Abstract
Previous studies have reported significant decreases in the incidence of mental health problems following SARS-CoV-2 vaccination. However, less relevant studies are published in China. We conducted a cross-sectional study involving Chinese adults aged 18–75 years with no known psychiatric diseases. The study used data from mental health of SARS-CoV-2 vaccinated and unvaccinated participants from May 2020 to July 2021.Three standardized scales, namely, the Generalized Anxiety Disorder-7 (GAD-7) for anxious symptoms, Patient Health Questionnaire-9 (PHQ-9) for depressive symptoms and Athens Insomnia Score-8 (AIS-8) for insomnia symptoms, as well as basic demographic questions were used. The hierarchical regression method was used for multivariate logistic regression analysis to explore the effects of SARS-CoV-2 vaccination on anxious, insomnia, and depressive symptoms. The results confirmed first that vaccinated participants experienced significantly lower anxious, insomnia, and depressive symptoms scores (P < 0.001) compared with unvaccinated participants. Second that vaccinated participants had a lower prevalence of anxious, insomnia, and depressive symptoms (P < 0.001). Third, after adjusting for potential confounders, we still observed a good correlation between vaccination and a reduced risk of anxious, insomnia, and depressive symptoms. The current study showed that SARS-CoV-2 vaccination may be helpful in improving anxious, insomnia, and depressive symptoms.
Similar content being viewed by others
Introduction
The prevalence of COVID-19 has brought unprecedented losses to society and seriously impacted our normal lives. By April 2022, more than 500 million cases had been confirmed worldwide, including more than 6 million deaths1,2. In addition, more than 210,000 cases occurred in China, including more than 5000 deaths according to the reported data of Chinese government.The pandemic not only brought the risk of infection and even death to people worldwide but also brought unprecedented psychological distress to humanity1,2,3. Previous studies have confirmed that the incidence rate of psychiatric disorders increased under the influence of the COVID-19 pandemic2,4,5,6,7. A national cross-sectional survey completed in Sweden showed that anxious symptoms and insomnia symptoms were significantly different, with incidence rates of 24.2% and 38%, respectively8. Undoubtedly, the prevalence of anxious symptoms and sleep disorders during the COVID-19 pandemic has been fully proven9,10, and people around the world are experiencing more serious mental health problems than before.
To control the spread of the pandemic, restore normal lifestyles as soon as possible, and reduce high mortality and economic losses, vaccination has become the most important and effective measure11. A study conducted in Israel showed that two doses of the SARS-CoV-2 vaccine BNT162b2 in more than 6 million people can prevent asymptomatic and symptomatic SARS-CoV-2 infections and reduce the incidence rate, severity, morbidity, and mortality of COVID-19 among all participants12. In addition, a study from the United States showed that vaccination with mRNA SARS-CoV-2 vaccine can reduce the possibility of progression to death or mechanical ventilation in hospitalized patients12. The results showed that SARS-CoV-2 vaccination could help control the pandemic13. Considering that vaccination can lower the risk of infection and mortality, we assume that vaccination against SARS-CoV-2 may reduce the incidence of anxious symptoms, insomnia symptoms, and/or depressive symptoms during the COVID-19 pandemic.
Previous studies have confirmed that the prevalence of anxious symptoms and depressive symptoms among vaccinated people in the United States is significantly lower than that among unvaccinated people14. Another study from Bangladesh explored the relationship between vaccination and other mental health problems and found that the prevalence of both anxious symptoms and depressive symptoms reduced after vaccination9. As of July, 2021, more than a million doses of SARS-CoV-2 vaccine have been reported according to the CDC data in China. However, to date, limited data have evaluated the effects of SARS-CoV-2 vaccination on mental health problems during COVID-19 in China. To resolve this problem, we investigated whether SARS-CoV-2 vaccination could alleviate the symptoms of anxiety, insomnia, and depression using a web-based tool in China. Our work should provide a better understanding of the effects of SARS-CoV-2 vaccination on mental health problems during the COVID-19 pandemic.
