Abstract
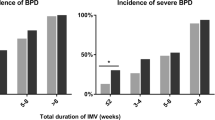
This multicenter retrospective study was conducted to explore the effects of different courses and durations of invasive mechanical ventilation (MV) on the respiratory outcomes of very low birth weight infants (VLBWI) in China. The population for this study consisted of infants with birth weight less than 1500 g needing at least 1 course of invasive MV and admitted to the neonatal intensive care units affiliated with the Chinese Neonatal Network within 6 h of life from January 1st, 2019 to December 31st, 2020. Univariate and multivariate logistic regression analyses were performed to evaluate associations between invasive MV and respiratory outcomes. Adjusted odds ratios (ORs) were computed with the effects of potential confounders. (1) Among the 3183 VLBWs with a history of at least one course of invasive MV, 3155 (99.1%) met inclusion criteria and were assessed for the primary outcome. Most infants received one course (76.8%) and a shorter duration of invasive MV (62.16% with ventilation for 7 days or less). (2) In terms of the incidence of all bronchopulmonary dysplasia (BPD) (mild, moderate, and severe BPD), there were no significant differences between different invasive MV courses [For 2 courses, adjusted OR = 1.11 (0.88, 1.39); For 3 courses or more, adjusted OR = 1.07 (0.72, 1.60)]. But, with the duration of invasive MV prolonging, the OR of BPD increased [8–21 days, adjusted OR = 1.98 (1.59, 2.45); 22–35 days, adjusted OR = 4.37 (3.17, 6.03); ≥ 36 days, adjusted OR = 18.44 (10.98, 30.99)]. Concerning severe BPD, the OR increased not only with the course of invasive MV but also with the duration of invasive MV [For 2 courses, adjusted OR = 2.17 (1.07, 4.40); For 3 courses or more, adjusted OR = 2.59 (1.02, 6.61). 8–21 days, adjusted OR = 8.42 (3.22, 22.01); 22–35 days, adjusted OR = 27.82 (9.08, 85.22); ≥ 36 days, adjusted OR = 616.45 (195.79, > 999.999)]. (3) When the interaction effect between invasive MV duration and invasive MV course was considered, it was found that there were no interactive effects in BPD and severe BPD. Greater than or equal to three courses would increase the chance of severe BPD, death, and the requirement of home oxygen therapy. Compared with distinct courses of invasive MV, a longer duration of invasive MV (> 7 days) has a greater effect on the risk of BPD, severe BPD, death, and the requirement of home oxygen therapy.
Similar content being viewed by others
Introduction
In mainland China, premature births are growing in frequency with the improved assisted reproductive technology and the increasing pregnancy rate at advanced maternal age1. However, because of immature lung development, many premature babies develop respiratory distress syndrome (RDS), apnea, pulmonary hemorrhage, and other respiratory complications, which result in the need for intubation and subsequent invasive mechanical ventilation (MV)2,3,4. Unfortunately, invasive MV is closely related to short-term and long-term complications such as atelectasis, air leak syndrome, ventilator-associated pneumonia, chronic lung disease, and neurodevelopmental disorders5,6. Therefore, an important issue faced by neonatologists is how to decrease the incidence and severity of respiratory diseases, thus reducing the need for invasive MV.
Existing studies have shown that early removal from invasive MV can lower the risk of airway injury, bronchopulmonary dysplasia (BPD), and other complications7,8. However, a considerable number of extremely preterm infants [gestational age (GA) < 28 weeks] still experience extubation failure and long-term invasive MV. 15–20% of these infants require three or more courses of invasive ventilation9. In very low birth weight infants (VLBWIs), the association between invasive MV and poor prognosis, including respiratory diseases, has not been fully clarified. Jensen et al. retrospectively analyzed the data from the US neonatal collaboration network and found that among all extremely low birth weight infants (ELBWIs), the risk of BPD was significantly higher in the multiple invasive MV courses group. However, concerning the surviving ELBWIs, the risk of BPD was not significantly different in distinct courses of invasive MV. In addition, they found that a longer duration of invasive MV was associated with a higher odds ratio (OR) of oxygen inhalation at discharge10. As far as mainland China is concerned, there has been no multicenter report on the above issues in VLBWIs. Given this situation, this paper conducted a retrospective multicenter study on VLBWIs and analyzed the effects of different courses as well as different durations of invasive MV on the respiratory outcomes of Chinese VLBWIs.
