Abstract
Burn injuries are among the common traumatic injuries, which can be accompanied with lifelong morbidity and mortality. The Lethal Area Fifty Percent (LA50) index is another reliable outcome measurement tool that assesses the standard of medical care at burn centers. It is widely used as a benchmark for assessing the quality of burn care and is considered the percentage at which 50% of burn patients are expected to die because of burn-related injuries. We aimed to determine and compare the LA50 in burn patients admitted to Shiraz Burn Referral Centers in 2018–2021 and 2011–2018 with regard to improving the quality of special care and infection control in the new hospital. We conducted a retrospective cohort analysis on patients admitted to Amir al-Momenin Burn Injury Hospital in Shiraz, Fars, Southern Iran. Data were retrospectively gathered from March 2011 to January 2022, and subsequently analyzed with standard statistical analysis, and also multivariate and probability analysis. A total of 7382 patients with acute burns injuries were identified. Among them, 4852 (65.7%) patients were men, and the median age was 27 years [Q1–Q3 7–40; range 1–98]. Most of the patients were in the pediatric and early adulthood age range, with 76.2% being younger than 40 years old. The median TBSA was 24% [IQR 14, 43], and the median duration of hospitalization was 11 [IQR 11] days. Most injuries were secondary to flame and fire (33.5%; n = 2472). The mortality rate in our study was 19.0% (n = 1403). We evaluated our patients based on two main time intervals: March 2011 till February 2018 (n = 3409; 46.2%), and March 2018 to January 2022 (n = 3973; 53.8%). Based on multivariate analysis, the second interval of our study was significantly correlated with a more female patients, higher age, lower TBSA, less burn injuries due to scald, contact, but more frequent fire and flame injuries, and also lower mortality rate. Factors correlated with higher mortality included male gender, older age, shorter hospitalization duration, higher TBSA, etiology of fire and flame, and accidental burn injuries. A Baux score of 76.5 had a sensitivity of 81.1%, specificity of 87.3%, accuracy of 86.1% in predicting mortality among our patients. The mortality probability for the study intervals were 20.67% (SD 33.0%) for 2011–2018, and 17.02% (SD 29.9%) for 2018–2022 (P < 0.001). The LA50 was 52.15 ± 2 for all patients. This ammount was 50 ± 2% in 2011–2018, and 54 ± 2 in 2018–2022 (P < 0.001). The mean LA50 values showed significant improvements following significant modifications in our critical care for burn victims, including augmented intensive care unit capacity, prompt relocation of inhalation burn cases to the intensive care unit, establishing a well-trained multidisciplinary team, and improved infection control. To improve outcomes for burn patients in developing countries, major changes should be made in the management of burn patients and LA50 is a reliable assessment tool for evaluating the how these changes affect patient’s outcomes.
Similar content being viewed by others
Introduction
Burn injuries are considered a common cause of trauma that significantly affects patients’ life, resulting in high morbidity and mortality, particularly in developing countries1,2,3,4,5,6. The classification of burns typically relies on their underlying cause, with thermal, electrical, and chemical injuries being the most commonly recognized categories7. The optimal management of burn patients has been a subject of significant debate, which can be costly, requiring prolonged hospitalization that can potentially lead to life-long sequelae7,8. It requires a comprehensive and interdisciplinary approach from the initial critical stage to recovery and rehabilitation9.
Recent developments in burn management, including optimal tissue excision and grafting, enhanced infection prevention and control measures, specialized critical care interventions, as well as tailored nutritional interventions have collectively contributed to the reduction of mortality rates in burn patients10,11. To assess the outcomes of burn patients, multiple factors must be considered including survival rate, wound healing, functional status, burn-related complications, and overall mortality rate. The Lethal Area Fifty Percent (LA50) index is another reliable outcome measurement tool that assesses the standard of medical care at burn centers. It is widely used as a benchmark for assessing the quality of burn care and is considered the percentage at which 50% of burn patients are expected to die because of burn-related injuries12,13. Repeated measurements of this index can be used to determine the effectiveness of burn care to patients.
