Abstract
This study aimed to evaluate the effect of two restrictive cumulative fluid balance (CFB) trends on survival and on major clinical outcomes in invasively ventilated patients with moderate to severe respiratory distress syndrome (ARDS) due to SARS-CoV-2. Prospective data collection was conducted on patients in the intensive care unit (ICU) originating from a tertiary university hospital. The primary outcomes were the risk association between the CFB trend during D0 to D7 and 28-day survival. The secondary outcomes were ICU mortality, in-hospital mortality, the need for invasive ventilation at D28, administration of vasoactive drugs at D7, time on invasive ventilation after D7, and length of ICU and hospital stay. 171 patients were enrolled in the study and divided according to their CFB trends during seven days of follow-up using model-based clustering [median CFB negative trend (n = 89) – 279 ml (− 664 to 203) and (n = 82) median CFB positive trend 1362 ml (619–2026)]. The group with CFB negative trend showed a higher chance of surviving 28-day in the ICU (HR: 0.62, 95% CI 0.41–0.94, p = 0.038). Moreover, this group had a reduced length of stay in the ICU, 11 (8–19) days versus 16.5 (9–29) days p = 0.004 and presented lower rates (OR = 0.22; 95% CI 0.09–0.52) of invasive ventilation after 28-days in the ICU. In patients invasively ventilated with moderate to severe ARDS due to COVID-19, the collective who showed a negative trend in the CFB after seven days of invasive ventilation had a higher chance of surviving 28 days in the ICU and lower length of stay in the ICU.
Similar content being viewed by others
Introduction
Patients with SARS-CoV-2 infection can express a broad spectrum of clinical manifestations, from asymptomatic to severe coronavirus disease 2019 (severe COVID-19) marked by a prominent acute respiratory distress syndrome (ARDS)1—the most frequent COVID-19-associated organ dysfunction2, pathophysiologically associated to the so-called COVID-19—hyperinflammation3.
Recent research links positive fluid balance in ICU and cumulative fluid balance (CFB) at ICU discharge with higher sepsis mortality4,5. In sepsis and ARDS patients, positive CFB worsens outcomes, including organ dysfunction and mortality, due to fluid-induced tissue edema6,7. Further, the Fluid and Catheter Treatment Trial (FACTT) study supports conservative fluid management, reducing ventilation duration and ICU stay without raising non-pulmonary organ dysfuntions8. Moreover, a negative fluid balance has been shown to predict patients' survival in septic shock9. In critical ill COVID-19 with ARDS, cumulative balance analysis on day 3 showed that negative balance was associated with higher chances of liberation from invasive ventilation10.
However, due to the lack of a clear definition of a restrictive fluid balance strategy, a broad spectrum of sub cohorts is present inside this collective8,9,11.Thus, which sub cohort inside a restrictive fluid strategy has a better outcome-related performance in the ICU, in special, in ARDS patients due to COVID-19 remains not completely elucidated. Therefore, our hypothesis is that patients with a tendency to negative CFB 7 days after the start of invasive ventilation will have a better chance of survival in the ICU. To test this hypothesis, we performed a survival analysis prospectively using a model-based clustering to evaluate the effect of restrictive trends in CFB seven days after initiation of invasive ventilation on 28-day survival in the ICU and other key outcomes.
Materials and methods
Study design
We conducted a prospective observational single-center cohort study in the ICU of a tertiary hospital. This study was performed from May 2020 to December 2020, before the start of vaccination against SARS-CoV-2.
Ethical approval and consent to participate
The hospital's ethical committee approved the study protocol (ethical approval number: 4.022.319 CEP, IAMSPE Ethical Committee, approval date: May 2020). It was conducted according to the STROBE-Guidelines for prospective observational studies12 and respecting the Helsinki Declaration. Informed consent was obtained from the patient’s relatives or legal representatives for all included patients. From survivors, informed consent was obtained after release from the ICU. The clinical chemistry and laboratory diagnostic of the involved hospital provided analysis of blood samples. For all study time points, the worst laboratory and clinical values within the preceding 24-h interval were considered for the final analysis.
Access of organ dysfunction and estimation of ICU mortality
Organ dysfunction was assessed at all study time points using the Sequential Organ Failure Assessment (SOFA) score13. To estimate ICU mortality, we used the simplified Acute Physiology Score (SAPS 3) on admission to the ICU.