Methods
The Chinese neonatal network and database
The Chinese Neonatal Network (CHNN) is a national network of Chinese tertiary neonatal intensive care units (NICUs) with the primary goal of conducting high-quality collaborative research dedicated to the improvement of neonatal-perinatal health in China. Hospitals enrolled in CHNN are required to be tertiary referral hospitals with large neonatal services and recognized expertise in caring for high-risk neonates. In 2019, 57 NICUs in 25 provinces and municipalities contributed to the CHNN, which prospectively collects standardized data on demographics, outcomes, selected clinical practices, and resource use on all infants born at 24.0–31.9 weeks GA or with a birth weight < 1500 g and admitted to participating hospitals.
This project was approved by the CHNN Executive Committee and the Research Ethics Board at the Children’s Hospital of Fudan University, Shanghai, China11. All methods were performed by the relevant guidelines and regulations.
Study population
The population for this study consisted of infants needing at least 1 course of invasive MV with birth weight less than 1500 g and GA less than 32 weeks. The subjects were admitted to the tertiary NICUs in the CHNN within 6 h of life from January 1st, 2019 to December 31st, 2020. We excluded any infants with major congenital anomalies.
Outcome
Primary outcome: Based on the criteria of the National Institute of Child Health and Human Development 2001, BPD is defined and graded as respiratory support at 36 weeks’ postmenstrual age (PMA) or discharge (whichever is earlier). Moderate BPD is defined as the persistent need for oxygen [fraction of inspiration O2 (FiO2) < 30%] at 36 weeks’ PMA. Severe BPD is defined as the persistent need for oxygen (FiO2 ≥ 30%) and/or ventilatory support (invasive or non-invasive MV) at 36 weeks’ PMA12.
Secondary outcomes: (1) mortality; (2) incidence of patent ductus arteriosus (PDA)13; (3) incidence of necrotizing enterocolitis (NEC) (Bell stage ≥ II)14; (4) incidence of severe retinopathy of prematurity (ROP) (stage ≥ 3)15); (5) incidence of periventricular leukomalacia (PVL)16; (6) incidence of cultural-proven sepsis; (7) length of hospital stay; (8) requirement of home oxygen therapy.
Exposure variable
Invasive MV means mechanical ventilation by endotracheal tube. The number of courses and durations of invasive MV were set as the exposure variable. Consequently, the study was first divided into three groups according to different courses: (1) 1 course of ventilation; (2) 2 courses of ventilation; (3) 3 courses of ventilation or more. Moreover, the VLBWIs were divided into four groups according to different durations of invasive MV: (1) ≤ 7d; (2) 8–21d; (3) 22–35d; (4) ≥ 36d. Distinct invasive MV courses were identified if separated by more than 24 h without MV. Cases where there was an interval of less than 24 h were still considered as one course of invasive ventilation.
Statistical analysis
Descriptive statistical methods were used to summarize the study population. The characteristics and outcomes were compared for multiple comparisons using the χ2 test for categorical variables, and the Student t-test or Wilcoxon rank-sum test, as appropriate, for continuous variables. We used a multivariate logistic regression model to adjust for potential confounders that were identified in the univariate analysis or based on clinical experience and previous reference10. This includes GA, birth weight, sex, small for gestational age (SGA), 5-min Apgar score, treatment with surfactant, treatment with dexamethasone (DART), PDA, NEC, cultural-proven sepsis during hospitalization, invasive MV duration, invasive MV course. To explore the effect of courses and duration of ventilation on BPD, we used the above model for determining adjusted ORs. In addition, the interaction effect between invasive MV duration and invasive MV course was also considered for further analysis.
Besides, we conducted subgroup analysis stratified by GA groups (GA ≤ 26 weeks, 26w < GA ≤ 28weeks, and GA ≥ 28 weeks) using the same multivariate logistic regression model (Supplements- supplementary tables). Data management and all statistical analysis were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA). The two-sided p-value of 0.05 was used to determine statistical significance.
Statement of ethics
This study was approved by the Ethics Review Board of Children’s Hospital of Fudan University, Approval No. 2018296. The requirement for informed consent was waived by the Ethics Review Board of the Children’s Hospital of Fudan University.
