Abstract
Our goal was to investigate the effects of head-thorax elevation (HUP) during chest compressions (CC) on lung ventilation. A prospective study was performed on seven human cadavers. Chest was automatically compressed-decompressed in flat position and during progressive HUP from 18 to 35°. Lung ventilation was measured with electrical impedance tomography. In each cadaver, 5 sequences were randomly performed: one without CC at positive end-expiratory pressure (PEEP) 0cmH2O, 3 s with CC at PEEP0, 5 or 10cmH2O and 1 with CC and an impedance threshold device at PEEP0cmH2O. The minimal-to-maximal change in impedance (VTEIT in arbitrary unit a.u.) and the minimal impedance in every breathing cycle (EELI) the) were compared between flat, 18°, and 35° in each sequence by a mixed-effects model. Values are expressed as median (1st–3rd quartiles). With CC, between flat, 18° and 35° VTEIT decreased at each level of PEEP. It was 12416a.u. (10,689; 14,442), 11,239 (7667; 13,292), and 6457 (4631; 9516), respectively, at PEEP0. The same was true with the impedance threshold device. EELI/VTEIT significantly decreased from − 0.30 (− 0.40; − 0.15) before to − 1.13 (− 1.70; − 0.61) after the CC (P = 0.009). With HUP lung ventilation decreased with CC as compared to flat position. CC are associated with decreased in EELI.
Similar content being viewed by others
Introduction
Standard cardiopulmonary resuscitation (CPR) includes chest compressions and mechanical/manual ventilation aiming at restoring spontaneous circulation and maintaining gas exchange. The level of evidence for ventilator settings during CPR is weak1, and our understanding of lung physiology during CPR is limited. During chest compressions, intrathoracic pressure increases, and end-expiratory lung volume (EELV) decreases below the closing volume leading to intra-thoracic airway closure2 and atelectasis3. During chest decompressions the increase in chest wall elastic recoil promotes venous return, thereby improving hemodynamics, and possibly favors inspiratory flow due to the negative pressure in the thorax and intra-thoracic airways. However, in the presence of airway closure the negative airway pressure (Paw) may not be transmitted to the airway opening preventing the inflow of air towards the alveoli4. Low levels of positive end-expiratory airway pressure (PEEP) can maintain airway patency and inspiratory flow4 but, on the other hand, PEEP may impair venous return, right ventricle function and cerebral perfusion. An impedance threshold device (ITD) that induces negative intra-thoracic and increases venous return improves coronary blood flow and energy requirement during a porcine model of ventricular fibrillation model5. Combination of ITD with active compression-decompression CPR improves survival with favorable neurologic outcome6.
Lung protection becomes a priority whenever mechanical ventilation is applied. This may also be the case during CPR, notwithstanding the above considerations regarding hemodynamic efficiency and gas exchange preservation that are of utmost importance in the setting of cardiac arrest7,8,9. Low PEEP during CPR should contribute to lung protection as do low tidal volume and a low respiratory rate1. Automated controlled sequential elevation of the head and thorax inclination (HUP) during CPR has been shown to improve cerebral perfusion in animal models10,11 and may improve outcome in patients12. Moreover, HUP in conjunction with ITD can improve neurological outcome in animal model of cardiac arrest13. Since this maneuver can potentially stabilize EELV and minimize the large swings in lung volume during CPR, it may benefit both the hemodynamic and respiratory components of CPR.
Electrical impedance tomography (EIT) is a noninvasive technique that measures lung ventilation at a high temporal resolution and its use is increasingly popular in the intensive care unit to set PEEP. To the best of our knowledge, except for an abstract14, there is no study about EIT during CPR published in full paper format. The present study was performed using fresh human cadavers aiming to explore whether the lung ventilation distribution measured by EIT was influenced by HUP during CPR. Our hypothesis is that lung ventilation should increase with HUP in particular in the dorsal lung regions provided that higher PEEP would not promote overdistension in the ventral lung regions and chest compressions would not decrease EELI.
Methods
This was a prospective experimental cross-over study on human cadavers carried out in the anatomy laboratory. The human bodies were donated for medical science use by the donators themselves and warranting no ethical committee agreement (Additional File 1).