Study population and eligibility
We screened and selected patients older than 18 years old with confirmed infection due to SARS-CoV-2 with a positive polymerase chain reaction (PCR) and a confirmed diagnosis of COVID-19 disease and moderate to severe ARDS according to the Berlin definition14, which required endotracheal intubation and mechanical ventilation within 24 h of admission at the intensive care unit (Patents with COVID-19 and moderate-severe ARDS requiring mechanical ventilation). None of the patients included in this study was vaccinated against SARS-CoV-2. All patients received the standard of care according to the Surviving Sepsis Campaign Guidelines on the Management of Critical ill Adults with COVID-1915 and were ventilated according to the guidelines for protective mechanical ventilation in patients with ARDS using low tidal volume (VT: 4–6 ml/kg PBW), targeting driving pressures lower than 15 cmH2O with individualized positive end-expiratory pressure (PEEP)16. There was no institutional protocol for a fluid restrictive strategy, yet in general there was a clinical practice of restricting fluids during the care of these patients. The detailed exclusion criteria are exposed in the Supplemental Digital Content S1.
Data collection and follow-up
All patients were followed until hospital discharge or death. The data collection was performed prospectively from the electronic patient healthy record (REDCap®). The demographic data were obtained after the enrolment in the study. Clinical and laboratory assessments were performed at all 3 study time points (D0, D3, and D7). D0 was considered as baseline data after intubation and the start of invasive ventilation. D3 was defined as three days after initiation of invasive ventilation, and D7 as seven days after invasive ventilation. Acute kidney injury (AKI) was defined according to the KDIGO-Guidelines (not graded) considering the baseline creatinine from D0 as any of the following increases in serum creatinine ≥ 0.3 mg/dl within 48 h or an increase in serum creatinine ≥ 1.5 times baseline or < 0.5 ml/kg/h for 6 h during D0–D7 (not graded)17. The clinical assessment of pulmonary function, patients' hemodynamics, and laboratory parameters are summarized in the Supplemental Digital Content S1.
Model-based clustering groups allocation
To minimize a dichotomization bias including some patient subgroups in the impropriated cohort it was chosen the K-mean using the trend mean as longitudinal vector trajectory to perform the correct allocation of subjects in the cohorts reducing the confounding bias of heterogeneous trends of CFB within a group of patients. To mitigate the risk of improper patient allocation into unsuitable clusters and to gauge the cohesiveness of the group, we leveraged the Silhouette score. This score yielded a value of 0.93, signifying a substantial degree of segregation among the groups, thus indicating a robust clustering arrangement (Supplemental Digital Content Fig. S1). Therefore, we use a model-based clustering group allocation based on their CFB predominant trend from D0 to D7 (> 50% of the 7 days)18 using k-means clustering in 100 sub-samples (n = 2/3 of the corresponding original sample size) within the sample of patients with complete data on the fluid balance for days 1 to 7. We restricted the number of possible clusters (k) to 2–15, and the optimum was obtained using the Calinski-Harabasz index (cluster boot function, R FPC package19,20. The K-mean cluster approach was based on the daily CFB within 7 days after initiation of invasive ventilation using the predominant trend from D0 to D7 as longitudinal vector trajectory for the clustering. Thus, after the model-based clustering, the collective was divided into two groups according to their CFB trend18,19,20 (Supplemental Digital Content Table S3 and Fig. S2).
Outcomes
The primary outcome is the risk association between the CFB trend during D0 to D7 and 28-day survival. As secondary outcomes, we evaluated the association of CFB trend during D0 to D7 and the need for invasive ventilation at day 28, administration of vasoactive drugs at D7, time on invasive ventilation after D7, ventilation and vasopressor free days, length of ICU stay, in-hospital mortality, ICU mortality and hospital stay (ICU-LOS and Hospital-LOS). Explorative we addressed the incidence of AKI at D7.
Statistical analyses
For the statistical analyses of the continuous demographic, clinical, and laboratory data, values were summarized as means (± SD) and median (Q1/3). We reported their absolute and relative absolute and relative frequencies for categorical variables. The distribution of the variables was tested using the Shapiro–Wilk test. To compare the baseline demographic D0 data between the groups we applied Mann–Whitney U tests for the continuous variables and χ2-tests for categorical variables. For the direct comparison between D0 and D7 from each group separately, we used Wilcoxon signed rank tests for the comparison between continuous variables and χ2-tests for the comparison between categorical variables. For the comparison of clinical and laboratory data between groups at D0, D3, and D7, we used generalized estimating equations (GEE) models with marginal Poisson distribution and an identity link function, assuming a first-order autoregressive (AR1)21 correlations between assessment times. The results were followed by Bonferroni multiple comparisons to identify the differences between groups and time points when significant22,23.
