Abstract
Donor against recipient one-way Human leukocyte antigen (HLA) mismatch (D → R one-way HLA MM) seemed strongly associated with graft-versus-host disease (GVHD). The aim of this study is to investigate the relevance of D → R one-way HLA MM in outcome of liver transplantation (LT). We retrospectively analyzed 2670 patients in Korean Organ Transplantation Registry database between April 2014 and December 2020. The patients were categorized into two groups whether D → R one-way HLA MM or not and evaluated the outcomes of LT between the two groups. 18 patients were found to be D → R one-way HLA MM. The incidence of GVHD (0.3% vs. 22.2%, p < 0.001) and mortality rate (11.6% vs. 38.9%, p = 0.003) was much higher in D → R one-way HLA MM group. D → R one-way HLA MM at 3 loci was seemed to be strongly associated with the incidence of GVHD (OR 163.3, p < 0.001), and found to be the strongest risk factor for patient death (HR 12.75, p < 0.001). Patients with D → R one-way HLA MM at 3 loci showed significantly lower overall survival (p < 0.001) but there were no significant differences in rejection-free survival and death-censored graft survival. D → R one-way HLA MM at 3 loci not only affects the overall survival of LT patients but also the incidence of GVHD.
Similar content being viewed by others
Introduction
Human leukocyte antigen (HLA) compatibility between donor and recipient is closely related to the clinical outcomes of most solid organ transplantation. However, unlike other solid organ transplantation, the influence of HLA compatibility in liver transplantation (LT) remains unclear1. It is obvious that higher HLA compatibility may decrease the probability of acute or chronic rejection after LT but some previous studies demonstrated “dualistic effect” of HLA compatibility on LT which can lead to adverse effect2,3. Therefore, nowadays, matching HLA type of donor and recipient is not routinely required before LT.
Graft-versus-host disease (GVHD) rarely occurs after LT, with an incidence rate of 0.1–2.0%4,5. However, it can result in devastating outcome, since the mortality rate of GVHD after LT has been reported to be up to 85%6,7. It is known that GVHD is caused by immunocompetent donor lymphocytes, which recognize the recipient’s antigen and amplify the immune response after transplantation7. Because of its low incidence rate and nonspecific symptoms, effective diagnostic tools or treatment options for GVHD have not yet been clearly established. To date, known risk factors for GVHD include recipient and donor age, glucose intolerance, LT for hepatocellular carcinoma and HLA compatibility8. Several studies suggested that donor against recipient one-way HLA mismatch (D → R one-way HLA MM) may highly increase the incidence of GVHD after living donor LT but could not give enough evidence due to the small case number of GVHD.
In this study, we investigate the relevance of D → R one-way HLA MM to GVHD as well as graft and patient survival in LT by analyzing Korean Organ Transplantation Registry (KOTRY) database.
Results
Patient characteristics
Patient selection criteria is shown in Fig. 1. Among 5105 patients who underwent LT between April 2014 and December 2020 in KOTRY database, 2670 patients with HLA typing data were included in this study. A total of 18 patients with D → R one way HLA MM were compared with 2652 patients without D → R one-way HLA MM as control group (no D → R one way HLA MM group).
Table 1 summarizes the patient characteristics between the D → R one way HLA MM group and no D → R one way HLA MM group. All patients in D → R one way HLA MM group underwent living donor LT, whereas in the control group, 75.1% of patients underwent living donor LT (p = 0.011). In D → R one way HLA MM group, a higher proportion of donors were offspring of recipients compared to the control group (47.7% vs. 83.3%, p = 0.002). In addition, there was significant difference in transplanted graft type between the two groups (p = 0.045). 83.3% of recipients in D → R one way HLA MM group received right hemiliver graft while no patient received whole liver graft from their donors. Median warm ischemic time during LT was longer in D → R one way HLA MM group (35.3 min vs. 50.0 min, p = 0.025). Among 2670 LT recipients, total 11 patients underwent GVHD after LT. The incidence of GVHD (0.3% vs 22.2%, p < 0.001) and death (11.6% vs. 38.9%, p = 0.003) was much higher in D → R one way HLA MM group compared to the control group.