Cadaver preparation
The trachea was intubated and connected to a ventilator (T60, Air Liquide Medical System, Antony, France) set in volume control mode, constant flow inflation profile, tidal volume 8 ml/kg predicted body weight (additional methods are available in the Additional File 1), respiratory rate 10 breaths/min, insufflation time 1 s, end-inspiratory pause 1 s, expiratory time 4 s, inspired oxygen fraction in air 21%, and PEEP 0 cmH2O. Airway pressure was measured at a heat-and-moisture exchanger (HME) (DAR, Covidien, Mansfield, MA) attached to the endotracheal tube. A flow-meter (Hamilton Medical, Switzerland) was inserted between the Y-piece and the HME. A nasogastric catheter (Nutrivent, Sidam, Mirandola, Italy) was inserted to measure oesophageal pressure. Flow, airway pressure and esophageal pressure signals were acquired at 200 Hz by a data-logger (Biopac 150, Biopac Inc., Golletta, CA). The ITD (ResQPOD ITD 16, Zoll Medical Corporation, Chelmsford, MA, USA) was inserted between the HME and the proximal tip of the endotracheal tube in part of the experiment. It generates a negative intrathoracic pressure at the time of chest decompression during CPR and hence increases the venous blood flow to the heart15.
Cardiopulmonary resuscitation
CPR was performed by actively compressing and passively decompressing the chest with the Lund University Cardiopulmonary Assist Device (LUCAS 2, Stryker, USA) at a rate of 102/min. Chest compressions were not synchronized with the ventilator.
Protocol
Five sequences were randomly assigned to each cadaver according to a computer-generated table: no CPR-PEEP0, CPR-PEEP0, CPR-PEEP5, CPR-PEEP10, CPR-PEEP0-ITD (Fig. 1).
Each CPR sequence was performed across the same trunk inclination order: flat, 18° and 35°. When flat the cadaver was installed in a supine position with the back-plate under the body to which the LUCAS device was attached and locked with the suction cup over the chest. Before elevating the head and thorax the back-plate was replaced with one that provided an 18° inclination (EleGARD System, Advanced CPR Solutions, Mineapolis, MN, USA), to which the body was attached and locked with the LUCAS device, as in the flat step. When this second back plate was switched-on the body was gradually raised to the 35° inclination over 2 min, i.e. by an angle of 0.17°per second. Chest compressions were applied at the same angle to the chest as they were in the flat position.
In flat position chest compressions were performed over 1 min. During the 18–35° inclinations the chest compressions were started at 18° for 1 min, continued until the 35° inclination was reached and then continued for 90 s.
Respiratory mechanics
Compliance of lung and chest wall was automatically measured breath by breath in the time without chest compressions in each trunk inclination, i.e. before and after chest compressions, via an application in Matlab (Matlab2021b, The Mathworks)16.
Electrical impedance tomography
EIT device
A ring of 16 EKG electrodes (Blue sensor BR, Ambu®, Ballerup, Denmark) was placed around the thorax 5 cm above the xiphoid and connected to an EIT device (Gottingen High-Performance, Sensor Medics, Eindhoven, The Netherlands). A 5-mA alternating electrical current was applied and thorax scans were performed at 13.58 Hz.
EIT signal processing (Additional File 2).
In each pixel and in the sum of all of them within a region of interest. The minimal and maximal values of the sum of all impedance pixel defined the onset and end, respectively, of inspiration (Fig. 2). The difference between them was termed VTEIT because the changes in impedance correlates with the volume variations17,18.
Time course of lung impedance (arbitrary units: a.u.) measured with electrical impedance tomography (EIT) in cadaver#6, (CPR-PEEP0 sequence, flat position) depicting the assessment of volume change (VTEIT) and end-expiratory lung impedance (EELI) before and after chest compressions. VTEIT highlighted with the continuous and dotted double green arrows is the change between the minimal and the maximal values of the filtered lung impedance signal (red line). EELI is the minimal value. EELI was measured over the last three breaths before (continuous vertical black arrows) and during chest compressions once the tracing was stable (dotted vertical black arrows). EELI was normalized to VTEIT of the corresponding breaths.
Time course of lung impedance (arbitrary units: a.u.) measured with electrical impedance tomography (EIT) in cadaver#6, (CPR-PEEP0 sequence, flat position) depicting the assessment of volume change (VTEIT) and end-expiratory lung impedance (EELI) before and after chest compressions. VTEIT highlighted with the continuous and dotted double green arrows is the change between the minimal and the maximal values of the filtered lung impedance signal (red line). EELI is the minimal value. EELI was measured over the last three breaths before (continuous vertical black arrows) and during chest compressions once the tracing was stable (dotted vertical black arrows). EELI was normalized to VTEIT of the corresponding breaths.