Results
Characteristics of the study participants
Among the 3183 VLBWs with a history of at least one course of invasive MV, 28 infants with major congenital anomalies were excluded. 3155 (99.1%) were finally included and assessed for the primary outcome. Demographic characteristics are given in Table 1. GA, birth weight, male, DART treatment, surfactant treatment, and invasive MV duration exhibited significant differences between distinct courses of invasive MV. Meanwhile, GA, birth weight, male, SGA, 5 min Apgar, DART treatment, surfactant treatment, and invasive MV courses showed statistical differences among groups with different invasive MV durations. Most infants received one course [76.8%] and a shorter duration of invasive MV [62.16% with ventilation for 7 days or less]. (Table 1).
Outcomes
It was found that the requirement of home oxygen therapy, length of hospital stay as well as incidences of BPD, severe BPD, PDA, NEC (Bell stage ≥ II), sepsis, severe ROP (stage ≥ 3), and death showed increasing trends with the ventilation courses growing. Similar results could be found among different invasive MV durations. (Table 2).
Adjusted ORs for respiratory outcomes
As far as BPD is concerned, there were no significant differences between different ventilation courses. Compared with that, the OR of BPD increased with the duration of invasive MV prolonging. With regard to severe BPD and death, the ORs evidently increased not only with the course of invasive MV but also with the duration of invasive MV. In comparison with the course of MV, the ventilation duration had a greater impact on the need for home oxygen therapy and the requirement of MV at discharge. (Table 3).
In addition, when the interaction effect was considered, it was found that death and requirement of home oxygen therapy showed significant interactive effect with invasive MV duration and invasive MV course. Compared with the above outcomes, there were no interactive effects in BPD, severe BPD, and the requirement of non-invasive/invasive MV at discharge. (Table 4).
Discussion
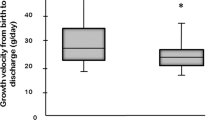
Due to immature development of lung and cerebral respiratory center, it is not uncommon for VLBWIs requiring reintubation after extubation failure. In mainland China, although there have been no large multicenter studies, according to recent cohort studies from other parts of the world, nearly 50% of VLBWIs and 60–70% of ELBWIs need at least two or more courses of invasive MV during hospitalization17,18. Shalish et al. found that reintubation was associated with lower gestational age/birth weight and greater morbidities compared with infants never reintubated in 216 newborns whose birth weight ≤ 1250 g19. Yossef et al. included 210 patients born at < 27 weeks from 2005 to 2011. They further found that long-term intermittent positive pressure ventilation patients were born earlier and had lower birth weight20. Markestad et al. performed a prospective observational study of 636 infants with a GA of 22–27 weeks or a birth weight of 500–999 g. For the survivors, days of invasive MV decreased from a median of 37 days to 3 days, and the proportion in need of oxygen at 36 weeks’ PMA decreased from 67 to 26% at 23 and 27 weeks’ GA, respectively21. The above evidence reflects the trend that more courses and longer duration of invasive MV are needed with decreasing GA and birth weight.
Because the course and duration of invasive MV are related to many potential reasons such as GA, birth weight, as well as sex. Besides the above known self-factors, the surfactant replacement and DART treatment are also closely associated with invasive MV. With the promotion of surfactant and dexamethasone therapies in the past several years, the application and duration of invasive MV have significantly been reduced and shortened. Our study found that the application of DART increases as the course and duration of invasive MV grow (Table 1). A similar growth trend can also be seen in surfactant administration (Table 1). This, to some extent, indicates that newborns who require multiple and long-term invasive MV have worse lung development and maturity. Univariate analysis of the outcomes firstly showed that multiple courses and longer duration of invasive MV are associated with the increased risks of BPD, severe BPD, PDA, death, sepsis, severe ROP, home oxygen therapy as well as longer hospital stay (Table 2). The above association has been partly confirmed by literature. For example, Tseng et al. found that invasive MV significantly increased the risk of ROP in a multicenter cohort study (n = 1,703,326, p < 0.0001)22. And, a persistent left-to-right shunt through PDA may impair pulmonary mechanics and is correlated with prolonged invasive MV needs23. In addition, Morrow et al. once performed a retrospective analysis of 660 newborns (GA ≤ 32 weeks) with BPD. The result showed that longer hospitalization was closely associated with invasive MV, supplemental oxygen need, etc24.