The estimated LA50 in the United States at its first description in 1940s was nearly 40%14. Nevertheless, significant improvements in burn and critical care management through the past decades led to a current LA50 value of nearly 90%15, meaning that patients now have a greater likelihood of surviving extensive burn injuries. In the developing countries however, the mortality rates are still high and there is not enough evidence about their LA50 values. After to 2018, our burn center witnessed significant modifications in the critical care for burn victims, including augmented intensive care unit capacity, prompt relocation of inhalation burn cases to the intensive care unit, and the integration of high-efficiency particulate air filters for the burn units. Subsequently, this study was designed to compare the outcomes of our patients prior and after this modification. Moreover, the study aims to characterize the changes in LA50 subsequent to these advancements in burn care.
Materials and methods
Study design and setting
We conducted a retrospective cohort analysis of patients admitted to Amir al-Momenin Burn Injury Hospital in Shiraz, a 75-bed tertiary care hospital that serves as a burn and plastic surgery referral center for over five million people in Fars province. Data were retrospectively gathered from March 2011 to January 2022, and patients were grouped throughout two consecutive time periods (2011–2018 and 2018–2022).
The database registry was initiated by Burn and Wound Healing Research Center located in Amir-al Momenin Hospital. The data element for this database questionnaire was designed by clinicians and epidemiologists. Dedicated clinical research assistants collected all data using a standardized electronic case report form. To remove mistakes caused by missing or inconsistent data, an extra researcher verified the correctness of data entry for 15% of patients. The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines of cohort studies was used for reporting and writing this study.
Study population
All patients admitted to Amir al-Momenin Burn Injury Hospital for acute burn injuries between March 2011 and January 2022 were included in our study. To focus our study on patients with burn injuries and receiving related in-hospital treatment, we excluded cases with concurrent additional serious injuries and traumas who were initially admitted to a primary trauma center, such as head trauma, major torso trauma, or long bone fractures, or those who died in the emergency department (dead-on-arrival) or were admitted for less than 24 h and did not have the opportunity to receive medical services, or without a comprehensive registry of medical records. Based on our hospital policy, all patients were evaluated during the first hour of admission and transferred to either the appropriate ward or the intensive care unit (ICU).
Data sources
Data were obtained from the Health Information System (HIS)—a population-based administrative database that tracks all care hospitalizations in the province of Fars, and also patient medical records. Collected data included demographical features such as age, gender, and admission year, and also clinical features such as etiology of burn injuries (defined by Herndon et al.6,16 and also previous studies, including flame burn, scald burn, contact burn, electrical burn, chemical burn, and explosion/blast burn), the reason of burn injuries (accident, suicide or homicide), total body surface area (% TBSA) burnt, length of hospitalization, and patient outcomes (mortality, transfer, discharge, and left against medical advice).
Ethical considerations
The ethical review committee of the Shiraz University of Medical Sciences (Ethical approval code: IR.SUMS.MED.REC.1400.638) approved the study. All experiments were performed in accordance with relevant guidelines and regulations. Based on the retrospective nature of the study, written informed consent waiver was approved by the Ethics committee of Shiraz University of Medical Sciences. Patients’ information were anonymized prior to analysis and confidentiality was assured by the researcher.
Statistical analysis
Data were initially entered into SPSS version 26.0 (SPSS Inc., Chicago, Illinois, USA) and subsequently analyzed. Qualitative data were presented in frequency, and percentages (%). Based on the skewed distribution of quantitative variables such as length of hospitalization, TBSA, and age, these variables were reported using the median, quartiles [Q1–Q3] and interquartile range [IQR]. The Mann–Whitney U and Kruskal Wallis test was done to compare the medians of two categorical variables, while the Chi-square test was used to compare categorical data.
In addition, binary univariable logistic regression was utilized to quantify the influence of a probable underlying factor on mortality in patients with acute burns by classifying the patients' outcomes as mortality or survival. Then, multivariable logistic regression was performed to modify the influence of factors whose P values were less than 0.2 in univariable logistic regression. The odds ratio (OR) and its associated 95% confidence interval were reported. In addition, the lethal area fifty percentage (LA50) is defined as the TBSA of burn with a 50% probability of death in the patient and was calculated in our study using a Probit model. We also calculated the Baux score in our patients, which is the sum of TBSA and the patients age, and evaluated its correlation with mortality along with assigning a relative cut-off based on receiver operating characteristic (ROC) curve analysis17. All tests were two-tailed, and a P value of less than 0.05 was considered the threshold for statistical significance.
