Abstract
High body mass index (BMI), or excess body weight (EBW), represents a significant risk factor for a range of diseases, including cardiovascular diseases and cancers. The study sought to determine the burden of diseases attributable to EBW in the Middle East and North Africa (MENA) region from 1990 and 2019. The analysis also included an exploration of this burden by age, sex, underlying cause, and sociodemographic index (SDI). We utilized publicly available data from the Global Burden of Disease (GBD) study 2019 to identify the deaths and disability-adjusted life-years (DALYs) of diseases associated with EBW in MENA, spanning the period from 1990 to 2019. The GBD estimated the mean BMI and the prevalence of EBW using hierarchical mixed-effects regression, followed by spatiotemporal Gaussian process regression to determine the most accurate BMI distribution through comparison with actual data. In 2019, there were an estimated 538.4 thousand deaths (95% UI 369.9–712.3) and 17.9 million DALYs (12.9–23.1) attributable to EBW in the region. The DALYs attributable to EBW were higher in men (9.3 million [6.5–12.4]) than in women (8.5 million [6.4–10.8]). The age-standardized death and DALY rates for the diseases associated with EBW increased by 5.1% (− 9.0–25.9) and 8.3% (− 6.5–28.8), respectively, during the study period which was not significant. Egypt had the highest age-standardized mortality rate due to EBW (217.7 [140.0, 307.8]), while Yemen (88.6 [45.9, 143.5]) had the lowest. In 2019, the highest number of DALYs occurred among individuals aged 60 to 64 years old. Furthermore, we found a positive association between a nation's SDI and the age-standardized DALY rate linked to EBW. Cardiovascular disease emerged as the leading contributor to the EBW burden in MENA. The disease burden attributable to EBW showed a non-significant increase in MENA from 1990 to 2019.
Similar content being viewed by others
Introduction
Overweight and obesity, collectively named excess body weight (EBW) or having a body mass index (BMI) ≥ 25 kg/m2, has shown clear associations with several chronic conditions, including cardiovascular, respiratory, neurological, gastrointestinal, and endocrinological diseases1,2. The relationships that EBW has with the burden of cancers3,4,5, osteoarthritis6, and other non-communicable diseases7 have also been established. EBW is a multifactorial and complex disease associated with multiple biological, psychological and socio-environmental risk factors8. It is influenced not only by genetic and epigenetic factors, such as genes of the leptin-melanocortin signaling pathway and the peroxisome proliferator-activated receptor gamma gene, but also by environmental factors, drugs, emotional factors, and even gut microbiota dysbiosis9,10. EBW has been declared a pandemic that demands global efforts for its prevention11.
During the period from 1975 to 2016, there was a notable rise in the age-standardized prevalence of EBW in across almost all regions of the world12. In 2017, the age-standardized rates of death and disability-adjusted life years (DALYs) linked to EBW were 109.5 and 3256.0 per 100,000 population, respectively1. In 2017, globally, cardiovascular diseases were the largest contributors to the burden of diseases linked to EBW, followed by diabetes and kidney diseases1. Moreover, the global age-standardized DALY rate associated with EBW-related diseases increased with advancing age in 2017, exception of for a decrease observed in the 75–84 years age group1. Furthermore, globally, the age-standardized DALY rate was higher for males up to 69 years, and then it was higher among females1. There was also an inverted-U shaped association between the burden of EBW-attributable diseases and socioeconomic development at regional levels1. In 2015, EBW accounted for 10.0% of all deaths and 6.3% of all DALYs in the Eastern Mediterranean Region13. Moreover, in 2017, the burden attributable to EBW was most pronounced in the 95 + age group and in regions characterized by intermediate levels of socioeconomic development1. The burden attributable to EBW in 2017 was also reported at the global level1, and in some regions and countries, such as the Eastern Mediterranean Region13 and Colombia14.
Economic modeling provides insights into the escalating economic cost of EBW, which is projected to rise from 1.8% of the gross domestic product in 2019 to an estimated 3.6% by the year 206015. In the case of children aged 2–5 years, a 0.13 decrease in BMI Z score can potentially save more than 36 thousand health-adjusted life years and approximately $31 million in healthcare costs16.
A previous study documented the worldwide burden of diseases associated with high BMI in 20171. However, here has not been any previous research on the burden of diseases associated with EBW in the Middle East and North Africa (MENA) region. The MENA region encompasses nations that have substantial variations in the level of social development, and the region has witnessed large changes in social, economic, and cultural patterns. Given the large changes in the dietary behaviors and lifestyles among the region’s population, it is important to evaluate the disease burden attributable to EBW17. Therefore, this study assessed the burden of diseases attributable to EBW by age, sex, underlying cause, and socio-demographic index (SDI) in the 21 countries of the MENA region from 1990 to 2019.
