Abstract
Sarcopenia is a disease characterized by decreased muscle mass and strength, affecting 20–70% of patients with cirrhosis, and is associated with poor prognosis, complications, and high mortality. At present, the epidemiological investigation of sarcopenia in patients with liver cirrhosis is relatively limited, and because of the differences in population characteristics, regions, diagnostic criteria and diagnostic tools, the prevalence of sarcopenia in various studies varies greatly. The definition of sarcopenia in this study adopted the criteria of the Asian Working Group on Sarcopenia (AWGS 2019), including muscle mass and muscle strength / physical performance. A total of 271 patients with liver cirrhosis were included in this cross-sectional study to explore the influencing factors of sarcopenia in patients with liver cirrhosis. The prevalence of sarcopenia was 27.7%, 27.3% in male and 28.4% in female. The results of binary logistic regression analysis showed that age, physical activity, BMI, mid-upper arm muscle circumference, hepatic encephalopathy, nutritional status, alkaline phosphatase, albumin and total cholesterol were significantly correlated with the occurrence of sarcopenia in patients with liver cirrhosis. After adjusting for the potential influencing factors, it was found that the correlation between age and sarcopenia was weakened (OR = 0.870, 95% CI 0.338–2.239). The current findings show that sarcopenia is common in patients with cirrhosis and is independently associated with age, physical activity, BMI, nutritional status, and albumin, and serum alkaline phosphatase and total cholesterol are associated with the development of sarcopenia. Regular exercise may help maintain the grip strength of patients with cirrhosis and delay the deterioration of liver function.
Similar content being viewed by others
Introduction
Sarcopenia is considered to be a progressive systemic skeletal muscle disorder associated with an increased likelihood of adverse outcomes such as falling down, bone fracture, physical disability, and death1. The 2016 World Health Organization International Classification of Diseases code for sarcopenia, ICD-10, has important clinical implications for the study of this disease2. With the widespread clinical recognition of muscle loss in chronic disease, aging-related muscle loss is considered “primary sarcopenia,” while "secondary sarcopenia" is sarcopenia occurring in chronic diseases3 such as advanced liver, heart, lung, and kidney diseases. Both primary and secondary sarcopenia are states of anabolic resistance or attenuated muscle response to nutrition and physical activity4. Among the various diseases related to secondary sarcopenia, the incidence of sarcopenia among patients with cirrhosis is high (20–70%)5, significantly higher than the rates observed in the general older people population (2.9–38.5%)6,7.
Studies have revealed sarcopenia is a significant predictor of mortality both before and after liver transplantation8. The causes of sarcopenia in liver cirrhosis (LC) are complex and multifactorial, encompassing factors such as inadequate energy intake, an accelerated starvation response, the liver-muscle axis, and systemic inflammation. Furthermore, sarcopenia is associated with an increased risk of infection, prolonged hospital stays, hepatic encephalopathy, poor quality of life, and increased healthcare costs among patients with cirrhosis8,9. Several studies have reported that exercise training and nutritional interventions can slow down the progression or even reverse muscle wasting, leading to improvements in physical function and frailty in patients with cirrhosis10. Several studies with small number of cases enrolled suggested that sarcopenia in liver cirrhotic patients might associated with the severity, etiology of liver disease, malnutrition, or alcohol intake11. However, the risk factors associated with sarcopenia in patients with liver cirrhosis has not been adequately assessed.
Therefore, this study aims to investigate the risk factors associated with sarcopenia in patients with liver cirrhosis, enabling the identification of high-risk groups and the development of early preventive interventions for sarcopenia in patients with cirrhosis.
Materials and methods
Study design
This study employed a case–control, observational, and descriptive exploratory design and followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines12.
Setting
Study participants were cirrhotic patients hospitalized in the Department of Infection and Gastroenterology at the Affiliated Hospital of Zunyi Medical University from July 2021 to July 2022. The Department of Infection serves approximately 500 patients with LC annually, while the Gastroenterology Department serves nearly 1000 such patients. The hospital is a tertiary teaching hospital and a leading medical center in the province.
Participants
Participants were recruited based on the following eligibility criteria, and all data for the eligibility screening were obtained from medical records in the hospital.