Ethics approval and consent to participate
The present study was approved by the medical ethics committee of the academy. The permission was obtained from the medical ethics committee of Shiraz University of Medical Sciences. Based on the retrospective nature of our study, written informed consent was waived by the Ethics committee of Shiraz University of Medical Sciences, and their information was obtained from their hospital records. Permission to carry out the study and access patient records was sought from the Shiraz University of Medical Science administrators and the study was conducted in compliance in accordance with the relevant guidelines and regulations and the Declaration of Helsinki and was also approved by the ethics committee of the university.
Results
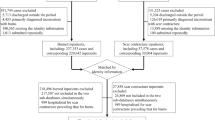
During the study period (2011–2022), a total of 7382 patients with acute burns injuries who fulfilled the study’s inclusion criteria were identified. Among them, 4852 (65.7%) patients were men, and the median age was 27 years [Q1–Q3 7–40; range 1–98] (Fig. 1). The baseline features of the patient and injury in our study and a comparison between 2011–2018 and 2018–2022 are shown in Table 1. We evaluated our patients based on two main time intervals: March 2011 till February 2018, and March 2018 to January 2022. The first interval included 3409 (46.2%) of the patients, while the second interval consisted of 3973 (53.8%) patients, demonstrating an annual rate of 487 cases and 993 cases (2.04-fold increase).
Most of the patients were in the pediatric and early adulthood age range, with 76.2% being younger than 40 years old. In addition, patients were significantly younger during the first interval of our study period (P < 0.001) and the age distribution shifted towards older ages during the last four years, especially among the 41– 60 and above 60 age group (from 14.4 to 18.0% and 5.5 to 9.1%, respectively) (Fig. 2). The median age was similar across the sexes (P = 0.509). However, the incidence of burn injuries among male patients significantly increased during our timeframe, in which the proportion of male patients increased from 63% in 2011–2018 to 68% in the 2018–2022 (OR = 0.797, CI 95% 0.724–0.878; P < 0.001).
The median TBSA throughout our study was 21% [IQR 28], which was significantly higher in females than males (24% [IQR 33] and 20% [IQR 26], respectively; P < 0.001). The median TBSA was 16%, 27%, 23% and 17% for under 21, 21–40, 41–60 and above 60 age group, respectively. Furthermore, there was a considerable drop in TBSA in 2018–2022 compared to 2011–2018 (18% [IQR 27] vs. 24% [IQR 29], respectively; P < 0.001).
We had 80 patients with TBSA of 100%, which all died after a median of 3 days (range 2–17), with 29 (37.2%) of them during the initial 48, and 16 (20.5%) during the initial 72 h.
Most injuries were secondary to flame and fire (33.5%; n = 2472), followed by an explosion/blast (27.4%; n = 2023) and scald (22.2%; n = 1642) burns, while a small proportion (1.2%; n = 92) were chemical in nature (Fig. 3). There was a significant increase in causes of burn due to scald (from 20.7% to 23.6%; OR 1.184; CI 95% 1.060–1.322; P = 0.003) and objects (1.2% to 4.8%; OR 4.026; CI 95% 2.873–5.642; P < 0.001), but a significant decrease in causes of burn due to fire (38.4–29.4%; OR 0.667; CI 95% 0.605–0.735; P < 0.001).
On the other hand, accidental burns grew with time (from 86.9% in 2011–2018 to 93.5% in 2018–2022; OR 2.159; CI 95% 1.838–2.536), but suicide burns dropped over time (from 11.5% in 2011–2018 to 5.3% in 2018–2022; OR 0.426; CI 95% 0.357–0.507; P < 0.001), however, homicidal changes were not significant (1.5% vs. 1.3% for 2011–2018 and 2018–2022, respectively; P = 0.299). Causes of suicide were documented in the recent years (2018–2022), in which the most common cause was family issues (71.29%), followed by mental health issues (20.57%), and financial issues (2.39%).
The total median duration of hospitalization was 11 [IQR 11] days, with no significant difference based on gender (P = 0.118). However, In the latter four years of the research, hospital stays were considerably shorter than in the first four (11 [IQR 10] vs. 12 [IQR 12], respectively; P < 0.001). Also, there was a significant decrease in hospital stay as the date of the year increases (Correlation Coefficient − 0.038; P = 0.001), and a significant increase in duration with the increase of age (Correlation Coefficient 0.100; P < 0.001).