HLA type comparison between donor and recipient with GVHD after LT
We analyzed HLA types at each locus (HLA-A, -B, -DR) of all 11 donors and recipients who were reported to develop GVHD after LT (Table 2). If they share the same HLA, it is highlighted with a gray box. Among 11 patients with GVHD after LT, 6 patients underwent living donor LT and all of them received liver grafts from their offspring. Four patients with living donor LT showed D → R one way HLA MM, and three had D → R one way HLA MM at 3 loci. All of the 5 patients who underwent deceased donor LT did not have D → R one way HLA MM.
Risk factors associated with GVHD, graft failure, patient death
We analyzed risk factors for GVHD by using multivariate logistic regression analysis (Table 3). In the multivariate analysis, only D → R one way HLA MM was found to be a strong independent risk factor of GVHD. In the presence of D → R one way HLA MM at 3 loci, the OR was calculated as 163.3 (95% CI = 34.15–780.89, p < 0.001) while the OR of 1&2 MM were 91.85 (95% CI = 8.98–939.32, p < 0.001).
Risk factors associated with death-censored graft failure, and patient death were analyzed using Cox regression analysis (Table 4). Recipient age (HR = 0 0.98, 95% CI = 0.97–0.99, p < 0.001) and re-transplantation (HR = 2.76, 95% CI = 1.16–6.92, p = 0.005) were found to be associated with death-censored graft failure. However, D → R one way HLA MM was not associated with death-censored graft failure. In the multivariate analysis, deceased donor LT (HR = 1.64, 95% CI = 1.11–2.41, p = 0.012), D → R one way HLA MM at 3 loci (HR = 12.75, 95% CI = 5.16–31.52, p < 0.001), donor age (HR = 1.01, 95% CI = 1.00–1.02, p = 0.047), recipient age (HR = 1.03, 95% CI = 1.01–1.04, p = 0.047), MELD score (HR = 1.04, 95% CI = 1.02–1.06, p < 0.001), and re-transplantation (HR = 2.01, 95% CI = 1.05–3.87, p = 0.036) were found to be independent risk factors of patient death. However, D → R one way HLA MM at 1 or 2 loci was not related to either death-censored graft failure or patient death.
Clinical courses and outcomes of cases with donor against recipient one-way HLA mismatch
Table 5 summarizes the clinical courses of 18 cases with D → R one way HLA MM after LT. The cases were classified according to the number of HLA mismatches at each locus. There were 11 cases of D → R one way HLA MM at 3 loci, 2 cases of D → R one way HLA MM at 2 loci, and 5 cases of D → R one way HLA MM at 1 locus. In cases with mismatch at 3 loci, all the donors’ HLA type showed homozygous pattern. Five out of 11 recipients with D → R one way HLA MM at 3 loci died within a year after LT and among them, GVHD was reported in 3 cases, all of which developed 1–2 months after transplantation. Among 5 cases of D → R one way HLA MM at 1 locus, 2 recipients died, and one of them was reported to have GVHD.
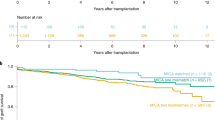
Figure 2 displays the survival curve according to the presence or absence of GVHD, and it is evident that patients who developed GVHD after liver transplantation showed significantly lower patient survival compared to those who did not. The patient survival, rejection free survival, and death-censored graft survival were also evaluated according to the number of HLA mismatches. D → R one-way HLA MM group again divided into two groups as patients with one-way MM at 3 loci and those with one-way MM at 1 or 2 loci. Patients with D → R one-way HLA MM at 3 loci showed significantly lower patient survival comparing to the control group (p < 0.001), while patients with D → R one-way HLA MM at 1 or 2 loci showed no difference against the control group (p = 0.159) (Fig. 3). Patient survival between D → R one-way HLA MM at 3 loci group and D → R one-way HLA MM at 1 or 2 loci group also showed no difference (p = 0.297). There were no significant differences in rejection-free survival (p = 0.133) and death-censored graft survival (p = 0.613) according to the number of D → R one-way HLA MM (Fig. 4).