Inclusion criteria
-
Adult, age ≥ 18 years; and
-
Diagnosis of cirrhosis based on typical clinical presentation, laboratory tests, imaging features, and/or representative pathological findings from liver biopsies.
Exclusion criteria
-
Comorbidity with other serious systemic diseases or presence of other end-stage complications (e.g., chronic obstructive pulmonary disease, renal failure, heart failure, and other malignancies);
-
Pregnant or lactating women;
-
Diseases that may lead to impaired nutritional metabolism, including inflammatory bowel disease and thyroid disease; and.
-
Receiving treatments with glucocorticoids or immunosuppressive drugs.
The study was approved by the Medical Ethics Committee of the Affiliated Hospital of Zunyi Medical University (reference number: KLLY-2021-149). Written informed consent was obtained from all participants. All methods were carried out in accordance with relevant guidelines and regulations of the Affiliated Hospital of Zunyi Medical University Ethics Committee.
Variables and measurement
Outcome
Sarcopenia was assessed as a dichotomous variable. According to the Asian Working Group for Sarcopenia 2019 (AWGS 2019), the diagnostic indicators of sarcopenia include three aspects: SMI, muscle strength, and physical mobility). The diagnosis of sarcopenia is made when the first criterion, plus the second and/or third criteria, are met13.
SMI
CT images were analyzed by two independent radiologists using the Slice-O-matic V5.0 software. Muscle tissues on CT images were based on Hounsfield unit (HU) thresholds, ranging from -29 HU to + 150 HU14. Skeletal muscle area (SMA) was measured by scanning the third lumbar spine vertebra cross-section, and the L3-SMI was calculated as the ratio of SMA to squared height (cm2/m2). The cut-off point for low SMI was defined as SMI ≤ 52.4 cm2/m2 for men and SMI ≤ 38.5 cm2/m2 for women15.
Muscle strength
Hand grip strength (HGS) measurements were performed using an electronic hand grip strength device (EH 101, from Xiangshan, Guangdong, China) following the standardized grip strength measurement guidelines established by the American Manual Therapy Association16. Each participant was tested by maintaining a right angle (90°) to both hands, twice for both the right and left hands, using the average of the available maximum strength data. In cases where measuring one hand was not possible, the maximum value for the other hand was recorded. The cut-off point for low grip strength was defined as < 28 kg for men and < 18 kg for women13.
Physical mobility
The 6-m walk test was used17. Participants were instructed to walk at their usual walking speed for six meters. A gait speed of < 1.0 m/s was diagnosed as poor physical mobility13.
Risk factors
The demographic data included gender, age, ethnicity, marital status, nature of work, educational attainment, residential area, co-living status, smoking, drinking, physical activity (≥ 30 min/time), monthly income, and medical insurance status.
The clinical data included the etiology of cirrhosis, duration of cirrhosis, stage of cirrhosis, hospitalization, cirrhosis-related complications, comorbidities, and prognosis based on Child–Pugh classification.
The cirrhosis-related biochemical data included hemoglobin, clotting profile, lipid profile, and liver function. The anthropometric data included height, weight, body mass index (BMI), triceps skinfold thickness (TSF), mid-upper arm muscle circumference, and waist-to-hip ratio.
The nutrition status was measured using the Royal Free Hospital-Nutritional Prioritizing Tool (RFH-NPT), which considers factors such as alcoholic hepatitis, tube feeding, body fluid retention status, BMI, unplanned body mass loss, and dietary intake reduction18. The scores obtained were used to classify the nutritional risk levels, with 0 indicating low risk of malnutrition, 1 for moderate risk, and 2–7 for high risk. This tool enables the classification of the nutritional risk of patients into three levels within 3 min: low, medium, and high. At present, this tool has been widely used in assessing the nutritional risk of patients, with research indicating its superior effectiveness in patients with LC compared to most clinical nutritional evaluation tools18.
Confounding factors
Given the study aimed to identify risk factors, confounders could not be pre-identified without the risk factors known. This study considered only old age (i.e., age ≥ 60 years) and gender as confounders.
Assessments of sarcopenia risk
The assessment of sarcopenia in this study was performed according to the diagnostic criteria for sarcopenia recommended by the Asian Working Group on Sarcopenia (AWGS 2019), when patients had low muscle mass and the presence of low muscle strength and / or low physical performance (Table 1).