Through further multivariate analysis, we evaluated the effect of longer duration and multiple courses of invasive MV on respiratory outcomes. In terms of BPD and severe BPD, it was found that longer duration not only increased the incidence of BPD, but also the risks of severe BPD and home oxygen therapy (Tables 3 and 4). In fact, the incidences of BPD and severe BPD have been proven associated with the duration of invasive MV. Previous studies have explored the association between the duration of invasive MV and BPD. For example, a retrospective whole-population study including all infants with GA < 28 weeks from the UK (n = 11,806) found invasive MV duration had areas under the curve of 0.793 and 0.703 in predicting BPD and home oxygen therapy, respectively. MV for more than 8 days predicted BPD development with 71% sensitivity and 71% specificity25. A prospective multicenter cohort study included 6,538 infants born at 23–31 weeks of GA who were admitted to 47 NICUs in China from January 2018 to December 2021. It further revealed that the onset of moderate-to-severe BPD was significantly associated with the duration of initial invasive MV (adjusted OR 1.97; 95% CI 1.10–2.67)26. For severe BPD, a single-center, retrospective cohort study included infants born at 22.0–25.9 weeks during 2005–2009 (88 infants in the early era) and 2011–2015 (102 infants in the late era), which was before and after implementing guidelines recommending delayed extubation. The result showed that the incidence of severe BPD was significantly higher, and the duration of invasive MV was longer in the late era (after adopting delayed extubation)27.
Except for the duration, the number of courses of invasive MV is another possible factor associated with BPD. But the evidence so far is mixed. Subgroup analysis of two large randomized controlled trials showed that reintubation within 5 and 7 days after extubation is associated with an increased incidence of respiratory diseases including BPD28,29. But, a single-center retrospective study (n = 244) from Li et al. found that reintubation was not an independent risk factor for moderate-to-severe BPD (for reintubations occurring within 72 h after extubation, adjusted OR = 1.714, 95% CI 0.546–5.374; for reintubations occurring within 7 d after extubation, adjusted OR = 1.501, 95% CI 0.482–4.678)30. Shalish W et al. found that reintubation within observation windows ranging from 24 h to 3 weeks post-extubation was not associated with the increased ORs of BPD among survivors19. However, the above studies did not consider the interference of the ventilation duration as an important confounding factor. A multicenter retrospective study from Jensen et al. further showed that reintubation did not increase the risk of discharge on oxygen. More importantly, invasive MV for less than 3 courses did not increase the risk of BPD. Only in the population with more than 4 courses of invasive MV [MV duration 59 (41–87) days] did the risk of BPD increase compared with those infants with only 1 course [OR 1.44 (1.04–2.01)]10. Our study also found that multiple courses of invasive MV did not increase the risk of BPD (Tables 3 and 4). But, Jensen’s study did not consider the effect of different courses on the incidence of severe BPD. According to our findings, it turns out that distinct invasive MV courses would increase the risk of severe BPD, even considering the interaction effect between invasive MV duration and invasive MV course. As a matter of fact, the need for multiple courses of invasive MV generally means severe immature lung development, repeated pulmonary infection, or tracheomalacia in clinical practice. And those reasons are high-risk factors or important features of severe BPD. Furthermore, our results firstly manifested that after adjusting for confounding factors, multiple courses, especially greater than or equal to three courses would also increase the chance of death and requirement of home oxygen therapy. This could also be attributed to the elevated risk of severe BPD.
Limitations
The main limitation of this study lies in the retrospective study design. And some factors such as the sample size of infants with severe BPD limit the reliability of the above results. It needs to be further studied by expanding the sample size in the future. In addition, extubation failure is an important and complicated issue. Extubation failure is common in extremely premature infants. However, many factors are related to extubation failure, such as lower birth weight, smaller GA, weaker spontaneous breath, different modes of MV, pneumonia, low vitality, etc. Since it is not the main objective of our research, the number of extubation failures and detailed time interval between two consecutive invasive MV were not further explored and included in this study.
Conclusion
In conclusion, greater than or equal to three courses would increase the chance of severe BPD, death and requirement of home oxygen therapy. Compared with distinct courses of invasive MV, the longer duration of invasive MV (more than 7 days) has a greater effect on the risk of BPD, severe BPD, death, and requirement of home oxygen therapy.