Patient survival according to the number of donor against recipient one-way HLA mismatch (A). Patient survival between control group and donor against recipient one-way HLA mismatch at 3 loci (B). Patient survival between control group and donor against recipient one-way mismatch at 1 or 2 loci (C).
Discussion
There have been several studies on the impact of HLA compatibility on the outcomes after LT. According to some previous studies, it was obvious that the higher the HLA compatibility, the lower the probability of acute rejection after LT, but the effect on overall graft survival has been controversial2,9. Donaldson et al.3, demonstrated that HLA class I matching may affect the graft survival by increasing the possibility of development of acute rejection and the vanishing bile duct syndrome. However, by analyzing the OPTN database, Navarro et al.10 showed that there has been no clinically significant relationship between the degree of HLA matching and 5 years graft survival of LT. Recently, Bricogne et al.11 found that locus-specific HLA-A mismatching was associated with reducing graft failure and patient survival after LT by increasing hepatic artery thrombosis and sepsis.
There also has been an effort on finding relationship between HLA compatibility and GVHD after LT. Some previous studies highlighted the importance of D → R one-way HLA MM as a strong risk factor for GVHD12,13. However, since the prevalence of GVHD is extremely low, studies on the topic have been very difficult to find in the past decades. The previous study published by Kim et al.14, a retrospective single-center study, indicated that the D → R one-way HLA MM at 3 loci significantly increased the incidence of GVHD after LT. However, our study was designed as a large-scale multi-institutional study that used a prospectively updated data from a KOTRY registry. By comparing the D → R one-way HLA MM patient group with no D → R one-way HLA MM patient group, this study revealed a significant difference in the incidence of GVHD between these two groups. Moreover, for the D → R one-way HLA MM patient group, further division was made based on the number of MM loci differences to analyze the risk of GVHD, graft failure, and patient survival. Thereby showing that this phenomenon is not restricted to a single center but has similar outcomes in other centers.
Since this study is based on KOTRY data, it is difficult to review the clinical course of each patient. Therefore, there is a possibility of underdiagnosing GVHD in the study population. However, even considering the omission of some GVHD patients due to underdiagnosed GVHD, it was found that the D → R one-way HLA MM group showed a much higher incidence rate. About 0.4% (11 out of 2670 patients) of all the study cohort in the study was reported to have GVHD after LT. A total of 22.2% of patients were reported to have GVHD in D → R one-way HLA MM group, while in the control group, only 0.3% of the patients were reported to have GVHD. To more accurately analyze the relationship between GVHD and D → R one-way HLA MM, we analyzed HLA type at each locus (HLA-A, -B, -DR) of all patients with GVHD after LT. Interestingly, 4 out of 6 cases of living donor LT with GVHD showed D → R one-way HLA MM but none of the deceased donor LT cases with GVHD showed D → R one-way HLA MM. Especially, D → R one-way HLA MM at 3 loci occurred when the HLA-homozygous donor shared haplotype with HLA-heterogenous recipient, and this combination of HLA type usually happened when transplantation was made between parent and child. In fact, in the present study, all recipients with GVHD after living donor LT received liver graft from their offspring, and D → R one-way HLA MM was seen in a large proportion, which was 66.7% of recipients with GVHD after living donor LT.
In previous studies, close matching of HLA types between donors and recipients, age of recipients, and glucose intolerance found out to be risk factors for GVHD after LT4,6,8. However, in our study, D → R one-way HLA MM was the only significant independent risk factor for GVHD after LT. In multivariate analysis, D → R one-way HLA MM at 3 loci and D → R one-way HLA MM at 1 or 2 loci seemed highly associated with GVHD with odd ratio of 163.3 and 91.85, respectively. On the other hand, D → R one-way HLA MM was not related to graft failure after LT, and D → R one-way HLA MM at 1 or 2 loci was found not to be a risk factor for patient death. Only D → R one-way HLA MM at 3 loci was identified as the strongest risk factor for patient death. These findings represent that D → R one-way HLA MM at 3 loci is one of the most potent risk factors for GVHD which could lead to a devastating outcome such as patient death. In addition, according to the Kaplan–meier survival curve analysis, not D → R one-way HLA MM at 1 or 2 loci but only D → R one-way HLA MM at 3 loci showed significant lower patient survival compared to those who do not have D → R one-way HLA MM. There were no significant differences in death-censored graft survival between D → R one-way HLA MM group and the control group. In terms of rejection-free survival, there was no statistically significant difference between the two groups. However, it was observed that there was no incidence of rejection in the patient group with D → R one-way HLA MM. From the perspective of the recipient in the D → R one-way HLA MM situation, there's no mismatch with the donor's HLA, implying a very low possibility of the existence of donor-specific antibodies (DSA). This can be seen as a result that supports previous research findings suggesting that DSAs can influence rejection after liver transplantation15,16,17,18.