Study size
The sample size was calculated using the formula: N = 4 (\({\mathrm{U}}_{\mathrm{\alpha }}\) S/\(\updelta\))2, where U is the test level, \({\mathrm{U}}_{\mathrm{\alpha }}\) represents the \(\mathrm{\alpha }\) corresponding U value, S represents the standard deviation, δ represents the tolerance error, and \(\mathrm{\alpha }\)=0.05. In this study, a two-sided test was performed with U = 1.96 and δ = [0.25S, 0.5S]5. Considering the possible existence of invalid samples or data, the study increased the sample size by 20%. The calculated sample size range was approximately 75–296 cases, and 271 patients were finally included in this study.
Statistical analysis
Before any statistical comparison, the Kolmogorov–Smirnov test and homogeneity variance test were used to test the normality of standard normal distribution for all variables. In descriptive analysis, continuous variables were described with mean and standard deviation or median and interquartile range, whereas categorical variables were described using frequency and percentage. To indicate the association between independent risk factors and sarcopenia, the Student’s t-test was used for continuous variables, and the χ2 test was used for categorical variables.
The logistic regression model included the following covariates: age, physical activity, BMI, mid-upper arm muscle circumference, hepatic encephalopathy, nutritional status, alkaline phosphatase, albumin, and total cholesterol, and considered gender as a potential sarcopenia related factor. A three-step approach was employed to identify the risk factors associated with sarcopenia. First, risk factors for sarcopenia were evaluated and identified using simple regression analysis (i.e., Model 1). Second, adjusted binary regression was performed using a stepwise method. Three models were used to illustrate the association between these risk factors and sarcopenia: Model 1 represents the unadjusted model, Model 2 incorporates all significant risk factors identified using the stepwise method, and Model 3 represents the model adjusted to known confounding factors.
All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 18.0, and all statistical tests were two-sided, with differences considered statistically significant at p < 0.05.
Institutional review board statement
This study protocol was approved by the Ethics Committee of the Affiliated Hospital of Zunyi Medical University on December 31, 2021, with the approval number: (KLLY-2021-149).
Informed consent statement
Informed consent was obtained from all subjects involved in the study.
Results
Participants
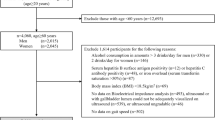
A total of 482 hospitalized patients with LC initially met the inclusion criteria for the study and were selected for qualification screening. However, 201 of these patients met the exclusion criteria and were not eligible to participate. Of the eligible 281 cirrhotic patients, 10 of them were withdrawn due to physical discomfort during the screening process. Finally, 271 participants completed the study (Fig. 1).
Descriptive data
The number of participants with sarcopenia was 75 (27.7%). Notably, 27.3% (50/183) of male participants and 28.4% (25/88) of female participants had sarcopenia (p = 0.851). The prevalence of sarcopenia increased with age, with rates of 24.6% for those under 60 years old and 38.3% for those aged 60 or older. The prevalence of sarcopenia was 38.9% (28/72) in alcohol drinkers compared to 23.6% (47/199) in non-drinkers (p = 0.013). The prevalence of sarcopenia was related to exercise status: 36.4% and 16.7% for < 3 times/week and ≥ 3 times/week, respectively (p < 0.001) (Table 2).
Outcome data
Compared with participants without sarcopenia, subjects with combined sarcopenia had higher hospital costs, longer hospitalization periods (p < 0.001), and were more likely to develop spontaneous bacterial peritonitis, hepatic encephalopathy, ascites, and electrolyte disturbances (p < 0.05). Furthermore, the severity of liver function was strongly associated with the development of sarcopenia (p = 0.001) (Table 3).
The median hand grip strength was 22.8 kg for participants with sarcopenia and 28.9 kg for those without sarcopenia. Participants with sarcopenia had lower L3-SMI, L3-SMA, gait speed, total cholesterol, albumin, weight, BMI, and mid-arm muscle circumference than those without comorbidities (p < 0.001). Additionally, participants with sarcopenia had higher total bilirubin than those without sarcopenia (p < 0.001) (Tables 4&5). Participants with sarcopenia had lower hemoglobin, triglycerides, high-density lipoprotein, and TSF than those without comorbid sarcopenia (p < 0.05). Furthermore, participants with sarcopenia had higher gamma-glutamyl transferase and alkaline phosphatase than those without sarcopenia (p < 0.05). The incidence of sarcopenia in cirrhotic patients with high malnutrition risk was higher than that in patients with low-medium malnutrition (p < 0.05) (Table 5).
