Abstract
KRAS is involved in the stability and expression of PD-L1. We investigated the expression of circulating mRNA (cmRNA) of KRAS4A and KRAS4B and the possible impact on progression-free survival (PFS) of patients with metastatic lung adenocarcinoma treated with immunotherapy. Patients without driver mutations undergoing Pembrolizumab (P) or P plus chemotherapy (PC) were prospectively accrued for liquid biopsy analysis of KRAS4A, KRAS4B, and PD-L1 cmRNA. Both KRAS isoforms were also studied for association with PD-L1 cmRNA. Of 56 patients, 28 received P and 28 PC. Patients with high levels of both KRAS isoforms showed significantly better PFS. The median PFS for KRAS4A was 29 months (95% CI 22–29 months) and KRAS4B 24 months (95% CI 13–29 months), respectively. The median PFS of patients with low levels of both isoforms was 12 months (95% CI 6–15 months for KRAS4A and 95% CI 5–20 months for KRAS4B). High KRAS4A retained a significant positive association with PFS in the multivariate model. An exploratory analysis in treatment subgroups found a positive association between high KRAS4A and KRAS4B with PFS in patients treated with P. PD-L1 cmRNA was significantly higher in patients with high KRAS isoforms levels and this effect was pronounced for high KRAS4A carriers. KRAS4A deserves further investigation as a potential marker for defining patients who may benefit the most from immune checkpoint inhibitors therapy and improving personalized cancer immunotherapeutic strategies.
Similar content being viewed by others
Introduction
Immune checkpoint inhibitors (ICI) targeting either programmed cell death protein 1 (PD-1) or programmed cell death ligand 1 (PD-L1) have become routinely part of the clinical approach for the management of Non-Small Cell Lung Cancer (NSCLC)1. Factors that affect the choice of treatments in NSCLC that lack a driver mutation include the level of PD-L1 expression on cancer cells, the extent of the disease and the tumor's histological characteristics. Specifically, patients with metastatic NSCLC and PD-L1 expression ≥ 50% are typically offered monotherapy with the anti-PD-1 antibody Pembrolizumab. For patients with PD-L1 expression < 50%, the combination of platinum-doublet chemotherapy and Pembrolizumab is the standard1. These treatment strategies have significantly improved the overall management of metastatic NSCLC with the capability to induce long-term responses and prolonged survival times in settings often refractory to all other treatments. Unfortunately, a relevant portion of patients does not respond to these treatments and/or they do not gain meaningful improvements in survival times2. To break through the limits of clinical effects, it is critical to make a profound understanding of the underlying mechanisms of sensitivity to expand the benefit of immunotherapy2.
KRAS mutations occur in 20–40% of lung adenocarcinomas, a prevalence that is higher in Western than in Asian populations (26 vs. 11%) and higher in smokers than non-smokers (30 vs. 10%)3. Retrospective analyses in clinical trials of ICI in metastatic lung cancer patients described a possible association between KRAS mutations and improved clinical outcomes3. In fact, the activity of Kras along the receptor tyrosine kinase (RTK)-Ras-MAPK pathway has been linked to immunomodulation4. Ras signaling can upregulate PD-L1 expression on tumor cells by stabilizing PD-L1 mRNA5,6 and increasing protein levels of PD-L1 with induction of the MAPK, PI3K and Akt pathways7,8,9.
In recent years, translational studies have been conducted in Asian and Western populations. In a retrospective analysis of a Chinese population of patients with KRAS-mutant advanced NSCLC, immunotherapy-based regimens achieved longer overall survival (OS) than chemotherapy-based regimens, which was independent of first or second-line setting, as well as of KRAS mutational subtypes10. The Food and Drug Administration (FDA) pooled data from 12 registrational clinical trials investigating ICI with or without chemotherapy, showing that patients with KRAS-mutated NSCLC derived the most significant benefit from the combination of chemotherapy-ICI as compared to ICI or chemotherapy alone11.
