxy-1,2,3,4-tetrahydro-isoquinoline at room temperature for 17 h. Yield = 42%; Rf (PhMe/EtOAc9:1) = 0.18; Colorless oil; 1H NMR (600 MHz, CDCl3) δ 6.62 (s, 1 H), 6.60 (br s, 1H), 4.69 (d, J = 2.6 Hz, 1 H), 4.59 (t, J = 1.9 Hz, 1 H), 4.55 (d, J = 10.3 Hz, 2 H), 4.31 (d, J = 10.4 Hz, 1 H), 3.90 (d, J = 10.9 Hz, 1 H), 3.86 (s, 6 H), 3.72–3.63 (m, 2 H), 3.18 (dd, J = 11.5, 4.7 Hz, 1 H), 2.77 (s, 2 H), 2.48 (td, J = 11.2, 5.8 Hz, 1 H), 2.06–1.96 (m, 1 H), 1.93–1.81 (m, 2 H), 1.78–1.70 (m, 2 H), 1.69 (s, 3 H), 1.67–1.48 (m, 8 H), 1.45–1.35 (m, 5 H), 1.31–1.17 (m, 4 H), 1.07–1.05 (m, 1 H), 1.04 (s, 3 H), 0.99 (s, 3 H), 0.97 (s, 3 H), 0.90 (td, J = 13.5, 4.7 Hz, 1 H), 0.82 (s, 3 H), 0.76 (s, 3 H), 0.68 (d, J = 9.4 Hz, 1 H); 13C NMR (151 MHz, CDCl3) δ 150.2, 147.7, 147.7, 137.9, 129.0, 128.2, 125.3, 111.5, 109.8, 79.0, 63.8, 56.0, 56.0, 55.3, 50.4, 48.8, 47.7, 46.7, 42.7, 40.9, 38.9, 38.7, 37.5, 37.2, 34.7, 34.2, 30.1, 29.7, 28.0, 27.4, 27.2, 25.2, 21.4, 20.8, 19.2, 18.3, 16.1, 15.3, 14.8; HR-ESI (m/z) [M + H+] calculated for C42H64NO5 662.4784. Found: 662.4775; HPLC analysis: peak area 98.6%, tR = 10.90 min, gradient: 90% (3 min to 90%) to 95% B over 5 min and from 95 to 100% B over 10 min.
Deprotection of compound 6j
To an ice-cold solution of 6j (9 mg, 0.01 mmol) in DCM (40 μL), trifluoroethanol (0.05 mmol, 5μL) and TFA (0.25 mmol, 20μL) were added and the reaction mixture was stirred at ambient temperature for 3 h. Volatile components were evaporated under vacuum, the oily residue was triturated with a mixture of diethyl ether (Et2O)/hexane, and refrigerated overnight. The desired trifluoroacetate salt 6k was afforded as pale-yellow oil. Yield = 90%; HR-ESI (m/z) [M+] calculated for C37H65N3O3+ 598.4942. Found: 598.4932; HPLC analysis: peak area 98.4%, tR = 8.28 min, gradient: 25% (3 min to 25%) to 75% B over 20 min.
Material for biological studies
3-(4,5-Dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide (MTT), histopaque 1077, lectin from Phaseolus vulgaris (PHA), and Rho123 were obtained from Sigma Aldrich (Sigma-Aldrich Co., St Louis, MO). Doxorubicin hydrochloride (Dox, 99.8%, Synbias Pharma Ltd.) was obtained from Nanox Release Technology (Buenos Aires, Argentina) and was prepared immediately prior to use dissolved in bi-distilled water. Verapamil hydrochloride 98.0% was provided by Parafarm (Buenos Aires, Argentina) while tariquidar was purchased from ChemFaces Biochemical Co., Ltd (Wuhan, China). Both were prepared in DMSO. Sterile plastic material was purchased from Greiner Bio-One (Frickenhausen, Germany). Flow cytometry was carried out in a Life Technologies Attune-NxT flow cytometer with 96-well autosampler (Thermo Fisher Scientific, USA).