Data availability
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
References
Cavoretto, P. et al. Risk of spontaneous preterm birth in singleton pregnancies conceived after IVF/ICSI treatment: meta-analysis of cohort studies. Ultrasound Obstet. Gynecol. 51(1), 43–53. https://doi.org/10.1002/uog.18930 (2018).
Donda, K. et al. Trends in epidemiology and outcomes of respiratory distress syndrome in the United States. Pediatr. Pulmonol. 54(4), 405–414. https://doi.org/10.1002/ppul.24241 (2019).
Fauroux, B. et al. Risk factors for bronchiolitis hospitalization in infants: A French nationwide retrospective cohort study over four consecutive seasons (2009–2013). PLoS One 15(3), e0229766. https://doi.org/10.1371/journal.pone.0229766 (2020).
Niesłuchowska-Hoxha, A. et al. A retrospective study on the risk of respiratory distress syndrome in singleton pregnancies with preterm premature rupture of membranes between 24+0 and 36+6 weeks, using regression analysis for various factors. Biomed. Res. Int. 2018, 7162478. https://doi.org/10.1155/2018/7162478 (2018).
Wielenga, J. M. et al. Protocolized versus non-protocolized weaning for reducing the duration of invasive mechanical ventilation in newborn infants. Cochrane Database Syst. Rev. 3, CD011106. https://doi.org/10.1002/14651858.CD011106.pub2 (2016).
Steer, P. et al. High dose caffeine citrate for extubation of preterm infants: A randomised controlled trial. Arch. Dis. Child Fetal Neonatal Ed. 89(6), F499-503. https://doi.org/10.1136/adc.2002.023432 (2004).
Sant’Anna, G. M. & Keszler, M. Weaning infants from mechanical ventilation. Clin. Perinatol. 39(3), 543–562. https://doi.org/10.1016/j.clp.2012.06.003 (2012).
Schmidt, B. et al. Long-term effects of caffeine therapy for apnea of prematurity. N. Engl. J. Med. 357(19), 1893–1902. https://doi.org/10.1056/NEJMoa073679 (2007).
Kirpalani, H. et al. A trial comparing noninvasive ventilation strategies in preterm infants. N. Engl. J. Med. 369(7), 611–620. https://doi.org/10.1056/NEJMoa1214533 (2013).
Jensen, E. A. et al. Effects of multiple ventilation courses and duration of mechanical ventilation on respiratory outcomes in extremely low-birth-weight infants. JAMA Pediatr. 169(11), 1011–1017. https://doi.org/10.1001/jamapediatrics.2015.2401 (2015).
Cao, Y. et al. Chinese neonatal network. Assessment of neonatal intensive care unit practices, morbidity, and mortality among very preterm infants in China. JAMA Netw. Open. 4(8), e2118904. https://doi.org/10.1001/jamanetworkopen.2021.18904 (2021).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respi. Crit. Care Med. 163(7), 1723–1729. https://doi.org/10.1164/ajrccm.163.7.2011060 (2001).
Sehgal, A. & McNamara, P. J. Does echocardiography facilitate determination of hemodynamic significance attributable to the ductus arteriosus?. Eur. J. Pediatr. 168(8), 907–914. https://doi.org/10.1007/s00431-009-0983-3 (2009).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187(1), 1–7. https://doi.org/10.1097/00000658-197801000-00001 (1978).
International Committee for the Classification of Retinopathy of Prematurity. The International classification of retinopathy of prematurity revisited. Arch. Ophthalmol. 123(7), 991–999. https://doi.org/10.1001/archopht.123.7.991 (2005).
Agut, T. et al. Preterm white matter injury: Ultrasound diagnosis and classification. Pediatr. Res. 87(1), 37–49. https://doi.org/10.1038/s41390-020-0781-1 (2020).
Shalish, W. et al. Patterns of reintubation in extremely preterm infants: A longitudinal cohort study. Pediatr. Res. 83(5), 969–975. https://doi.org/10.1038/pr.2017.330 (2018).
Caffarelli, C. et al. Best practices, challenges and innovations in pediatrics in 2019. Ital. J. Pediatr. 46(1), 176. https://doi.org/10.1186/s13052-020-00941-1 (2020).