Therefore, pre-clinical and clinical data have propelled research in KRAS analyses for defining populations of metastatic cancer patients who may benefit the most from current immunotherapy. A more precise evaluation of the role of KRAS for predictive/prognostic purposes should consider the increasing evidence on the role of KRAS4A and KRAS4B isoforms12. The precursor mRNA (pre-mRNA) of KRAS is alternatively spliced to give rise to two products, Kras4A and Kras4B. The number of amino acids and molecular weight of Kras4A and Kras4B are almost identical. However, the last 24 and 25 amino acids on their C-terminal regions are coded by different exons and are, therefore, significantly different. The different C-terminal results in the aforementioned difference in post-translational modification, namely, the palmitoylation of Kras4A but not Kras4B13. Kras4A-specific interacting proteins are involved in mitosis, DNA damage, ion transport and apoptosis14. The wild-type Kras4B showed anti-apoptotic activity in animal models, while wild-type Kras4A showed pro-apoptotic activity15. It was proven in experimental carcinogenesis models that both homozygous and heterozygous KRAS4A knockout animals produced larger colonic adenocarcinomas with shorter survivor, with wild-type KRAS4A having a tumor suppressive effect16. Adenomas not expressing KRAS4A had significantly increased cell proliferation and significantly decreased apoptotic activity with evidence of activation of MAPK and Akt pathways16. Notably, in experimental models, the Kras4A-RAF1 interaction led to increased RAF-MEK-ERK signaling14, which in turn contributed to PD-L1 stabilization17. Due to the reversibility of palmitoylation, Kras4A exists in bimodal signaling states which may occur under different oncogenic cell/tissue conditions. The de-palmitoylated Kras4A is co-localized with hexokinase 1 (HK1) at the outer mitochondrial membrane. In experimental models, Kras4A was found to regulate HK118, which catalyzes the first step of glucose metabolism with glucose phosphorylation to form glucose-6-phosphate. According to experimental and pre-clinical studies, the enhanced glycolytic flux due to the Kras4A-HK1 interaction18 may sustain an immune-stimulatory tumor microenvironment19. Moreover, glycolytic activity may enhance PD-L1 expression on tumor cells and thus promote anti-PD-1/PD-L1 immunotherapy response19. Emerging work has confirmed the non-overlapping functions of the splice variants. Also, the observation that Kras4B but not Kras4A is localized on lysosomes may explain differential protein–protein interactions20. The findings that both isoforms are widely expressed in cancers with heterogeneity across tumor tissues and regardless of the mutational KRAS status21,22,23 make them worthy of translational studies addressing their role in cancer progression and resistance to current treatment options, including immunotherapy.
According to this background and considering the feasibility of mRNA quantification for both KRAS isoforms and PD-L1 in liquid biopsy24, we planned a prospective study in metastatic lung cancer patients who were candidates to first-line systemic therapy with Pembrolizumab alone or in combination with standard chemotherapy. The cmRNA expression levels of KRAS4A and KRAS4B results were analyzed and associated with PFS and cmRNA expression levels of PD-L1.
Results
Study population
Between August 2021 and December 2022, sixty patients were enrolled. Four patients were not assessable: one patient due to technical failure of mRNA analysis, one patient did not receive Pembrolizumab for medical reasons and two patients were staged with locally advanced, non-metastatic disease. The characteristics of the 56 fully assessable patients are listed in Table 1. There were 28 patients treated with Pembrolizumab and 28 patients treated with Pembrolizumab plus chemotherapy. At the time of the analysis (September 2023), 33 patients had progression (59%), and the remaining 23 (41%) were censored observations. In the whole group, the median PFS time was 15.5 months (95% CI 12–24 months).
Mean Cy0-values for KRAS4A and KRAS4B cmRNA expression levels were 30.33 (95% CI 29.96–30.70) and 29.47 (95% CI 29.02–29.92), respectively. Correlation analysis showed that Cy0-values for KRAS4A and KRAS4B are highly correlated (0.99 Pearson correlation coefficient). Mean Cy0-values for PD-L1 cmRNA was 32.90 (95% CI 32.67–33.13), the Pearson correlation coefficient between KRAS isoforms and the PD-L1 Cy0 was 0.35.
A random sample of 14 patients (25%) underwent a second liquid biopsy after 12 weeks at the time of first re-staging of disease (T1). We found comparable results between baseline (T0) and T1 cmRNA values. In detail, mean Cy0-values for KRAS4A cmRNA at T0 and T1 were 31.38 (95% CI 30.61–32.14) and 31.01 (95%CI 29.98–32.02), respectively. Mean Cy0-values for KRAS4B cmRNA at T0 and T1 were 30.71 (95% CI 29.67–31.64) and 30.23 (95%CI 28.87–31.58), respectively. Mean Cy0-values for PD-L1 cmRNA at T0 and T1 were 33.43 (95% CI 33.04–33.82) and 33.05 (95%CI 32.41–33.69), respectively.
