Abstract
Here we report the results of a study on the association between drug delivery via intravenous route or intraosseous route in out-of-hospital cardiac arrest. Intraosseous drug delivery is considered an alternative option in resuscitation if intravenous access is difficult or impossible. Intraosseous uptake of drugs may, however, be compromised. We have performed a retrospective cohort study of all Danish patients with out-of-hospital cardiac arrest in the years 2016–2020 to investigate whether mortality is associated with the route of drug delivery. Outcome was 30-day mortality, death at the scene, no prehospital return of spontaneous circulation, and 7- and 90-days mortality. 17,250 patients had out-of-hospital cardiac arrest. 6243 patients received no treatment and were excluded. 1908 patients had sustained return of spontaneous circulation before access to the vascular bed was obtained. 2061 patients were unidentified, and 286 cases were erroneously registered. Thus, this report consist of results from 6752 patients. Drug delivery by intraosseous route is associated with increased OR of: No spontaneous circulation at any time (OR 1.51), Death at 7 days (OR 1.94), 30 days (2.02), and 90 days (OR 2.29). Intraosseous drug delivery in out-of-hospital cardiac arrest is associated with overall poorer outcomes than intravenous drug delivery.
Similar content being viewed by others
Introduction
Out-of-hospital cardiac arrest (OHCA) is a general healthcare issue with a high mortality rate and a large burden for healthcare organisations1. In Denmark, up to 5000 people suffer from OHCA each year2 and 14% survive for 30 days. Treatment of OHCA consists of a time-critical sequence of interventions3. Advanced life support includes adrenaline for patients with pulseless electric activity (PEA) or asystole and amiodarone combined with adrenaline for patients with shock-refractory ventricular fibrillation or pulseless ventricular tachycardia4,5,6,7,8. When choosing the route of administration for these drugs, the prehospital clinician has several options4 including intraosseous or intravenous access.
Current resuscitation guidelines recommend the use of intravenous access as the first choice when vascular access is required during cardiopulmonary resuscitation (CPR)4,9,10. The same guidelines encourage the resuscitation provider to consider intraosseous access if attempts at intravenous access are unsuccessful or intravenous access is not feasible4. Establishing intravenous access can be challenging in OHCA because of the compromised circulation, the difficult work conditions in the out-of-hospital setting, and the urgency of the procedure. Intraosseous access provides fast access to the circulatory system and has a high success rate11,12,13,14. Previous studies have indicated poorer outcomes for patients treated with intraosseous access when compared to an intravenous access15,16,17,18,19,20. In a randomized study, Daya et al.19 investigated patients who were randomised to lidocaine, amiodarone, or placebo and found that the point estimates for the effects of both drugs in comparison with placebo were significantly greater for the intravenous than for the intraosseous. Until now, no consensus has been established on whether intraosseous access equates to intravenous access.
In this retrospective study we compare the outcomes of patients with OHCA treated via an intraosseous access with patients with OHCA treated through an intravenous access. The outcomes are: 30-day mortality, no prehospital return of spontaneous circulation, patient pronounced dead at the scene, 7-day mortality, and 90-day mortality.
Methods
System setting
Denmark has a population of approximately 5.8 million people. The emergency medical system is a tax-funded three-tiered system providing services without direct costs to the patient21. For simple emergencies, an ambulance manned with emergency medical technicians (EMT) and/or paramedics is dispatched. In more complicated cases, for example, OHCA, both an ambulance and a rapid response vehicle with a paramedic or a Mobile Emergency Care Unit manned by a specialist in anaesthesiology22 are dispatched to the site. In cases where the site of emergency is in a remote area, the Helicopter Emergency Medical Service may be dispatched23. During and immediately after the treatment of a patient, the attending EMT, paramedic, and the prehospital anaesthesiologist all register the findings and the treatment administered in the nationwide prehospital medical records22.