EIT indexes
In addition to VTEIT, other EIT indexes based on the specific purpose of the study. The anterior-to-posterior VTEIT ratio was determined for each region of interest. An anterior-to-posterior VTEIT ratio of 1 reflected a balanced distribution of the ventilation between the dorsal and ventral lung regions. A ratio > 1 or < 1 indicated that most of the lung ventilation was distributed towards the anterior or the posterior lung regions, respectively. The pendelluft phenomenon was computed as the sum of all pixels belonging to regions of interest with negative VTEIT differences. Pendelluft was normalized to the overall VTEIT value and expressed as %VTEIT. Hence, as measured the pendelluft was in antiphase with the volume generated by the ventilator and thus pendelluft had a negative value. The pendelluft reflects an internal movement of gas during inspiration, from some parts of the lungs to other parts of the lung probably due to regional inequality in lung mechanics. This phenomenon, frequent in ICU patients19, is important because it is a mechanism by which dependent parts of the lung may get overdistended when they receive part of the inflated tidal volume from the non-dependent lung during the same inspiration20. The regional ventilation delay (RVD) measures the time delay to re-open atelectactic area with mechanical insufflation. It was computed according to Muders et al.21 on the EIT signal. In each pixel, the RVD was the percentage of the inflation time taken to reach 40% of the maximal value. An increase in the standard deviation of RVD (SDRVD) indicates a more heterogeneous distribution of regional inflation. The global inhomogeneity index (GII) measures the global spatial heterogeneity of ventilation. It was computed according to Zhao et al.22. The heterogeneity of ventilation increases with higher GII.
The end-expiratory lung impedance (EELI) was taken as the minimum value of lung impedance in each breath and normalized for VTEIT (EELI/VTEIT) (Fig. 2).
EIT data analysis
VTEIT, anterior-to-posterior VTEIT ratio and pendelluft were measured on the same breaths over 60 s (10 cycles) during chest compressions in flat, 18° and 35° trunk inclinations. Figure 3 depicts the time course of lung impedance during elevation from 18° to 35° over which the EIT measurements were performed.
EELI and EELI/VTEIT were measured over the last three breaths without and with cardiac compressions (Fig. 2).
Statistical analysis
The primary end-point was VTEIT. The secondary end-points were: anterior-to-posterior distribution of VTEIT, pendelluft, EELI/VTEIT and lung and chest wall compliance.
The analysis was conducted using a mixed-effects model for each sequence where the dependent variables were VTEIT, anterior-to-posterior VTEIT, pendelluft and EELI/VTEIT, the inclination (flat, 18°, 35°) the factor with fixed effect and the cadaver with the factor with a random effect . The reference position was flat, to which the two other inclinations were compared. The accuracy of the model was checked by plotting the standardized residuals to the fitted values.
Lung and chest all compliance were compared before and after cardiac compressions in flat position by using a mixed-effects model. They were also compared before cardiac compression at 18° versus after compression at 35° for the sequences 2–5. This was due to the fact that the chest compressions were continuously performed during elevation, and hence this comparison includes the effect of cardiac compression and of trunk inclination change as well. Values are presented as median (1st-3rd quartiles) unless otherwise stated.
Ethics approval and consent to participate
The human bodies used in this study were donated for medical science use by the donators themselves. Written and witnessed consent to donate their bodies to science for anatomical and pedagogical purposes was given prior to death. This donation was free, anonymous, and regulated by the French funeral legislation. According to French law, no other approval was necessary by French authorities or by the local ethical board.
Results
Seven cadavers (4 females and 3 males) of 89 ± 9 (mean ± SD) years of age and 51 ± 8 kgs predicted body weight were used (Additional File 3). Esophageal pressure was not available for one cadaver (failure to insert the nasogastric catheter in cadaver#1).
Effect of inclination on VTEIT
As shown in Table 1, the VTEIT did not change significantly across the trunk inclination when the chest was not compressed. When chest compressions were performed VTEIT decreased with trunk elevation as compared to flat position (Table 1). This decrease was consistently significant at 35° in every sequences with chest compressions and also at 18° in the CPR-PEEP0-ITD sequence. EIT parametric images of VTEIT are shown in Fig. 4.
