Abstract
Sleep variability (e.g. intra-individual variabilities in sleep duration or sleep timing, social jetlag, and catch-up sleep) is an important factor impacting health and mortality. However, limited information is available on the distribution of these sleep parameters across the human life span. We aimed to provide distribution of sleep variability related parameters across lifespan by sex and race in a national representative sample from the U.S. population. The study included 9981 participants 6 years and older from the National Health and Nutrition Examination Survey (NHANES) 2011–2014, who had 4–7 days of valid 24-h accelerometer recording with at least one day obtained during weekend (Friday or Saturday night). Of the study participants, 43% showed ≥ 60 min sleep duration standard deviation (SD), 51% experienced ≥ 60 min catch-up sleep, 20% showed ≥ 60 min sleep midpoint SD, and 43% experienced ≥ 60 min social jetlag. American youth and young adults averaged greater sleep variability compared to other age groups. Non-Hispanic Blacks showed greater sleep variability in all parameters compared to other racial groups. There was a main effect of sex on sleep midpoint SD and social jetlag with males averaging slightly more than females. Our study provides important observations on sleep variability parameters of residents of the United States by using objectively measured sleep patterns and will provide unique insights for personalized advice on sleep hygiene.
Similar content being viewed by others
Introduction
Adequate sleep is vital to overall human health and the importance of sufficient sleep duration is well-known1. However, recent research has begun to show that sleep variability, in terms of duration and timing, is also critical to optimal health2. Sleep variability encompasses the daily fluctuations in sleep behavior, offering a more comprehensive understanding of sleep patterns compared to a sole focus on the average value of sleep duration. Modern society commonly experiences considerable interference in sleep due to lifestyle demands which vary from day to day3. Furthermore, the constraints of school/work schedules and individual chronotypes drive differences in sleep patterns on weekdays compared to weekends when individuals typically try to “catch up on sleep”3. The difference of sleep timing on weekdays vs weekends is known as social jetlag. The variation of sleep duration and sleep timing from day to day can also be measured by the standard deviation of sleep duration (sleep duration SD) and the standard deviation of sleep midpoint (sleep midpoint SD). Inconsistency in sleep patterns has been linked to numerous negative health outcomes including cardiovascular disease, metabolic disruptions, immune system regulation, and many other adverse health conditions4,5,6,7. For example, large variability in sleep duration (> 1 h of sleep duration SD) has been associated with an increased risk of cardiovascular disease in older adults and suicidal ideation in young adults4,8. Previous studies have even indicated that irregular sleep patterns may be more strongly associated with cardiovascular disease than inadequate sleep duration itself9,10. The protective effects of catch-up sleep on health have also been found to be offset in individuals with habitual increased sleep variability11.
The variability of sleep patterns changes with age, and a nationally representative sample is required to estimate these changes across the lifespan unbiasedly, including possible modifying demographic factors such as sex and race. A recent nationally representative cross-sectional analysis which assessed the prevalence of social jetlag among US adults using self-report questionnaire data found that almost half averaged at least 1 h of social jetlag12, indicating the high prevalence of sleep irregularity in US adults. While limited by variations in methodologies, a recent systematic review comprising 53 studies involving participants aged 18 and above assessed the extent to which daily intraindividual variability (IIV) in sleep timing, duration, and quality were associated with non-sleep related factors13. From an analysis of data extracted from 15 of these studies, it was discerned that older age was linked to reduced variability in sleep timing, while minority race was associated with increased sleep duration variability13. However, the evaluation of the relationship between sex and sleep/wake IIV yielded inconclusive results, likely due to constraints posed by a limited sample size13. Like this study, most existing research on sleep variability primarily involves adults, with limited attention given to children and adolescents. However, it is important to recognize that sleep variability may have significant implications in childhood development. A recent international systematic review explored six different sleep IIV parameters, including duration IIV and onset IIV, in children and adolescents14. This review identified a consistent trend such that as age increased, there was an increase in sleep duration IIV and onset/waking IIV. This pattern perhaps suggests that adolescence may be a critical period in which sleep variability exerts a notable impact.
Moreover, within this study inconsistent associations were seen between sleep variability in childhood and adolescence and various health conditions such as obesity and neurodevelopmental disorders, emphasizing the need for more standardized and consistent data measurements in future research endeavors. It is also worth noting that none of the studies included directly compared sleep IIV across different age groups which underscores the importance of further literature to investigate sleep variability across differing age groups.