Methods
Study participants
A descriptive, cross-sectional survey with non-probabilistic (snow-ball) sampling method was designed to assess the symptoms of anxiety, insomnia, and depression in vaccinated and unvaccinated participants during the COVID-19 pandemic using an anonymous online questionnaire survey platform (“Questionnaire Star”, WeChat app, Tencent Company). The study recruited participants aged 18–75 years by distributing the questionnaire to different WeChat groups and users. We briefly introduced the purpose and significance of the study, as well as the requirements (including age range and whether to participate voluntarily, etc.) before the survey began. Each participant received a survey link that will be useless once the questionnaire was submitted, making this a close-ended survey that did not permitted to be submitted multiple times. Each question was clear and easy to understand in our survey. All participants came from China using WeChat and provided their written informed consent prior to their participation.
Participants who met the following conditionswere enrolled: (1) aged 18–75 years, (2) could complete questionnaire survey, (3) WeChat user, and (4) volunteered for the survey. Exclusion criteria included the following: (1) without complete information (2) unable to understand the questionnaire, (3) with a history of psychiatric diseases. The study flowchart is shown in Fig. 1. Ultimately, 9452 questionnaires (response rate, 99.46%) were included in the final analysis. 51 questionnaires were excluded due to missing information or other reasons. This study was approved by the Ethics Committee of Changde Hospital, Xiangya School of Medicine, Central South University (The first people’s hospital of Changde city), Hunan Province, China (No. 2021–040-01). The research was also performed in accordance with the relevant guidelines and regulations.
Data collection
A standard questionnaire was developed to assess demographic characteristics (age, gender, education level, occupation, marital status, and personal monthly income) and other demographic and socioeconomic indicators, as well as the scores of the GAD-7, AIS-8, and PHQ-9 (explained below). The focus of this research was to understand whether the symptoms of anxiety, insomnia, and depression of all participants can improve after SARS-CoV-2 vaccination. The survey was conducted between May 2020 and July 2021. Ultimately 2245 unvaccinated and 7207 vaccinated individuals were included in this study.
Survey tools
Generalized anxiety disorder-7 (GAD-7)
The GAD-7 is a self-assessment scale for screening and diagnosing anxiety, and it is a 7-item anxious symptoms assessment with scores ranging from 0 to 2115. The severity of anxious symptoms can be determined according to the following thresholds:1–4 (minimal symptoms), 5–9 (mild symptoms), 10–14 (moderate symptoms), and ≥ 15 (severe symptoms)16. A score of five or above can be used as the critical value for anxiety17. This study considered a total score of more than 5 for anxiety. The Cronbach’s alpha for this study was 0.941.
Athens Insomnia Scale-8 (AIS-8)
AIS-8 is a self-assessment scale for the screening and diagnosis of insomnia. The scale consisted of eight sub-items18. Scores ranged from 0 to 24 based on 0–3 (0 = none, 1 = lowest, 2 = significant, and 3 = severe). A total score of 6 points was considered critical for the diagnosis of insomnia with clinical significance19. The Cronbach’s alpha for this study was 0.914.
Patient Health Questionnaire-9 (PHQ-9)
We used the Patient Health Questionnaire-9 (PHQ-9) to assess depressive disorders. This instrument includes nine items coded on a scale from 0 to 3 (0 = not at all, 1 = several days, 2 = more than half of the days, and 3 = nearly every day). Total scores ranged from 0 to 27, with a higher score suggesting the presence of a more severe depressive disorder. The depressive symptoms categories were defined as normal (0–4), mild (5–9), moderate (10–14) and severe (≥ 15). A cutoff of ≥ 5 on the PHQ-9 was used as an indicator of clinical depressive disorders20. The Cronbach’s alpha for this study was 0.916.
Statistical analysis
All analyses were performed using SPSS 26.0, Stata/SE 15.0, and the test level α was set to 0.05. Forest plots were drawn using R programming language.