Outcome data
The binary ordered regression with sarcopenia as the dependent variable revealed several significant associations. In the adjusted model for the associated risk factors for sarcopenia (Model 2), the prevalence of sarcopenia increased with decreasing physical activity frequency (OR 2.498; 95% CI 1.063–5.874). High malnutrition risk was also linked to a higher prevalence of sarcopenia (OR 2.579; 95% CI 1.127–5.898), as was hepatic encephalopathy (OR 3.658; 95% CI 1.539–8.694). Age (OR 2.688; 95% CI 1.012–7.137) and high ALP levels (OR 1.007; 95% CI 1.003–1.011) were associated with a high risk of sarcopenia. In contrast, BMI (OR 0.663; 95% CI 0.551–0.799), MAMC (OR 0.833; 95% CI 0.716–0.969), albumin (OR 0.831; 95% CI 0.762–0.907), and total cholesterol (OR 0.389; 95% CI 0.230–0.659) were negatively correlated with sarcopenia risk. After further adjustment for gender in Model 3, the association between age and risk of sarcopenia was reduced (OR 2.631; 95% CI 0.981–7.058) (Table 6).
Discussion
In this study, hepatitis B infection was identified as the leading cause of cirrhosis, while alcoholic hepatitis was a common disease abroad. The prevalence of sarcopenia was higher in patients with cirrhosis (27.68%). In Model 1, the risk of sarcopenia was positively associated with age, physical activity < 3 times/week, high risk of malnutrition, hepatic encephalopathy, and high ALP levels. Conversely, it was negatively associated with high BMI, MAMC, albumin, and total cholesterol. After adjusting for gender in Model 3, the association between age and the risk of sarcopenia was attenuated. In addition, patients with advanced liver disease had a higher likelihood of developing sarcopenia.
The prevalence of sarcopenia in patients with cirrhosis remains a subject of debate. A study that included 201 subjects with cirrhosis reported a prevalence of sarcopenia 57.2%, with no significant difference between males and females19. Kim et al. found that the complication rate of sarcopenia in patients with LC was 30%–70%, with a higher prevalence among males20. In the present study, there was no statistical difference in the prevalence of sarcopenia between males and females. This disparity in findings may be attributed to the differences in racial characteristics, body size, and disease etiology between individuals from Asian and Western countries. Notably, the prevalence of sarcopenia has been reported as 10% for Child–Pugh A, 34% for Child–Pugh B, and 54% for Child–Pugh C21, similar to the results of the present study, suggesting that muscle mass loss in cirrhotic patients is more pronounced as the liver reserve deteriorates.
The present study made extensive efforts to account for potential confounding variables and identified aging as a significant risk factor for developing sarcopenia. However, this association was attenuated after adjusting for gender. This attenuation may be due to the small sample size of patients in the study. Research has shown that there can be a substantial loss of skeletal muscle mass, estimated at 20–30%, from ages 20 to 8022. Muscle strength begins to decline around the age of 30 and declines rapidly around the age of 50 years23. These age-related changes are characterized by motor unit remodeling, increased muscle fiber denervation, reduced protein synthesis, and a decrease in the number of muscle satellite cells required for skeletal muscle growth and repair6, ultimately leading to a decrease in muscle fiber cross-sectional area. Therefore, both the AWGS 2019 and the European Working Group on Sarcopenia in Older People 2 (EWGSOP 2) recommend early screening and intervention for sarcopenia in older adults to alleviate the burden of this condition in a high-risk population1,13.