Cell lines and cell culture
The sensitive CML cells K562 and its counterpart P-gp-overexpressing K562/Dox cells, formerly Lucena 1 with MDR phenotype mainly characterized by the overexpression of ABCB1/P-gp54, were cultured in RPMI-1640 medium (Invitrogen Life Technologies, Carlsbad, CA) supplemented with 10% fetal bovine serum, 2 mM L-glutamine, 100 U/mL penicillin, and 100 μg/mL streptomycin (Invitrogen Life Technologies, Carlsbad, CA) at 37 °C in a 5% CO2 humidified atmosphere. Both cell lines were provided by Dr. V. Rumjanek, Universidade Federal do Rio de Janeiro, Rio de Janeiro, Brazil54. Passages were performed twice a week and cells in exponential growth phase with a viability of 90%, determined by trypan blue exclusion, were used for the experiments. To give rise to the MDR phenotype, resistant lines were subjected to continuous treatment with 60 nM of Dox. This treatment was interrupted 4 days before each trial. K562/Dox displayed 32.3-fold more resistance to Dox than K562, as evidenced by the IC50 values obtained by MTT assay (IC50 = 84.21 ± 7.08 and 2.61 ± 0.70 µM, respectively). This level of resistance correlates with the level of expression of P-gp31.
MTT colorimetric assay
The cytotoxic effect of the compounds and of the gold standards verapamil and tariquidar was determined against K562/Dox and K562 using MTT assay. This colorimetric technique is based on the ability of viable cells to capture MTT and reduce it through the mitochondrial enzyme succinic dehydrogenase to its insoluble form, formazan crystals55. The target compounds dissolved in DMSO (0.5% v/v as final concentration which was non-toxic to cells) at a maximum concentration of 50 µM were exposed to 5 × 104 cells distributed in a 96-well plate and incubated for 48 h. At the end of the incubation period, the cells were treated with 5 mg/mL of MTT solution prepared in phosphate buffered saline (PBS) and incubated at 37 °C in a humid atmosphere with 5% CO2 for another 4 h. After this time, the plate was centrifuged at 2000 rpm for 10 min, and 100 µL of DMSO was added to dissolve the formazan crystals formed. Absorbance (Abs) was read at a wavelength of 595 nm in an iMark microplate reader (Bio-Rad, USA). The percentages of cytotoxicity were determined as compared to DMSO treated control cells, which were considered 100% viable as showing the same level of growth as the untreated cells. Those compounds showing a cytotoxicity > 55% at 50 µM were further assayed with a range of two-fold decreasing concentrations for their IC50 values, which were calculated as previously reported56,57 using non-linear regression by GraphPad Prism 7 (GraphPad Software, Inc., San Diego, CA, USA, www.graphpad.com).
Rhodamine 123 and doxorubicin intracellular accumulation assays
The ability of the compounds to increase the intracellular concentration of Rho123 or of Dox by the inhibition of P-gp was evaluated using flow cytometry, as described earlier32,33,58. K562/Dox or K562 cells adjusted to a density of 5 × 104 cells/well were seeded in 96-well plates, previously containing RPMI-1640 medium in the presence of each compound dissolved in DMSO, at concentrations ranging from 0.049 to 50 µM and from 6.25 to 50 µM for each cell line, respectively. Cells treated only with DMSO at 0.5% v/v were used as negative controls, while those treated with the standard P-gp inhibitors42, verapamil and tariquidar were used as positive controls. No differences between negative controls and untreated cells were observed. The samples were incubated for 1 h at 37 °C in a humid atmosphere with 5% CO2. At the end of the incubation period, the corresponding fluorescent substrate, Rho123 (500 ng/mL) or Dox (5 μM), was added, and the cells were incubated for another 1 h. Subsequently, cells were thoroughly washed twice with cold PBS and kept in dark and cold. Samples were gated on a forward versus size scatter, and 15,000 events from each were analyzed to determine the cell-associated fluorescence. It is important to notice that the target derivatives were not fluorescent by themselves (data not shown).