In the analyses of our primary outcomes, we conducted a survival analysis using the CFB trend as a dependent variable for outcomes estimating the cumulative-event probabilities. We calculated adjusted Hazard ratio (HR) and 95% confidence in the Kaplan–Meier survival by Cox Model stepwise, and the odds ratio were calculated using a multiple logistic regression stepwise model adjusted for possible confounders (age, gender, BMI, Charlson-comorbidity index, and SAPS 3 baseline [D0]). Variables with multicollinearity were removed from the final analysis. For the risk analysis of our secondary outcomes, we calculated the odds ratio and 95% confidence using a multiple logistic regression adjusted for possible confounders using the CFB trend as a dependent variable, excluding variables with multicollinearity from the final analysis. The logistic regression models were tested using a generalized Hosmer–Lemeshow goodness-of-fit test24.
Statistical analysis was performed with IBM SPSS 26 (IBM Corporation, Armonk, NY, USA) and Graphpad Prism 7.05 (Graphpad Software Inc., San Diego). We applied a significance level of 5% and reported two-sided p-values.
Results
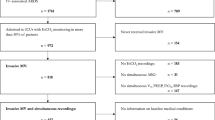
Figure 1 describes the study design. Initially, 258 patients were screened. After removing patients based on exclusion criteria and patients who did not present complete data before D7, 171 patients were included in the final cohort. Using a model-based clustering group allocation based on their CFB trend from D0 to D7, 89 patients were clustered into the CFB negative trend median -279 ml group and 82 patients into the CFB positive trend group median 1362 ml (Supplemental Digital Content Fig. S3).
Baseline characteristics
Table 1 shows the descriptive demographic data. Both studied groups had similar demographic characteristics, including age, sex, BMI, Charlson-comorbidity index, SOFA and SAPS III scores, ventilatory and laboratory parameters, and need for vasopressor drugs. In summary, both patient cohorts were median-aged (66 years), overweight (BMI ≥ 26 kg/m2), mostly male, and had comparable preexisting comorbidities. Clinically, they exhibited a similar degree of organ dysfunction (SOFA score of 6) and a similar level of pulmonary dysfunction, with a median oxygenation index of 110 in the CFB negative trend group and 100 in the CFB positive trend group, both meeting the criteria for moderate ARDS according to the Berlin criteria14.
Clinical and laboratory parameters
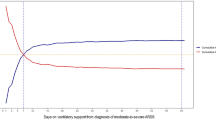
Table 2 demonstrates the clinical and laboratory parameters of the studied groups at study times D0 and D7. In the CFB negative trend group, comparing their baseline to D7, the analyzed values presented not a statistically significant difference regarding the SOFA score but significantly increased creatinine and lactate plasma levels and a significant decrease in MAP and serum hemoglobin. Similarly, in the CFB positive trend group, the comparison of the D0 and D7 values also presented no statistically significant difference in the SOFA Score. However, in this group, there was a significant increase in serum creatinine and a decrease in serum hemoglobin. Comparing the D7 data of each group, there was no statistically significant difference in the SOFA Score, creatinine, and lactate levels. Still, the CFB negative trend group presented significantly lower MAP and higher hemoglobin values than the CFB positive trend group. An exploratory comparison was made at D3 between laboratory, clinical and CFB trend of both cohorts (Supplementary Table S5, Fig. 2, D3 time point). In summary, at D3 the CFB negative trend presented higher levels of MAP than the positive trend, However, interestingly, the group with a positive tendency had higher creatinine levels.
Figure 2 shows the ventilatory and laboratory parameters at different study time points. Both groups showed a dynamic improvement in respiratory parameters such as reduced FiO2, increased oxygenation index, and arterial oxygen saturation. However, the group CFB with a negative trend presented lower PEEP levels on D7 (Fig. 2B). The two groups showed similar oxygenation index and FiO2 values with no statistical difference in all study time points (Fig. 2A,D).