The limitation of this study is that since it is a retrospective multicenter study using the KOTRY data, information on other types of HLA alleles such as HLA-C, -DQ, and -DP were lacking, making it difficult to analyze on those HLA alleles. Likewise, it was unavailable to use the latest and more precise PCR based HLA typing data. Prior research in hematopoietic stem cell transplantation indicated that an antigen mismatch at the HLA-C * 14:02 locus might elevate the risk of GVHD, implying that a similar mismatch of antigens could also adversely affect liver transplantation outcomes19. However, Hirata et al.20 reported that the influence of HLA-C, HLA-DQ, and HLA-DP on GVHD was not as pronounced as that of HLA-A, HLA-B, and HLA-DR. We anticipate that with the accumulation of additional data on high-resolution sequence-based HLA typing and epitope matching in the future, we can proceed with further research and potentially undertake a more accurate mismatch analysis which may influence the outcome of liver transplantation, especially for GVHD. It was also hard to review the specific clinical course of each case from KOTRY data. Therefore, due to the non-specific symptoms and difficulties in making a definitive diagnosis of GVHD, there might be cases which were omitted to be diagnosed as GVHD. However, prospectively data collecting multicenter data clearly showed that HLA type, specifically, D → R one-way HLA MM at 3 loci is an extremely lethal prognostic factor for the occurrence of both GVHD and patient death which have its strength in generalizability of the finding.
Although there have been some studies reporting the risk of D → R one-way HLA MM at 3 loci on GVHD, we can assume that the importance is not quite emphasized to the general field of LT, since there are still cases with living donor LT with D → R one-way HLA MM. This may be due to the minimal reporting data on the topic since the odds are very low even in living donor LT setting. Before the LT community find the solution for this devastating condition, the only solution is not to perform transplantation in this high-risk combination of donor and recipient.
In conclusion, among patients considering living donor LT, if donors’ HLA type shows homozygous pattern and shares haplotype of HLA with their recipients, the probability of D → R one-way HLA MM at 3 loci would be very high, which is associated with GVHD. This could lead to fatal outcome, leading to the death of the patient. Therefore, in such a case, it is necessary to select alternative donor or to withhold transplantation. However, although the possibility of developing D → R one-way HLA MM is extremely rare in the case of deceased donor LT, there is still possibility that GVHD can occur so that further research should be needed on GVHD which occurs during deceased donor LT.
Patients and methods
Study cohort
This study is a retrospective cohort study of patients enrolled in KOTRY database. KOTRY is a prospective, multicenter cohort registry, which is composed of 5 solid organ transplantation cohorts, including kidney, liver, pancreas, heart, and lung21. Patients who underwent LT from 15 institutions in South Korea are enrolled in KOTRY. After receiving written informed consent prior to transplantation, patients were registered in the KOTRY database, and routinely followed-up. This study was reviewed and approved by the Institutional Ethics Committees of each participating center, according to the Regulations on Human Organ Transplant and national legal requirements. The procedures were in accordance with the Helsinki declaration.
We reviewed 5105 patients who underwent LT between April 2014 and December 2020 in KOTRY database. In South Korea, the HLA typing test of LT patients was not yet implemented in earnest until 2016, and since it was a retrospective study using the KOTRY data, HLA typing test results were often omitted. Therefore, among them, 2670 patients with serologic HLA typing of both recipient and donor were included in this study while who do not have the data were excluded. The cohort was divided into two groups according to the presence of D → R one-way HLA MM. The diagnosis of GVHD in the study was based on the reports of the participating centers.