Regarding patient’s outcomes, 19.0% (n = 1403) died, 72.7% (n = 5352) were discharged, 0.4% (n = 30) were transferred to other hospitals, 7.6% (n = 558) left against medical advice. Meanwhile, the mortality rate was significantly higher among male patients (male/female 52.6% vs. 47.4%; OR 1.988; CI 95% 1.766–2.237; P < 0.001). We achieved a significant decrease in mortality rates from the first interval to the second interval of our study period, in which the mortality rate in 2011–2018 was 21.5%, while in 2018–2022 was 16.9% (OR 0.741; CI 95% 0.659–0.832; P < 0.001). When evaluating the changes in mortality patterns among gender, there was a significant decrease in female mortality rates throughout the two study intervals (30.6% vs. 22.1% for 2011–2018 and 2018–2022, respectively; OR 0.642; CI 95% 0.537–0.768; P < 0.001); however, this change was not significant among male patients (16.2% vs. 14.5% for first and second interval, respectively; P = 0.093). Furthermore, the pattern of decrease in mortality was significant among all age groups (≤ 20: OR 0.660, P = 0.001; 21–40: OR 0.765, P = 0.003; 41–60: OR 0.686, P = 0.006; > 60: OR P = 0.004).
We evaluated our data based on univariate and multivariate analysis, to access factors correlated with burn patient mortality. As demonstrated in Table 2, the second interval of our study (2018–2022) was significantly correlated with a lower mortality rate compared to the first interval (2011–2018). Further risk factors for mortality included male gender, older age, shorter hospitalization duration, higher TBSA, etiology of fire and flame, and accidental burn injuries (Table 2).
We also evaluated our data based on univariate and multivariate analysis, to access factors correlated with the study intervals. As demonstrated in Table 3, compared to the first interval (2011–2018), the second interval of our study (2018–2022) was significantly correlated with a more female patients, higher age, lower TBSA, less burn injuries due to scald, contact, but more frequent fire and flame injuries, and also lower mortality rate (Table 3).
After adjusting variables based on cofounding factors explored in the multiple regression analysis, the overall average probability of death in our study was 18.71%. The mortality probability for the study intervals were 20.67% (SD 33.0%) for 2011–2018, and 17.02% (SD 29.9%) for 2018–2022 (P < 0.001). Figure 4 demonstrates the probability of mortality among the variables in our study.
The LA50 was 52.15 ± 2 for all patients. This ammount was 50 ± 2% in 2011–2018, and 54 ± 2 in 2018–2022 (P < 0.001).
We also calculated the Baux score in our study, in which ranged from 2 to 186 [Median 53; IQR 49]. The Baux score was significantly higher during 2018–2022 compared to 2011–2018 (P < 0.001), and also significantly higher in patients who passed away (P < 0.001). Furthermore, the Baux score had a significant direct correlation with probability of mortality in our study (Correlation coefficient 0.901; P < 0.001). Based on ROC curve analysis, with an AUC of 0.926, the Baux score demonstrated a satisfactory correlation with mortality. Based on Fig. 5, a Baux score of 76.5 had a sensitivity of 81.1%, specificity of 87.3%, accuracy of 86.1%, positive predictive value of 60.1%, negative predictive value of 95.1% in predicting mortality among our patients.
Discussion
This study was primarily designed to investigate patient’s outcomes between two time intervals of 2011–2018 and 2018–2021, when significant modifications have been made to our approach toward management of critically ill burn victims. These modifications include rapid transfer of severe burn patients to the ICU, establishing a well-trained multidisciplinary team, improved infection control, and utilization of specialized equipment for the management of burn patients. Our findings showed that the overall mortality was significantly decreased in patients after these modifications. In addition, this study showed a significant increase in LA50 value between the two time frames, which is an indicator of improved healthcare to the burn patients.
Generally, the LA50 value is an efficient indicator for the quality of healthcare given, particularly for patients with more severe burns13. It’s considered a useful standard for comparing critical care quality among burn centers or across different time periods. When we compare our results to the reports of developed countries, our results were considerably lower in terms of LA50 value. For instance, Tung et al.18 reported an approximate LA50 value of 80% TBSA for their patients with a mortality rate of 3.1%, which compared to our study was significantly lower18. A significant contributing factor to this difference could be that their study population had a mean burn area of 14% TBSA, which was considerably lower than our study where it was 24%. As our study findings suggested that TBSA is a major risk factor for higher mortality in burn patients.