Primary and secondary endpoints
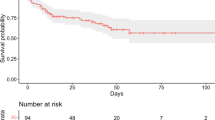
Eighty-nine patients in the CFB negative trend group and 82 in the CFB positive trend group were in the follow-up. 28-day mortality was 46% vs. 64% and the ICU mortality 30% vs. 46% respectively (Fischer’s exact test p = 0.021 and p = 0.003). However, the in-hospital mortality had no significant difference 40.4% vs. 55% (Fischer’s exact test p = 0.059). Figure 3 shows the Kaplan–Meier survival curve for the 28-day follow-up in the ICU. The unadjusted survival hazard in the CFB negative trend group was HR: 0.62, 95% CI 0.41–0.94, p = 0.032. After adjustments to minimize the effect of confounding variables, the CFB negative trend group maintained a higher chance of survival 28-day in the ICU (adjusted Odds Ratio: 0.70, 95% CI 0.24–0.98, p = 0.038). Table 3 summarize the secondary outcomes. The CFB negative trend group showed decreased risk of requiring invasive ventilation at D28, and higher odds to need vasopressors drugs at D7 and being more days on use of vasopressor in comparison with the CFB positive trend group. This group showed also decreased ICU LOS but no significant difference in the Hospital LOS. The incidence of AKI at D7 didn’t differ between the groups (50.56% CFB negative trend and 40.2% CFB positive trend Fischer’s exact test p = 0.219).
Discussion
In this prospective single-center observational study in patients with moderate to severe ARDS due to SARS-CoV-2, one could observe a higher hazard of 28-day survival in patients with CFB with a negative trend seven days after invasive ventilation. It is noteworthy that our patient cohort demonstrated similar demographic characteristics to those previously described for individuals afflicted with severe COVID-19. In our study, both collectives were predominantly male, over 60 years old, and overweight. Older age, male gender, and being overweight are risk factors for developing severe and critical COVID-19 disease and sepsis from other etiology25,26,27,28,29.
In critically ill patients and in patients undergoing major surgeries fluid overload is associated with worse outcomes increasing their morbidity and mortality11,30. Data obtained from observational studies that included septic patients and patients with critical neurological diseases indicate a deterioration in clinical outcomes in presence of fluid overload6,31. This deterioration is manifested by prolonged stays in the ICU, increased in-hospital mortality rates, and a progression of organ dysfunctions, including the worsening of lung function6,30,32. In a different clinical context, involving patients with moderate to severe ARDS due to the SARS-CoV-2 virus, we were able to show a worsening in the clinical outcome of patients who tended to have a positive fluid screen within 7 days. In the other hand, patients with a negative CFB trend had better outcomes. This was translated to an increased likelihood of survival and a reduced duration of stay in the ICU. Interestingly, this group had less time on mechanical ventilation after day 7 and need of invasive Ventilation after 28 days, although there was no difference in the days free of mechanical ventilation and in the in-hospital mortality.
Currently, there is no established consensus for guiding fluid management in patients with ARDS33,34,35. There is a logical propensity to prioritize fluid restriction since the pathophysiological mechanism to explain the improvement of hematosis by restricting the fluid input is the reduction of tissue, cellular, interstitial, and alveolar edema caused by the lesion of the alveolar-capillary bed by the inflammatory process36,37. However, the absence of a clearly defined restrictive fluid management strategy in sepsis4,5,9,38 in patients with ARDS33,35,39, and now in patients with ARDS caused by SARS-CoV-240, makes it challenging to compare various studies and their findings. This challenge arises from the lack of consensus regarding the specific limits for defining a fluid balance as restrictive and the absence of a universally accepted clinical protocol34,41.
Nonetheless, moderate to severe ARDS induced by SARS-CoV-2 closely resembles non-COVID-19 ARDS physiologically, making findings from COVID-19 ARDS studies relevant to ARDS from various causes42.Improved lung function and ventilation parameters have been demonstrated in studies evaluating restrictive fluid replacement therapy in ARDS due to sepsis43,44. We could observe these findings in invasively ventilated patients with moderate to severe ARDS due to COVID-19-sepsis. Both the CFB negative and positive trends showed improvement in oxygenation and ventilation parameters when comparing the evolution of their baseline, D3, and D7 values.