Diagnosis criteria of GVHD
When clinical symptoms such as skin rash, cytopenia, or diarrhea were observed after a liver transplant, raising suspicions of GVHD, a pathological biopsy (confirmed through methods like skin biopsy or mucosal biopsy via colonoscopy) was conducted. Whenever possible, positive chimerism of the peripheral blood was also performed to diagnose GVHD. The diagnostic approach was carried out in accordance with the protocols of each hospital.
Definition of donor against recipient one-way HLA mismatch (D → R one-way HLA MM)
Serologic HLA typing with HLA-A, -B, -DR locus-specific analysis of both recipient and donor was performed before transplantation. The number of serologic HLA mismatches on each locus between donors and recipients were identified. When all the donor’s HLA types were included in recipient’s HLAs while some of the recipient’s HLAs were different from the donors’ HLAs, the condition was defined as donor against recipient one-way HLA mismatch (D → R one-way HLA MM).
Statistical analysis
Numerical variables of the two groups were presented as median with interquartile range (IQR) which were analyzed by Mann–Whitney test. Categorical variables of the two groups were presented as percentage and were analyzed by Pearson’s chi-squared test or Fischer’s exact test. Logistic regression analysis was used for analyzing risk factors of GVHD. Univariate and multivariate Cox proportional hazard regression model was used in analyzing risk factors associated with graft failure, and patient death after LT. Kaplan–Meier survival curve analysis was performed to estimate the overall patient survival, rejection-free survival, and death-censored graft survival between the two groups. Statistical analyses were conducted with SPSS 26.0 (SPSS Inc., Chicago, IL).
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- LT:
-
Liver transplantation
- GVHD:
-
Graft-versus-host disease
- HLA:
-
Human leukocyte antigen
- LDLT:
-
Living donor liver transplantation
- GRWR:
-
Graft-recipient weight ratio
- IQR:
-
Interquartile range
- MELD:
-
Model for end-stage liver disease
- DDLT:
-
Deceased donor liver transplantation
References
Sheldon, S. & Poulton, K. HLA typing and its influence on organ transplantation. Methods Mol. Biol. 333, 157–174. https://doi.org/10.1385/1-59745-049-9:157 (2006).
Markus, B. H. et al. Histocompatibility and liver transplant outcome. Does HLA exert a dualistic effect?. Transplantation 46, 372–377 (1988).
Donaldson, P. et al. Influence of human leukocyte antigen matching on liver allograft survival and rejection: “The dualistic effect”. Hepatology 17, 1008–1015 (1993).
Taylor, A. L., Gibbs, P. & Bradley, J. A. Acute graft versus host disease following liver transplantation: the enemy within. Am. J. Transpl. 4, 466–474. https://doi.org/10.1111/j.1600-6143.2004.00406.x (2004).
Chan, E. Y. et al. Recipient and donor factors influence the incidence of graft-vs.-host disease in liver transplant patients. Liver Transpl. 13, 516–522. https://doi.org/10.1002/lt.21082 (2007).
Smith, D. M. et al. Liver transplant-associated graft-versus-host disease. Transplantation 75, 118–126. https://doi.org/10.1097/00007890-200301150-00022 (2003).
Murali, A. R. et al. Graft versus host disease after liver transplantation in adults: A case series, review of literature, and an approach to management. Transplantation 100, 2661–2670. https://doi.org/10.1097/TP.0000000000001406 (2016).
Elfeki, M. A. et al. Graft-versus-host disease after orthotopic liver transplantation: Multivariate analysis of risk factors. Clin. Transpl. 29, 1063–1066. https://doi.org/10.1111/ctr.12627 (2015).
Neumann, U. P. et al. Impact of human leukocyte antigen matching in liver transplantation. Transplantation 75, 132–137. https://doi.org/10.1097/00007890-200301150-00024 (2003).
Navarro, V., Herrine, S., Katopes, C., Colombe, B. & Spain, C. V. The effect of HLA class I (A and B) and class II (DR) compatibility on liver transplantation outcomes: an analysis of the OPTN database. Liver Transpl. 12, 652–658. https://doi.org/10.1002/lt.20680 (2006).