Jeevan et al.19 found results similar to ours, with a mean LA50 of 60% TBSA estimated for burn patients in the UK. They also observed that age is a significant risk factor for increased mortality, as evidenced by LA50 values of 71.08% for patients aged 15–44, 56.64% for those aged 45–64, and 28.82% for those aged 65 and19. Our results showed similar findings that age is a significant factor contributing to higher mortality and lower LA50 values. Similar results were observe in the study by Roberts et al.17, showing lower LA50 values in advanced ages.
Reports from the developing countries showed lower rates of survival following burn injuries20,21, which points to the significance of critical care managements of burn victims. However, the same correlation between age and LA50 was observed. For instance, the LA50 for adults in a report from Kuwait was 76.5%, whereas for the elderly, it was 41.8%20. To improve outcomes for burn patients in developing countries, it appears that significant modifications in critical management, as well as the implementation of more educational and preventive programs, may be necessary. As shown by our results, implementing these changes can lead to significant improvements in patient outcomes. Aside from the changes in the LA50 value, significant changes in the Baux index across the two time intervals demonstrated similar trend in terms of patient’s outcomes. In contrast with recent literature, our findings suggested that male sex is a risk factor for unfavorable outcomes in burn patients. The results of both univariate and multivariate regression analyses in our study revealed that men are more likely to have lower LA50 values in both time intervals, compare with women. Aside from the LA50 values, the overall rate of mortality was significantly higher in men (male/female 52.6% vs. 47.4%). Also, our results indicated that the there was no difference regarding the duration of hospital stay between the two genders, which was in contrast with previous publications.
Numerous studies have examined gender differences and the influence of gender on outcomes after burn injuries. Many of these reports have shown that women have a lower proportion of injuries, smaller burn extent, and a higher incidence of scald burns compared to men, and are at a greater risk for unfavorable outcomes with extensive burn injuries, particularly with TBSA of more than 50%22,23,24. Christofides et al.25 reported a greater risk (OR 2.17) of mortality among female patients in South Africa. Research on burn populations in Australia and New Zealand similarly identified a higher female mortality rate (OR 2.35)26. There are uncertainties regarding the exact reason behind this trend. It has been thought that it can be due to the higher rate of self-immolation in female patients, which generally is associate with less favorable outcomes27,28. However, we speculate that the reason behind our discrepancy with the existing literature may be the difference in the overall incidence of burn injuries between the two genders. In our cohort, burn incidence was significantly higher amongst men (65.7% in men vs. 34.3% in women), which may have led to this finding. Also, men may be susceptible to traumatic events due to their higher levels of occupational exposure to injuries and comorbid diseases, which can increase their vulnerability to poor outcomes29,30. The same trend seems to hold true for burn injuries as well.
In line with previous reports, age was another major predictor of mortality in our study. During the two time intervals in our study, older age remained a significant non-modifiable risk factor for poor outcomes and mortality. Elderly population, most commonly referenced as ages ≥ 65 years old, are at greatest risk of death as a result of burn injuries. This elevated risk can primarily be attributed to pre-existing health conditions, age-related immunodeficiencies and skin thinning, all of which contribute to a greater extent of TBSA affected by burns after injury31,32.
The cause of the burn was identified as another risk factor for burn patients. Our findings suggest that injuries caused by fire and flames are more strongly associated with unfavorable outcomes in burn victims. Belba et al.33 reported similar findings to our study, showing that burn patients with fire as the cause of injury were 2.6 times more likely to experience mortality. When controlling for patient’s outcomes, there was no significant association between intentional injuries and mortality. Self-immolation is a devastating action and method of suicide with high fatality rates, and has been reported in our country34,35. Although univariant analysis reported suicide as a risk factor for unfavorable outcomes in our study cohort, the multivariable model showed no correlation between the two. Nevertheless, our study showed that accidental burns are more strongly correlated with poor outcomes, which may be attributed to the severity of burn injuries in accidental settings.
There were several limitations to this study, the primary one being that our center served as a referral center for burn injuries. Consequently, patients with minor burns may have received outpatient treatment elsewhere and were therefore not included in the study, potentially leading to underestimation of burn incidence and selection bias. However, these patients are at lower risk for mortality, and we believe that this selection does not affect the overall findings of our study regarding the LA50 values. Additionally, the study's retrospective design is another limitation. Nevertheless, this study provides one of the most comprehensive datasets on patients with burn injuries and is one of the few studies that utilized LA50 to evaluate patient outcomes.