Methods
Overview
The Global Burden of Disease (GBD), an initiative led by the Institute for Health Metrics and Evaluation (IHME), is an ongoing project aimed at assessing the global disease burden. The most recent edition, GBD 2019, sought to gauge the burden of 369 diseases and injuries along with 87 risk factors for the years 1990 to 2019 across 204 countries and 21 regions18,19. Among these regions, the MENA region consists of the following 21 countries: Afghanistan, Algeria, Bahrain, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Palestine, Qatar, Saudi Arabia, Sudan, the Syrian Arab Republic, Tunisia, Turkey, the United Arab Emirates and Yemen. The Comparative Risk Assessment (CRA) method was employed to model the burden attributed to 87 risk factors, including EBW. The methods used to estimate the disease and injury burdens, as well as the influence of risk factors have been extensively documented in previous publications18,19. The fatal and non-fatal data can be obtained from the following websites: https://vizhub.healthdata.org/gbd-compare/ and http://ghdx.healthdata.org/gbd-results-tool. In this study, data on EBW, defined by BMI, were collected from sources such as surveys and systematic literature reviews. Different models were then used to estimate the burden of diseases associated with EBW in each country by age, sex, and SDI.
Case definition and data sources
BMI was used to determine whether adults were overweight (BMI 25–30.0 kg/m2) or obese (BMI > 30 kg/m2). The burden of diseases linked to EBW was determined using the GBD 2019 methodology19. The prevalence of high BMI was estimated in the GBD 2019, for both children and adults, in 204 countries and territories from 1990 to 2019. The exact methodology used to estimate mean BMI has been reported previously19,20. To identify studies that estimated the prevalence of EBW and mean BMI at the national or subnational level, the IHME conducted a comprehensive search of the online Medline database in 2015. This comprehensive literature review was updated using the same process for articles published in 2016 (January 1 to December 31). In addition, a search of the Global Health Data Exchange (GHDx) database was conducted to identify individual-level information from large international or national surveys19,21. The search strategy and data sources obtained for each country and territory have been previously published19,21.
The IHME extracted information from the literature on sample size, mean BMI, prevalence of overweight, prevalence of obesity, uncertainty measures for overweight and obesity, and locations and years for the most accurate age and sex categories available. In addition, IHME also collected details about each data source such as primary sampling unit, strata, and survey weights, which were used to formulate individual-level microdata and provide more accurate estimates of uncertainty. Three study-level variables were created to provide information on whether: (1) the sample was representative of the population; (2) the study was conducted primarily in urban areas, rural areas, or both; and (3) height and weight data were self-reported or measured. For countries with multiple data sources, all were incorporated into the analyses19.
Estimations of BMI and the prevalence of overweight and obesity
To calculate the avarage BMI, a stratified hierarchical mixed-effects regression was applied to examine the connection between BMI, overweight and obesity in data sources that provided information on all three variables. For this purpose, sex-specific MR-BRT models were used to analyze both overweight and obesity. These models focused on the logit disparity between measured and self-reported data. The coefficients derived from this regression were then used in a spatiotemporal Gaussian process regression (ST-GPR) to model the prevalence of individuals with overweight and obesity in each country by age, sex and year. Multiple distributions were evaluated against the actual data to determine the BMI distribution that most closely resembled it. The final form of the beta distribution was determined using the mean BMI and the prevalence of being classified as overweight or obese in each country, by age, sex and year. For a more comprehensive understanding of the modeling process please refer to the GBD capstone paper19.
The prevalence of overweight and obesity was calculated via ST-GPR models19,22. To enhance estimates in countries with limited data, three country-level covariates were used: per capita energy intake with a 10-year lag, country latitude, and the urban population proportion. The selection of these three variables was informed by extensive prior research20,22, as they demonstrated the most favorable fit and coefficients that aligned with anticipated trends19,21.
In GBD 2019, Meta-Regression with Bayesian priors, Regularization and Trimming (MR-BRT) was used to adjust for self-report bias. Sex-specific MR-BRT models were conducted, with a fixed effect for super-region on the logit difference between overweight and obesity, depending on whether they were measured or self-reported19.
Data on the estimated relative risk
The evidence substantiating the relationships high BMI had with the different diseases was evaluated using the CRA approach. In brief, the CRA contains six main steps, which include: identification of the risk-outcome pairs to utilise in the analysis; estimating the relative risk as a function of exposure; estimating exposure levels and distributions; determining the counterfactual level of exposure; computing the fraction of the population that can be attributed and the burden that can be attributed; and estimating the mediation of various risk factors19. Additional information on this estimation process has been published previously19. The evidence indicated that the following conditions are associated with high BMI: cardiovascular diseases, diabetes and kidney diseases, neoplasms, gallbladder and biliary diseases, asthma, cataracts, osteoarthritis, low back pain, gout, as well as Alzheimer’s disease and other dementias19.