Cirrhosis is usually associated with protein-energy malnutrition and low physical activity, leading to sarcopenia, with the prevalence of protein malnutrition ranging from 20 to 30% in patients with chronic liver disease (CLD) to over 60% in patients with cirrhosis24. Sarcopenia, characterized by decreased muscle/fat mass, increased pro-inflammatory cytokines, and anorexia, can potentially be mitigated with nutritional supplements, potentially slowing its progression to sarcopenia25. In the present study, a high risk of malnutrition (OR 2.579; 95% CI, 1.127–5.898) was associated with an increased risk of sarcopenia in cirrhotic patients with physical activity < 3 times/week (OR 2.498; 95% CI, 1.063–5.874). High ALP levels were also associated with the development of sarcopenia in cirrhotic patients. Lee et al.26 explored the relationship between serum ALP levels and low muscle mass index in 15,579 adults in Korea, and the findings suggested that serum ALP may serve as a marker of inflammation and a predictor of sarcopenia. Further research is needed to confirm whether ALP can predict sarcopenia development in cirrhosis patients. Serum albumin levels have been recognized as an important factor associated with decreased muscle size and strength27. Montano et al.28 also confirmed that decreased albumin levels were independently associated with a higher risk of sarcopenia and a poor prognosis. In the present study, albumin levels were significantly associated with the risk of sarcopenia in patients with cirrhosis. Regression analysis showed that normal total cholesterol levels were associated with the development of sarcopenia in cirrhotic patients. Previous studies have reported that obesity due to abnormal total cholesterol levels is a significant risk factor for the development of sarcopenia in cirrhotic patients29.
BMI is an indicator to assess the nutritional status of the body. A low BMI typically indicates low body fat. Several studies have confirmed that L3-SMI is positively correlated with BMI30,31. In our study, the median BMI among participants with sarcopenia was 22.8 kg/m2, consistent with the findings of Landi32, who found that older people with a BMI greater than 21 kg/m2 had 0.76 times the risk of sarcopenia compared to those with a BMI less than 21 kg/m2. MAMC is strongly associated with lean muscle mass and body fat, has good intra- and inter-observer reproducibility, and has been shown to predict mortality33,34. While muscle mass is crucial, muscle strength is a more significant factor in determining physical function35. HGS has proven to be a better predictor of poor clinical outcomes than CT measurements of muscle mass and the Model for End-Stage Liver Disease. Even small improvements in HGS, as little as 1 kg, suggest a significant reduction in mortality36,37. Early identification of sarcopenia through routine imaging, convenient assessment tools, and clinical observation is an integral part of the care of patients with cirrhosis. Considering that screening tests need to be of high sensitivity, we recommend the combination of MAMC and grip strength as an initial screening test for sarcopenia rather than SARC-F in patients with CLD. SARC-F has demonstrated low sensitivity (15%–45%) in patients with CLD38, limiting its clinical application. Early detection of sarcopenia facilitates timely referral for confirmation of the diagnosis and implementation of primary prevention measures in high-risk populations.
This study confirms that hepatic encephalopathy is an independent risk factor for the development of sarcopenia. Hyperammonemia has been shown to increase muscle growth inhibitor expression through toll-like receptor—independent activation of nuclear factor kappa β in animal models39, increasing the risk of developing sarcopenia in patients with cirrhosis. Furthermore, Nardelli et al.40 reported an association between the development of sarcopenia in patients with cirrhosis and the development of hepatic encephalopathy. Several studies have reported that branched-chain amino acids (BCAA) are beneficial in the treatment of hepatic encephalopathy41. For cirrhotic patients with protein intolerance or inability to meet protein targets, guidelines recommend a BCAA intake of 0.25 g·kg−1d−142. However, there is a paucity of research on the potential of BCAA in ameliorating sarcopenia.
The current study has several limitations. First, this is a case–control study conducted in a local hospital in China, which could potentially limit the generalizability of the findings. Second, there was no healthy control group to serve as a reference for comparing the prevalence of sarcopenia; therefore, only indirect comparisons could be made. Third, the sample size was relatively small, and there may be inherent bias among cases. In future research, we plan to address these limitations by including a larger cohort of cirrhotic patients and conducting follow-up assessments to enhance the study's reliability and generalizability.
Conclusions
In conclusion, this study found a higher prevalence of sarcopenia in patients with cirrhosis. Advanced age, low physical activity, low BMI, decreased MAMC, hepatic encephalopathy, and nutritional status were associated with an increased risk of sarcopenia, whereas liver function-related indices such as ALP, albumin, and total cholesterol levels were associated with an increased risk of sarcopenia. These findings suggest that promoting physical activity in cirrhotic patients, with a focus on reducing body fat and enhancing cognitive function, plays a crucial role in preventing sarcopenia.