Dox and Rho123 were excited at 488 nm, and the fluorescence emitted was collected with 585/42 nm or 530/30 nm bandpass filters, respectively. Mean fluorescence intensity (MFI) was analyzed using Flowjo software (Tree Star, Inc. Ashland, OR). The blocking of the P-gp transport function was evaluated by the parameter fluorescence activity ratio (FAR), calculated as the ratio of the MFI of Rho123 or Dox with the addition of the likely inhibitor to the MFI of Rho123 or Dox alone.
Doxorubicin resistance reversal assay
These experiments were undertaken to evaluate the ability of the two most effective compounds to potentiate Dox cytotoxicity by inhibiting the outward transport mediated by P-gp. MTT staining was used, for which 5 × 104 K562/Dox and K562 cells/well and increasing concentrations of Dox (3.4–431 and 0.33–34.5 µM, respectively) in the absence or presence of 0.024 to 1.56 µM and 0.19 to 1.56 µM of compounds 6g and 6i, respectively, were incubated in 96-well plates containing RPMI-1640 medium. DMSO (0.5% v/v) was used as a negative control, while verapamil was chosen as standard inhibitor. Simultaneously, viability controls were run with no addition of the dissolution solvent. The cells were incubated at 37 °C at 5% CO2 for 48 h and the same protocol described above was followed. The potency of the compounds was established by means of the fold reversal (FR) values calculated from dividing the IC50 of Dox alone by the IC50 of Dox with different concentrations of each compound tested.
Cytotoxicity on peripheral blood mononuclear cells and hemolysis assay
In order to preliminarily determine the safety of the active compounds 6g and 6i in normal cells, different concentrations (1.56–50 µM) of these were assayed by the MTT technique on peripheral blood mononuclear cells (PBMC) according to published works33,58. PBMC were isolated by the Ficoll-Hypaque density gradient centrifugation technique of fresh heparinized blood from healthy human volunteers. The protocol was previously approved by the Catholic University of Córdoba Research Ethics Board. Signed informed consents were obtained from donors. All methods were performed in accordance with the relevant guidelines and regulations. Briefly, 1 × 105 cells/well in a 96-well plate were incubated with 10 µg/mL PHA, in the presence of the corresponding concentrations of the compounds or 0.5% v/v DMSO (negative control) for 48 h, and processed as above described for the MTT method. The percentages of inhibition on cell proliferation were determined by comparison with negative controls, and the corresponding IC50 values were calculated from the best fit of the concentration-dependent inhibition curves in GraphPad Prism 7.
For the erythrocyte hemolysis assay, the red blood cell suspension was obtained from fresh heparinized blood collected from healthy human volunteer donors, without receiving any treatment. The blood sample was centrifuged at 2,500 rpm for 10 min at 4 °C. The supernatant was discarded, and the red blood cell pellet was subjected to two consecutive washes with sterile PBS, using the same centrifugation conditions. An aliquot of the pellet obtained was resuspended in PBS (3% v/v). The compounds were incubated at decreasing concentrations starting from 50 µM with the suspension at 37 °C for 1 h. Controls with 1% DMSO and no solvent were included.
Statistical analysis
The results are expressed as the mean ± standard error (SE). Data were analyzed using the one-tailed paired Student's t-test and one-tailed unpaired Student's t-test, as appropriate, by GraphPad Prism 7.0. p values ≤ 0.05 were considered statistically significant. Each experiment was performed in triplicate or quadruplicate and done independently at least three times.
Molecular modeling
The structural model of the P-gp was based on the structure cocrystallized with paclitaxel (PDB entry 6QEX)51, and prepared as described in detail in Laiolo et al.33. In this work, the structure 7A69, cocrystallized with the antitumoral agent vincristine52, was also used for checking the docking procedure, although the simulations of vincristine were made on the same receptor (based on 6QEX) used for the rest of the substrates and inhibitors.