Estimation of the proportion of diseases associated with EBW
The population-attributable fraction (PAF) was employed to gauge the disease burden linked to EBW by country, age group, sex, and year. The theoretical minimum risk exposure level (TMREL), measured using the estimated relative risk (RR), was used in GBD 2019 to estimate the level of exposure to each risk factor that would minimize the chances of suffering any EBW-related burden. The following formula was used to calculate the PAF:
n is the lowest level of exposure observed, m is the highest level of exposure recorded, RR(x) is the relative risk at an exposure level of x and P(x) is the fraction of risk exposure19.
Compilation of results
In GBD 2019, the number of deaths and DALYs linked to EBW were estimated for each nation, age group, sex, year and attributable disease by multiplying the appropriate numbers with the corresponding PAFs. Detailed information regarding the methods utilized for estimating the number of deaths and the disease-attributable DALYs has been reported previously19. All estimations were presented as numerical counts, proportions (PAFs), and age- standardized rates per 100,000. Furthermore, they were accompanied by 95% uncertainty intervals (UIs) which encompassed the 25th and 975th values of the 1000 ordered draws19. The association between socio-economic development and the diseases attributable to EBW was also examined. The GBD project measures socio-economic development using SDI, which is a composite measure comprised of three components: the fertility rate for women under 25 years old, the average years at school for individuals over 15 years old, and the lag-distributed income per capita. SDI ranges from the least developed (0) to the most developed1.
Ethical approval
The present study was approved by the ethics committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.PHNS.REC.1401.101). All methods were performed in accordance with the national guidelines and regulations. This study is based on publicly available data and solely reflects the opinion of its authors and not that of the Institute for Health Metrics and Evaluation.
Results
The Middle East and North Africa region
In 2019, there were 538.4 thousand deaths (95% UI 369.9 to 712.3) linked to EBW in the MENA region. This accounted for 17.4% (12.2 to 22.5) of all deaths in the region (Table 1). Also in 2019, there were 272.3 (177.8 to 368.5) thousand deaths in men that were attributable to EBW and 266.2 (190.4 to 344.0) thousand deaths among women (Table S1). The age- standardized death rate in 2019 (133.6 [90.0 to 179.0] per 100,000) was 5.1% higher (-9.0 to 25.9) than in 1990 (127.1 [79.2 to 181.3]) (Table S2). In 2019, EBW caused 17.9 million DALYs (12.9 to 23.1), which accounted for 10.9% (7.9 to 13.9) of all DALYs in both males and females combined, with 9.3 (6.5 to 12.4) million DALYs in men and 8.5 (6.4 to 10.8) million DALYs among females (Table S3). Over the period 1990-2019, the age-standardized DALY rate (per 100,000) increased from 3488.8 (2262.5 to 4798.5) to 3777.2 (2692.6 to 4943.3), a relative increase of 8.3% (− 6.5 to 28.8) (Table S4).
Country level
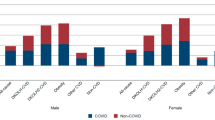
In 2019, the proportion of all deaths linked with EBW varied markedly between countries (from 6.7% to 26.4%). Bahrain (26.4 [19.3 to 32.4]), the United Arab Emirates (26.2% [20.3 to 31.4]) and Jordan (23.4% [16.9 to 29.0]) had the three highest PAFs. Conversely, the lowest PAFs were observed in Yemen (6.7% [3.8 to 9.9]), Afghanistan (8.8% [5.7 to 12.0]) and Sudan (12.1% [7.8 to 16.9]) (Table 1). The age-standardized mortality rate linked to EBW in 2019 ranged from 88.6 to 217.7 per 100,000. In 2019, Egypt (217.7 [140.0 to 307.8]), Qatar (209.6 [137.1 to 285.7]) and the United Arab Emirates (203.0 [138.4 to 274.6]) had the three highest rates per 100,000 with the lowest found in Yemen (88.6 [45.9 to 143.5]), Iran (91.7 [63.9 to 122.1]) and Kuwait (93.6 [62.4 to 125.4]) (Table 1). Figure 1A presents the age-standardized death rate attributable to EBW in 2019 by sex. The largest increases in the age-standardized death rate linked to EBW, between 1990 and 2019, were observed in Oman (55.7% [12.3 to 150.1]), Sudan (44.6% [8.4 to 123.9]) and Yemen (37.8% [− 2.0 to 131.9]). Conversely, the largest decreases were observed in Turkey (− 25.4% [− 42.5 to − 4.8]), Bahrain (− 23.6% [− 37.9 to − 2.5]) and Kuwait (− 23.4% [− 34.9 to − 7.4]) (Table S2). Figure S1 shows the percentage change in the age-standardized death rate, from 1990 to 2019, by sex.
Age- standardized death (A) and DALY (B) rates (per 100,000 population) of diseases attributable to excess body weight in the Middle East and North Africa region, by sex and country. DALY = disability adjusted life years. (Generated from data available from http://ghdx.healthdata.org/gbd-results-tool).