All in all, national survey data on objective measurements of sleep variability is limited. More recently, increasing the usage of rest activity data provided by research-grade activity monitors (i.e. accelerometers) in population studies allows for more objective estimates of sleep parameters that can be used to measure multiple parameters of sleep variability. In the current study, using nationally representative accelerometer data from the National Health and Nutrition Examination Survey (NHANES) from 2011 to 2014, we aimed to evaluate the distribution of sleep variability across the lifespan using objectively obtained multiple sleep variability parameters in 9981 participants aged 6 years and older.
Method
Study population
This study used data from the NHANES survey. The survey is the collection of health examination data for a weighted nationally representative sample of the U.S. population through a multistage probability sampling design15. The survey consists of questionnaires administered at the participants home followed by a health examination in a mobile examination center15. Participants receive compensation and a report of their medical findings15. The NHANES surveys from the 2011–2012 and 2013–2014 were used. These cycles were selected due to their availability of 24 h accelerometer data. The National Center for Health Statistics Research Ethics Review Board approved all NHANES protocols, and written informed consent was obtained from all participants or their parents or guardians. All methods were performed in accordance with the relevant guidelines and regulations. Our analytic sample (n = 9981) was selected from participants with age ≥ 6 years old (n = 16,733) that had (1) 4–7 days of valid 24-h accelerometer recording with at least one day obtained during weekend (Friday or Saturday night) (n = 10,153), and (2) all sleep variability parameters < 5 (n = 9981). NHANES does not specify participant’s age after 80 years old for participant privacy, so all participants over 80 were coded as 80 years old. Figure 1 illustrates the flow chart for participants selected for inclusion within the analysis. In comparison with the final sample (n = 9981), the excluded participants (n = 6752) were younger and less likely to be female or Non-Hispanic (NH) Whites (Supplementary Table S1). Also in comparison with the final sample, the excluded participants due to extreme sleep variability parameters (n = 172) were also likely to be NH Whites (Supplementary Table S1).
Sleep parameters
Sleep parameters were derived from accelerometer data. Accelerometer recordings and data preprocessing were documented previously16 and summarized in the Supplementary document. The calculation of sleep onset time, wakeup time, and sleep duration from the accelerometer data has also been described previously. Briefly, a Hidden Markov Model (HMM)-based unsupervised sleep–wake identification algorithm was used to infer the sequence of “hidden states” of sleep or wake for each individual17. The block of the longest sleep period in the day (noon-noon) was identified as the sleep period time (SPT) window. The start of the SPT window was defined as the sleep onset time and the end of the SPT window was defined as the wakeup time. Wake/activity bouts were identified during the SPT window. Sleep duration was defined using the following equation: sleep duration = the SPT window duration –the summed duration of all wake bouts. The sleep midpoint was assessed by the sleep onset time and wakeup time. The variability parameters for sleep duration included the standard deviation of sleep duration (sleep duration SD) and catch-up sleep (the absolute value of the difference in sleep duration between the average of weekdays and the average of weekends). The variability parameters for timing of sleep included the standard deviation of the sleep midpoint (sleep midpoint SD) and social jetlag (the absolute value of the difference in sleep midpoint between the average of weekdays and the average of weekends).
Age, sex, and race
The NHANES demographic file was used to obtain age, sex, and race information. Participants were divided into 10 different age groups (i.e. 6–9, 10–13, 14–17, 18–25, 26–35, 36–45, 46–55, 56–65, 66–75, and ≥ 75 years) for the description of the distributions of sleep variability parameters. Race was divided into 4 classifications: Non-Hispanic (NH) White, NH Black, Mexican American, and other race (i.e. other Hispanic, Asian and other ethnicity).
Statistical analysis
Analyses were completed using the survey data analysis in STATA (v16) to generate representative estimates of the US population and account for complex survey design. Four-year survey weights were calculated and used in all analyses to adjust for unequal selection probability and non-response bias in accordance with NHANES analytical guidelines18. Population means, proportions, and standard deviation (SD) were estimated and reported. Survey weighted linear regression was used to assess the distribution of sleep variability parameters across age, sex and race. Due to the nonlinear relationship between age and sleep variability parameters, linear, quadratic, cubic and quartic trends were fitted by including age, age2, age3 and age4 in the regression model to understand the changes of sleep variability parameters with age. The interactions between sex and age (i.e. linear, quadratic, cubic and quartic) or between race and age were also tested to examine whether the associations of sleep variability parameters with age were modified by sex or race. Statistical significance was set at p < 0.05.