Design and data sources
In this retrospective cohort study, we used data from two national healthcare registers and national prehospital medical records22. Data regarding all Danish OHCA patients from January 1, 2016, to December 31, 2020, were collected from The Danish Cardiac Arrest Registry2,24. Subsequently, general health data were collected using the unique patient identifier the Danish Civil Personal register number assigned to all Danish residents25.
The following variables were collected from The Danish Cardiac Arrest Registry:
Age, sex, date of the OHCA, information whether the OHCA was witnessed by bystanders or not, the provision of basic life support initiated before the arrival of an ambulance, the provision of defibrillation by a bystander, the provision of defibrillation by ambulance personnel, the first observed cardiac rhythm (dichotomised as shockable or non-shockable), the patient´s status at arrival to hospital (stratified into four groups: resuscitation terminated, ongoing resuscitation, unconscious patient with spontaneous circulation or conscious patient with spontaneous circulation) and response time of the first prehospital vehicle.
We collected information on pharmacological access route for drugs (intraosseous or intravenous) from the national prehospital medical record system22. This information was gathered from formalised registration boxes in which the prehospital provider ticks the route of administration of drugs (i.e., intravenous administration, intraosseous administration). Furthermore, all text fields were scrutinized for written indications of the use of an intraosseous access (i.e., words containing "intraosseous", "osseous", the abbreviation "IO)".
The Danish Civil Registration System provided information on dates of death25. No distinctions were made regarding the causes of death.
Outcomes
Five parameters were included in the analysis. The primary outcome was “30-day mortality (I)”. The secondary outcomes were “No ROSC at any point during treatment” (II), “Death at the scene (III)”, “7-day mortality (IV)”, and “90-day mortality (V)”.
Statistical analysis
The predictor variables were compared in the two groups using a Pearson’s chi-squared test for categorical variables and either a Wilcoxon rank-sum or student t-test for continuous variables. The associations between intraosseous access or intravenous access and the outcomes were calculated using logistic regression. Both crude and adjusted analyses were conducted. All analyses used clustered robust standard errors to consider that the same person may be included multiple times. The adjusted analysis included factors known to impact the outcome variables. The analyses were adjusted for age, sex, witnessed OHCA or not, basic life support provided before ambulance arrival, bystander defibrillation, defibrillation administered by ambulance personnel, ambulance response time, and shockable/non-shockable rhythm26. A 5% significance level was applied. Results are presented as Odds-Ratios (OR). Data management and analyses were performed using Stata 16 (Stata Corp LP, College Station, Texas, USA).
Ethical approvals
All research was performed in accordance with relevant guidelines and regulations. The project was approved by the Danish Patient Safety Authorities (Ref. No. 31-1521-434). According to the Act on Processing of Personal Data, in register-based studies approved by the Danish Patient Safety Authorities, no consent for the use of data already deposited in the registry is required. No further approvals are necessary according to Danish law and accordingly, the requirement for informed consent was waived27. In addition to the necessary approvals being obtained, all data handling was carried out respecting the Danish and European legislation concerning person-identifiable data28,29.
Results
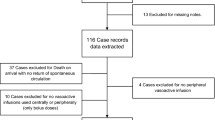
In total, 17,250 cardiac arrest patients were included in the study. As illustrated in Fig. 1, 6243 patients were declared dead at the scene without treatment by the attending prehospital anaesthesiologist. 1908 patients had return of spontaneous circulation (for example as a result of the defibrillation) before an access to the vascular bed was procured. In 2061 cases, no reliable personal identification was obtained, and 286 cases were excluded because of incomplete data. Overall, 6752 patients were included in the statistical analysis. Of these, 773 (11.4%) received an intraosseous access, and 5979 (88.6%) received an intravenous access. The latter group of patients were on average 3 years older (70 years) than patients in the intraosseous access group (67 years) (p < 0.001, Student´s t-test). The intravenous access group contained significantly more patients with a shockable rhythm as the first observed rhythm compared with the intraosseous access group (20.7% vs. 14.5%, p < 0.001, Pearson´s Chi2 test).