Conclusion
Our study suggested that higher TBSA, male gender, older age, shorter hospitalization duration, etiology of fire and flame, and accidental burn injuries are major risk factors for poor outcomes in burn victims. Also, when comparing the trend and changes in factors among burn patients after our applied policies on 2018, more female patients, higher age, lower TBSA, less burn injuries due to scald, contact, but more frequent fire and flame injuries, and also lower mortality rate was documented. In addition, the mean LA50 values showed significant improvements following significant modifications in our critical care for burn victims, including augmented intensive care unit capacity, prompt relocation of inhalation burn cases to the intensive care unit, establishing a well-trained multidisciplinary team, and improved infection control. To improve outcomes for burn patients in developing countries, major changes should be made in the management of burn patients and LA50 is a reliable assessment tool for evaluating the how these changes affect patient’s outcomes.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request and with permission of the Research Ethics Committee of the School of Medicine-Shiraz University of Medical Sciences.
References
Sarbazi, E. et al. Epidemiology and the survival rate of burn-related injuries in Iran: a registry-based study. Ann. Burns Fire Disasters 32(1), 3 (2019).
Sadeghian, F. et al. The trend of burn mortality in Iran—a study of fire, heat and hot substance-related fatal injuries from 1990 to 2015. Burns 45(1), 228–240 (2019).
Danesh, H. A. et al. Epidemiology and mortality of burn injuries in Eastern Iran since 2009: an analysis of 2115 cases. Int. J. High Risk Behav. Addict. 8, 1 (2019).
Forbinake, N. A. et al. Mortality analysis of burns in a developing country: a CAMEROONIAN experience. BMC Public Health 20(1), 1–6 (2020).
Hoghoughi, M. A. et al. Burn injuries in people who used drug, 2009 to 2017: a case-control study in Shiraz, Southern Iran. J. Burn. Care Res. 43(5), 1170–1174 (2022).
Mohammadi, A. A. et al. Socioeconomic features of burn injuries in southern Iran: A cross-sectional study. J Burn Care Res 43(4), 936–941 (2022).
Hop, M. J., Polinder, S., van der Vlies, C. H., Middelkoop, E. & van Baar, M. E. Costs of burn care: a systematic review. Wound Repair Regener. 22(4), 436–450 (2014).
Mohammadi, A. A. et al. Evaluation of epilepsy and burn patterns in a tertiary hospital in southwestern Iran. Epilepsy Behav. 111, 107213 (2020).
Palmieri, T. L., Przkora, R., Meyer, W. J. 3rd. & Carrougher, G. J. Measuring burn injury outcomes. Surg. Clin. North. Am. 94(4), 909–916 (2014).
Gupta, J. L., Makhija, L. K. & Bajaj, S. P. National programme for prevention of burn injuries. Indian J. Plast. Surg. 43(Suppl), S6–S10 (2010).
Prelack, K., Dylewski, M. & Sheridan, R. L. Practical guidelines for nutritional management of burn injury and recovery. Burns 33(1), 14–24 (2007).
Hashemi, S. S., Mahmoodi, M., Tohidinik, H. R., Mohammadi, A. A. & Mehrabani, D. The epidemiology of burn and lethal area of fifty percentage (LA50) in children in Shiraz, Southern Iran. World J. Plast. Surg. 10(1), 66–70 (2021).
Mobayen, M., Farzan, R., Dadashi, A., Rimaz, S. & Aghebati, R. Effect of early grafting on improvement of lethal area index (la50) in burn patients: A 7-year investigation in a burn referral centre in the North of Iran. Ann. Burns. Fire Disast. 30(3), 189–192 (2017).
Saffle, J. R. Predicting outcomes of burns. Mass Med. Soc. 338, 387–388 (1998).
Kasten, K. R., Makley, A. T. & Kagan, R. J. Update on the critical care management of severe burns. J. Intensive Care Med. 26(4), 223–236 (2011).
Herndon, D. N. Total burn care (Elsevier Health Sciences, 2007).
Roberts, G. et al. The Baux score is dead. Long live the Baux score: A 27-year retrospective cohort study of mortality at a regional burns service. J. Trauma Acute Care Surg. 72(1), 251–256 (2012).