Continuous variables satisfying normality were described as mean ± SD, and an independent sample t-test was used for inter-group comparison; continuous variables that did not meet normality were described by median and quartile (Q1, Q3). Dichotomous or unordered multi-category variables were described by the number of cases (n) and percentage (%), and the groups were compared using the χ2 test. Ordinal categorical variables (rank variables: anxious symptoms and depressive symptoms) were described by the number of cases (N) and percentage (%). Ordinal categorical variables (rank variables: anxious symptoms level and depressive symptoms level) were described by the number of cases (N) and percentage (%), and the Wilcoxon rank-sum test was used for comparisons between groups.
Variables with statistical significance (P < 0.05) in the above comparison between groups were used as independent variables, and the hierarchical regression method was used for multivariate logistic regression analysis to explore the effect of vaccination on anxious and insomnia symptoms. When anxiety was used as the dependent variable, the second layer was adjusted for age and gender, and the third layer was adjusted for education level, marital status, and personal monthly income. When insomnia was used as the dependent variable, the second layer was adjusted for age and gender; the third layer was adjusted for education level, marital status, personal monthly income, and the fourth level was adjusted for anxious symptoms. When depression was the dependent variable, the second stratum was adjusted for age and gender; the third stratum was adjusted for education level, marital status, and personal monthly income; the fourth stratum was adjusted for anxious symptoms; and the fifth stratum was adjusted for insomnia symptoms.
Results
Characteristics of all participants
This study included 9452 participants, of which 2245 (23.8%) were unvaccinated and 7207 (76.2%) were vaccinated. The average age of all respondents was 35.97 ± 11.62 years old, and the male-to-female ratio was 1:1.3. Over two-thirds were from urban areas; about half of the respondents were professional and technical personnel or self-employed/business personnel, 68.5% were married, most participants (85.5%) had a personal monthly income of 10,000 RMB or less, and more than three-fifths had a college/undergraduate education. Among all the respondents, 1676 (17.7%) participants presented with anxious symptoms, 2150 (22.7%) presented with insomnia symptoms, and 2681 (28.4%) had depressive symptoms (Table 1).
The symptoms of anxiety, insomnia and depression of participants before and after vaccination
The median of the interquartile range (IQR) of the GAD-7, AIS-8, and PHQ-9 scores of unvaccinated individuals were 3 (0–7), 4 (0–7), and 6 (0, 10), respectively, which were higher than the scores of 0 (0–0), 1 (0–4), and 0 (0, 3) of vaccinated individuals (P < 0.001). Moreover, vaccination with the SARS-CoV-2 vaccine significantly reduced the prevalence of anxiety and depression severity ([Z = − 38.05, P < 0.001] and [Z = − 35.45, P < 0.001]), as detailed in Table 2.
The symptoms of anxiety, insomnia and depression of participants with different characteristics
As shown in Table 3, the prevalence of anxiety among the vaccinated respondents was 9.7%, which was much lower than that among the unvaccinated respondents (43.7%; χ2 = 1356.13, P < 0.001). The mean age of the participants with anxious symptoms was lower than that of the subjects without anxious symptoms (t = 19.18, P < 0.001). In addition, significant differences in the prevalence of anxious symptoms were found among respondents with different gender, occupation, marital status, monthly income, and educational level (P < 0.001).
As shown in Table 4, the prevalence of insomnia among vaccinated respondents was much lower than that among unvaccinated respondents (16.2% vs. 43.7%) (χ2 = 738.56, P < 0.001). The prevalence of insomnia symptoms in participants with anxious symptoms was 63.3%, which was significantly higher than that in participants without anxious symptoms (4.3%; χ2 = 3961.93, P < 0.001). Significant differences in the prevalence of insomnia symptoms were found among respondents with different occupations, marital status, monthly income, and educational level (P < 0.001).