Effect of inclination on anterior-to-posterior VTEIT, pendelluft and EELI/VTEIT, SDRVD and GII
The anterior-to-posterior VTEIT did not statistically significantly change with trunk elevation in any sequence (Table 1). The same was true for pendelluft except that it was lower at 18° in the sequence 1 without chest compression. EELI/VTEIT became more negative, i.e. EELI decreased, with trunk elevation in every sequence but the first, the difference being statistically significant only for the CPR-PEEP10 sequence (Table 1). There was a non-significant trend to a reduction in SDRVD with body inclination in every sequence (Table 1). With body inclination GII non-significantly tended to decrease in absence of chest compression and at PEEP 0 and to increase in the other conditions (Table 1).
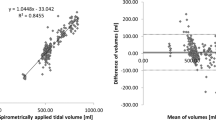
Effect of chest compressions on EELI/VTEIT
After chest compressions EELI/VTEIT was significantly lower than before chest compressions in every sequence with CPR (Fig. 5). Across all of them it significantly decreased from − 0.30 (− 0.40; − 0.15) before to − 1.13 (− 1.70; − 0.61) after the chest compressions (P = 0.009).
Box-and-whisker plots of end expiratory lung impedance to change in impedance (EELI/VTEIT) ratio before and after chest compressions during the 4 sequences with chest compressions. CPR cardiopulmonary resuscitation, PEEP positive end-expiratory pressure, ITD impedance threshold device. *P < 0.05 vs before.
Effect of chest compressions on lung and chest wall compliance
In the flat position the lung and chest wall compliance increased after chest compressions except in the CPR-PEEP0-ITD sequence for the lung compliance and in the CPR-PEEP5 sequence for the chest wall (Table 2). During trunk elevation, the chest wall and lung compliances were higher after than before chest compressions, expect for lung compliance, which was lower in sequence CPR-PEEP5 and also in CPR-PEEP0-ITD sequence though not significantly.
Discussion
To our knowledge, this is the first study that measures the distribution of lung ventilation with EIT during flat and HUP-CPR in human cadavers. The main findings were: (1) with HUP-CPR, VTEIT decreased at PEEP values of 0, 5 and 10 cmH2O compared to flat CPR, but its anterior-to-posterior distribution did not significantly change; the same was found with ITD in place; (2) the chest compressions decreased EELI/VTEIT.
Methodology
Before to discuss present results, a critique of our methodology is required. The study challenged the EIT technology in many ways. One was the location of the electrodes across the thorax. Using a ring of electrodes rather than a belt was thought more flexible to accommodate the LUCAS installation. Another issue was the baseline recording. EIT depends on a measurement of change in impedance relative to a baseline. Performing a continuous EIT recording that would have taken more than one hour had several risks. One was a potential electrode contact defect during the different maneuvers and the loss of parts of the records. Therefore, the design took into account this issue and the experiment was split into 5 sequences for which the baseline was as close as possible to the recording of the head elevation maneuver. Another risk was the skin contact of the electrodes. To manage it, the EIT device continuously monitored the electrode impedance in order to maintain it in the appropriate range. Finally, the issue of filtering the EIT signal disturbed by chest compression artefacts was solved as shown in Figs. 1, 2 giving a good signal-to-noise ratio. Furthermore, the accuracy of filtering was tested after each recording with our flexible application developed in Matlab. Contrary to most of the commercial EIT systems with which the sternum and spine are avoided with electrodes placed to inject more electric current into the chest cavity, our device included one sternal and one spinal electrode. As we argued in the Additional File 2, we decided not to use a conventional EIT belt due to the presence of the CPR device placed in the mid-sternum. We reasoned that by using a series of 16 EIT electrodes would facilitate the management of the CPR with that device. It is true that placing the electrodes 1 and 9 at the sternum and spine, respectively, was the way the EIT prototype was used and published in many publications about EIT18,23,24,25 before the new commercial devices came up. To the best of knowledge, there was no comparison between the single 16 electrodes and the 16-electrodes belt.
Model validation
The present study shows that EIT is feasible during CPR in humans, which has clinical and research implications. Beyond this, we are aware that it is important to make sure that the present results are consistent with past and future findings.