We performed a sensitive analyses by repeating the analyses in the participants with at least 6 days accelerometer data (86.3% of the participants) to exclude the potential bias from the inclusion of a small percentage of the participants with a relatively short period of accelerometer recording.
Results
The complete dataset consisted of 19,931 participants with 16,733 aged ≥ 6 years. A total of 6752 participants were further excluded from analysis based on exclusion criteria (Fig. 1). Our final sample size included 9981 participants aged ≥ 6 years (mean ± SD: 41.9 ± 21.5 years), representing 178.8 million noninstitutionalized residents of the United States. The general characteristics of age, sex, race, and sleep variability parameters of participants are presented in Table 1.
Correlations among these sleep variability parameters are listed in Supplementary Table S2. As expected, strong correlations were observed between the two parameters for day-to-day deviations in sleep duration (r = 0.52 between sleep duration SD and catch-up sleep) as well as between the two parameters for day-to-day deviations in sleep timing (r = 0.64 between sleep midpoint SD and social jetlag).
The distributions of sleep duration SD, catch-up sleep, sleep midpoint SD and social jetlag by age groups are presented in Supplementary Table S3 and Table S4. The medians ranged from 42 to 67 min for sleep duration SD, 49–82 min for catch-up sleep, 31–47 min for sleep midpoint SD and 32–86 min for social jetlag across the age groups, with the peak values shown either in the age group of 14–17 or the age group of 18–25. In the overall sample, 43% of US school-aged children and adults showed ≥ 60 min sleep duration SD, 51% experienced ≥ 60 min catch-up sleep, 20% showed ≥ 60 min sleep midpoint SD, and 43% experienced ≥ 60 min social jetlag. The prevalence of sleep irregularity defined by the cutoff of 60 min, 90 min and 120 min by these 4 sleep variability parameters by age groups are presented in Tables 2 and 3.
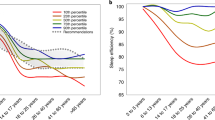
Figure 2 displays the changes in the sleep duration SD and catch-up sleep with age and possible effect modifiers of sex and race. Sleep duration SD increased until its first peak around age 20 then gradually declined until around age 50. After age 50, it showed a small increase again until around 70 to where it declined once more (Fig. 2A-1). There was no overall main effect of sex on sleep duration SD but there was a significant interaction between sex and age2. As shown in Fig. 2A-2, the decline in sleep duration SD from around age 20 to age 40 was larger in females. Furthermore, there was a significant main effect of race (p < 0.001) as NH Blacks had the highest median sleep duration SD of 64 min compared to 53 min (p < 0.001), 55 min (p < 0.001), and 55 min (p < 0.001) for NH Whites, Mexican Americans, and other races respectively (Fig. 2A-3). There were no significant interactions between race and age observed for sleep duration SD.
Catch-up sleep followed a similar pattern as sleep duration SD as it increased till around age 20 then gradually declined throughout with a small plateau between ages 50 and 70 (Fig. 2B-1). There was no overall main effect of sex on catch-up sleep and there were no significant interactions between sex and age observed (Fig. 2B-2). However, there was a significant main effect of race (p < 0.001). NH Blacks had the highest median catch-up sleep of 73 min compared to 58 min (p < 0.001), 66 min (p = 0.062), and 65 min (p = 0.019) for NH Whites, Mexican Americans, and other races respectively (Fig. 2B-3). In addition, the difference between Mexican American and NH Whites in catch-up sleep also reached significance (p = 0.013). There were no significant interactions between race and age observed for catch-up sleep.
Figure 3 displays the changes in the sleep midpoint SD and social jetlag with age and possible effect modifiers of sex and race. As shown in Fig. 3A-1, sleep midpoint SD increased with age until its peak around age 20. After age 20, sleep midpoint SD gradually declined until around age 50 where it leveled off until around age 70 before declining once again. There was a significant main effect of sex (p = 0.011) with males averaging 2 more minutes of midpoint of sleep SD compared to females (Fig. 3A-2). There was also a significant main effect of race (p < 0.001) observed with NH Blacks averaging 9 more minutes of midpoint of sleep SD compared to NH Whites (p < 0.001) and 5 more minutes compared to Mexican Americans (p < 0.001) and other races (p < 0.001) (Fig. 3A-3). There were no significant interactions between race and age observed.