For instance, two large trials shared similar findings. Firstly, the FACTT trial showed the benefit of the conservative fluid strategy over a liberal approach. That trial showed significant oxygenation and ventilatory improvements without an increase in other organ dysfunction but no significant reduction in 60-day mortality was found. Some points may explain the mortality difference found between the two restrictive trends of CFB in our study: (1) We studied a group of patients with ARDS due to COVID-19-sepsis, unlike the FACTT trial, where only 14.3% of the patients had pneumonia or sepsis; (2) the two groups evaluated by our study are restrictive, making our data only comparable to the restrictive arm of the FACTT trial; (3) the baseline characteristics such as the predominance of elderly and obese patients of patients with ARDS due to COVID-19 differed from that found for ARDS of other origins, as the studied collective in the FACTT trial showed (4), FACTT trial had a interventional nature with an established protocol for fluid restriction differs from our present observational study. and finally (5) We evaluate mortality within a brief timeframe of 28 days.
An insight from the PRoVent-COVID-19 study evaluated the association between early CFB and successful liberation from invasive ventilation in COVID-19 ARDS patients. In terms of the studied collective, the baseline characteristics of our collective of patients with ARDS due to COVID-19-sepsis resemble demographically, clinically and laboratory the collective presented by the sub-analysis from the PRoVent-COVID-19 study. This study analyzed three groups of patients: higher, intermediate, and lower groups, having a median CFB of 1.98 L (1.27–7.72 L), 0.78 L (0.26–1.27 L), and − 0.35 L (− 6.52 to 0.26 L), respectively. In summary, this study found a risk of a lower likelihood of successful release from invasive ventilation on day 28 in the group with higher CFB on day 3. In addition, this group showed longer invasive ventilation time and hospital length of stay. Still, no difference was found regarding the incidence of AKI, 28-day mortality, and length of stay in the ICU40.
In the present study, comparing the two CFB trends, we were able to show a higher hazard of 28-day survival and lower length of stay in the ICU. Although our study observed less need for invasive ventilation in the restrictive CFB, an essential difference in study design may explain the difference in survival and organ dysfunction in our study like the assessment of the risk association between the CFB trend and 28-day mortality over a more extended observation period (seven days). A fact that can more comprehensively characterize the clinical progression of patients of this category pertains to the noteworthy average duration of mechanical ventilation, which spans 13.5 days10,45. Employing an observation window of 7 days could offer a more accurate portrayal of the patient's trajectory and enable the discernment of the impacts of fluid-restrictive strategies. It is worth noting that a substantial proportion of extant research studies typically evaluate the effects of these strategies over a mere 3-day interval10. This relatively short observational period may not adequately elucidate the potential advantages associated with a restrictive strategy, since both groups are still in the post-acute phase due to possible fluid overload, characteristic of the acute phase of critically ill patients30,32,46. Our own analysis corroborates this contention, as we observed that, within the initial 3 days of monitoring, there were no discernible or statistically significant disparities in the clinical parameters pertinent to respiratory outcomes between the two cohort.
Considering our observations regarding 28-day survival and mortality, given the absence of a distinction in in-hospital mortality within our study, it becomes imperative that future randomized investigations and meta-analyses are conducted to assess the potential advantages of fluid-restrictive interventions and evaluation of CFB trends in patients with ARDS, particularly in cases of viral sepsis, such as those resulting from SARS-CoV-2 infection.
Restrictive fluid strategies have being associated in critical ill patients with higher need of vasopressors and development of AKI47. Indeed, our study found higher need of vasopressor in patients with CFB with negative trend. Restrictive fluid management in critically ill patients with ARDS has been associated with a decline in intravascular pressures and increased use of vasopressors to maintain adequate hemodynamics40. On the other hand, the group with a negative trend showed higher lactate levels, which may indicate a worsening in tissue perfusion. A fact that may be associated with greater organ dysfunction48. Nonetheless, regarding the incidence of AKI, no statistical difference was found using the ungraded KDIGO criteria for AKI17 (50.5% in the CFB negative trend group and 40.2% in the CFB positive group), equally finding to PRoVent-COVID-19 study40. Our findings align with a large observational study showing similar incidence of AKI in hospitalized patients with COVID-19.