The median PFS time in the 28 patients treated with Pembrolizumab was 24 months (95% CI 15–29 months). Mean Cy0-values for KRAS4A and KRAS4B cmRNA expression levels were 30.27 (95% CI 29.71–30.84) and 29.42 (95% CI 28.73–30.10). In the 28 patients treated with Pembrolizumab plus chemotherapy, the median PFS time was 12.5 months (95% CI 6–23 months). Mean Cy0-values for KRAS4A and KRAS4B mRNA expression levels were 30.39 (95% CI 29.87–30.90) and 29.52 (95% CI 28.88–30.15).
PFS and KRAS isoforms expression
In the analysis of the KRAS4A isoform in the 56 patients, based on ROC (area under the curve, AUC4A-plasma = 0.731, 95% CI 0.596–0.841), the Youden index (the maximum product of sensitivity and specificity observed) achieved 73% sensitivity and 74% specificity when the Cy0-values > 29.72 was used as the cut-off for Kaplan–Meier plots. In the analysis of the KRAS4B isoform in the 56 patients, based on ROC (area under the curve, AUC4B-plasma = 0.697, 95% CI 0.559–0.812), the Youden index (the maximum product of sensitivity and specificity observed) achieved 62% sensitivity and 74% specificity when the Cy0-values > 28.74 was used as the cut-off for Kaplan–Meier plots.
As shown in Fig. 1, in the Kaplan–Meier plots, there was a statistically significant difference in PFS times between patients with high and low expression of the KRAS4A and the KRAS4B cmRNA isoforms (Fig. 1a and b, respectively). In both analyses, patients classified with high expression showed better PFS than patients classified with low expression with a more pronounced effect for the KRAS4A isoform. The median PFS times of patients with high KRAS4A and high KRAS4B expressions were 29 months (95% CI 22–29 months) and 24 months (95% CI 13–29 months), respectively. Median PFS of patients with low KRAS4A and low KRAS4B cmRNA expression were 12 months (95% CI 6–15 months) and 12 months (95% CI 5–20 months), respectively.
Considering the results of the log-rank test analyses for PFS and the results of the Pearson correlation that showed a high correlation between the expression levels of the two KRAS isoforms, only the expression levels of the KRAS4A were included in the multivariate model (Table 2). The analysis also considered all available clinical features and the PD-L1 cmRNA expression. The KRAS4A expression retained a significant association with PFS.
An exploratory analysis was performed according to treatment groups (Fig. 2). In the 28 patients treated with Pembrolizumab (PD-L1 expression ≥ 50%), patients with high KRAS4A and high KRAS4B expression (Fig. 2a and b, respectively) showed significantly better PFS time than patients with low KRAS4A and low KRAS4B cmRNA expression. In the 28 patients treated with Pembrolizumab plus chemotherapy (PD-L1 expression < 50%), none of the two isoforms (Fig. 2c and d, respectively) showed a significant split of PFS curves between high and low expression groups.
As far as PD-L1 cmRNA expression is concerned, high levels (Youden index of Cy0-values > 32.87) were associated with reduced risk of progression (0.69 Hazard Ratio, 034–1.37 95% confidence intervals), but without achieving statistical significance.
Objective responses and isoforms expression
The expression of the KRAS4A and KRAS4B cmRNA isoforms was analyzed in the context of objective responses attained with immunotherapy alone or combined with chemotherapy (Table 3). There was an overall trend for higher response rates (complete plus partial responses) in high KRAS4A and KRAS4B cmRNA expression groups. Notably, a statistically significant difference was achieved in the analysis of patients treated with Pembrolizumab alone, who were selected for single-agent immunotherapy because of PD-L1 > 50% in tumor tissues.
Expression analysis
First, the high and low cmRNA levels of PD-L1, KRAS4A and KRAS4B were analyzed for association with clinical features of the study population, including the metastatic pattern (i.e., the presence of brain lesions) and KRAS mutational status. However, no significant association was observed (data not shown).
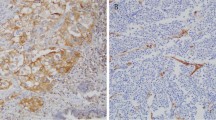
Then, the expression of the KRAS4A and KRAS4B cmRNA isoforms, together with KRAS mutational status and PD-L1 tumor expression by immunohistochemistry (IHC) were evaluated for their association with PD-L1 cmRNA level. Table 4 shows the results of this analysis. The mean cmRNA PD-L1 Cy0-value was significantly higher in the high expression group of both KRAS4A and KRAS4B isoforms. The KRAS mutational status and PD-L1 tumor expression by IHC did not seem to correlate with PD-L1 cmRNA Cy0-value.