Our primary outcome, 30-day mortality, was 90.5% for all patients included in the study. 30-day mortality were higher in the intraosseous access group than in the intravenous access group (95.3% vs. 89.9%, p < 0.001, Pearson´s Chi2 test). Patients in the intraosseous access group were less prone to achieve ROSC than patients in the intravenous access group (No-ROSC: 72.1% vs. 62.4%, p < 0.001, Pearson´s Chi2 test). Significantly more patients in the intraosseous group were declared dead at the scene following EMS treatment than in the intravenous access group (83.4% vs. 80.6%, p < 0.001, Pearson´s Chi2 test). The 7-day mortality was higher in the intraosseous access group than in the intravenous access group (93.8% vs. 87.1%, p < 0.001, Pearson´s Chi2 test). 90-day mortality was higher in the intraosseous group than the intravenous access group (96.1% vs. 90.4%, p < 0.001, Pearson´s Chi2 test). See Table 1 for details.
Adjusted analyses
The outcome variables were analysed with independent variables that are known predictors for survival of OHCA26. Apart from the variable “Dead at the scene” which did not differ when adjusted for confounders, for all variables, the use of an intraosseous access to the vascular bed was associated with poorer outcomes than the use of an intravenous access with a crude OR of being dead at 30 days of 2.28 (95% CI 1.62; 3.22) and an adjusted OR of 2.02 (95% CI 1.34; 3.05). For crude and adjusted OR for the outcome variables “Dead at the scene”, “No return of spontaneous circulation”, “Dead at the scene”, “7-day mortality”, and “90-day mortality”, see Table 2.
Discussion
In this retrospective, observational study comparing intraosseous versus intravenous access in OHCA the main findings were: (1) a significant increase in mortality following OHCA in patients treated with drug delivery through an intraosseous access than in patients treated through an intravenous access, (2) a more than two-fold increased odds ratio of dying within 30 days following an OHCA when treated via an intraosseous access compared with treatment via an intravenous access.
The current guideline on resuscitation suggests that the same drug doses are used regardless of the administration site being an intravenous access or an intraosseous access4,10. The effect of amiodarone and adrenaline used in treatment of OHCA has been described in previous studies30,31,32. Although adrenaline is considered to increase the likelihood of achieving ROSC and may lead to improved overall survival, it is still uncertain if the increased number of patients with ROSC comes at a cost of an increase in the number of patients with neurological injury5,31,33,34,35. As most of the studies on the subject have not investigated the administration site, it is less certain what the effects are when the drugs are administered intraosseously. Despite the low evidence on the subject, intraosseous access is frequently used in the acute setting, as it provides fast, non-collapsible access to the venous plexus in the bone marrow, with a higher first-attempt success rate than intravenous access14,36. A randomised controlled trial (RCT) investigated administration of amiodarone, adrenaline, and placebo, via intravenous or intraosseous access in OHCA using neurological outcome and survival as outcomes. Overall, neither amiodarone nor lidocaine resulted in a significantly higher rate of survival or favourable neurologic outcome15. The study did not address the site of administration. However, a sub-analysis of the results revealed that point estimates for the effects of both drugs compared to placebo were greater for the intravenous than intraosseous route across all outcomes and beneficial only for intravenous19. Further, a recent retrospective study from Germany including 212, 228 OHCA patients over 31 years also found an association between poorer clinical effect of intraosseous adrenaline in OHCA20. All these studies support our findings that intraosseous access compared with intravenous access might be associated with a higher OR of mortality, not all studies have shown the drug administration route to be relevant in OHCA. One retrospective study investigated the first access site attempted. Based on the outcome ROSC at hospital arrival, the authors reported that a first intraosseous access approach was non-inferior to a first intravenous approach37. A common trait in these studies is the potential for confounding by indication. Intuitively, the intravenous access to the vascular bed is the primary target for gaining access to the vascular bed. There are undoubtedly cases in which the prehospital clinician only resort to an intraosseous access once intravenous access has proven impossible. Indeed, the figures found in our study (773 patients with an intraosseous access and 5979 patients with an intravenous access), it should be obvious that the first attempt to gain access to the vascular bed most often is an intravenous access. This may result in “resuscitation time bias” as the intraosseous access group may, inherently, have had a delay in drug administration resulting in time spent trying to insert an intravenous access before resorting to intraosseous access38.