Shalish, W. et al. The impact of time interval between extubation and reintubation on death or bronchopulmonary dysplasia in extremely preterm infants. J. Pediatr. 205, 70-76.e2. https://doi.org/10.1016/j.jpeds.2018.09.062 (2019).
Yossef, L., Shepherd, E. G., Lynch, S., Reber, K. M. & Nelin, L. D. Factors associated with long-term mechanical ventilation in extremely preterm infants. J. Neonatal Perinatal Med. 11(1), 29–35. https://doi.org/10.3233/NPM-181711 (2018).
Markestad, T. et al. Early death, morbidity, and need of treatment among extremely premature infants. Pediatrics 115(5), 1289–1298. https://doi.org/10.1542/peds.2004-1482 (2005).
Tseng, H. C. et al. Population based retrospective cohort study on risk of retinopathy of prematurity in twins. PLoS One 15(3), e0230346. https://doi.org/10.1371/journal.pone.0230346 (2020).
Clyman, R. I. Patent ductus arteriosus, its treatments, and the risks of pulmonary morbidity. Semin. Perinatol. 42(4), 235–242. https://doi.org/10.1053/j.semperi.2018.05.006 (2018).
Morrow, C. B., McGrath-Morrow, S. A. & Collaco, J. M. Predictors of length of stay for initial hospitalization in infants with bronchopulmonary dysplasia. J. Perinatol. 38(9), 1258–1265. https://doi.org/10.1038/s41372-018-0142-7 (2018).
Dassios, T., Williams, E. E., Hickey, A. & Greenough, A. Duration of mechanical ventilation and prediction of bronchopulmonary dysplasia and home oxygen in extremely preterm infants. Acta Paediatr. 110(7), 2052–2058. https://doi.org/10.1111/apa.15801 (2021).
Dou, C. et al. Longer duration of initial invasive mechanical ventilation is still a crucial risk factor for moderate-to-severe bronchopulmonary dysplasia in very preterm infants: A multicentrer prospective study. World J. Pediatr. https://doi.org/10.1007/s12519-022-00671-w (2023).
Söderström, F., Ågren, J. & Sindelar, R. Early extubation is associated with shorter duration of mechanical ventilation and lower incidence of bronchopulmonary dysplasia. Early Hum. Dev. 163, 105467. https://doi.org/10.1016/j.earlhumdev.2021.105467 (2021).
Manley, B. J., Doyle, L. W., Owen, L. S. & Davis, P. G. Extubating extremely preterm infants: Predictors of success and outcomes following failure. J. Pediatr. 173, 45–49. https://doi.org/10.1016/j.jpeds.2016.02.016 (2016).
Chawla, S. et al. Eunice Kennedy shriver national institute of child health and human development neonatal research network. Markers of successful extubation in extremely preterm infants, and morbidity after failed extubation. J. Pediatr. 189, 113-119.e2. https://doi.org/10.1016/j.jpeds.2017.04.050 (2017).
Li, J. et al. The impact of time interval between first extubation and reintubation on bronchopulmonary dysplasia or death in very low birth weight infants. Front. Pediatr. 25(10), 867767. https://doi.org/10.3389/fped.2022.867767 (2022).
Acknowledgements
We thank the data abstractors from the Chinese Neonatal Network. We thank all the Chinese Neonatal Network coordinating center staff for providing organizational support (Lin Yuan, Ph.D.; Tong-ling Yang, RN; Hao Yuan, RN; Li Wang, RN; Yu-lan Lu, Ph.D.). We thank MS. Dianna for revising this manuscript.
Funding
Shoo K. Lee is supported by the Canadian Institutes of Health Research (CTP87518).
Author information
Authors and Affiliations
Consortia
Contributions
R.C. supervised the study; She also conceptualized and designed the study. S.K.L., J.S., and Y.C. supervised the study. Y.Y. conceptualized and designed the study; drafted the manuscript; and acquired, analyzed, and interpreted the data. Z.L. and S.P. helped design this study. J.W. revised this manuscript. X.G. acquired, analyzed, and interpreted the data. All authors critically revised the manuscript for important intellectual content, approved the final manuscript as submitted, and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, Y., Gu, Xy., Lin, Zl. et al. Effect of different courses and durations of invasive mechanical ventilation on respiratory outcomes in very low birth weight infants. Sci Rep 13, 18991 (2023). https://doi.org/10.1038/s41598-023-46456-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46456-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.