As shown in Fig. 3B-1, social jetlag is present in early ages beginning almost at an average of one hour around age 6 and gradually increasing until around age 20. After around age 20, social jet lag steadily declines with age. There was a main effect of sex (p = 0.006) with males averaging 5 more minutes than females (Fig. 3B-2). There were no interactions between sex and age found. However, there also was a main effect of race (p = 0.001) which was driven by the significant difference (p < 0.001) between NH Blacks and NH Whites with NH Blacks averaging 12 more minutes of social jet lag compared to NH Whites (Fig. 3B-3). Mexican Americans and other races had higher values than NH Whites and lower values than NH Blacks in social jetlag, and the differences were significant in the comparisons with NH Blacks (p = 0.039 for Mexican Americans and p = 0.018 for other races). There were no interactions observed between race and age.
In the sensitivity analyses of excluding participants with short duration of accelerometer recording, the results remained the same (Supplementary Table S5, Table S6, Figure S1 and Figure S2).
Discussion
Within our study, we used actigraphy data to provide objective estimates of multiple sleep variability parameters: sleep duration SD, catch-up sleep, sleep midpoint SD, and social jetlag. Our study is the first to show the distribution of these parameters in a nationally representative sample of the United States. We explored the differences in these parameters of sleep variability across the life span as well as the potential modifying effects of sex and race. We found that American youth and young adults as well as NH Blacks had the largest variability across all sleep variability parameters compared to the other age groups or the other racial groups. The high rates of sleep variability in youth and young adults is especially concerning given its relationship with suicidal ideation and the observation that suicide death is the second leading cause of death among youth in the US19.
American young adults aged 18–25 had the highest sleep duration SD averaging 70 min which is consistent with a recent study on eight-pooled datasets which found that the 18–24 age group had the highest sleep duration SD averaging 77 min in the datasets using accelerometer recording20. Additionally, children aged 6–9 and 10–13 had lower rates of sleep duration SD when compared to post-pubertal adolescents (ages 14–17). Research from a 2011 review paper delved into the intricate connection between bioregulatory mechanisms and psychosocial factors on worsened sleep patterns in teenagers21. The findings of this work suggested that maturation leads to a delayed shift in adolescents’ circadian rhythms in addition to increased evening alertness21,22. Additionally, children growing older is associated with less strict parent-set bedtimes, increased screen time, and greater academic demands22. Unfortunately, this shift towards later bedtimes is often not matched with later wake times, as school start times remain relatively early. The interplay between all of these factors could underlie increasing sleep duration SD through adolescent maturation. Substance usage like caffeine, alcohol, and marijuana might also play a role, particularly in young adults. Although limited, studies on sleep schedule regularity and academic performance in adolescents and young adults indicate that a higher index of sleep regularity is associated with better academic performance23,24. Notably, students with failing grades reported greater differences between weekend and weekday sleep schedules23. This emphasizes the importance of further research on sleep variability in children and young adults.
Sleep duration SD showed a bimodal distribution with peaks around ages 20 and 70. This distribution held true when accounting for the impact of sex and race. Aging is associated with increased prevalence of multiple components which impact sleep such as multimorbidity, polypharmacy, psychosocial factors and many primary sleep disorders. All of which could contribute to increasing sleep duration SD after age 5025. The average age of retirement in 2013 was around 63 years old which also factors in as adults may taper off working hours leading into official retirement26.
The Multi-Ethnic Study of Atherosclerosis (MESA) in 1922 participants aged 45–84 found that almost 40% participants had > 90 min of sleep duration SD and these participants had higher averages of BMI, blood pressure, and diabetes prevalence compared to those with < 90 min of sleep duration SD4. After adjusting for cardiovascular disease risk factors, this study also found that every 1 h increase in sleep duration SD was associated with a 36% higher rate of cardiovascular risk4. Of the 4125 participants over the age of 45 within the current study only 14% had > 90 min of sleep duration SD. In addition to our study being conducted in a national representative sample, another potential reason for this difference could be that the previous study had different racial demographics. Of the participants of MESA 28% were African American compared to our study which had 11% NH Black participants. As shown in our study and prior research, NH Black Americans have greater amounts of sleep variability compared to other racial categories. Regardless, these findings illustrate the important impact of increasing sleep duration SD on the health of the geriatric population and emphases the need for ensuring public health education targeting on this topic. In addition, most research on the negative health impacts of sleep variability focus on older adults; however, our finding that 16% of participants aged 6–9 and 32% of participants aged 10–13 had 59 min of sleep duration SD highlights that variability in sleep pattern begins early in childhood. This warrants longitudinal studies to understand the impact of chronic sleep variability in childhood on different health parameters in later life.