Discussion
To the best of our knowledge, this is the first report focusing on KRAS isoforms cmRNA with emphasis on clinical outcomes in patients with metastatic lung adenocarcinoma treated with an ICI. The main findings are the association between high levels of KRAS4A and KRAS4B cmRNA high levels and high levels of PD-L1 cmRNA and the correlation between high levels of KRAS4A cmRNA and improved PFS. However, in the multivariate model, high levels of KRAS4B cmRNA showed a positive effect on PFS, but the association of this isoform did not achieve statistical significance. In the exploratory analysis according to treatment subgroups, patients with high tumor PD-L1 expression (≥ 50%) by IHC who received single-agent pembrolizumab seemed to derive the most significant PFS benefit in the presence of high KRAS4A cmRNA levels. Moreover, the responses analysis seems to parallel these findings with improved objective response rates in patients with high KRAS4A cmRNA, especially in patients treated with single-agent Pembrolizumab.
The results of our study confirm previous pre-clinical and translational studies indicating that Ras signaling can up-regulate PD-L15,6,7,8,9, which in turn may improve the therapeutic effect of an ICI20. In fact, high KRAS4A and KRAS4B levels were significantly associated with PD-L1 cmRNA levels. Notably, the same association was not detected when KRAS4A and KRAS4B quantification was correlated with tumor PD-L1 expression by IHC. This finding could be explained on the basis of the “dynamic” of PD-L1 expression in tumor tissues. To this regard, several studies have demonstrated that PD-L1 expression is highly heterogeneous between primary and metastatic lesions20. Hwang et al.25 found a significantly higher PD-L1 expression in metastatic lung cancer specimens than in the corresponding primary tumor. Moreover, cellular intrinsic factors may regulate PD-L1 expression over time20. In fact, Lacour et al.26 showed a significant increase in PD-L1 expression at tumor recurrence in NSCLC.
Although high KRAS4A and high KRAS4B cmRNA levels were comparable to high PD-L1 cmRNA levels, KRAS4A only displayed an independent association with PFS. Due to the relatively small sample size, it cannot be ruled out that also KRAS4B may achieve a statistically significant association with survival outcomes. However, in the only two available translational studies on KRAS isoforms, Yang et al.27 and Abubaker et al.28 found an association between KRAS4A abundance measures (high expression and proportion) and favorable OS of patients with lung adenocarcinoma and colorectal carcinoma. Likely, differences in biological effects between the two isoforms and peculiar properties of KRAS4A should be taken into account.
The exploratory analysis by treatment subgroups suggests that the positive effect on PFS of high KRAS4A quantification seems dominant in patients with high (≥ 50%) PD-L1 tumor expression and therefore treated with single-agent Pembrolizumab. Conversely, the impact of high KRAS4A levels seems weakened in patients treated with chemotherapy plus Pembrolizumab because of low (< 50%) PD-L1 expression. Notably, in the present study, among the 28 patients treated with chemotherapy plus Pembrolizumab, 20 patients (71.5%) had PD-L1 positivity between 1 and 5% (data not shown). These data suggest firstly that the effect of KRAS4A on PD-L1 expression or stabilization may be a mechanism that impacts the treatment outcomes of immunotherapy5,6,7,8,9. Secondly, the interplay between KRAS4A and PD-L1 may be additive and the magnitude of the clinical effect increases according to the intrinsic PD-L1 levels in the tumor microenvironment. Overall, these signals would suggest that further investigation on KRAS4A expression levels as predictive marker could be useful in patients with high PD-L1 expression.
Obviously, these results should be looked at with caution because of the limited sample size. Furthermore, they deserve validation in additional studies. Also, additional experimental studies should corroborate the hypothesis that links KRAS isoforms to the induction of the Ras pathway and finally to PD-L1 stimulation or stabilization. Another limitation of the study is the lack of information about other mutational or expression analysis in tumor tissue (i.e. TP53, MAPK plus other effectors of the KRAS cascade). However, it should be considered that small biopsies are obtained in the diagnostic evaluation of metastatic lung cancer. A histopathologic sample is usually collected from larger gauge needle biopsies (also referred to as core biopsies), such as those commonly performed during computed tomography-guided biopsies or from small-gauge needle biopsies (also referred to as fine-needle aspirates), such as those performed during bronchoscopic transbronchial needle aspirations (TBNA) of mediastinal lymph nodes. Therefore, as in our case, ancillary testing is difficult or impossible if the sparse material from small biopsy specimens has already been exhausted for routine diagnostic purposes.