In addition, Table 5 shows that vaccinated respondents had a lower prevalence of depressive symptoms symptoms than unvaccinated respondents (19.7% vs. 56.1%) (χ2 = 1116.69, P < 0.001). The prevalence of depressive symptoms was 93.4% among participants with anxious symptoms and 81.7% among participants with insomnia symptoms, which was significantly higher than those without anxious or insomnia symptoms (P < 0.001). In addition, there were significant differences in the prevalence of depressive symptoms among respondents with different occupation, marital status, monthly income, and education level (P < 0.001).
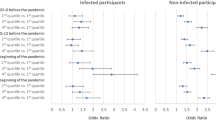
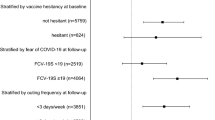
Association between vaccination and anxious symptoms
Figure 2 suggests a significant association between vaccination and anxious symptom. Specifically, Model 1 showed that vaccinated respondents had an 86.2% lower risk of anxiety (OR = 0.138, 95% CI 0.123–0.155). After adjusting for age and gender, the risk of anxiety decreased by 0.856 times after vaccination (OR = 0.144, 95% CI 0.127–0.163; Model 2). After further adjustment for known factors such as education level, occupation, marital status, and monthly income based on Model 2, vaccinated respondents had a lower risk of anxiety than unvaccinated respondents (OR = 0.150, 95% CI 0.132–0.172; Model 3).
Forest plot showing the association between vaccination and anxious symptoms. CI = confidence interval, OR = odds ratio. The independent variable of Model 1 is vaccination. Model 2 adjusted the age and gender at the base of Model 1, and Model 3 adjusted the education level, occupation, marital status and monthly income at the base of Model 2.
Association between vaccination and insomnia symptoms
Figure 3 shows a significant association between vaccination and insomnia symptoms. Specifically, Model 1 showed that vaccinated respondents had 75.2% decreased odds of insomnia symptoms (OR = 0.248, 95% CI 0.224–0.276). According to the second model, the risk of insomnia symptoms decreased 0.749 times after vaccination (OR = 0.251, 95% CI 0.224–0.282). Based on Model 3, vaccinated respondents had lower odds of insomnia symptoms than unvaccinated respondents (OR = 0.230, 95% CI 0.198–0.267). After further adjusted for anxious symptoms, Model 4 showed a 40.2% reduction in the odds of insomnia symptoms among vaccinated respondents (OR = 0.598, 95% CI 0.492–0.729).
Forest plot showing the association between vaccination and insomnia symptoms. CI = confidence interval, OR = odds ratio. The independent variable of Model 1 is vaccination. Model 2 adjusted the age and gender at the base of Model 1, and Model 3 adjusted education level, occupation, marital status and monthly income at the base of Model 2. Model 4 adjusted anxious symptom at the base of Model 3.
Association between vaccination and depressive symptoms
Figure 4 shows a significant association between vaccination and depressive symptoms. Specifically, Model 1 showed that vaccinated respondents had an 80.8% reduced risk of depressive symptoms (OR = 0.192, 95% CI 0.174–0.213). According to Model 2, the risk of depressive symptoms decreased by 0.799 after vaccination (OR = 0.201, 95% CI 0.180–0.225). Based on Model 3, vaccinated respondents had a lower risk of depressive symptoms than unvaccinated respondents (OR = 0.194, 95% CI 0.169–0.224). After adjusting for anxious symptoms, the relationship persisted (OR = 0.412, 95% CI 0.342–0.497), as detailed in Model 4. This association remained significant after adjusting for insomnia symptoms (yes/no) (OR = 0.433, 95% CI 0.354–0.530; Model 5).
Forest plot showing the association between vaccination and depressive symptoms. CI = confidence interval, OR = odds ratio. The independent variable of Model 1 is vaccination. Model 2 adjusted the age and gender at the base of Model 1, and Model 3 adjusted the education level, occupation, marital status and monthly income at the base of Model 2. Model 4 adjusted anxious symptoms at the base of Model 3. Model 5 adjusted insomnia symptoms at the base of Model 4.