In addition, our study examined the distribution of catch-up sleep across the lifespan. We found that 25% of participants aged 14–17 had greater than 2 h of catch-up sleep which aligned with a previous study that reported 25.5% of adolescents in their study had > 120 min of catch-up sleep27. Prior literature has demonstrated that amounts of weekend catch-up sleep greater than 2 h may be associated with mood and behavior disorders in adolescents28. Additional research is needed to understand the impact of different amounts of catch-up sleep on health through the lifespan.
Many factors like work and school schedules cause individuals to wake and sleep earlier during weekdays compared to weekends. This discrepancy is referred as social jetlag. We explored the distribution of social jetlag across all age groups. We found that social jetlag peaked around age 20 but all ages had varying amounts of social jetlag even young children. There is limited data on the quantity of social jetlag in various age groups; however, there have been studies which assessed total social jetlag in adolescents and in adults. A previous study used questionnaires to quantify social jetlag in non-shift workers aged 18–78 and found that almost 30% of participants had 1 to 2 h of social jetlag29. In our study, the average social jetlag for participants aged 18–78 was 64 min with 26% experiencing ≥ 1.5 h social jetlag. In addition, a study of undergraduate students which used actigraphy estimated that students averaged about 40 min of social jetlag30. This is lower than our finding of an average of 1 h 12 min of social jetlag in the age group of 18–25 in our study. This discrepancy could be related to the small sample size (n = 84) of the earlier study and all the participants being university students. A recent study found that greater social jetlag was associated with lower semester GPAs in older adolescents further emphasizing the link between sleep variability and academic performance in youth31. Moreover, our investigation into sleep variability trends within a large United States cohort exhibits alignment with analogous cross-sectional studies in other countries. A study of Australian children (n = 4032) between 9 and 18 years old delineated that older age groups had more pronounced differences in sleep–wake patterns on weekdays to weekends32. This result was supported by a study in Germany exhibiting lower levels of social jetlag in younger children aged 5 to 7 when compared to older children aged 8–2033. Further research should be conducted to explore how sleep variability trends in the United States relate to other countries as cultural differences likely influence sleep patterns, especially in children and youth34,35. These cultural differences could include meal times, family routines, or duration of daily schooling. For example, youth in Croatia attend school in the afternoon to accommodate work schedules36. Differing societal stressors including political or economic turmoil could also alter sleep patterns and should be considered.
Similar to the findings from the study on the eight-pooled datasets, we did not find a consistent difference between males and females in sleep variability parameters20. Sleep duration SD and catch-up sleep did not show significant differences between male and female; however, there was a significant main effect of sex on sleep midpoint SD and social jetlag as males averaged greater amounts of each compared to females.
Current literature is growing on sleep through a social-environmental perspective. Multiple studies have indicated that race, as a social category, impacts sleep quality and quantity across the lifespan implicating race as a critical factor in current sleep disparities37,38,39. Many of these studies focused on comparisons between NH Black Americans and NH White Americans. However, as a nationally representative US sample, our study consisted of 65% NH White Americans, 11% NH Black Americans, 10% Mexican Americans and 14% of others. This allowed for reporting of sleep variability characteristics in Mexican Americans which is rarely cited in current research. We observed that Mexican Americans had significantly lower amounts of sleep duration SD, sleep midpoint SD and social jetlag compared to NH Blacks. Mexican Americans also had significantly higher amounts of catch-up sleep compared to NH Whites. In line with previous reports, NH Black Americans had worse sleep variability compared to all other racial groups. These findings align with a previous study which found that NH White youth had more sufficient sleep compared to NH Black youth38. A multitude of factors may underlie the reasoning for these results. For instance, shift work tends to have variable shifts which could impact sleep variability, and people from minority racial group disproportionately hold shift work positions39. In addition, minority racial groups undergo an increased amount of daily stressors comparatively which is a potential underlying factor as stress is known to disrupt sleep patterns39. Moreover, a recent actigraphy study explored the relationship between racial disparities in sleep characteristics and hypertension prevalence and concluded that sleep maintenance mediated over 11% of the difference in hypertension prevalence between NH Blacks and NH Whites within their sample40. These findings highlight the significance for multifaceted approaches that include racial disparity when studying the impacts of sleep on health outcomes.