Notwithstanding this, it is to be emphasized the prospective nature of the study adopting liquid biopsy and enrolling consecutive patients with metastatic lung adenocarcinoma, which formed a homogeneous population treated with Pembrolizumab-base systemic therapy. Also, we planned the study focusing on a blood test that could represent dynamic alterations of the evolving cancer. In conclusion, our findings emphasize the possibility of identifying markers associated with different efficacy of immune checkpoint inhibitors in lung cancer. In particular, in the present study, the KRAS4A isoform was found to be a promising candidate. Progress along this approach is critical to build reasoning for novel therapeutic combinations and setting a more personalized cancer immunotherapeutic strategy.
Methods
Patients and treatments
This is a prospective study, which was performed among three participating Institutions in “Regione Marche” between August 2021 and December 2022. Patients with metastatic lung adenocarcinoma without driver mutations, candidates for first-line systemic therapy, were considered eligible for study entry. Patients with central nervous system metastases were not excluded, provided that they underwent stereotactic radiotherapy of a single lesion documented by computed tomography and magnetic resonance. According to current clinical practice, patients with PD-L1 expression ≥ 50% received Pembrolizumab, whereas patients with PD-L1 expression < 50% received Pembrolizumab and chemotherapy. All patients received 200 mg of Pembrolizumab administered intravenously every three weeks. Chemotherapy consisted of Cisplatin (75 mg per square meter of body-surface area) or Carboplatin (area under the concentration–time curve, 5 mg per milliliter per minute) plus Pemetrexed (500 mg per square meter), all administered intravenously every three weeks. All patients received premedication with folic acid, vitamin B12, and glucocorticoids, administered according to local guidelines for pemetrexed use.
Enrolled patients underwent a pre-treatment blood sampling for liquid biopsy analyses. Re-staging procedures were scheduled every twelve weeks or earlier in the case of signs/symptoms of progression29. The Immune-modified response evaluation criteria in solid tumors (imRECIST) were used for the assessment of response30.
Real-time quantitative polymerase chain reaction (qPCR)
Samples were collected from the three Oncology Units of the Azienda Sanitaria Territoriale (AST) Pesaro-Fano-Urbino, Regione Marche, Italy. For each patient, two tubes/K3EDTA (6 ml each) of fresh peripheral blood were collected. Then, samples were immediately centrifuged at 1830 g for 10 min at 4 °C, and plasma was transferred to a new tube and then stored at − 80 °C. Total RNA was extracted using Trizol LS Reagent (Thermo Fisher Scientific, Waltham, MA, USA) according to the manufacturer's instructions with minor changes. Briefly, 1 volume of plasma was mixed with 3 volumes of TRIzol LS reagent. After 10 min of incubation, for each 750 µl of TRizol used, 200 µl of chloroform was added to the mixture. The mixture was incubated for 3 min at RT and then centrifuged at 3200 g for 75 min at 4 °C. The aqueous layer was transferred to a new tube and measured. RNA precipitation was performed by adding to the aqueous phase 0.8 volumes of isopropanol and 1 μl of GlycoBlue (Thermo Fisher Scientific, Waltham, MA, USA) for each 250 µl of plasma collected. The mixture was left at − 20 °C for 15 min and then centrifuged at 12,000 g for 10 min at 4 °C. The RNA was washed with cold 70% ethanol and air dried for 10 min. Next, 90 μl of DEPC-treated water was added to the pellet and incubated at 56 °C for 10 min. The RNA was quantified at the Qubit™ Fluorometer using Qubit™ RNA HS Assay Kit (Thermo Fisher Scientific, Waltham, MA, USA). Qubit™ Fluorometer uses fluorescent dyes that specifically bind to the target molecule and can distinguish intact from degraded RNA, even in extremely small amounts, providing accurate, specific and sensitive quantification of RNA. In order to overcome the problem of finding a reliable reference gene in the quantitative evaluation of target genes, we chose a different approach, based on the quantification of the RNA by the Qubit™ Fluorometer first, and then adding the same amount of cDNA (7 ng) in each assay. The RNA was concentrated to a final volume of 14 μl and SuperScript™ VILO™ cDNA Synthesis Kit (Thermo Fisher Scientific, Waltham, MA, USA) was used to generate first-strand cDNA according to the manufacturer instructions. The qPCR for the expression analyses of PD-L1, KRAS4A and KRAS4B cmRNA were performed in duplicate. TaqMan probes of the target genes were labeled with two fluorescent dyes that emit at different wavelengths (FAM or VIC for the reporter dye). The following TaqMan Gene Expression Assays, selected to avoid binding to genomic DNA specifically, were chosen: Hs00204257_m1 (PD-L1, labeled FAM), Hs00932330_m1 (KRAS4A, labeled FAM) and Hs00270666_m1 (KRAS4B, labeled VIC) (Thermo Fisher Scientific, Waltham, MA, USA). We carried out co-amplification assays when the probes were labeled with fluorescent dyes that emitted at different wavelengths.