As these studies are based on retrospective analyses, there is no possibility to adjust for this potential confounding effect. There is only limited knowledge on the effect of administration site and the outcomes “survival” or “favourable neurological outcome”. Reports from several clinical studies vary with findings of both similar outcomes regardless of access route39,40,41 and differing outcomes16,17,18,19,42,43 when comparing intraosseous drug delivery and intravenous drug delivery in OHCA patients.
Animal studies comparing intravenous and intraosseous administration of amiodarone in cardiac arrest have produced conflicting results regarding both clinical outcomes and pharmacokinetic outcomes, for example time to peak concentrations (\({T}_{max}\))44. One animal study suggested that a higher dose of intraosseous adrenaline might be needed to generate coronary perfusion pressure values similar to what could be achieved using standard doses intravenously during resuscitation in prolonged ventricular fibrillation45. Other studies comparing intraosseous and intravenous administration of drugs in porcine models have reported a difference in peak serum concentration (\({C}_{\mathrm{max}}\)) values; intraosseous adrenaline not reaching concentrations equalling the concentrations obtained in intravenous treatment46,47. If the described findings concerning mechanisms of action are transferable from animals to humans, this could explain our findings of an association of a poorer outcome following resuscitation with drugs administered intraosseously, as the concentration of the drugs given through an intraosseous access might be too low to achieve the same effect as when given through an intravenous access.
The main limitation of our study is the risk of confounding by indication. To some clinicians intraosseous access may be considered an emergency procedure to revert to only after intravenous access fails. Insertion of an intraosseous cannula may be caused by the clinician´s inability to insert an intravenous access. One or more failed attempts to place an intravenous access before reverting to an intraosseous access may thus cause a delay in the medical treatment. The mere presence of an intraosseous access may even reflect the possibility that access to the vascular bed may have taken priority and maybe even delayed basic life support, such as chest compression and/or rescue breaths. This phenomenon, called resuscitation time bias may limit our conclusions38.
On the other hand, there is a notion among Danish clinicians that in cases where the rapid response vehicle with only one paramedic is first at the scene, the intraosseous access is widely used as it is easier and faster than attempts at establishing an intravenous access48. As our study is a register-based study, we have no possibility to adjust for these potential confounders and we have no data allowing us to discriminate between patients in whom the intraosseous access was the first choice and patients that had an intraosseous access placed after a failed intravenous attempt.
Although other retrospective studies have the same limitations in interpreting the results, our findings of a poorer outcome being associated with intraosseous access are supported by previous studies, which indicate a poorer outcome for patients treated through an intraosseous access16,17,18,19,40,42,43.
One limitation of this study is that the group of patients having intravenous access placed during their treatment was significantly younger and to a larger extent had shockable rhythm. However, we adjusted for these two variables in our analysis of Odds-Ratios. Another apparent limitation of this study is the large number of patients excluded from analysis despite initial inclusion into the Danish National Cardiac Arrest Registry2,24. 6243 patients were in effect dead but had been subjected to resuscitation attempts by lay persons. As the criterion defining a patient´s eligibility for being registered in the registry is “any basic life support administered prehospitally”, these patients were registered in the Danish National Cardiac Arrest Registry. They were, however, declared dead at the arrival of the prehospital physician and no treatment was thus initiated. 1908 patients had return of spontaneous circulation following defibrillation before any vascular access had been attempted. These patients were excluded from the analysis. In 2061 cases, the unique civil personal register number of the patient was not known at the time of registering the patient. These patients were lost to follow-up. In 286 cases, errors in registration, for example, a patient without a cardiac arrest being erroneously registered as dead, were apparent. These two latter groups, comprising 2367 patients, constitute the real limitation of the study.