There are some limitations to this study. First, although accelerometer recordings provide objective measurements of sleep parameters, this method cannot detect a difference between lying still while awake or being asleep. Second, occupation status was not obtained from participants in the NHANES 2011–2014 cycle, therefore, exclusion criteria for certain occupations like shift workers could not be performed. Third, the accelerometer data were obtained during the period of 2011–2014 and these accelerometer-data based sleep parameters might not represent the sleep measurements of the current US population. More recent accelerometer data from national surveys are warranted. Forth, calculating parameters of sleep variability usually requires a weeklong accelerometer recording41. Although 7-day accelerometer data were available for the NHANES 2011–2014 cycle data, after preprocessing and quality control, we kept the participants with at least 4 days (with at least one day recorded during the weekend) of high-quality accelerometer data to maximize the sample size. In the sensitive analyses, we repeated the analyses in these participants with at least 6 days high-quality accelerometer data and observed the same results, indicating that the small percentage of the participants with a relatively short period of qualified accelerometer recording does not affect the findings of this study. On the other hand, the study by Fischer et al.41 also showed that sleep regularity index (SRI) displayed the least dependence on the length of the availability of accelerometer recordings. SRI measures the similarity of an individual’s sleep–wake patterns from one day to the next, based on binary sleep–wake state classifications. It calculates the percentage probability of an individual being in the same state (sleep vs. wake) at any two time points 24-h apart, averaged across the study. The SRI is scaled to range from 0 (random) to 100 (perfectly regular). We repeated the analysis using SRI as an index of sleep regularity (Supplementary Figure S3) and observed the similar findings as the other sleep variability parameters with males and NH Black participants having lower SRI than females and NH White participants and the lowest SRI displaying at age 18–25. This further supported that our findings were not biased by the inclusion of participants with relatively short duration of accelerometer recordings. However, future studies with longer recording periods are still recommended, especially for catch-up sleep and social jetlag for which 14 days of accelerometer recording capturing 2 weekends will be able to provide more reliable findings. Fifth, the minute summary count of accelerometer data was used for the detection of the sleep period time window (i.e. the block of the longest sleep period in the day [noon–noon]), therefore the napping period was not captured. Further studies are warranted to explore how napping impacts sleep variability parameters. Another limitation arises from the inability to account for environmental factors that may alter sleep habits, particularly when minority populations are often more susceptible to these external determinants potentially worsening their sleep outcomes. Finally, as the findings are based on a cross-sectional analysis, temporal comparisons are limited.
In conclusion, for the first time our study provides the distribution of multiple objectively measured sleep variability parameters over lifespan by sex and race in a US nationally representative sample. This study not only provided solid evidence on the high prevalence of irregular sleep patterns in the US population, but also indicated that irregular sleep begins in childhood and shows racial disparity. These findings provide understanding of sleep patterns for residents of the United States as well as emphasize the importance in future research on the social determinants of sleep from multiple aspects. Sleep variability is likely a modifiable risk factor for a variety of health conditions. This information can also further research and public health agendas on sleep hygiene.
Data availability
All data are publicly and freely available from the US Centers for Disease Control and Prevention’s National Center for Health Statistics and can be accessed at https://www.cdc.gov/nchs/nhanes/index.htm.
References
St-Onge, M. P. et al. Sleep duration and quality: Impact on lifestyle behaviors and cardiometabolic health: A scientific statement from the american heart association. Circulation 134, e367–e386. https://doi.org/10.1161/CIR.0000000000000444 (2016).
Chaput, J. P. et al. Sleep duration and health in adults: An overview of systematic reviews. Appl. Physiol. Nutr. Metab. 45, S218–S231. https://doi.org/10.1139/apnm-2020-0034 (2020).
Wittmann, M., Dinich, J., Merrow, M. & Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 23, 497–509. https://doi.org/10.1080/07420520500545979 (2006).
Huang, T., Mariani, S. & Redline, S. Sleep irregularity and risk of cardiovascular events: The multi-ethnic study of atherosclerosis. J. Am. Coll. Cardiol. 75, 991–999. https://doi.org/10.1016/j.jacc.2019.12.054 (2020).
LeMay-Russell, S. et al. Longitudinal associations between facets of sleep and adiposity in youth. Obesity (Silver Spring) 29, 1760–1769. https://doi.org/10.1002/oby.23281 (2021).
Culver, M. N. et al. Sleep duration irregularity is associated with elevated blood pressure in young adults. Chronobiol. Int. 39, 1320–1328. https://doi.org/10.1080/07420528.2022.2101373 (2022).
Rutters, F. et al. The association between sleep duration, insulin sensitivity, and beta-cell function: The EGIR-RISC study. J. Clin. Endocrinol. Metab. 101, 3272–3280. https://doi.org/10.1210/jc.2016-1045 (2016).