The qPCR reaction volume included 7 ng of the sample, 1 µl of 20X TaqMan Gene Expression Assay of each target, 10 µl of 2 × Hot-Rescue Real-Time PCR Kit-Fluoprobe (MBK0012, Diatheva, Italy), 0.125 µl of Taq Polymerase (5U/µl) (Diatheva, Italy) and H2O up to the final volume of 20 µl. The reaction mixture was incubated at 50 °C for 2 min followed by 95 °C for 10 min, and then amplified for 40 cycles at 95 °C for 15 s and 60 °C for 1 min. The qPCR was performed by using an Applied Biosystems 7500 Real-Time PCR system. The cycle-threshold (Ct)-values obtained by the qPCR assays were transformed through an algorithm31 into a more accurate and precise value named Cy0.
Cy0-values were used in subsequent analyses, and they are inversely correlated with the amount of template in the assay. Therefore, a higher cmRNA expression level corresponds to a smaller Cy0-value.
Statistical analysis
The primary end-point of the study was the analysis of the possible association between KRAS4A and KRAS4B cmRNA expression levels with PFS, defined as the time from the date of the first cycle of therapy to disease progression or death, whichever happened first. Secondary end-points were the association of KRAS4A and KRAS4B cmRNA expression levels with tumor response and the association of the KRAS4A and KRAS4B cmRNA expression with PD-L1 cmRNA levels.
Receiver operating characteristic (ROC) curves served to calculate the Youden index to define the optimum cut-off values for Cy0-values for the binary classification of patients32.
With 29 events and assuming a 33% prevalence of patients with high KRAS4A and high KRAS4B cmRNA levels (categorized low Cy0-values according to the Youden index), the scenario for sample size estimation would allow the detection of a 66% reduced risk of progression with a power of 80% and a two-sided type I error of 5%. The hypothesized high performance of the studied biomarkers would pursue a meaningful clinical impact, which could justify additional validation studies33.
Mean values with 95% confidence interval (CI) for Cy0-values were reported and comparisons of means were performed adopting the t-test and the Wilcoxon test. The Pearson correlation coefficient was used to determine the correlation between KRAS4A, KRAS4B and PD-L1 cmRNA expression levels. The Fisher’s exact test analyzed categorical variables in contingency tables. The Kaplan–Meier method was used to estimate survival curves and the log-rank test was used to compare survival times between groups. A multivariable Cox proportional hazards model was then used to adjust according to clinical and pathologic features. All reported p-values were two-sided and confidence intervals (CIs) were at the 95% level. A p-value < 0.05 was considered statistically significant. Significant associations were required to be detectable with the target genes. Analyses were performed using MedCalc for Windows, version 15.0 (MedCalc Software, Ostend, Belgium).
Ethical approval
This was a local study, involving three hospitals: Pesaro, Fano and Urbino of Marche Region (Italy). For this reason it was not registered in the clinicaltrials.gov registry. The study was performed in accordance with the International Conference on Harmonization Good Clinical Practice Guidelines, the Declaration of Helsinki (1996) and approved by the local Ethics Committee (CERM, Comitato Etico Regionale delle Marche) on 29/07/2021 (Protocol code n. 2021 234). The datasets generated and/or analyzed during the current study are not publicly available due indications by the ethical committee, but they are available from the corresponding author on reasonable request.
Informed consent
All patients gave written informed consent before being included in the study.
Data availability
Research data supporting this publication are available upon request from the corresponding author.
References
Reck, M., Remon, J. & Hellmann, M. D. First-Line Immunotherapy for Non-Small-Cell Lung Cancer. J. Clin. Oncol. 40(6), 586–597. https://doi.org/10.1200/JCO.21.01497 (2022).