Discussion
In this study, we investigated whether SARS-CoV-2 vaccination has a potentially positive effect on the symptoms of anxiety, insomnia, and depression during the COVID-19 pandemic. To address this issue, we conducted a cross-sectional study that recruited 9425 respondents. This work may be the first largest survey enrolling vaccinated and unvaccinated respondents during the COVID-19 pandemic in China. Our results showed that the scores for anxious, insomnia, and depressive symptoms in vaccinated subjects were significantly lower than those in unvaccinated subjects (all P < 0.001). In addition, SARS-CoV-2 vaccination could significantly reduce the prevalence of anxious, insomnia, and depressive symptoms, and mild or greater anxious ([Z = − 38.05, P < 0.001] and depressive symptoms [Z = − 35.45, P < 0.001]). Furthermore, we observed a good association between SARS-CoV-2 vaccination and a reduced risk of anxious, insomnia, and depressive symptoms. In addition, these associations were independent of potential confounders including age, gender, education level, marital status, personal income, and occupation.
As previously mentioned, our results confirmed that anxious and depressive symptoms scores were significantly reduced after vaccination. These data were consistent with a prior study conducted in Bangladesh9, which suggested that vaccinated healthcare workers had significantly lower scores for the symptoms of depression (1.0 [1.0–2.0] vs. 3.0 [2.0–5.0]; P < 0.01) and insomnia (3.0 [4.0–7.0] vs. 6.0 [5.0–11.0]; P < 0.01). Expecting similar findings, this study further confirmed that the quartile scores of post-traumatic stress disorder and loneliness symptoms were lower in the vaccinated groups with the present work, and that vaccination may effectively alleviate mental health problems. From Tables 3, 4, 5, our findings are also similar to those of another study from the United States, which concluded that the prevalence of anxious and depressive symptoms is higher in unvaccinated participants than in vaccinated participants14. A domestic study focusing on 1336 medical students showed that the risk of depression and anxiety symptoms of participants vaccinated twice decreased by 0.6–0.8 times compared with those unvaccinated21. The completion of vaccination had a positive influence on mental health outcomes22. Despite the limited number of similar studies, the literature showed that the risk of death of vaccinated patients infected with COVID-19 would be significantly reduced12. Alternatively, vaccination can reduce constraints during a pandemic and is effective in improving people’s mental health problems. The psychological problems of widowed, divorced, separated, high-income people (monthly income > 10,000 CNY) were alleviated more significantly after SARS-CoV-2 vaccination23. However, among people with lower education levels, the relief of anxious and insomnia symptoms caused by vaccination showed more obvious results. Such people lack awareness of the negative effects of the vaccine, and vaccine hesitancy is common in highly educated groups24. In addition, vaccination could reduce the probability of insomnia symptoms in our study, but this has not been identified in the studies by Alam et al.25 and Wu et al.21. The main reasons for this discrepancy may be related to sample size, demographic structure, respondents, and contextual differences.
The model data obtained by hierarchical regression showed that anxious, insomnia, and depressive symptoms risk of vaccinated participants decreased significantly, and vaccination was still statistically correlated with the above psychological problems even after adjusting for several related factors. Previous studies have shown that vaccination can block the transmission of pathogens in addition to protecting oneself26. It can not only reduce the economic burden caused by diseases but also form a protective barrier against other infections and further alleviate the pressure on public health and psychological problems27,28. In the current situation of the COVID-19 pandemic, vaccination not only reduces the chance of infection and severe illness but also reduces the fear of the COVID-19 pandemic and improves mental health. This is similar to the findings of a previous study in the United States29. Although nearly 70 anxiety-related events have been reported in 8624 Janssen COVID-19 vaccine recipients in 202130, which may bring new mental and psychological problems to vaccine recipients at an early stage of vaccination, we believe that any vaccination may lead to anxiety-related events. This observation may simply be a chance occurrence; however, our research has added similar data.