Bernert, R. A., Hom, M. A., Iwata, N. G. & Joiner, T. E. Objectively assessed sleep variability as an acute warning sign of suicidal ideation in a longitudinal evaluation of young adults at high suicide risk. J. Clin. Psychiatry 78, e678–e687. https://doi.org/10.4088/JCP.16m11193 (2017).
Brouwer, A. et al. Sleep and HbA(1c) in patients with type 2 diabetes: Which sleep characteristics matter most?. Diabetes Care 43, 235–243. https://doi.org/10.2337/dc19-0550 (2020).
Hoopes, E. K. et al. Sleep duration regularity, but not sleep duration, is associated with microvascular function in college students. Sleep https://doi.org/10.1093/sleep/zsaa175 (2021).
Park, S. et al. Effect of weekend catch-up sleep on high-sensitivity C-reactive protein levels according to bedtime inconsistency: A population-based cross-sectional study. Sci. Rep. 12, 21619. https://doi.org/10.1038/s41598-022-25787-x (2022).
Di Hongkun, M., Guo, Y. & Daghlas, I. Evaluation of sleep habits and disturbances among US adults, 2017–2020. JAMA Netw. Open 5, 11 (2022).
Bei, B., Wiley, J. F., Trinder, J. & Manber, R. Beyond the mean: A systematic review on the correlates of daily intraindividual variability of sleep/wake patterns. Sleep Med. Rev. 28, 108–124. https://doi.org/10.1016/j.smrv.2015.06.003 (2016).
Becker, S. P., Sidol, C. A., Van Dyk, T. R., Epstein, J. N. & Beebe, D. W. Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: A systematic review. Sleep Med. Rev. 34, 94–121. https://doi.org/10.1016/j.smrv.2016.07.004 (2017).
Johnson, C. L., Dohrmann, S. M., Burt, V. L. & Mohadjer, L. K. National health and nutrition examination survey: Sample design, 2011–2014. Vital. Health Stat. 2, 1–33 (2014).
Su, S., Li, X., Xu, Y., McCall, W. V. & Wang, X. Epidemiology of accelerometer-based sleep parameters in US school-aged children and adults: NHANES 2011–2014. Sci. Rep. 12, 7680. https://doi.org/10.1038/s41598-022-11848-8 (2022).
Li, X., Zhang, Y., Jiang, F. & Zhao, H. A novel machine learning unsupervised algorithm for sleep/wake identification using actigraphy. Chronobiol. Int. 37, 1002–1015. https://doi.org/10.1080/07420528.2020.1754848 (2020).
(U.S.), N. C. f. H. S. National Health and Nutrition Examination Survey. Estimation Procedures, 2011–2014; Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, <https://www.cdc.gov/nchs/nhanes/index.htm> (2018).
Heron, M. Deaths: Leading causes for 2019. Natl. Vital .Stat. Rep. 70, 1–114 (2021).
Messman, B. A. et al. How much does sleep vary from night-to-night? A quantitative summary of intraindividual variability in sleep by age, gender, and racial/ethnic identity across eight-pooled datasets. J. Sleep Res. 31, e13680. https://doi.org/10.1111/jsr.13680 (2022).
Carskadon, M. A. Sleep in adolescents: The perfect storm. Pediatr. Clin. N. Am. 58, 637–647. https://doi.org/10.1016/j.pcl.2011.03.003 (2011).
Crowley, S. J., Wolfson, A. R., Tarokh, L. & Carskadon, M. A. An update on adolescent sleep: New evidence informing the perfect storm model. J. Adolesc. 67, 55–65. https://doi.org/10.1016/j.adolescence.2018.06.001 (2018).
Wolfson, A. R. & Carskadon, M. A. Understanding adolescents’ sleep patterns and school performance: A critical appraisal. Sleep Med. Rev. 7, 491–506. https://doi.org/10.1016/s1087-0792(03)90003-7 (2003).
Phillips, A. J. K. et al. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci. Rep. 7, 3216. https://doi.org/10.1038/s41598-017-03171-4 (2017).
Miner, B. & Kryger, M. H. Sleep in the aging population. Sleep Med. Clin. 15, 311–318. https://doi.org/10.1016/j.jsmc.2020.02.016 (2020).
Lytle, M. C., Clancy, M. E., Foley, P. F. & Cotter, E. W. Current trends in retirement: Implications for career counseling and vocational psychology. J. Career Dev. 42, 170–184. https://doi.org/10.1177/0894845314545785 (2015).