The proportion of all DALYs linked with EBW in 2019 differed substantially between countries (from 3.5% to 17.4%). The United Arab Emirates (17.4% [13.6 to 21.0]), Bahrain (17.2% [12.9 to 20.9]) and Egypt (16.0% [11.3 to 20.3]) had the three highest PAFs. Conversely, the lowest PAFs were observed in Yemen (3.5% [2.0 to 5.2]), Afghanistan (4.6% [3.0 to 6.5]) and Sudan (6.6% [4.3 to 9.2]) (Table 1). In 2019, the age-standardized DALY rate due to EBW ranged from 2580.9 to 5929.6 per 100,000. Egypt (5929.6 [3973.1 to 8107.8]), the United Arab Emirates (5732.9 [4111.7 to 7383.3]) and Afghanistan (5098.6 [3230.9 to 7244.7]) had the three highest age-standardized DALY rates. Conversely, the lowest rates were found in Iran (2580.9 [1845.1 to 3337.3]), Yemen (2595.6 [1422.7 to 4079.9]) and Turkey (2662.6 [1804.0 to 3599.4]) (Table 1). Fig. 1B displays the age standardized DALY rates in 2019 by sex. The largest increases in the DALY rates, between 1990 and 2019, were observed in Yemen (41.1% [− 1.6 to 137.9]), Sudan (39.9% [4.8 to 116.8]) and Oman (38.5% [2.0 to 109.5]). Conversely, the largest decreases were observed in Turkey (− 23.3% [− 37.6 to − 5.4]), Bahrain (− 21.2% [− 35.0 to − 3.1]), and Jordan (− 19.5% [− 32.3 to − 1.0]) (Table 1). Figure S2 presents the percentage change in the age-standardized DALY rates, from 1990 to 2019, by sex.
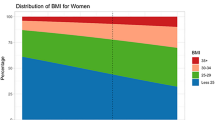
Age and sex patterns
In 2019, the number of deaths linked to EBW in MENA peaked in the 60–64 age group for males and 65–69 age group for females. The mortality rate due to EBW increased with age and the highest values were found in the 95 + age group (Fig. 2A). Furthermore, in 2019 the number of DALYs linked with EBW in the region were highest in the 60–64 age group for both sexes. The DALY rate increased with rose age but decreased in the 80–84 age group. There were no significant sex in the DALY rates (Fig. 2B).
Numbers of deaths and death rate (A) and number of DALYs and the DALY rate (B) of diseases attributable to excess body weight in the Middle East and North Africa region, by age and sex in 2019. The right axis corresponds to the line chart and the left axis corresponds to the bar chart. DALY = disability adjusted life years. (Generated from data available from http://ghdx.healthdata.org/gbd-results-tool).
Attributable diseases
In 2019, cardiovascular diseases were the largest cause of deaths, with the highest death rates due to EBW observed in the 65–69 and 95+ categories (Fig. 3A). The death rates attributable to diabetes and kidney diseases were second in all age groups except for the 95+ age group (Fig. 3A). The DALY rate associated with cardiovascular diseases exhibited an increased up to the 75–79 age group, followed by a decreased in the 80–84 age group, before increasing over the subsequent age groups. In addition, the DALY rate attributable to diabetes and kidney diseases increased up to those aged 60–64 years old, reached a plateau in the 65–79 age groups, then declined in the 80–84 age group, before increasing over the remaining age groups (Fig. 3B).
Numbers of deaths and death rate (A) and number of DALYs and the DALY rate (B) of diseases attributable to excess body weight in the Middle East and North Africa region, by age and cause in 2019. The right axis corresponds to the line chart and the left axis corresponds to the bar chart. DALY = disability adjusted life years. (Generated from data available from http://ghdx.healthdata.org/gbd-results-tool).
Burden of diseases attributable to EBW by the Socio-demographic Index (SDI)
There was a generally positive relasionship between a country’s SDI and their corresponding age-standardized DALY rates associated with EBW. Countries like Afghanistan, Iraq, and Egypt had higher-than-expected burdens, while Yemen, Iran, Tunisia, Lebanon, Algeria, and Libya had lower-than-expected burdens. In addition, the age-standardized DALY rates increased from 1990 to 2019 in most of the MENA countries (Fig. 4).
Age- standardized DALY rates of diseases attributable to excess body weight for 21 countries from 1990 to 2019, by SDI; Expected values based on the Socio-demographic Index and disease rates in all locations are shown as the black line. Each point shows the observed age- standardized DALY rate for each country. DALY = disability adjusted life years. SDI = Socio-demographic Index (Generated from data available from http://ghdx.healthdata.org/gbd-results-tool).