Data availability
Data associated with this study can be obtained by reasonable request to the corresponding author (P.Y.).
References
Cruz-Jentoft, A. J. et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 48(4), 601 (2019).
Anker, S. D., Morley, J. E. & von Haehling, S. Welcome to the ICD-10 code for sarcopenia. J. Cachexia Sarcopenia Muscle 7(5), 512–514 (2016).
Cruz-Jentoft, A. J. et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39(4), 412–423 (2010).
Bellar, A., Welch, N. & Dasarathy, S. Exercise and physical activity in cirrhosis: opportunities or perils. J. Appl. Physiol. 128(6), 1547–1567 (2020).
Ponziani, F. R. & Gasbarrini, A. Sarcopenia in patients with advanced liver disease. Curr. Protein Pept. Sci. 19(7), 681–691 (2018).
Wang, J. et al. Prevalence and associated factors of possible sarcopenia and sarcopenia: Findings from a Chinese community-dwelling old adults cross-sectional study. BMC Geriatr. 22(1), 592 (2022).
Wu, X. et al. Sarcopenia prevalence and associated factors among older Chinese population: Findings from the China Health and Retirement Longitudinal Study. PLoS One 16(3), e247617 (2021).
Saiman, Y. & Serper, M. Frailty and sarcopenia in patients pre- and post-liver transplant. Clin. Liver Dis. 25(1), 35–51 (2021).
van Vugt, J. et al. Low skeletal muscle mass is associated with increased hospital costs in patients with cirrhosis listed for liver transplantation-a retrospective study. Transpl. Int. 31(2), 165–174 (2018).
Williams, F. R. et al. Review article: Impact of exercise on physical frailty in patients with chronic liver disease. Aliment Pharmacol. Ther. 50(9), 988–1000 (2019).
Jeong, J. Y. et al. Presence of sarcopenia and its rate of change are independently associated with long-term mortality in patients with liver cirrhosis. J. Korean Med. Sci. 33(50), e299 (2018).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 12(12), 1495–1499 (2014).
Chen, L. K. et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 21(3), 300–307 (2020).
Mitsiopoulos, N. et al. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J. Appl. Physiol. 85(1), 115–122 (1998).
Prado, C. M. et al. Assessment of nutritional status in cancer–the relationship between body composition and pharmacokinetics. Anticancer Agents Med. Chem. 13(8), 1197–1203 (2013).
Shechtman, O., Gestewitz, L. & Kimble, C. Reliability and validity of the DynEx dynamometer. J. Hand Ther. 18(3), 339–347 (2005).
Anton, S. D. et al. Successful aging: Advancing the science of physical independence in older adults. Ageing Res. Rev. 24(Pt B), 304–327 (2015).
Wu, Y. et al. Royal free hospital-nutritional prioritizing tool improves the prediction of malnutrition risk outcomes in liver cirrhosis patients compared with Nutritional Risk Screening 2002. Br. J. Nutr. 124(12), 1293–1302 (2020).
Topan, M. M. et al. Impact of sarcopenia on survival and clinical outcomes in patients with liver cirrhosis. Front. Nutr. 8, 766451 (2021).
Kim, G. et al. Prognostic value of sarcopenia in patients with liver cirrhosis: A systematic review and meta-analysis. PLoS One 12(10), e186990 (2017).
Tandon, P. et al. Severe muscle depletion in patients on the liver transplant wait list: Its prevalence and independent prognostic value. Liver Transpl. 18(10), 1209–1216 (2012).
Carmeli, E., Coleman, R. & Reznick, A. Z. The biochemistry of aging muscle. Exp. Gerontol. 37(4), 477–489 (2002).
Dodds, R. M. et al. Grip strength across the life course: Normative data from twelve British studies. PLoS One 9(12), e113637 (2014).
Abdelbasset, W. K. et al. Prevalence and nonpharmacological interventions for sarcopenia among cirrhotic patients. Dis. Markers 2021, 8866093 (2021).
Duarte-Rojo, A. et al. Exercise and physical activity for patients with end-stage liver disease: Improving functional status and sarcopenia while on the transplant waiting list. Liver Transpl. 24(1), 122–139 (2018).