Two findings deserve attention in the perspective of a model validation. Without chest compressions at PEEP0, EELI/VTEIT did not change with HUP in present study. By contrast, in acute respiratory distress syndrome patients HUP was associated with, on one hand, an increased EELV26,27,28,29, and, on the other hand, higher plateau pressure and lower respiratory system compliance that improved with chest strapping30. Both findings suggest that HUP may induce end-inspiratory overdistension and that an increase in EELV may reflect overdistension. The anterior-to-posterior distribution of VTEIT was markedly greater than 1 in the flat position in all the sequences, indicating a marked distribution of tidal volume towards the most anterior parts of the lung during mechanical ventilation and CPR. This may also reflect atelectasis in the dorsal lung regions.
Effect of HUP and chest compressions on VTEIT at different PEEP values
In present study we measured VTEIT, its anterior-to-posterior distribution and the pendelluft during chest compressions at various trunk inclinations. In the flat position, VTEIT was twice higher with CPR at any PEEP than without at PEEP0 (Table 1). We did not formally compare these values because the baseline may differ across the sequences. VTEIT decreased with HUP consistently across all PEEP levels. This finding may reflect overdistension with HUP, in particular in the ventral lung regions, or by collapse in the dorsal lung regions or by a combination of both. Our study design did not permit to further explore these mechanisms. Ascribing the findings entirely to ventral overdistension might be too simplistic, in particular because the VTEIT distribution did not change between conditions. The fact that GII increased, though not significantly, with body inclination at PEEP 5 and 10 when RVD decreases may suggest overinflation in the ventral regions, should it be assumed that the lower SDRDV reflects recruitment in the dorsal lung regions. It should be noted, however, that there were changes in that distribution but these were not statistically significant perhaps by lack of power. However, the anterior-to-posterior distribution of VTEIT did not change significantly with HUP as compared to baseline. With the ventral lung regions overdistended, the ventilation in those regions, and hence the anterior-to-posterior of VTEIT would likely be lower with HUP. On the other hand, the pendelluft phenomenon, which was present in the flat position in each sequence, did not significantly change with HUP during the chest compressions.
Yang et al. measured some EIT indexes in 30 normal volunteers breathing spontaneously at 0, 30, 60 and 90 degrees from the horizontal plane in the supine position31. They found that with the sitting positioning the dorsal ventilation increased and the ventilation became more heterogeneous. Moreover, the authors had concern about keeping the same the position of the electrodes over the range of inclination. Our results are difficult to compare with that of Yang et al. given the difference in subjects and ventilation regimen31.
Effect of chest compressions on EELI/VTEIT
We measured EELI/VTEIT before and after chest compressions at different trunk angulations and PEEP values. The present study confirms that chest compressions during non-synchronous mechanical ventilation decreases EELI, as already reported for EIT in an experimental model of cardiac arrest in pigs14 and in other studies32,33. This also argues in favor of the model’s validity. The clinical implication for this finding would be to set some PEEP during the chest compressions or once the circulation is restored in order to optimize ventilation, the balance with the effect on cerebral perfusion and venous return is still to be determined. However, in present study even with PEEP, EELI/VTEIT decreased with HUP, suggesting that HUP would not improve lung ventilation.
Lung and chest wall mechanics
In human cadavers a previous study found that the chest wall compliance increased over time after chest compressions34. In present study we assessed the chest wall compliance by using esophageal manometry and also found it was higher after than before chest compressions, in each trunk inclination and at each PEEP value. The chest wall was softened by the prolonged chest compression. This confirmative finding is another evidence validating our experimental model. In the absence of lung CT scans it was not possible to assess the nature and extent of lung injury, if any, in the cadavers we used. It is, however, likely that the bodies had some degree of lung edema and or tissue edema.
Limitations
Our study has several limitations. One is the use of a cadaver model. For this reason, no recommendation can be made regarding inclination or the use if an ITD because no information about hemodynamics and cerebral perfusion could be collected during present experiment. Tidal volume measured by EIT does not account for the presence of pulmonary ventilation due to chest compressions, which may also be influenced by chest elevation and PEEP. As mentioned above, the lack of lung CT to better define the presence and extent of lung injury at baseline is a limitation. Our study is a pilot study and probably underpowered due to the cost and availability of cadavers. Therefore, it only allows us to track trends and we cannot draw any firm conclusions. A better understanding of the effects of chest compressions and the impact of mechanical ventilation during CPR on lung ventilation distribution could impact the use of mechanical ventilation after cardiac arrest35.