Discussion
This study found that about 17% of deaths and 11% of all DALYs in MENA were attributable to EBW. Egypt, the United Arab Emirates, and Afghanistan had the highest attributable burden in 2019, whereas Iran, Yemen and Turkey had the lowest. Moreover, the EBW-attributable burden increased with advancing age and had a positive association with socioeconomic development. Cardiovascular diseases accounted for the largest number of deaths and DALYs in 2019, followed by diabetes and kidney diseases.
A previous study using GBD 2017 data showed decreases in the age-standardized death (4.7%) and DALY (2.2%) rates attributable to EBW in MENA over the period from 1990 to 20171. In contrast, in the Eastern Mediterranean Region, the death and DALY rates attributable to obesity increased by 11.0% and 13.9%, respectively, between 1990 and 201513. Our findings of a 5.1% increase in the age-standardized death rate and an 8.3% increase in the DALY rate were slightly lower than the increases observed in the Eastern Mediterranean Region. This minor differences between these two studies may be due to the different time periods measured, differences in the geographical location (e.g., Eastern Mediterranean Region vs. MENA), the reporting of age-standardized vs. all age rates, or the use of different data sources and definitions for EBW. The MENA region includes 21 countries, as mentioned in the Methods section, and the classification is based on the GBD study. In contrast, the Eastern Mediterranean Region includes 22 countries (i.e. Afghanistan, Bahrain, Djibouti, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Pakistan, Palestine, Qatar, Saudi Arabia, Somalia, Sudan, Syrian Arab Republic, Tunisia, United Arab Emirates, and Yemen) and is the classification system used by the World Health Organization. Nevertheless, there is a clear increasing trend in the age-standardized prevalence of EBW in the Eastern Mediterranean Region and globally, which suggests the potential for further increases in the EBW-attributable burden23. Furthermore, the age-standardized mortality and DALY rates of diseases due to EBW were higher in 2019 than they were in 2017, as reported by Dai and colleagues (133.6 vs. 109.5 per 100,000 for age-standardized death rates and 3777.2 vs. 3256.0 for age-standardized DALY rates)1. The results of our research underscore the importance of implementing preventive measures against EBW at various stages to mitigate the prospective disease burden lined to it.
Egypt registered the largest age-standardized mortality rate (217.7) and DALY rate (5929.6) per 100,000 in 2019, followed by Qatar, the United Arab Emirates and Afghanistan. Likewise, the GBD 2017 data indicated that Egypt had the highest age-standardized mortality (187.3 per 100,000) and DALY rates (5322.5 per 100,000) associated with high BMI1. Moreover, in Egypt, the prevalence of EBW among adolescents (aged 12–15 years) increased by 1.44 times between 2006 and 201124. The consistent relationships between high BMI and poor health outcomes in Egypt are concerning. Previous studies have indicated that, despite Egypt’s status as a high-income country, the prevalence of obesity is high not only among the educated and wealthy, but also among the less educated and less wealthy25. Furthermore, many children in Egypt tend to be overnourished. Health survey data from 2000 showed that 47% of children received more than 100% of their Recommended Daily Allowance (RDA), compared with only 14% in 199526. The increasingly sedentary lifestyles, coupled with the modernization and globalization of the food supply, have contributed to the rising obesity problem. Unfortunately, efforts to prevent and manage obesity are not currently on the Egyptian government’s agenda. This was revealed in qualitative data obtained from 25 interviews involving 22 organizations relevant to the obesity epidemic in Egypt27. Consequently, there is a need for more research and attention to generate awareness and solutions to the obesity problem in Egypt. Qatar, facing a situation akin to that of to Egypt, has recognised the significance of obesity prevention by prioritising it in the Qatari National Health Strategy (2018–22)28. Furthermore, in 2019, Yemen and Iran had among the lowest EBW-attributable burdens in MENA. Encouragingly, Iran has implemented the recommendations from the World Health Organization on Ending Childhood Obesity (WHO-ECHO), known as IRAN-ECHO, to prevent and control EBW in the Iranian population29,30. In addition, the results showed that eight countries in the Eastern Mediterranean Region, namely Afghanistan, Kuwait, Oman, the occupied Palestinian Territory, Qatar, Sudan, Syria, and Yemen, have implemented nutritional surveillance systems as part of the WHO Recommended Policies and Interventions on Healthy Diets. This initiative aims to improve nutrition in order to reduce the prevalence of EBW31.
Previous studies have consistently shown that the burden of diseases attributed to EBW was slightly higher in women compared to men, both at the global and regional levels, although these differences were relatively modest1. Moreover, research has highlighted the fact that in Middle Eastern countries and the broader Eastern Mediterranean Region, females exhibited a greater prevalence of EBW13,32. Building upon these established findings, the present study also found that the age-standardized mortality and DALY rates were higher among females, with these disparities being particularly notable among older adults. Furthermore, it is noteworthy that the 60-64 age group had the largest number of DALYs which underscores the importance of addressing this issue among those nearing retirement. In addition, the highest age-standardized rates due to EBW were identified in individuals aged 95 years and older, further reinforcing the importance of preventive measures and interventions targeting this group. These findings were also in accordance with research by Dai et al. using GBD 2017 data1. In summary, it is advisable to implement preventive measures during adolescence and among young adults to reduce the burden attributable to EBW later in life.