Limitations
Our findings should be taken into consideration in regard of the study limitations. First, we conducted a single-center study, making the projection of our data to other centers difficult. In addition, it was an observational, not randomized, study without interventions. Moreover, the lack of an institutional protocol for fluid restriction restricts the application of results in other centers. Further, the effect of different diuretic drugs including the different off-label therapies for COVID-19 on outcomes was not assessed. An important fact to mention is that we did not grade acute renal dysfunction, making the evaluation of the effect or risk associations of this variable difficult. Moreover, we did not evaluate the parameters of fluid responsiveness and intracardiac pressures by echocardiography. Finally, the causal etiology of need for vasopressor was not addressed as well as the fact that the inclusion of some patients with a slight reduction in LVEF (between 40 and 50%) could be a potential confounding factor. However, taking in consideration our findings, this study can serve as a basis for multicenter clinical randomized studies based on the CFB trend in the assessment of the effect of restrictive fluid balance in patients with moderate to severe ARDS.
Conclusion
In patients invasively ventilated with moderate-severe ARDS due to COVID-19, the collective who showed a negative trend inside the CFB after seven days of invasive ventilation had a higher chance of surviving 28 days and lower length of stay in the ICU. Further, studies are needed to confirm these benefits, especially in patients with ARDS of viral origin.
Data availability
All patient-related work data or statistical analysis is available for the next 10 years for free consultation. The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733. https://doi.org/10.1056/NEJMoa2001017 (2020).
Puelles, V. G. et al. Multiorgan and renal tropism of SARS-CoV-2. N. Engl. J. Med. 383, 590–592. https://doi.org/10.1056/NEJMc2011400 (2020).
Chen, L. Y. C., Hoiland, R. L., Stukas, S., Wellington, C. L. & Sekhon, M. S. Confronting the controversy: Interleukin-6 and the COVID-19 cytokine storm syndrome. Eur. Respir. J. 56, 2003006. https://doi.org/10.1183/13993003.03006-2020 (2020).
Acheampong, A. & Vincent, J. L. A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit. Care (London, England) 19, 251. https://doi.org/10.1186/s13054-015-0970-1 (2015).
Yoo, M. S. et al. Association of positive fluid balance at discharge after sepsis management with 30-day readmission. JAMA Netw. Open 4, e216105–e216105. https://doi.org/10.1001/jamanetworkopen.2021.6105 (2021).
Huang, A.C.-C. et al. Fluid balance correlates with clinical course of multiple organ dysfunction syndrome and mortality in patients with septic shock. PloS One 14, e0225423–e0225423. https://doi.org/10.1371/journal.pone.0225423 (2019).
Jaffee, W., Hodgins, S. & McGee, W. T. Tissue edema, fluid balance, and patient outcomes in severe sepsis: An organ systems review. J. Intensive Care Med. 33, 502–509. https://doi.org/10.1177/0885066617742832 (2018).
Comparison of two fluid-management strategies in acute lung injury. N. Engl. J. Med. 354, 2564–2575. https://doi.org/10.1056/NEJMoa062200 (2006).
Alsous, F., Khamiees, M., DeGirolamo, A., Amoateng-Adjepong, Y. & Manthous, C. A. Negative fluid balance predicts survival in patients with septic shock: A retrospective pilot study. Chest 117, 1749–1754. https://doi.org/10.1378/chest.117.6.1749 (2000).
Ahuja, S. et al. Association between early cumulative fluid balance and successful liberation from invasive ventilation in COVID-19 ARDS patients—insights from the PRoVENT-COVID study: a national, multicenter, observational cohort analysis. Crit. Care (London, England) 26, 157. https://doi.org/10.1186/s13054-022-04023-y (2022).
Palomba, H. et al. Intraoperative fluid balance and cardiac surgery-associated acute kidney injury: A multicenter prospective study. Braz. J. Anesthesiol. 72, 688–694. https://doi.org/10.1016/j.bjane.2022.07.006 (2022).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Internal Med. 147, 573–577. https://doi.org/10.7326/0003-4819-147-8-200710160-00010 (2007).
Vincent, J. L. et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 22, 707–710. https://doi.org/10.1007/bf01709751 (1996).
Bellani, G. et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 315, 788–800. https://doi.org/10.1001/jama.2016.0291 (2016).
Alhazzani, W. et al. Surviving sepsis campaign guidelines on the management of adults with coronavirus disease 2019 (COVID-19) in the ICU: First update. Crit. Care Med. 49 (2021).
Pelosi, P. et al. Personalized mechanical ventilation in acute respiratory distress syndrome. Crit. Care (London, England) 25, 250. https://doi.org/10.1186/s13054-021-03686-3 (2021).
Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron. Clin. Pract. 120, c179-184. https://doi.org/10.1159/000339789 (2012).
Fraley, C. & Raftery, A. E. Model-based clustering, discriminant analysis, and density estimation. J. Am. Stat. Assoc. 97, 611–631. https://doi.org/10.1198/016214502760047131 (2002).
Hennig, C. Cluster-wise assessment of cluster stability. Comput. Stat. Data Anal. 52, 258–271 (2007).
Hennig, C. Dissolution point and isolation robustness: Robustness criteria for general cluster analysis methods. J. Multivar. Anal. 99, 1154–1176. https://doi.org/10.1016/j.jmva.2007.07.002 (2008).
Glonek, G. F. & McCullagh, P. Multivariate logistic models. J. R. Stat. Soc. Ser. B (Methodological) 57, 533–546 (1995).
Neter, J., Kutner, M. H., Nachtsheim, C. J. & Wasserman, W. Applied linear statistical models. (1996).
Zheng, B. Summarizing the goodness of fit of generalized linear models for longitudinal data. Stat. Med. 19, 1265–1275. https://doi.org/10.1002/(SICI)1097-0258(20000530)19:10%3c1265::AID-SIM486%3e3.0.CO;2-U (2000).
Fagerland, M. W. & Hosmer, D. W. A generalized hosmer-lemeshow goodness-of-fit test for multinomial logistic regression models. Stata J. 12, 447–453. https://doi.org/10.1177/1536867x1201200307 (2012).
Junior, J. M. S. et al. Response of patients with acute respiratory failure caused by COVID-19 to awake-prone position outside the intensive care unit based on pulmonary involvement. Clinics 76. https://doi.org/10.6061/clinics/2021/e3368 (2021).
Wang, W. et al. Definition and risks of cytokine release syndrome in 11 critically Ill COVID-19 patients with pneumonia: Analysis of disease characteristics. J. Infect. Dis. 222, 1444–1451. https://doi.org/10.1093/infdis/jiaa387 (2020).
Wang, Y. et al. Risk factors for postoperative sepsis-induced cardiomyopathy in patients undergoing general thoracic surgery: A single center experience. J. Thorac. Dis. 13, 2486–2494. https://doi.org/10.21037/jtd-21-492 (2021).
Wang, H. E., Griffin, R., Judd, S., Shapiro, N. I. & Safford, M. M. Obesity and risk of sepsis: A population-based cohort study. Obesity (Silver Spring) 21, E762-769. https://doi.org/10.1002/oby.20468 (2013).
Martin, G. S., Mannino, D. M. & Moss, M. The effect of age on the development and outcome of adult sepsis. Crit. Care Med. 34, 15–21. https://doi.org/10.1097/01.ccm.0000194535.82812.ba (2006).
Messmer, A. S. et al. Fluid overload and mortality in adult critical care patients—a systematic review and meta-analysis of observational studies*. Crit. Care Med. 48, 1862–1870. https://doi.org/10.1097/ccm.0000000000004617 (2020).
Wiegers, E. J. A. et al. Fluid balance and outcome in critically ill patients with traumatic brain injury (CENTER-TBI and OzENTER-TBI): A prospective, multicentre, comparative effectiveness study. Lancet Neurol. 20, 627–638. https://doi.org/10.1016/S1474-4422(21)00162-9 (2021).
Seitz, K. P., Caldwell, E. S. & Hough, C. L. Fluid management in ARDS: An evaluation of current practice and the association between early diuretic use and hospital mortality. J. Intensive Care 8, 78. https://doi.org/10.1186/s40560-020-00496-7 (2020).
Simmons, R. S. et al. Fluid balance and the adult respiratory distress syndrome. Am. Rev. Respir. Dis. 135, 924–929. https://doi.org/10.1164/arrd.1987.135.4.924 (1987).
Humphrey, H., Hall, J., Sznajder, I., Silverstein, M. & Wood, L. Improved survival in ARDS patients associated with a reduction in pulmonary capillary wedge pressure. Chest 97, 1176–1180. https://doi.org/10.1378/chest.97.5.1176 (1990).
Martin, G. S. et al. Albumin and furosemide therapy in hypoproteinemic patients with acute lung injury. Crit. Care Med. 30, 2175–2182. https://doi.org/10.1097/00003246-200210000-00001 (2002).