Tung, K. Y. et al. A seven-year epidemiology study of 12,381 admitted burn patients in Taiwan–using the Internet registration system of the Childhood Burn Foundation. Burns 31 Suppl 1(1), S12-17 (2005).
Jeevan, R., Rashid, A., Lymperopoulos, N. S., Wilkinson, D. & James, M. I. Mortality and treatment cost estimates for 1075 consecutive patients treated by a regional adult burn service over a five year period: the Liverpool experience. Burns 40(2), 214–222 (2014).
Khashaba, H., Al-Fadhli, A. N., Al-Tarrah, K., Wilson, Y. & Moiemen, N. Epidemiology and outcome of burns at the Saud Al Babtain Burns, Plastic Surgery and Reconstructive Center, Kuwait: our experience over five years (from 2006 to 2010). Ann. Burns Fire Disast. 25(4), 178 (2012).
Tyson, A. F. et al. Survival after burn in a sub-Saharan burn unit: challenges and opportunities. Burns 39(8), 1619–1625 (2013).
Karimi, K. et al. Increased mortality in women: Sex differences in burn outcomes. Burns Trauma 5, 18 (2017).
Kobayashi, K. et al. Epidemiological and outcome characteristics of major burns in Tokyo. Burns 31 Suppl 1(1), S3–S11 (2005).
Lam, N. N., Hung, N. T. & Duc, N. M. Influence of gender difference on outcomes of adult burn patients in a developing country. Ann. Burns Fire Disast. 32(3), 175–178 (2019).
Christofides, C., Moore, R. & Nel, M. Baux score as a predictor of mortality at the CHBAH adult burns unit. J. Surg. Res. 251, 53–62 (2020).
Moore, E. C., Pilcher, D., Bailey, M. & Cleland, H. Women are more than twice as likely to die from burns as men in Australia and New Zealand: An unexpected finding of the Burns Evaluation And Mortality (BEAM) study. J. Critic. Care 29(4), 594–598 (2014).
Theodorou, P. et al. Suicide by burning: Epidemiological and clinical profiles. Ann. Plast. Surg. 66(4), 339–343 (2011).
Thombs, B. D. & Bresnick, M. G. Mortality risk and length of stay associated with self-inflicted burn injury: Evidence from a national sample of 30,382 adult patients. Critic. Care Med. 36(1), 118–125 (2008).
George, R. L., McGwin, G. Jr., Metzger, J., Chaudry, I. H. & Rue, L. W. III. The association between gender and mortality among trauma patients as modified by age. J. Trauma Acute Care Surg. 54(3), 464–471 (2003).
George, R. L. et al. Age-related gender differential in outcome after blunt or penetrating trauma. Shock 19(1), 28–32 (2003).
Lionelli, G., Pickus, E., Beckum, O., Decoursey, R. & Korentager, R. A three decade analysis of factors affecting burn mortality in the elderly. Burns 31(8), 958–963 (2005).
Jeschke, M. G., Pinto, R., Costford, S. R. & Amini-Nik, S. Threshold age and burn size associated with poor outcomes in the elderly after burn injury. Burns 42(2), 276–281 (2016).
Belba, M. K., Deda, L. N. & Belba, G. P. Measurements of injury-related outcomes: Statistical and analytical data from Albania. Ann. Burns Fire Disast. 34(4), 301–311 (2021).
Mohammadi, A. A. et al. Suicide by self-immolation in southern Iran: An epidemiological study. BMC Public Health 20(1), 1646 (2020).
Shahriarirad, R. et al. Prevalence of suicide by self-immolation among children in southern Iran. J. Burn Care Res. https://doi.org/10.1093/jbcr/irad023 (2023).
Author information
Authors and Affiliations
Contributions
R.S. and A.K. designed the study. M.Z. and M.A collected the data. R.S. and S.N. analyzed the data. Ra.S. and S.N. drafted the manuscript. R.S., A.K., and S.M.K.T revised the manuscript. All authors proofread the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shahriarirad, R., Shekouhi, R., Nabavizadeh, S.S. et al. Cohort analysis of 50% lethal area (LA50) and associating factors in burn patients based on quality improvements and health policies. Sci Rep 13, 19034 (2023). https://doi.org/10.1038/s41598-023-45884-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45884-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.