Another limitation in the present study was that we could not differentiate between tibial intraosseous access or humeral intraosseous access or assess any use of a pressurised fluid bag when using intraosseous access. This could have influenced the efficiency of the drugs46,47,49,50.
Although our results should be interpreted with caution, our findings suggest that the survival of OHCA patients is associated with the method that the prehospital personnel uses to gain access to the vascular bed. Administration of drugs through intraosseous access is associated with poorer outcome in almost all the parameters that are usually reported in OHCA. It is possible that the clinical practice of applying intraosseous access should be reviewed.
Data availability
Anonymised data are available from the corresponding author on reasonable request.
References
Myat, A., Song, K. J. & Rea, T. Out-of-hospital cardiac arrest: current concepts. Lancet 391(10124), 970–979 (2018).
The Danish Cardiac Arrest Registry. Retrieved from 16, May 2023 https://hjertestopregister.dk/?page_id=428
Nolan, J., Soar, J. & Eikeland, H. The chain of survival. Resuscitation 71, 270–271 (2006).
Soar, J. et al. European resuscitation council guidelines 2021: Adult advanced life support. Resuscitation 161, 115–151 (2021).
Jacobs, I. G., Finn, J. C., Jelinek, G. A., Oxer, H. F. & Thompson, P. L. Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomised double-blind placebo-controlled trial. Resuscitation 82, 1138–1143 (2011).
Shao, H. & Li, C. S. Epinephrine in out-of-hospital cardiac arrest: Helpful or harmful?. Chin Med J. 130, 2112–2116 (2017).
Wissa, J. et al. Time to amiodarone administration and survival outcomes in refractory ventricular fibrillation. Emerg. Med. Australas. 33, 1088–1094 (2021).
Mujović, N., Dobrev, D., Marinković, M., Russo, V. & Potpara, T. S. The role of amiodarone in contemporary management of complex cardiac arrhythmias. Pharmacol. Res. 151, 104521 (2020).
Soar, J. et al. Adult advanced life support: 2020 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 156, A80–A119 (2020).
Panchal, A. R. et al. Part 3: Adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 142(16_suppl_2), S366–S468 (2020).
Greenstein, Y. Y., Koenig, S. J., Mayo, P. H. & Narasimhan, M. A serious adult intraosseous catheter complication and review of the literature. Crit. Care Med. 44, e904–e909 (2016).
Leidel, B. A. et al. Is the intraosseous access route fast and efficacious compared to conventional central venous catheterization in adult patients under resuscitation in the emergency department? A prospective observational pilot study. Patient Saf. Surg. 3, 24 (2009).
Fuchs, S. & LaCovey, D. A prehospital model of intraosseous infusion. Ann. Emerg. Med. 20, 371–374 (1991).
Reades, R., Studnek, J. R., Vandeventer, S. & Garrett, J. Intraosseous versus intravenous vascular access during out-of-hospital cardiac arrest: A randomized controlled trial. Ann. Emerg. Med. 58, 509–516 (2011).
Kudenchuk, P. J. et al. Amiodarone, lidocaine, or placebo in out-of-hospital cardiac arrest. N. Engl. J. Med. 374, 1711–1722 (2016).
Mody, P. et al. Intraosseous versus intravenous access in patients with out-of-hospital cardiac arrest: Insights from the resuscitation outcomes consortium continuous chest compression trial. Resuscitation 134, 69–75 (2019).
Kawano, T. et al. Intraosseous vascular access is associated with lower survival and neurologic recovery among patients with out-of-hospital cardiac arrest. Ann. Emerg. Med. 71, 588–596 (2018).
Feinstein, B. A., Stubbs, B. A., Rea, T. & Kudenchuk, P. J. Intraosseous compared to intravenous drug resuscitation in out-of-hospital cardiac arrest. Resuscitation 117, 91–96 (2017).