The docking protocol was fairly similar to that in Laiolo et al.33. Briefly, the box included the whole TM region (no assumption about a particular binding site) and the docking was run with Autodock Vina 1.1.2-559, collecting the first 12 lowest energy poses or those within 3 kcal/mol above the lowest. The “exhaustiveness” parameter was set between 64 and 192 (much bigger than the default, 8, due to the size of the region), and repeating the simulation at least 12 times. Standard Gagsteiger’s charges59 were set for all ligands except for Rho123, for which RESP charges60 at the CAM-B3LYP/6–31 + G(d) level of theory61 were used to correctly draw the charge delocalization of the cationic dye. The structure of the ligands were obtained by full geometry optimization with the semiempirical PM6 Hamiltonian as implemented in Gaussian 16 Rev. A0362 The structures were confirmed as minima by diagonalization of the Hessian matrix.
The initial structures for the MD simulations were prepared from the most stable docked structures using the AMBER1863 utilities LEaP, parmchk2 and antechamber64. The atomic charges on the ligands were obtained with the AMBER18 module sqm, using AM1 quantum calculations and the parameters assigned based on the auxiliary force field GAFF.63. The protocol for running the MD simulations was successfully applied in Laiolo et al.32,33. This involves: (I) 250 steepest descent minimization steps of the whole system, keeping the protein tightly restrained and embedded into a box of TIP3P water molecules with a minimum distance of 10 Å to each wall, and enough chloride counter-ions to reach electro-neutrality; (II) 6500 conjugate gradient minimization steps of the whole system; (III) 100 ps slowly heating in the NTV ensemble with the protein positionally restrained in the backbone; (IV) 60 ns of simulation in the NTP ensemble, at 1 atm and 300 K. Procedures III-IV were repeated in two or three independent trajectories using the Andersen thermostat and barostat65. In the reasonably equilibrated system, the RMSd of the ligand and all residues surrounding it within 5 Å was in most cases between 1.1 and 1.6 Å, excluding hydrogens (examples in Supplementary Material Fig. S6). Due to the transmembrane nature of P-gp, a 50.0 kcal/Å2 harmonic restraint was kept for the backbone atoms. Electrostatic interactions were computed using the Particle Mesh Ewald (PME) method with a cutoff of 10 Å66. The SHAKE algorithm, as implemented in pmemd.cuda, was applied to constrain hydrogen-heavy atom bonds63. The force field used for the atoms of the protein was ff14SB67.The trajectory analyses were made with cpptraj63 and VMD 1.9.368, with the latter also used for graphics rendering.
The free energy calculations were made using the mmpbsa module of AMBER 18 by applying Poisson–Boltzman (PB) and Generalized Born (GB) models69. The energy analyses were made for the last 8–12 ns of simulation as the average over at least two independent trajectories. The frames were sampled once each 10–20 ps in order to keep the energy self-correlation negligible. A detailed analysis of the dynamics of the contacts was made for all simulated compounds by partitioning the energy contribution of each amino acid with the inhibitor from one representative run as shown for Rho123, vincristine, and compounds 6g, 6i, 6f, 3a, and 3d displayed in Fig. 11. For comparison purposes, the pattern obtained for compound 6 m (which slightly departs in its mode of binding from the subset of compounds that behave as compound 6i) is shown in the Supplementary Material Fig. S5, together with data previously obtained using the same modeling models for doxorubicin and tariquidar as other reference agents run as substrate and inhibitor, respectively33.
The average total number of H-bonds were in general between 0.5 and 1.5 during the equilibrated trajectories, with some examples shown as Supplementary Material Fig. S7. Chimera 1.1570 was used for clustering analyses, using the last 50 ns of each trajectory and for the graphics rendering of representative conformations thus obtained.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
Abbreviations
- CML:
-
Chronic myelogenous leukemia
- DCC:
-
N,N΄-dicyclohexylcarbodiimide
- DIPEA:
-
N,N΄-diisopropylehtylamine
- DMAP:
-
4-Dimethylaminopyridine
- Dox:
-
Doxorubicin
- FR:
-
Fold reversal
- HOBt:
-
1-Hydroxybenzotriazole
- MDR:
-
Multidrug resistance
- NBD:
-
Nucleotide binding domain
- Rho123:
-
Rhodamine 123
- TFE:
-
2,2,2-Trifluoroethanol
References
Kipps, T. J. & Choi, M. Y. Targeted therapy in chronic lymphocytic leukemia. Cancer J. (Sudbury Mass.) 25, 378 (2019).