Conclusions
HUP during chest compressions decreased lung ventilation compared to standard flat CPR. This reduction might be linked with the reduction in pulmonary overdistension during CPR or simply a decrease below normal values. Chest compressions decreased end-expiratory lung impedance.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- CPR:
-
Cardiopulmonary resuscitation
- EELV:
-
End-expiratory lung volume
- PEEP:
-
Positive end-expiratory pressure
- ITD:
-
Impedance threshold device
- HUP:
-
Head-up
- EIT:
-
Electrical impedance tomography
- HME:
-
Heat and moisture exchanger
- LUCAS:
-
Lund University Cardiopulmonary Assist
- VTEIT:
-
Change in lung impedance during breathing cycles
- EELI:
-
End-expiratory lung impedance
- GII:
-
Global inhomogeneity index
- SDRVD:
-
Standard deviation of regional ventilation delay
References
Orso, D. et al. Mechanical ventilation management during mechanical chest compressions. Respir. Care 66(2), 334–346 (2021).
Cordioli, R. L. et al. Impact of ventilation strategies during chest compression. An experimental study with clinical observations. J. Appl. Physiol. (1985) 120(2), 196–203 (2016).
Markstaller, K. et al. Effect of chest compressions only during experimental basic life support on alveolar collapse and recruitment. Resuscitation 79(1), 125–132 (2008).
Charbonney, E. et al. A new physiological model for studying the effect of chest compression and ventilation during cardiopulmonary resuscitation: The Thiel cadaver. Resuscitation 125, 135–142 (2018).
Lurie, K. G. et al. Improving active compression-decompression cardiopulmonary resuscitation with an inspiratory impedance valve. Circulation 91(6), 1629–1632 (1995).
Aufderheide, T. P. et al. A trial of an impedance threshold device in out-of-hospital cardiac arrest. N. Engl. J. Med. 365(9), 798–806 (2011).
Olasveengen, T. M. et al. Adult basic life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 142(16_suppl_1), S41–S91 (2020).
Wyckoff, M. H. et al. 2021 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: Summary from the basic life support; advanced life support; Neonatal life support; education, implementation, and teams; first aid task forces; and the COVID-19 working group. Resuscitation 169, 229–311 (2021).
Soar, J. et al. 2019 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 145, 95–150 (2019).
Huang, C. C. et al. The effect of the head-up position on cardiopulmonary resuscitation: A systematic review and meta-analysis. Crit. Care 25(1), 376 (2021).
Varney, J. et al. Efficacy of heads-up CPR compared to supine CPR positions: Systematic review and meta-analysis. Health Sci. Rep. 5, e644 (2022).
Moore, J. C. et al. Head and thorax elevation during cardiopulmonary resuscitation using circulatory adjuncts is associated with improved survival. Resuscitation 179, 9–17 (2022).
Moore, J. C. et al. Controlled sequential elevation of the head and thorax combined with active compression decompression cardiopulmonary resuscitation and an impedance threshold device improves neurological survival in a porcine model of cardiac arrest. Resuscitation 158, 220–7 (2021).
Szczyrba, M. et al. Influence of chest compressions during cardiopulmonary resuscitation on regional ventilation distribution by electrical impedance tomography. Eur. J. Anaesthesiol. 28, 190 (2011).
Lurie, K. et al. Use of an inspiratory impedance threshold valve during cardiopulmonary resuscitation: A progress report. Resuscitation 44(3), 219–230 (2000).
Riad, Z., Mezidi, M., Subtil, F., Louis, B. & Guerin, C. Short-term effects of the prone positioning maneuver on lung and chest wall mechanics in patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 197(10), 1355–1358 (2018).
Frerichs, I. et al. Chest electrical impedance tomography examination, data analysis, terminology, clinical use and recommendations: Consensus statement of the TRanslational EIT developmeNt stuDy group. Thorax 72(1), 83–93 (2017).
Richard, J. et al. Electrical impedance tomography compared to positron emission tomography for the measurement of regional lung ventilation: An experimental study. Crit. Care 13(3), R82 (2009).
Chi, Y., Zhao, Z., Frerichs, I., Long, Y. & He, H. Prevalence and prognosis of respiratory pendelluft phenomenon in mechanically ventilated ICU patients with acute respiratory failure: A retrospective cohort study. Ann. Intensive Care 12(1), 22 (2022).
Yoshida, T., Uchiyama, A., Matsuura, N., Mashimo, T. & Fujino, Y. The comparison of spontaneous breathing and muscle paralysis in two different severities of experimental lung injury. Crit. Care Med. 41(2), 536–545 (2013).