Tonetti, L. et al. Different effects of social jetlag and weekend catch-up sleep on well-being of adolescents according to the actual sleep duration. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph20010574 (2022).
Zhang, J. et al. Sleep patterns and mental health correlates in US adolescents. J. Pediatr. 182, 137–143. https://doi.org/10.1016/j.jpeds.2016.11.007 (2017).
Islam, Z. et al. Social jetlag is associated with an increased likelihood of having depressive symptoms among the Japanese working population: The Furukawa Nutrition and Health Study. Sleep https://doi.org/10.1093/sleep/zsz204 (2020).
Yoshizaki, T. & Togo, F. Objectively measured chronotype and social jetlag are associated with habitual dietary intake in undergraduate students. Nutr. Res. 90, 36–45. https://doi.org/10.1016/j.nutres.2021.04.003 (2021).
Smarr, B. L. & Schirmer, A. E. 3.4 million real-world learning management system logins reveal the majority of students experience social jet lag correlated with decreased performance. Sci. Rep. 8, 4793. https://doi.org/10.1038/s41598-018-23044-8 (2018).
Olds, T., Maher, C., Blunden, S. & Matricciani, L. Normative data on the sleep habits of Australian children and adolescents. Sleep 33, 1381–1388. https://doi.org/10.1093/sleep/33.10.1381 (2010).
Randler, C., Vollmer, C., Kalb, N. & Itzek-Greulich, H. Breakpoints of time in bed, midpoint of sleep, and social jetlag from infancy to early adulthood. Sleep Med. 57, 80–86. https://doi.org/10.1016/j.sleep.2019.01.023 (2019).
Milan, S., Snow, S. & Belay, S. The context of preschool children’s sleep: Racial/ethnic differences in sleep locations, routines, and concerns. J. Fam. Psychol. 21, 20–28. https://doi.org/10.1037/0893-3200.21.1.20 (2007).
Patrick, K. E., Millet, G. & Mindell, J. A. Sleep differences by race in preschool children: The roles of parenting behaviors and socioeconomic status. Behav. Sleep Med. 14, 467–479. https://doi.org/10.1080/15402002.2015.1017101 (2016).
Koscec, A., Radosevic-Vidacek, B. & Bakotic, M. Morningness-eveningness and sleep patterns of adolescents attending school in two rotating shifts. Chronobiol. Int. 31, 52–63. https://doi.org/10.3109/07420528.2013.821128 (2014).
Smith, J. P., Hardy, S. T., Hale, L. E. & Gazmararian, J. A. Racial disparities and sleep among preschool aged children: A systematic review. Sleep Health 5, 49–57. https://doi.org/10.1016/j.sleh.2018.09.010 (2019).
Guglielmo, D., Gazmararian, J. A., Chung, J., Rogers, A. E. & Hale, L. Racial/ethnic sleep disparities in US school-aged children and adolescents: A review of the literature. Sleep Health 4, 68–80. https://doi.org/10.1016/j.sleh.2017.09.005 (2018).
Grandner, M. A., Williams, N. J., Knutson, K. L., Roberts, D. & Jean-Louis, G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 18, 7–18. https://doi.org/10.1016/j.sleep.2015.01.020 (2016).
Rasmussen-Torvik, L. J. et al. The mediation of racial differences in hypertension by sleep characteristics: Chicago area sleep study. Am. J. Hypertens. 29, 1353–1357. https://doi.org/10.1093/ajh/hpw093 (2016).
Fischer, D., Klerman, E. B. & Phillips, A. J. K. Measuring sleep regularity: Theoretical properties and practical usage of existing metrics. Sleep https://doi.org/10.1093/sleep/zsab103 (2021).
Acknowledgements
X. W. receives funding from NIH DK117365 and AHA SFRN863620 and S. S. receives funds from NIH HL143440 and MD013307.
Author information
Authors and Affiliations
Contributions
E.P. conducted the analysis and drafted the manuscript; X.L. conducted the analysis and critically revised the manuscript; X.Y. conducted the analysis and critically revised the manuscript; W.M. and A.M. critically revised the manuscript; S.S. designed the original study and critically revised the manuscript; and X.W. designed the study, participated in the draft of the manuscript and made critical revisions of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Price, E., Li, X., Xu, Y. et al. Age, sex and race distribution of accelerometer-derived sleep variability in US school-aged children and adults. Sci Rep 13, 22114 (2023). https://doi.org/10.1038/s41598-023-49484-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-49484-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.