Link, W. Principles of Cancer Treatment and Anticancer Drug Development (Springer, 2019).
Lee, Y. T., Tan, Y. J. & Oon, C. E. Molecular targeted therapy: Treating cancer with specificity. Eur. J. Pharmacol. 834, 188–196 (2018).
Engle, K. & Kumar, G. Cancer multidrug-resistance reversal by ABCB1 inhibition: A recent update. Eur. J. Med. Chem. 239, 114542 (2022).
Vaidya, F. U. et al. Molecular and cellular paradigms of multidrug resistance in cancer. Cancer Rep. 5, e1291 (2020).
Wang, J., Seebacher, N., Shi, H., Kan, Q. & Duan, Z. Novel strategies to prevent the development of multidrug resistance (MDR) in cancer. Oncotarget 8, 84559–84571 (2017).
Maia, R. C., Vasconcelos, F. C., Souza, P. S. & Rumjanek, V. M. Towards comprehension of the ABCB1/P-glycoprotein role in chronic myeloid leukemia. Molecules 23, 119 (2018).
Vasconcelos, F. C., de Souza, P. S., Hancio, T., de Faria, F. C. C. & Maia, R. C. Update on drug transporter proteins in acute myeloid leukemia: Pathological implication and clinical setting. Crit. Rev. Oncol. Hematol. 160, 103281 (2021).
Faderl, S. et al. The biology of chronic myeloid Leukemia. N. Engl. J. Med. 341, 164–172 (1999).
Gupta, S. K., Singh, P., Chhabra, R. & Verma, M. Novel pharmacological approach for the prevention of multidrug resistance (MDR) in a human leukemia cell line. Leuk. Res. 109, 106641 (2021).
Hochhaus, A. et al. Expert opinion—Management of chronic myeloid leukemia after resistance to second-generation tyrosine kinase inhibitors. Leukemia 34, 1495–1502 (2020).
Ma, X. et al. TRIB2 knockdown as a regulator of chemotherapy resistance and proliferation via the ERK/STAT3 signaling pathway in human chronic myelogenous leukemia K562/ADM cells. Oncol. Rep. 39, 1910–1918 (2018).
Zhou, X. et al. Let-7b regulates the adriamycin resistance of chronic myelogenous leukemia by targeting AURKB in K562/ADM cells. Leuk. Lymphoma 61, 3451–3459 (2020).
Gupta, S. K., Singh, P., Ali, V. & Verma, M. Role of membrane-embedded drug efflux ABC transporters in the cancer chemotherapy. Oncol. Rev. https://doi.org/10.4081/oncol.2020.448 (2020).
Ammar, M. et al. Overexpression of P-glycoprotein and resistance to Imatinib in chronic myeloid leukemia patients. J. Clin. Lab. Anal. 34, e23374 (2020).
Fan, J., To, K. K. W., Chen, Z.-S. & Fu, L. ABC transporters affects tumor immune microenvironment to regulate cancer immunotherapy and multidrug resistance. Drug Resist. Updat. 66, 100905 (2023).
Qiu, Z. et al. Development and application of a UPLC–MS/MS method for P-glycoprotein quantification in human tumor cells. J. Chromatogr. B 1084, 14–22 (2018).
Wang, J. Q. et al. ATP-binding cassette (ABC) transporters in cancer: A review of recent updates. J. Evid.-Based Med. 14, 232–256 (2021).
Szatmári, P. & Ducza, E. Changes in Expression and Function of Placental and Intestinal P-gp and BCRP Transporters during Pregnancy. Int. J. Mol. Sci. 24, 13089 (2023).
Sajid, A., Lusvarghi, S., Chufan, E. E. & Ambudkar, S. V. Evidence for the critical role of transmembrane helices 1 and 7 in substrate transport by human P-glycoprotein (ABCB1). PLoS ONE 13, e0204693 (2018).
Wang, L. & Sun, Y. Efflux mechanism and pathway of verapamil pumping by human P-glycoprotein. Arch. Biochem. Biophys. 696, 108675 (2020).