Li, H., van der Merwe, P. A. & Sivakumar, S. Biomarkers of response to PD-1 pathway blockade. Br. J. Cancer 126(12), 1663–1675. https://doi.org/10.1038/s41416-022-01743-4 (2022).
Adderley, H., Blackhall, F. H. & Lindsay, H. R. KRAS-mutant non-small cell lung cancer: Converging small molecules and immune checkpoint inhibition. EbioMedicine 41, 711–716. https://doi.org/10.1016/j.ebiom.2019.02.049 (2019).
Yi, M., Niu, M., Xu, L., Luo, S. & Wu, K. Regulation of PD-L1 expression in the tumor microenvironment. J. Hematol. Oncol. 14(1), 10. https://doi.org/10.1186/s13045-020-01027-5 (2021).
Coelho, M. A. et al. Oncogenic RAS signaling promotes tumor immunoresistance by stabilizing PD-L1 mRNA. Immunity 47(6), 1083–1099. https://doi.org/10.1016/j.immuni.2017.11.016 (2017).
Glorieux, C. et al. Regulation of PD-L1 expression in K-ras-driven cancers through ROS-mediated FGFR1 signaling. Redox Biol. 38, 101780. https://doi.org/10.1016/j.redox.2020.101780 (2020).
Stutvoet, T. S. et al. MAPK pathway activity plays a key role in PD-L1 expression of lung adenocarcinoma cells. J. Pathol. 249(1), 52–64. https://doi.org/10.1002/path.5280 (2019).
Sumimoto, H., Takano, A., Teramoto, K. & Daigo, Y. RAS-mitogen-activated protein kinase signal is required for enhanced PD-L1 expression in human lung cancers. PLoS One 11(11), e0166626. https://doi.org/10.1371/journal.pone.0166626 (2016).
Lastwika, K. J. et al. Control of PD-L1 expression by oncogenic activation of the AKT-mTOR pathway in non-small cell lung cancer. Cancer Res. 76(2), 227–238. https://doi.org/10.1158/0008-5472.CAN-14-3362 (2016).
Peng, L. et al. Efficacy of immunotherapy in KRAS-mutant advanced NSCLC: A real-world study in a Chinese population. Front. Oncol. 12, 1070761. https://doi.org/10.3389/fonc.2022.1070761 (2023).
Nakajima, E. C. et al. Outcomes of first-line immune checkpoint inhibitors with or without chemotherapy according to KRAS mutational status and PD-L1 expression in patients with advanced NSCLC: FDA pooled analysis. J. Clin. Oncol. 40, 9001–9001. https://doi.org/10.1200/JCO.2022.40.16_suppl.9001 (2022).
Nuevo-Tapioles, C. & Philips, M. R. The role of KRAS splice variants in cancer biology. Front. Cell Dev. Biol. 10, 1033348. https://doi.org/10.3389/fcell.2022.1033348 (2022).
Rásó, E. Splice variants of RAS-translational significance. Cancer Metastasis Rev. 39(4), 1039–1049. https://doi.org/10.1007/s10555-020-09920-8 (2020).
Zhang, X., Cao, J., Miller, S. P., Jing, H. & Lin, H. Comparative nucleotide-dependent interactome analysis reveals shared and differential properties of KRas4a and KRas4b. ACS Cent. Sci. 4(1), 71–80. https://doi.org/10.1021/acscentsci.7b00440 (2018).
Plowman, S. J. et al. The K-Ras 4A isoform promotes apoptosis but does not affect either lifespan or spontaneous tumor incidence in aging mice. Exp. Cell Res. 312(1), 16–26. https://doi.org/10.1016/j.yexcr.2005.10.004.2006 (2005).
Luo, F. et al. K-ras exon 4A has a tumor suppressor effect on carcinogen-induced murine colonic adenoma formation. J. Pathol. 220(5), 542–550. https://doi.org/10.1002/path.2672 (2010).
Xiao, X. et al. ERK and USP5 govern PD-1 homeostasis via deubiquitination to modulate tumor immunotherapy. Nat. Commun. 14(1), 2859. https://doi.org/10.1038/s41467-023-38605-3 (2023).
Amendola, C. R. et al. KRAS4A directly regulates hexokinase 1. Nature 576(7787), 482–486. https://doi.org/10.1038/s41586-019-1832-9 (2019).