Daya, M. R. et al. Survival after intravenous versus intraosseous amiodarone, lidocaine, or placebo in out-of-hospital shock-refractory cardiac arrest. Circulation 141, 188–198 (2020).
Monaco, T. et al. Impact of the route of adrenaline administration in patients suffering from out-of-hospital cardiac arrest on 30-day survival with good neurological outcome (ETIVIO study). Scand. J. Trauma Resusc. Emerg. Med. 31, 14 (2023).
Mikkelsen, S. & Lassen, A. T. The Danish prehospital system. Eur. J. Emerg. Med. 27, 394–395 (2020).
Lindskou, T. A. et al. The Danish prehospital emergency healthcare system and research possibilities. Scand. J. Trauma Resusc. Emerg. Med. 27, 100 (2019).
Andersen, M. S. et al. Implementing a nationwide criteria-based emergency medical dispatch system: A register-based follow-up study. Scand. J. Trauma Resusc. Emerg. Med. 21, 53 (2013).
Jensen, T. W. et al. The national danish cardiac arrest registry for out-of-hospital cardiac arrest—A registry in transformation. Clin. Epidemiol. 14, 949–957 (2022).
Schmidt, M., Pedersen, L. & Sørensen, H. T. The Danish civil registration system as a tool in epidemiology. Eur. J. Epidemiol. 29, 541–549 (2014).
Sasson, C., Rogers, M. A. M., Dahl, J. & Kellermann, A. L. Predictors of survival from out-of-hospital cardiac arrest: A systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes 3, 63–81 (2010).
Thygesen, L. C., Daasnes, C., Thaulow, I. & Brønnum-Hansen, H. Introduction to Danish (nationwide) registers on health and social issues: Structure, access, legislation, and archiving. Scand. J. Public Health 39, 12–16 (2011).
Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation) (Text with EEA relevance) (OJ L 119 04.05.2016, p. 1, ELI. Retrieved from 12 June 2023 http://data.europa.eu/eli/reg/2016/679/oj).
The Ministry of Justice [Law on General Data Protection, supplemental to Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation), LOV nr 502 af 23/05/2018 ] In Danish. Retrieved from 12 June 2023 https://www.retsinformation.dk/eli/lta/2018/502.
Perkins, G. D. et al. A randomized trial of epinephrine in out-of-hospital cardiac arrest. N. Engl. J. Med. 379, 711–721 (2018).
Gough, C. J. R. & Nolan, J. P. The role of adrenaline in cardiopulmonary resuscitation. Crit. Care. 22, 139 (2018).
Riva, E. et al. Pharmacokinetics of amiodarone in man. J. Cardiovasc. Pharmacol. 4, 264–269 (1982).
Loomba, R. S., Nijhawan, K., Aggarwal, S. & Arora, R. R. Increased return of spontaneous circulation at the expense of neurologic outcomes: Is prehospital epinephrine for out-of-hospital cardiac arrest really worth it?. J. Crit. Care. 30, 1376–1381 (2015).
Perkins, G. D. et al. Adrenaline to improve survival in out-of-hospital cardiac arrest: The PARAMEDIC2 RCT. Health Technol. Assess. Winch. Engl. 25, 1–166 (2021).
Finn, J., Jacobs, I., Williams, T. A., Gates, S. & Perkins, G. D. Adrenaline and vasopressin for cardiac arrest. Cochrane Database Syst. Rev. 1, CD103179 (2019).
Tan, B. K. K. et al. Clinical evaluation of intravenous alone versus intravenous or intraosseous access for treatment of out-of-hospital cardiac arrest. Resuscitation 159, 129–136 (2021).
Clemency, B. et al. Intravenous vs. intraosseous access and return of spontaneous circulation during out of hospital cardiac arrest. Am. J. Emerg. Med. 35, 222–226 (2017).
Andersen, L. W., Grossestreuer, A. V. & Donnino, M. W. “Resuscitation time bias”-A unique challenge for observational cardiac arrest research. Resuscitation 125, 79–82 (2018).