The current study showed that cardiovascular diseases had the highest death and DALY numbers and rates, which is consistent with the findings reported in 20171. Diabetes and kidney disease accounted for the second highest number of deaths and death rates. It’s important to note that EBW serves as a well-established risk factors for all of these conditions, with particularly strong associations with cardiovascular diseases and diabetes. Unfortunately, lipid accumulation and fatty streaks develop in young adults33, with obesity accelerating atherosclerotic changes through mechanisms such as insulin resistance and inflammation34. The presence of obesity can lead to the exacerbation of metabolic cardiovascular risk factors, such as elevated blood pressure, dyslipidemia and hyperglycemia, all of which play a significant role in the development and progression of various diseases in affected individuals. For obesity-related kidney diseases, mechanisms include activation of the renin–angiotensin–aldosterone system, systemic inflammation, endothelial dysfunction, adipokine release, insulin resistance, and hypertension35. Importantly, these modifiable risk factors can be effectively prevented and managed through improved diet and lifestyle, as shown in clinical trials36,37,38, underscoring the potential of these strategies to mitigate the disease burden associated with excess body weight.
Several preventive strategies for obesity have been developed, primarily in high-income countries like Australia39, the USA40, and the UK41, which focus on improved nutrition, physical activity, optimal sleep and stress reduction. In the MENA region, prevention strategies have been developed based on recommendations provided by the World Obesity Federation42. In addition to understanding the problem of obesity and its underlying causes, MENA prevention strategies are generally in line with those of high-income countries. However, countries in the MENA region face several different obstacles compared to those in high-income countries. These include a severely limited number of health professionals, inconsistencies in training and approaches to obesity prevention, a lack of formal sponsored guidelines, poor public transport systems, and insufficient funding for obesity research. The frameworks developed by the WHO guide obesity prevention strategies in the MENA region, encompassing both individual and societal level changes. These changes include limiting energy intake from total fats, increasing consumption of fruit, vegetables, legumes, whole grains, and nuts, restricting sugar intake, and promoting regular physical activity42. Public health prevention at the national and regional level is also being considered, including the use of mandatory food labeling, marketing restrictions, taxation of certain foods and beverages, and responsible marketing practices, especially when targeting children. The prevention of excess body weight requires multi-factorial strategies, but individual behavior change is also required.
Strengths and limitations
This study has several strengths, including the use of advanced analyses to study the burden of diseases linked to EBW, as well as its focus on the MENA region over a 30-year period. However, it also has several limitations. One of these limitations pertains to the absence of high-quality data in several low- and middle-income countries in the MENA region, a circumstance that may introduce the potential for either underestimating or over-estimating the burden associated with EBW. Moreover, the GBD study employed a different modeling system to estimate the burden in countries with no data available, meaning that the findings are based on estimations rather than real data. Secondly, certain diseases attributable to EBW, such as reproductive disorders (e.g. infertility)43, dental disorders (e.g. periodontitis)44 and psychiatric disorders (e.g. depression)45, were not reported in the present study. Thirdly, the study’s definition of overweight and obesity solely relied on BMI, a practical but imprecise measure, whereas more sophisticated methods like computed tomography, magnetic resonance imaging or dual-energy x-ray absorptiometry, which can offer greater accuracy, were not incorporated in the present study. Finally, race/ethnicity specific data were not reported, despite the known relationship between EBW and socioeconomic factors like race/ethnicity46. Additionally, data for sub-geography were not available for all 21 countries in MENA, making it impossible to report the attributable burden by sub-geography. Furthermore, in MENA there are large differences in the level of economic development, which is a predisposing factor for EBW. These shortcomings should be addressed to ensure more comprehensive and accurate estimations in the future.
Conclusions
The burden of disease associated with EBW has increased in MENA, with substantial differences between the different countries in the region. Efforts to develop and implement effective preventive programs are imperative on both the regional and national scales, especially in those countries categorized as having higher levels of socioeconomic development. Furthermore, there is a demand for primary and secondary prevention measures aimed at addressing diseases associated with EBW, especially cardiovascular diseases, neoplasms, diabetes, and kidney diseases.
Ethics approval and consent to participate
This study was approved by the Shahid Beheshti University of Medical Sciences, Tehran, Iran (IR.SBMU.PHNS.REC.1401.101) and the Tabriz University of Medical Sciences, Tabriz, Iran (IR.TBZMED.REC.1401.957).
Data availability
The data used for these analyses are all publicly available at https://vizhub.healthdata.org/gbd-results/.