Jiang, Z., Liu, Z., Li, M., Chen, C. & Wang, X. Increased glycolysis correlates with elevated immune activity in tumor immune microenvironment. EBioMedicine 42, 431–442. https://doi.org/10.1016/j.ebiom.2019.03.068 (2019).
Zhao, X. et al. From rough to precise: PD-L1 evaluation for predicting the efficacy of PD-1/PD-L1 blockades. Front. Immunol. 13, 920021. https://doi.org/10.3389/fimmu.2022.920021 (2022).
Tsai, F. D. et al. K-Ras4A splice variant is widely expressed in cancer and uses a hybrid membrane-targeting motif. Proc. Natl. Acad. Sci. USA 112(3), 779–784. https://doi.org/10.1073/pnas.1412811112 (2015).
Plowman, S. J. et al. K-ras 4A and 4B are co-expressed widely in human tissues, and their ratio is altered in sporadic colorectal cancer. J. Exp. Clin. Cancer Res. 25(2), 259–267 (2006). Erratum in: J. Exp. Clin. Cancer Res. 26(1), 2 (2007).
Eilertsen, I. A. et al. Alternative splicing expands the prognostic impact of KRAS in microsatellite stable primary colorectal cancer. Int. J. Cancer 144(4), 841–847. https://doi.org/10.1002/ijc.31809 (2019).
Cai, L. L. & Wang, J. Liquid biopsy for lung cancer immunotherapy. Oncol. Lett. 17(6), 4751–4760. https://doi.org/10.3892/ol.2019.10166 (2019).
Hwang, D. M. et al. Prevalence and heterogeneity of PD-L1 expression by 22C3 assay in routine population-based and reflexive clinical testing in lung cancer. J. Thorac. Oncol. 16(9), 1490–1500. https://doi.org/10.1016/j.jtho.2021.03.028 (2021).
Lacour, M. et al. The need of re-biopsy: Increase in PD-L1 expression from initial stage to recurrence of non-small cell lung cancer. Ann. Oncol. https://doi.org/10.1093/annonc/mdy292.040 (2018).
Yang, I. S. & Kim, S. Isoform specific gene expression analysis of KRAS in the prognosis of lung adenocarcinoma patients. BMC Bioinform. 19(Suppl 1), 40. https://doi.org/10.1186/s12859-018-2011-y (2018).
Abubaker, J. et al. Prognostic significance of alterations in KRAS isoforms KRAS-4A/4B and KRAS mutations in colorectal carcinoma. J. Pathol. 219(4), 435–445. https://doi.org/10.1002/path.2625 (2009).
Seymour, L. et al. iRECIST: Guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 18(3), e143–e152. https://doi.org/10.1016/S1470-2045(17)30074-8 (2017). Erratum in: Lancet Oncol. 20(5), e242 (2019).
Hodi, F. S. et al. Immune-modified response evaluation criteria in solid tumors (imRECIST): Refining guidelines to assess the clinical benefit of cancer immunotherapy. J. Clin. Oncol. 36(9), 850–858. https://doi.org/10.1200/JCO.2017.75.1644 (2018).
Guescini, M., Sisti, D., Rocchi, M. B., Stocchi, L. & Stocchi, V. A new real-time PCR method to overcome significant quantitative inaccuracy due to slight amplification inhibition. BMC Bioinform. 9, 326. https://doi.org/10.1186/1471-2105-9-326 (2008).
Hajian-Tilaki, K. The choice of methods in determining the optimal cut-off value for quantitative diagnostic test evaluation. Stat. Methods Med. Res. 27(8), 2374–2383. https://doi.org/10.1177/0962280216680383 (2018).
Ballman, K. V. Biomarker: Predictive or prognostic?. J. Clin. Oncol. 33(33), 3968–3971. https://doi.org/10.1200/JCO.2015.63.3651 (2015).
Acknowledgements
FanoAteneo (Italy) has financially supported this study.
Author information
Authors and Affiliations
Contributions
Conceptualization and writing the main manuscript text: F.G., A.R., S.P., R.C. Data curation: F.G., A.R, S.P., R.E., D.S. Formal analysis: F.G., A.R., S.P. Methodology project: F.G., A.R., S.P., R.C. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chiari, R., Palladino, S., Emili, R. et al. KRAS4A and KRAS4B in liquid biopsy of metastatic lung adenocarcinoma patients treated with Pembrolizumab or chemotherapy plus Pembrolizumab. Sci Rep 13, 21036 (2023). https://doi.org/10.1038/s41598-023-48304-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48304-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.