Granfeldt, A. et al. Intravenous vs. intraosseous administration of drugs during cardiac arrest: A systematic review. Resuscitation 149, 150–157 (2020).
Baert, V. et al. Intraosseous versus peripheral intravenous access during out-of-hospital cardiac arrest: A comparison of 30-day survival and neurological outcome in the French national registry. Cardiovasc. Drugs Ther. 34, 189–197 (2020).
Hsieh, Y. L. et al. Intraosseous versus intravenous vascular access during cardiopulmonary resuscitation for out-of-hospital cardiac arrest: A systematic review and meta-analysis of observational studies. Scand. J. Trauma Resusc. Emerg. Med. 29, 44 (2021).
Morales-Cané, I., Valverde-León, M. D. R., Rodríguez-Borrego, M. A. & López-Soto, P. J. Intraosseous access in adults in cardiac arrest: A systematic review and meta-analysis. Emerg. Rev. Soc. Espanola Med. Emerg. 32, 49–56 (2020).
Zhang, Y. et al. Intravenous versus intraosseous adrenaline administration in out-of-hospital cardiac arrest: A retrospective cohort study. Resuscitation 149, 209–216 (2020).
Hampton, K. et al. The effects of tibial intraosseous versus intravenous amiodarone administration in a hypovolemic cardiac arrest procine model. Am. J. Disaster Med. 11, 253–260 (2016).
Mader, T. J., Coute, R. A., Kellogg, A. R. & Harris, J. L. Coronary perfusion pressure response to high-dose intraosseous versus standard-dose intravenous epinephrine administration after prolonged cardiac arrest. Open J. Emerg. Med. 2, 1–7 (2014).
Burgert, J. et al. Comparison of tibial intraosseous, sternal intraosseous, and intravenous routes of administration on pharmacokinetics of epinephrine during cardiac arrest: a pilot study. AANA J. 80, S6–S10 (2012).
Hoskins, S. L., Nascimento Do, P., Lima, R. M., Espana-Tenorio, J. M. & Kramer, G. C. Pharmacokinetics of intraosseous and central venous drug delivery during cardiopulmonary resuscitation. Resuscitation 83, 107–112 (2012).
Vallentin, M. F. et al. Effect of intravenous or intraosseous calcium vs saline on return of spontaneous circulation in adults with out-of-hospital cardiac arrest: A randomized clinical trial. JAMA 326, 2268–2276 (2021).
Dalsey, W. C. et al. Comparison of superior vena caval and inferior vena caval access using a radioisotope technique during normal perfusion and cardiopulmonary resuscitation. Ann. Emerg. Med. 13, 881–884 (1984).
Lee, K. J. et al. Performance comparison of intraosseous devices and setups for infusion of whole blood in a cadaveric swine bone model. Am. J. Emerg. Med. 54, 58–64 (2022).
Acknowledgements
This study was funded by the Danish Air Ambulance who had no role in planning, data collection, interpretation of data nor writing of this paper.
Author information
Authors and Affiliations
Contributions
F.N.N., H.P., L.M., J.S.K., A.C.B., and S.M. contributed to this manuscript with the idea and design of the study. F.N.N., S.B.-B., H.C.C., and S.M. contributed to this manuscript with acquisition of data. F.N.N., S.B.-B., H.C.C., and S.M. contributed to this manuscript with analysis of data. F.N.N., S.B.-B., H.P., S.M. drafted the first version of the manuscript. L.M., P.M.H., E.F.C., J.S.K., H.C.C., F.F., D.H.-B., U.V., A.C.B., and S.M. contributed to this manuscript with comprehensive revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nilsson, F.N., Bie-Bogh, S., Milling, L. et al. Association of intraosseous and intravenous access with patient outcome in out-of-hospital cardiac arrest. Sci Rep 13, 20796 (2023). https://doi.org/10.1038/s41598-023-48350-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48350-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.