References
Dai, H. et al. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: An analysis of the Global Burden of Disease Study. PLoS Med. 17(7), e1003198 (2020).
Fruh, S. M. Obesity: Risk factors, complications, and strategies for sustainable long-term weight management. J. Am. Assoc. Nurse Pract. 29(S1), S3–S14 (2017).
Sung, H. et al. Global patterns in excess body weight and the associated cancer burden. CA Cancer J. Clin. 69(2), 88–112 (2019).
Safiri, S. et al. Global, regional, and national burden of cancers attributable to excess body weight in 204 countries and territories, 1990 to 2019. Obesity 30(2), 535–545 (2022).
Zhi, X., Kuang, X. H., Liu, K. & Li, J. The global burden and temporal trend of cancer attributable to high body mass index: Estimates from the Global Burden of Disease Study 2019. Front Nutr. 9, 918330 (2022).
Zhao, G. et al. Global Burden of osteoarthritis associated with high body mass index in 204 countries and territories, 1990–2019: findings from the Global Burden of Disease Study 2019. Endocrine 79, 60 (2022).
Lin, X. et al. Global burden of noncommunicable disease attributable to high body mass index in 195 countries and territories, 1990–2017. Endocrine 69(2), 310–320 (2020).
Lee, E. Y. & Yoon, K.-H. Epidemic obesity in children and adolescents: Risk factors and prevention. Front. Med. 12(6), 658–666 (2018).
Diels, S., Vanden Berghe, W. & Van Hul, W. Insights into the multifactorial causation of obesity by integrated genetic and epigenetic analysis. Obes. Rev. 21(7), e13019 (2020).
Heindel, J. J. et al. Obesity II: Establishing causal links between chemical exposures and obesity. Biochem. Pharmacol. 199, 115015 (2022).
Hepatology, The Lancet Gastroenterology. Obesity: Another ongoing pandemic. Lancet Gastroenterol Hepatol. 6(6), 411 (2021).
Abarca-Gómez, L. et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. The Lancet. 390(10113), 2627–2642 (2017).
El Bcheraoui, C. et al. Burden of obesity in the Eastern Mediterranean Region: Findings from the Global Burden of Disease 2015 study. Int. J. Public Health. 63(1), 165–176 (2018).
Gil-Rojas, Y. et al. Burden of disease attributable to obesity and overweight in Colombia. Value Health Reg. Issues 20, 66–72 (2019).
Okunogbe, A., Nugent, R., Spencer, G., Ralston, J. & Wilding, J. Economic impacts of overweight and obesity: Current and future estimates for eight countries. BMJ Global Health. 6(10), e006351 (2021).
Brown, V. et al. The potential for long-term cost-effectiveness of obesity prevention interventions in the early years of life. Pediat. Obes. 14(8), e12517 (2019).
Farrag, N. S., Cheskin, L. J. & Farag, M. K. A systematic review of childhood obesity in the Middle East and North Africa (MENA) region: Prevalence and risk factors meta-analysis. Adv. Pediatr. Res. 4, 8 (2017).
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258), 1204–1222 (2020).
Murray, C. J. et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258), 1223–1249 (2020).
The GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377(1), 13–27 (2017).
Stanaway, J. D. et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159), 1923–1994 (2018).
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 384(9945), 766–781 (2014).
Chooi, Y. C., Ding, C. & Magkos, F. The epidemiology of obesity. Metabolism 92, 6–10 (2019).
Fan, H. & Zhang, X. Recent trends in overweight and obesity in adolescents aged 12 to 15 years across 21 countries. Pediatr. Obes. 17(1), e12839 (2022).
Aitsi-Selmi, A. et al. Interaction between education and household wealth on the risk of obesity in women in Egypt. PLOS ONE 7(6), e39507 (2012).
Hassan, H., Moussa, W. & Ismail, I. Assessment of dietary changes and their health implications in countries. Double Burd. Malnutr. Case Stud. Six Dev. Count. 84, 43 (2006).
Shahin, H. Putting the puzzle pieces together: Identifying gaps and highlighting assets for public and private entities to develop obesity programs and direct best practices in Egypt. 11(1) (2020).
Qatar MoPHo. National Health Strategy 2018–2022 2022 [Available from: https://www.moph.gov.qa/Style%20Library/MOPH/Files/strategies/National%20Health%20Strategy%202018%20-%202022/NHS%20EN.pdf
Sayyari, A. A. et al. Methodology of the comprehensive program on prevention and control of overweight and obesity in Iranian children and adolescents: The IRAN-ending childhood obesity (IRAN-ECHO) program. Int. J. Prev. Med. 8, 107 (2017).
Zahra, A. et al. Effect of an educational intervention on healthy lifestyle in Iranian children and adolescents: The Iran-ending childhood obesity (IRAN-ECHO) program. J. Nutr. Sci. Diet. 5(1), 32 (2019).