To our knowledge, this maybe the largest sample study in China to explore whether anxious, insomnia, and depressive symptoms can be alleviated after vaccination. Our findings contribute to fill the gap in understanding the impact of SARS-CoV-2 vaccination on mental health status in China. The current study also has some limitations that should be considered in the analysis. First, the cross-sectional study conducted in China could hardly be generalized to other regions and our results can only reflect the situation and influencing factors in the specific period of time (May 2020 to July 2021). Second, the data were collected based on the participants’ self-reports, which may have led to a certain degree of reporting bias. Third, the research population concentrated on respondents aged 18–75 years. Therefore, the research results maybe not extended to other age groups. Fourth, most participants (76.2%) in this study were vaccinated, and only 23.8% were unvaccinated. A large difference in sample size was noted between the two groups, which may reduce the power of the statistical analysis. To compensate for these drawbacks, future research should consider increasing the elderly and minor populations, especially those without vaccination.
In summary, the current study confirmed that SARS-CoV-2 vaccination during the COVID-19 pandemic may be effective in alleviating anxious, insomnia, and depressive symptoms. After adjusting for potential factors, we found a good correlation between vaccination and reduction in anxious, insomnia, and depressive symptoms. In addition, our research may provide favorable conditions for improving vaccination programmes in China and worldwide in the future.
Data availability
The raw data supporting the conclusions of this article is available from the corresponding author (Jian Xu) on reasonable request.
References
Adam, D. COVID’s true death toll: Much higher than official records. Nature 603, 562 (2022).
Zhang, Q., Bastard, P., Effort, C. H. G., Cobat, A. & Casanova, J. L. Human genetic and immunological determinants of critical COVID-19 pneumonia. Nature 603, 587–598 (2022).
Baker, N. & Adam, D. Coronapod: COVID death toll is likely millions more than official counts. Nature https://doi.org/10.1038/d41586-022-00171-x (2022).
Caycho-Rodriguez, T. et al. Predictors of mental health during the COVID-19 pandemic in older adults: The role of socio-demographic variables and COVID-19 anxiety. Psychol. Health Med. 27, 453–465 (2022).
Egede, L. E. et al. Short-term impact of COVID-19 on quality of life, perceived stress, and serious psychological distress in an adult population in the midwest United States. Qual. Life Res. 31, 2387–2396 (2022).
Lasalvia, A. et al. The psychological impact of COVID-19 among primary care physicians in the province of Verona, Italy: A cross-sectional study during the first pandemic wave. Fam. Pract. 39, 65–73 (2022).
Varma, P., Junge, M., Meaklim, H. & Jackson, M. L. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog. Neuropsychopharmacol. Biol. Psychiatry 109, 110236 (2021).
McCracken, L. M., Badinlou, F., Buhrman, M. & Brocki, K. C. Psychological impact of COVID-19 in the Swedish population: Depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur. Psychiatry 63, e81 (2020).
Mamun, M. A. et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: A population-based nationwide study. J. Affect. Disord. 279, 462–472 (2021).
Pizzonia, K. L. et al. Insomnia during the COVID-19 pandemic: The role of depression and COVID-19-related risk factors. Cogn. Behav. Ther. 50, 246–260 (2021).
Graham, B. S. Rapid COVID-19 vaccine development. Science 368, 945–946 (2020).
Haas, E. J. et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: An observational study using national surveillance data. Lancet 397, 1819–1829 (2021).
Menni, C. et al. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: A prospective observational study. Lancet Infect. Dis. 21, 939–949 (2021).
Chen, S., Aruldass, A. R. & Cardinal, R. N. Mental health outcomes after SARS-CoV-2 vaccination in the United States: A national cross-sectional study. J. Affect. Disord. 298, 396–399 (2022).
Liu, Y. et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J. Affect. Disord. 278, 144–148 (2021).