Roch, A. & Allardet-Servent, J. Physiopathologie de l’œdème pulmonaire. Réanimation 16, 102–110 (2007).
Roch, A., Guervilly, C. & Papazian, L. Fluid management in acute lung injury and ards. Ann. Intensive Care 1, 16. https://doi.org/10.1186/2110-5820-1-16 (2011).
Meyhoff, T. S. et al. Restriction of intravenous fluid in ICU patients with septic shock. N. Engl. J. Med. 386, 2459–2470. https://doi.org/10.1056/NEJMoa2202707 (2022).
van Mourik, N. et al. Cumulative fluid balance predicts mortality and increases time on mechanical ventilation in ARDS patients: An observational cohort study. PloS one 14, e0224563 (2019).
Ahuja, S. et al. Association between early cumulative fluid balance and successful liberation from invasive ventilation in COVID-19 ARDS patients—insights from the PRoVENT-COVID study: A national, multicenter, observational cohort analysis. Crit. Care 26, 157. https://doi.org/10.1186/s13054-022-04023-y (2022).
Mitchell, J. P., Schuller, D., Calandrino, F. S. & Schuster, D. P. Improved outcome based on fluid management in critically ill patients requiring pulmonary artery catheterization. Am. Rev. Respir. Dis. 145, 990–998. https://doi.org/10.1164/ajrccm/145.5.990 (1992).
Brault, C. et al. COVID-19- versus non-COVID-19-related acute respiratory distress syndrome: differences and similarities. Am. J. Respir. Crit. Care Med. 202, 1301–1304. https://doi.org/10.1164/rccm.202005-2025LE (2020).
Silversides, J. A. et al. Conservative fluid management or deresuscitation for patients with sepsis or acute respiratory distress syndrome following the resuscitation phase of critical illness: A systematic review and meta-analysis. Intensive Care Med. 43, 155–170. https://doi.org/10.1007/s00134-016-4573-3 (2017).
Mekontso Dessap, A. et al. Natriuretic peptide-driven fluid management during ventilator weaning: A randomized controlled trial. Am. J. Respir. Crit. Care Med. 186, 1256–1263. https://doi.org/10.1164/rccm.201205-0939OC (2012).
Botta, M. et al. Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): A national, multicentre, observational cohort study. Lancet Respir. Med. 9, 139–148. https://doi.org/10.1016/S2213-2600(20)30459-8 (2021).
Stein, A. et al. Fluid overload and changes in serum creatinine after cardiac surgery: predictors of mortality and longer intensive care stay. A prospective cohort study. Crit. Care (London, England) 16, R99. https://doi.org/10.1186/cc11368 (2012).
Early restrictive or liberal fluid management for sepsis-induced hypotension. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2212663 (2023).
Subramanian, S. et al. Liberal vs conservative vasopressor use to maintain mean arterial blood pressure during resuscitation of septic shock: An observational study. Intensive Care Med. 34, 157–162. https://doi.org/10.1007/s00134-007-0862-1 (2008).
Acknowledgements
Ricardo Esper Treml and Tulio Caldonazo are supported by the Clinical Scientist Program (Jena University Hospital). The authors thank all patients and healthcare personnel involved in the study.
Funding
RET and TC were funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) Clinician Scientist Program OrganAge funding number 413668513 and by the Interdisciplinary Center of Clinical Research of the Medical Faculty Jena.
Author information
Authors and Affiliations
Contributions
Conceptualization, R.E.T. and J.S.; methodology, R.E.T. and T.C.; validation, J.S., P.D. and P.R.; formal analysis, R.E.T. and T.C.; investigation, P.H.F., A.L.M. and A.C.; data curation, P.H.F., A.L.M. and A.C.; writing—original draft preparation, R.E.T. and T.C.; writing—review and editing, P.R. and J.S.; supervision, P.R. and J.S.; project administration, R.E.T. All authors have read and agreed to the published version of the manuscript. The manuscript has been read and approved for submission by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Esper Treml, R., Caldonazo, T., Filho, P.H.A. et al. Effect of restrictive cumulative fluid balance on 28-day survival in invasively ventilated patients with moderate to severe ARDS due to COVID-19. Sci Rep 13, 18504 (2023). https://doi.org/10.1038/s41598-023-45483-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45483-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.