Lee, J. H., Cho, A. R. & Lee, Y. J. Relationship between serum alkaline phosphatase and low muscle mass index among Korean adults: A nationwide population-based study. Biomolecules 11(6), 842 (2021).
Hiraoka, A. et al. Relative changes in handgrip strength and skeletal muscle volume in patients with chronic liver disease over a 2-year observation period. Hepatol. Res. 48(7), 502–508 (2018).
Montano-Loza, A. J. et al. Inclusion of sarcopenia within MELD (MELD-Sarcopenia) and the prediction of mortality in patients with cirrhosis. Clin. Transl. Gastroenterol. 6(7), e102 (2015).
Hida, T. et al. Sarcopenia and physical function are associated with inflammation and arteriosclerosis in community-dwelling people: The Yakumo study. Mod. Rheumatol. 28(2), 345–350 (2018).
Ebadi, M. et al. Sarcopenia severity based on computed tomography image analysis in patients with cirrhosis. Nutrients 12(11), 3463 (2020).
Ohashi, K. et al. Relationship between sarcopenia and both physical activity and lifestyle in patients with chronic liver disease. J. Clin. Med. Res. 10(12), 920–927 (2018).
Landi, F. et al. Prevalence and risk factors of sarcopenia among nursing home older residents. J. Gerontol. A Biol. Sci. Med. Sci. 67(1), 48–55 (2012).
Buchard, B. et al. Assessment of malnutrition, sarcopenia and frailty in patients with cirrhosis: Which tools should we use in clinical practice?. Nutrients 12(1), 186 (2020).
Hu, F. J. et al. Mid-upper arm circumference as an alternative screening instrument to appendicular skeletal muscle mass index for diagnosing sarcopenia. Clin. Interv. Aging 16, 1095–1104 (2021).
Nishikawa, H. et al. Sarcopenia and frailty in liver cirrhosis. Life (Basel) 11(5), 339 (2021).
Carey, E. J. et al. A North American expert opinion statement on sarcopenia in liver transplantation. Hepatology 70(5), 1816–1829 (2019).
Plauth, M. et al. ESPEN guideline on clinical nutrition in liver disease. Clin. Nutr. 38(2), 485–521 (2019).
Hanai, T. et al. Utility of the SARC-F questionnaire for sarcopenia screening in patients with chronic liver disease: A multicenter cross-sectional study in Japan. J. Clin. Med. 10(15), 3448 (2021).
Qiu, J. et al. Hyperammonemia in cirrhosis induces transcriptional regulation of myostatin by an NF-kappaB-mediated mechanism. Proc. Natl. Acad. Sci. U. S. A. 110(45), 18162–18167 (2013).
Nardelli, S. et al. Muscle alterations are associated with minimal and overt hepatic encephalopathy in patients with liver cirrhosis. Hepatology 70(5), 1704–1713 (2019).
Gluud, L. L. et al. Branched-chain amino acids for people with hepatic encephalopathy. Cochrane Database Syst. Rev. 5(5), D1939 (2017).
EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J. Hepatol. 70(1), 172–193 (2019).
Acknowledgements
Thank all the patients with liver cirrhosis who participated in this study for cooperating with the questionnaire survey and body index measurement, and thank all the medical staff in the Department of Gastroenterology for their support for this study.
Funding
This work was supported by a project funded by the Guizhou Provincial Science and Technology Department Fund (Qiankehe Support [2021] General 049).
Author information
Authors and Affiliations
Contributions
L.Y.X. and M.D. were resposible for the formal analysis, manuscript editing; F.Z. was resposible for the literature research, manuscript editing; Y.S.S. was resposible for the data acquisition & Investigation; R.Y.C.K. was resposible for the study concepts & design; J.T.S. was resposible for critical revision of the manuscript for important intellectual content; Y.W.L. was resposible for the manuscript preparation; Q.L. was resposible for the definition of intellectual content; Y.P. and L.Z. were resposible for the guarantor of integrity of the entire study, study concepts & design, manuscript review. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xiao, L., Dai, M., Zhao, F. et al. Assessing the risk factors associated with sarcopenia in patients with liver cirrhosis: a case–control study. Sci Rep 13, 21845 (2023). https://doi.org/10.1038/s41598-023-48955-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48955-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.