Clouser, A. F. & Atkins, W. M. Long range communication between the drug-binding sites and nucleotide binding domains of the efflux transporter ABCB1. Biochemistry (Mosc) 61, 730–740 (2022).
Zhang, H. et al. Chemical molecular-based approach to overcome multidrug resistance in cancer by targeting P-glycoprotein (P-gp). Med. Res. Rev. 41, 525–555 (2021).
Szakacs, G., Paterson, J. K., Ludwig, J. A., Booth-Genthe, C. & Gottesman, M. M. Targeting multidrug resistance in cancer. Nat. Rev. Drug Discov. 5, 219–234 (2006).
Palmeira, A., Sousa, E., Vasconcelos, H. & Pinto, M. Three decades of P-gp inhibitors: skimming through several generations and scaffolds. Curr. Med. Chem. 19, 1946–2025 (2012).
Yuan, S. et al. Discovery of new 4-indolyl quinazoline derivatives as highly potent and orally bioavailable P-glycoprotein inhibitors. J. Med. Chem. 64, 14895–14911 (2021).
Davison, E. K. & Brimble, M. A. Natural product derived privileged scaffolds in drug discovery. Curr. Opin. Chem. Biol. 52, 1–8 (2019).
Di Nardo, G. & Gilardi, G. Natural compounds as pharmaceuticals: the key role of cytochromes P450 reactivity. Trends Biochem. Sci. 45, 511–525 (2020).
Cardoso, D. S. P. et al. Alkylated monoterpene indole alkaloid derivatives as potent P-glycoprotein inhibitors in resistant cancer cells. Eur. J. Med. Chem. 210, 112985 (2020).
Huang, W. et al. Design, synthesis, and tumor drug resistance reversal activity of novel hederagenin derivatives modified by nitrogen-containing heterocycles. Eur. J. Med. Chem. 232, 114207 (2022).
González, M. L. et al. Mechanism underlying the reversal of drug resistance in P-glycoprotein-expressing leukemia cells by pinoresinol and the study of a derivative. Front. Pharmacol. https://doi.org/10.3389/fphar.2017.00205 (2017).
Laiolo, J. et al. Plant extracts and betulin from Ligaria cuneifolia inhibit P-glycoprotein function in leukemia cells. Food Chem. Toxicol. 147, 111922 (2021).
Laiolo, J. et al. Structure activity relationships and the binding mode of quinolinone-pyrimidine hybrids as reversal agents of multidrug resistance mediated by P-gp. Sci. Rep. 11, 1–18 (2021).
Qiu, Q. et al. Design, synthesis and biological evaluation of N-(4-(2-(6, 7-dimethoxy-3, 4-dihydroisoquinolin-2 (1H)-yl) ethyl) phenyl)-4-oxo-3, 4-dihydrophthalazine-1-carboxamide derivatives as novel P-glycoprotein inhibitors reversing multidrug resistance. Bioorg. Chem. 86, 166–175 (2019).
Yang, Z. et al. Design, synthesis and biological evaluation of novel phenylfuran-bisamide derivatives as P-glycoprotein inhibitors against multidrug resistance in MCF-7/ADR cell. Eur. J. Med. Chem. 248, 115092 (2023).
Li, Y.-S. et al. Design, synthesis and bioactivity study on 5-phenylfuran derivatives as potent reversal agents against P-glycoprotein-mediated multidrug resistance in MCF-7/ADR cell. Eur. J. Med. Chem. 216, 113336 (2021).
Zhang, N. et al. 4, 5-Di-substituted benzyl-imidazol-2-substituted amines as the structure template for the design and synthesis of reversal agents against P-gp-mediated multidrug resistance breast cancer cells. Eur. J. Med. Chem. 83, 74–83 (2014).
Wong, I. L. et al. Synthesis and evaluation of stereoisomers of methylated catechin and epigallocatechin derivatives on modulating P-glycoprotein-mediated multidrug resistance in cancers. Eur. J. Med. Chem. 226, 113795 (2021).