Johnson, S. U., Ulvenes, P. G., Oktedalen, T. & Hoffart, A. Psychometric properties of the general anxiety disorder 7-item (GAD-7) scale in a heterogeneous psychiatric sample. Front. Psychol. 10, 1713 (2019).
Zou, X. et al. Factors associated With healthcare workers’ insomnia symptoms and fatigue in the fight against COVID-19, and the role of organizational support. Front. Psychiatry 12, 652717 (2021).
Fu, W. et al. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl. Psychiatry 10, 225 (2020).
Enomoto, K. et al. Reliability and validity of the Athens Insomnia Scale in chronic pain patients. J. Pain Res. 11, 793–801 (2018).
Kroenke, K. PHQ-9: Global uptake of a depression scale. World Psychiatry 20, 135–136 (2021).
Wu, H. et al. Psychological health and sleep quality of medical graduates during the second wave of COVID-19 pandemic in post-epidemic Era. Front. Public Health 10, 876298 (2022).
Mazereel, V., Van Assche, K., Detraux, J. & De Hert, M. COVID-19 vaccination for people with severe mental illness: Why, what, and how?. Lancet Psychiatry 8, 444–450 (2021).
Ciuffreda, G. et al. Factors associated with depression and anxiety in adults ≥60 years old during the COVID-19 pandemic: A systematic review. Int. J. Environ. Res. Public Health 18, 11859 (2021).
Ozceylan, G., Toprak, D. & Esen, E. S. Vaccine rejection and hesitation in Turkey. Hum. Vaccin. Immunother. 16, 1034–1039 (2020).
Alam, M. D., Paul, S. K., Momi, M., Ni, L. & Xu, Y. Factors associated with psychological outcomes among vaccinated and unvaccinated health care workers against COVID-19 infection in Bangladesh. Front. Med. 9, 852922 (2022).
Doherty, M., Buchy, P., Standaert, B., Giaquinto, C. & Prado-Cohrs, D. Vaccine impact: Benefits for human health. Vaccine 34, 6707–6714 (2016).
Nandi, A. & Shet, A. Why vaccines matter: Understanding the broader health, economic, and child development benefits of routine vaccination. Hum. Vaccin. Immunother. 16, 1900–1904 (2020).
Scholz, S. et al. Public health impact and cost-effectiveness analysis of routine infant 4CMenB vaccination in Germany to prevent serogroup B invasive meningococcal disease. Infect. Dis. Ther. 11, 367–387 (2022).
Koltai, J., Raifman, J., Bor, J., McKee, M. & Stuckler, D. Does COVID-19 vaccination improve mental health? A difference-in-difference analysis of the Understanding Coronavirus in America study. medRxiv https://doi.org/10.1101/2021.07.19.21260782 (2021).
Hause, A. M. et al. Anxiety-related adverse event clusters after Janssen COVID-19 vaccination—five U.S. mass vaccination sites, April 2021. MMWR Morb. Mortal. Wkly. Rep. 70, 685–688 (2021).
Acknowledgements
The authors wish to thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (82102632, 82160412), Changde Hospital, Xiangya School of Medicine, Central South University (The first people’s hospital of Changde city) (2022ZZ11), The science and technology innovation program of Changde city (2022.51.1) and COVID-19 Emergency Special Project of Changde Science and Technology Bureau (2020SK005).
Author information
Authors and Affiliations
Contributions
J.X., Y.C., X.B.Z. and Q.Y. wrote the paper. M.X.L., L.Z. collected the data. C.P.W. analyzed the data. X.B.Z. and Q.Y. proofread the manuscript. All the authors contributed reviewing the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, X., Yue, Q., Li, M. et al. SARS-CoV-2 vaccination may improve anxious, insomnia and depressive symptoms among Chinese population aged 18–75 years during the COVID-19 pandemic. Sci Rep 13, 22029 (2023). https://doi.org/10.1038/s41598-023-48977-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48977-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.