Al-Jawaldeh, A. et al. Implementation of WHO recommended policies and interventions on healthy diet in the countries of the eastern Mediterranean region: From policy to action. Nutrients 12(12), 3700 (2020).
Okati-Aliabad, H., Ansari-Moghaddam, A., Kargar, S. & Jabbari, N. Prevalence of obesity and overweight among adults in the middle east countries from 2000 to 2020: A systematic review and meta-analysis. J. Obes. 2022, 8074837 (2022).
Strong, J. P. et al. Prevalence and extent of atherosclerosis in adolescents and young adultsimplications for prevention from the pathobiological determinants of atherosclerosis in youth study. JAMA 281(8), 727–735 (1999).
McGill, H. C. et al. Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation 105(23), 2712–2718 (2002).
Stasi, A. et al. Obesity-related chronic kidney disease: Principal mechanisms and new approaches in nutritional management. Front. Nutr. 9, 925619 (2022).
de Lorgeril, M. et al. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction. Circulation 99(6), 779–785 (1999).
Collins, R. A. J., Parish, S., Sleigh, P. & Peto, R. Heart protection study collaborative group, MRC/BHF heart protection study of cholesterol-lowering with simvastatin in 5963 people with diabetes: A randomised placebo-controlled trial. Lancet 361(9374), 2005–2016 (2003).
Collaboration, B. P. L. T. T. Effects of different blood-pressure-lowering regimens on major cardiovascular events: Results of prospectively-designed overviews of randomised trials. Lancet 362(9395), 1527–1535 (2003).
Australian Government- Department of Health and Aged Care. National Obesity Strategy 2022–2032 2022 [Available from: https://www.health.gov.au/resources/publications/national-obesity-strategy-2022-2032.
Centers for Disease Control and Prevention (CDC). Overweight and Obesity 2022 [Available from: https://www.cdc.gov/obesity/strategies/index.html.
United Kingdom- Department of Health and Social Care. Tackling obesity: empowering adults and children to live healthier lives 2020 [Available from: https://www.gov.uk/government/publications/tackling-obesity-government-strategy/tackling-obesity-empowering-adults-and-children-to-live-healthier-lives.
World Obesity Federation (World Obesity). Handbook on Addressing Obesity in the MENA Region 2019 [Available from: http://s3-eu-west-1.amazonaws.com/wof-files/11344_-_WOF_-_MENA_Handbook_WEB.pdf.
Talmor, A. & Dunphy, B. Female obesity and infertility. Best Pract. Res. Clin. Obstet. Gynaecol. 29(4), 498–506 (2015).
Suvan, J., D’Aiuto, F., Moles, D. R., Petrie, A. & Donos, N. Association between overweight/obesity and periodontitis in adults. A systematic review. Obes. Rev. 12(5), e381–e404 (2011).
Mannan, M., Mamun, A., Doi, S. & Clavarino, A. Is there a bi-directional relationship between depression and obesity among adult men and women? Systematic review and bias-adjusted meta analysis. Asian J. Psychiatr. 21, 51–66 (2016).
Andrea, S. B., Hooker, E. R., Messer, L. C., Tandy, T. & Boone-Heinonen, J. Does the association between early life growth and later obesity differ by race/ethnicity or socioeconomic status? A systematic review. Ann. Epidemiol. 27(9), 583–92.e5 (2017).
Acknowledgements
We would like to thank the Institute for Health Metrics and Evaluation staff and its collaborators who prepared these publicly available data. We would also like to acknowledge the support of the Shahid Beheshti University of Medical Sciences, Tehran, Iran. This study is related to the MPH project from the Department of Epidemiology, School of Public Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran. In addition, we would also like to acknowledge the support of the Social Determinants of Health Research Center at the Tabriz University of Medical Sciences, Tabriz, Iran. We would also like to thank the Clinical Research Development Unit of Tabriz Valiasr Hospital, Tabriz University of Medical Sciences, Tabriz, Iran for their assistance in this research.
Funding
The Bill and Melinda Gates Foundation, which was not involved in any way in the preparation of this manuscript, funded the GBD study. The Tabriz University of Medical Sciences, Tabriz, Iran (Grant No 71138) also supported the present report.
Author information
Authors and Affiliations
Contributions
Si.S. and Sa.S. designed the study. Sa.S. analyzed the data and performed statistical analyses. SAN, SiS, AAK, MJMS, JAG, and NK drafted the initial manuscript. Si.S., Sa.S., and A.A.K. supervised the project. All authors reviewed the drafted manuscript for critical content. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nejadghaderi, S., Grieger, J.A., Karamzad, N. et al. Burden of diseases attributable to excess body weight in the Middle East and North Africa region, 1990–2019. Sci Rep 13, 20338 (2023). https://doi.org/10.1038/s41598-023-46702-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46702-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.