Yuan, J. et al. Synthesis of methylated quercetin derivatives and their reversal activities on P-gp- and BCRP-mediated multidrug resistance tumour cells. Eur. J. Med. Chem. 54, 413–422 (2012).
Ghosh, A. K. & Brindisi, M. Organic carbamates in drug design and medicinal chemistry. J. Med. Chem. 58, 2895–2940 (2015).
Kuete, V. et al. Cytotoxicity of four Aframomum species (A. arundinaceum, A. alboviolaceum, A. kayserianum and A. polyanthum) towards multi-factorial drug resistant cancer cell lines. BMC Complement Altern. Med. 14, 340 (2014).
Dei, S. et al. Design and synthesis of new potent N, N-bis(arylalkyl)piperazine derivatives as multidrug resistance (MDR) reversing agents. Eur. J. Med. Chem. 147, 7–20 (2018).
Lyon, P. C. et al. Quantifying cell death induced by doxorubicin, hyperthermia or HIFU ablation with flow cytometry. Sci. Rep. 11, 1–19 (2021).
Delou, J. M., Capella, M. A. M. & Gattass, C. R. Betulinic acid does not modulate the activity of P-gp/ABCB1 or MRP1/ABCC1 in a non-tumoral renal cell line: Possible utility in multidrug resistance cancer chemotherapy. Mol. Med. Rep. 2, 271–275 (2009).
Wang, L., Zhang, L., Liu, F. & Sun, Y. Molecular energetics of doxorubicin pumping by human P-glycoprotein. J. Chem. Inf. Model. 59, 3889–3898 (2019).
Dewanjee, S. et al. Natural products as alternative choices for P-glycoprotein (P-gp) inhibition. Molecules 22, 871 (2017).
Yoshida, N., Koizumi, M., Adachi, I. & Kawakami, J. Inhibition of P-glycoprotein-mediated transport by terpenoids contained in herbal medicines and natural products. Food Chem. Toxicol. 44, 2033–2039 (2006).
Ferreira, R. J. et al. Terpenoids from Euphorbia pedroi as multidrug-resistance reversers. J. Nat. Prod. 81, 2032–2040 (2018).
Song, X. et al. Aptamer functionalized upconversion nanotheranostic agent with nuclear targeting as the highly localized drug-delivery system of doxorubicin. Frontiers in Bioeng. Biotechnol. 9, 639487 (2021).
Kitzinger, R., Fritz, G. & Henninger, C. Nuclear RAC1 is a modulator of the doxorubicin-induced DNA damage response. Biochim. et Biophys. Acta (BBA) Mol. Cell Res. 1869, 119320 (2022).
Alam, A., Kowal, J., Broude, E., Roninson, I. & Locher, K. P. Structural insight into substrate and inhibitor discrimination by human P-glycoprotein. Science 363, 753 (2019).
Nosol, K. et al. Cryo-EM structures reveal distinct mechanisms of inhibition of the human multidrug transporter ABCB1. Proc. Natl. Acad. Sci. 117, 26245–26253 (2020).
Pediconi, N. et al. Design and synthesis of piperazine-based compounds conjugated to humanized ferritin as delivery system of siRNA in cancer cells. Bioconj. Chem. 32, 1105–1116 (2021).
Moreira, M. A. M. et al. Changes in gene expression profile in two multidrug resistant cell lines derived from a same drug sensitive cell line. Leuk. Res. 38, 983–987 (2014).
Mosmann, T. Use of MTT colorimetric assay to measure cell activation. J. Immunol. Methods 65, 55 (1983).
García Manzano, M. F., Joray, M. B., Laiolo, J., Palacios, S. M. & Carpinella, M. C. Cytotoxic activity of germacrane-type sesquiterpene lactones from Dimerostemma aspilioides. J. Nat. Prod. 83, 1909–1918 (2020).
Joray, M. B. et al. P53 tumor suppressor is required for efficient execution of the death program following treatment with a cytotoxic limonoid obtained from Melia azedarach. Food Chem. Toxicol. 109, 888–897 (2017).
Laiolo, J. et al. Analogues of the lignan pinoresinol as novel lead compounds for P-glycoprotein (P-gp) inhibitors. ACS Med. Chem. Lett. 9, 1186–1192 (2018).