Bricogne, C. et al. Donor-recipient human leukocyte antigen A mismatching is associated with hepatic artery thrombosis, sepsis, graft loss, and reduced survival after liver transplant. Liver Transpl. 28, 1306–1320. https://doi.org/10.1002/lt.26458 (2022).
Kamei, H. et al. Fatal graft-versus-host disease after living donor liver transplantation: differential impact of donor-dominant one-way HLA matching. Liver Transpl. 12, 140–145. https://doi.org/10.1002/lt.20573 (2006).
Uchiyama, H. et al. Relevance of HLA compatibility in living donor liver transplantation: The double-edged sword associated with the patient outcome. Clin. Transpl. 26, E522-529. https://doi.org/10.1111/ctr.12019 (2012).
Kim, S. J. et al. The clinical impact of donor against recipient HLA one way mismatch on the occurrence of graft versus host disease in liver transplantation. Sci. Rep. https://doi.org/10.1038/s41598-022-24778-2 (2022).
Kaneku, H. et al. De novo donor-specific HLA antibodies decrease patient and graft survival in liver transplant recipients. Am. J. Transpl. 13, 1541–1548. https://doi.org/10.1111/ajt.12212 (2013).
O’Leary, J. G. et al. Preformed class II donor-specific antibodies are associated with an increased risk of early rejection after liver transplantation. Liver Transpl. 19, 973–980. https://doi.org/10.1002/lt.23687 (2013).
O’Leary, J. G. et al. The role of donor-specific HLA alloantibodies in liver transplantation. Am. J. Transpl. 14, 779–787. https://doi.org/10.1111/ajt.12667 (2014).
Jucaud, V. et al. Prevalence and impact of de novo donor-specific antibodies during a multicenter immunosuppression withdrawal trial in adult liver transplant recipients. Hepatology 69, 1273–1286. https://doi.org/10.1002/hep.30281 (2019).
Morishima, S. et al. High-risk HLA alleles for severe acute graft-versus-host disease and mortality in unrelated donor bone marrow transplantation. Haematologica 101, 491 (2016).
Hirata, M. et al. Donor-dominant one-way matching of human leukocyte antigen-A/B/DR alleles predicts graft-versus-host disease following living donor liver transplantation. Hepatol. Res. 51, 135–148 (2021).
Yang, J. et al. Design and methods of the Korean organ transplantation registry. Transpl. Direct 3, e191. https://doi.org/10.1097/TXD.0000000000000678 (2017).
Acknowledgements
This research was supported by a fund (2014-ER6301-00, 2014-ER6301-01, 2014-ER6301-02, 2017-ER6301-00, 2017-ER6301-01, 2017-ER6301-02, 2020-ER7201-00) by Research of Korea Centers for Disease Control and Prevention Agency. The Korean Organ Transplantation Registry Study Group: Young Rok Choi, Dong Jin Joo, Young Kyoung You, Bong-Wan Kim, Yang Won Nah, Jai Young Cho, Tae-Seok Kim, Geun Hong, Man Ki Ju, Suk-Won Suh, Jae Do Yang, Pyoung Jae Park, Jaehong Jeong, Ju Ik Moon, Dong-Sik Kim.
Author information
Authors and Affiliations
Consortia
Contributions
S.P. and J.R. developed the research idea and participated in the study design and writing of the paper. S.P., J.R., Y.R.C., D.J.J., Y.K.Y., B.K., Y.W.N., J.Y.C., T.K., G.H., M.K.J., S.S., J.D.Y., P.J.P., J.J., J.I.M., and D.K. participated in data acquisition and interpretation. S.P. and J.R. participated in statistical analysis. Each author contributed important intellectual content during manuscript drafting. J.R. and D.K. provided supervision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, S., Choi, Y.R., Joo, D.J. et al. The effect of donor against recipient one-way HLA mismatch on liver transplantation outcomes from a multicenter registry analysis. Sci Rep 13, 22296 (2023). https://doi.org/10.1038/s41598-023-49178-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-49178-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.