Muders, T. et al. Tidal recruitment assessed by electrical impedance tomography and computed tomography in a porcine model of lung injury*. Crit. Care Med. 40(3), 903–911 (2012).
Zhao, Z., Steinmann, D., Frerichs, I., Guttmann, J. & Moller, K. PEEP titration guided by ventilation homogeneity: A feasibility study using electrical impedance tomography. Crit. Care 14(1), R8 (2010).
Frerichs, I., Dargaville, P. A., Dudykevych, T. & Rimensberger, P. C. Electrical impedance tomography: A method for monitoring regional lung aeration and tidal volume distribution?. Intensive Care Med. 29(12), 2312–2316 (2003).
Frerichs, I. et al. Detection of local lung air content by electrical impedance tomography compared with electron beam CT. J. Appl. Physiol. 93(2), 660–666 (2002).
Frerichs, I. et al. Gravity effects on regional lung ventilation determined by functional EIT during parabolic flights. J. Appl. Physiol. (1985) 91(1), 39–50 (2001).
Mezidi, M. & Guerin, C. Effect of body position and inclination in supine and prone position on respiratory mechanics in acute respiratory distress syndrome. Intensive Care Med. 45(2), 292–294 (2019).
Spooner, A. J. et al. Head-of-bed elevation improves end-expiratory lung volumes in mechanically ventilated subjects: A prospective observational study. Respir. Care 59(10), 1583–1589 (2014).
Richard, J. C. et al. Effects of vertical positioning on gas exchange and lung volumes in acute respiratory distress syndrome. Intensive Care Med. 32(10), 1623–1626 (2006).
Dellamonica, J. et al. Effect of different seated positions on lung volume and oxygenation in acute respiratory distress syndrome. Intensive Care Med. 39(6), 1121–1127 (2013).
Selickman, J. et al. Paradoxical positioning: Does “Head Up” always improve mechanics and lung protection?. Crit. Care Med. 50(11), 1599–1606 (2022).
Yang, L. et al. The influence of gravity on electrical impedance tomography measurements during upper body position change. Heliyon 9(5), e15910 (2023).
Charbonney, E. et al. Ventilation during cardiopulmonary resuscitation: What have we learned from models?. Respir. Care 64(9), 1132–1138 (2019).
Charbonney, E., Savary, D., Badat, B., Grieco, D. L. & Richard, J. C. Low ventilation associated with chest compression, an old observation that requires new physiological interpretation. Am. J. Emerg. Med. 37(6), 1212–3 (2019).
Segal, N. et al. Chest compliance is altered by static compression and decompression as revealed by changes in anteroposterior chest height during CPR using the ResQPUMP in a human cadaver model. Resuscitation 116, 56–59 (2017).
Robba, C. et al. Ventilatory settings in the initial 72 h and their association with outcome in out-of-hospital cardiac arrest patients: A preplanned secondary analysis of the targeted hypothermia versus targeted normothermia after out-of-hospital cardiac arrest (TTM2) trial. Intensive Care Med. 48(8), 1024–1038 (2022).
Acknowledgements
We thank our English language expert, who is and English native speaker with skills in Medicine, for critically reading and editing the manuscript.
Author information
Authors and Affiliations
Contributions
H.D. Conceptualization, Data curation, Formal analysis, investigation, Methodology, Resources, Validation, Writing—review & editing. N.T. Conceptualization, Data curation, Formal analysis, investigation, Methodology, Resources, Validation, Writing—review & editing. N.S. Data curation, investigation, Resources, Writing—review & editing. A.B. Data curation, investigation, Resources, Project administration, Writing—review & editing. C.S. Data curation, investigation, Resources, Writing—review & editing. B.L. Conceptualization, Data curation, Formal analysis, investigation, Methodology, Software, Validation, Writing—review & editing. G.D. Conceptualization, Data curation, Formal analysis, investigation, Methodology, Validation, Writing—review & editing. C.G. Conceptualization, Data curation, Formal analysis, investigation, Methodology, Software, Validation, Writing—original draft, Writing—review & editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duhem, H., Terzi, N., Segond, N. et al. Effect of automated head-thorax elevation during chest compressions on lung ventilation: a model study. Sci Rep 13, 20393 (2023). https://doi.org/10.1038/s41598-023-47727-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-47727-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.