Trott, O. & Olson, A. J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 31, 455–461 (2010).
Besler, B. H., Merz, K. M. Jr. & Kollman, P. A. Atomic charges derived from semiempirical methods. J. Comput. Chem. 11, 431–439 (1990).
Yanai, T., Tew, D. P. & Handy, N. C. A new hybrid exchange–correlation functional using the Coulomb-attenuating method (CAM-B3LYP). Chem. Phys. Lett. 393, 51–57 (2004).
Gaussian 16 Rev. C.01 (Wallingford, CT, 2016).
Case, D. et al. AMBER 2018 (University of California, 2018).
Wang, J., Wang, W., Kollman, P. A. & Case, D. A. Automatic atom type and bond type perception in molecular mechanical calculations. J. Mol. Graph. Model. 25, 247–260 (2006).
Andersen, H. C. Molecular dynamics simulations at constant pressure and/or temperature. J. Chem. Phys. 72, 2384–2393 (1980).
Essmann, U. et al. A smooth particle mesh Ewald method. J. Chem. Phys. 103, 8577–8593 (1995).
Maier, J. A. et al. ff14SB: Improving the accuracy of protein side chain and backbone parameters from ff99SB. J. Chem. Theory Comput. 11, 3696–3713 (2015).
Humphrey, W., Dalke, A. & Schulten, K. V. M. D. Visual molecular dynamics. J. Mol. Graph. 14, 33–38 (1996).
Genheden, S. & Ryde, U. The MM/PBSA and MM/GBSA methods to estimate ligand-binding affinities. Expert Opin. Drug Discov. 10, 449–461 (2015).
Pettersen, E. F. et al. UCSF chimera—A visualization system for exploratory research and analysis. J. Comput. Chem. 25, 1605–1612 (2004).
Acknowledgements
This work was supported by the Catholic University of Córdoba, CONICET (PIP- 2021-2023), FONCyT (PICT 2017-1381, PICT 2019-2019-00721, PICT-2020-SERIEA-01627, PICT-2021-CAT-II-00045) and Andreas Mentzelopoulos Foundation. We thank Joss Heywood for revising the English language. The authors would also like to acknowledge the networking contribution by the COST Action CA17104 “New diagnostic and therapeutic tools against multidrug resistant tumours”. J. L. and C.L.B. acknowledge receipt of a Scholarship from the National Research Council of Argentina (CONICET). M.B.J., D.M.A.V. and M.C.C. are staff members of CONICET. The cell lines were generous gifts from Dr. V. Rumjanek, Universidade Federal do Rio de Janeiro, Rio de Janeiro, Brazil, and Dr. H. Martinez is acknowledged for the maintenance of these. Finally, we would like to thank the Instrumental Analysis Laboratory (IAL, School of Natural Sciences, University of Patras) for recording the NMR spectra, the Unit of Environmental, Organic and Biochemical high-resolution analysis-Orbitrap-LC-MS of the University of Ioannina for providing access to their facilities, and Vasiliki Boti for performing the HRMS analyses.
Author information
Authors and Affiliations
Contributions
J.L. was responsible for cell culture and performed the biological assays as well as the statistical analysis, D.G.G. performed the synthesis of compounds, wrote the synthetic procedures and did the spectroscopic characterization, C.L.B conducted docking and MD studies, M.B.J. perfomed resistance reversal assays, A.I.A. performed HPLC analysis, drafted and revised the chemistry part of the supplementary information, D.M.A.V. performed docking and MD studies, drafted and revised the manuscript. C.M.A. conceived and designed the synthetic part of the study and wrote and supervised the synthesis of compounds and revised the manuscript, M.C.C. conceived and designed the study, analyzed the results, wrote the paper and was responsible for the granting. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laiolo, J., Graikioti, D.G., Barbieri, C.L. et al. Novel betulin derivatives as multidrug reversal agents targeting P-glycoprotein. Sci Rep 14, 70 (2024). https://doi.org/10.1038/s41598-023-49939-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-49939-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.