Abstract
The loss of hypocretin is thought to be the main pathophysiological mechanism of narcolepsy. There is strong evidence that hypocretin is related to the regulation of endocrine functions and depression. To explore thyroid hormone levels in narcolepsy patients was our aim. In addition, further is to analyze the relationship between thyroid hormone levels and sleep quality, anxiety, and depression in narcolepsy patients. There are 40 patients with narcolepsy and 40 healthy controls (HCs) were conducted. Blood samples were explored for thyroid function. Correlation analysis between thyroid hormones and clinical characteristics of narcolepsy was performed using Pearson or Spearman. Narcolepsy patients had significantly lower free thyroxine (FT4) levels in comparison to controls (p < 0.001). No subject was diagnosed with primary hypothyroidism. There were 4 (10%) subjects with subclinical hypothyroidism. The serum FT4 levels were positively correlated with HAMA14 score (r = − 0.343, p = 0.030) by Pearson correlation analysis. The serum TSH levels and HAMD24 score (r = − 0.807 p ˂0.001), and ESS score (r = − 0.317, p = 0.046) both showed a negative correction. Hypocretin deficiency may be associated with the regulation of thyroid hormones in narcolepsy patients. The serum thyroid hormones may affect the severity and neuropsychological functions of narcolepsy patients.
Similar content being viewed by others
Introduction
Nacolepsy type 1 (NT1) is associated with cataplexy attacks, orexin deficiency, and excessive daytime sleepiness (EDS)1,2. It is estimated that approximately affects 1/2000 individuals3. The destruction of hypocretin neurons were thought to be the autoimmune-mediated, which was the main pathophysiological mechanism of NT14,5,6.Besides, more than 98% of NT1 with cataplexy patients are positive for HLA-DQB1*06026,7,8. Additionally, more evidence has demonstrated that environmental factors and genetic also involved in the pathogenic mechanism of NT19.
Recently, the association between NT1 and thyroid disease is attractive, which supports the hypothesis of a causal autoimmune disorder or co-existing ones10. A previous study has found that NT1 patients may have concomitant thyrotropin deficiency11. However, the results were conducted from only seven NT1 patients, which is limited to relatively small numbers of subjects to draw firm conclusions. Interestingly, a case report found significant improvement in EDS symptoms with levothyroxine treatment in a euthyroid patient with NT112. There is strong evidence that hypocretin is related to the regulation of endocrine functions and depression13. Besides, a previous study showed that the hypothalamic-pituitary-thyroid (HPT) axis can be modulated by hypocretin14. In addition, electrical stimulation of the lateral hypothalamic area (LHA) has been demonstrated to induce morphological changes in the thyroid gland15. As accumulated pieces of evidence suggested that neurophysiological and behavioral processes of mood disorders can be significantly affected by hypocretin13. Thyroid hormone is involved in regulating psychological function and emotion16. The relationship between the HTA axis and mood disorder has been increasingly studied17. Growing evidence have indicated that NT1 patients have an increased prevalence of psychiatric comorbidities18. Our aim was to assess differences in serum thyroid hormone levels between patients with NT1 and healthy controls (HCs) in this case–control study.
Materials and methods
Research subjects
This case–control study was conducted from 2019 to 2022. There are 40 NT1 patients and 40 healthy individuals during the same period. The International Classification of Sleep Disorders (ICSD-3) diagnostic criteria was used to confirm NT1 diagnosis19. The healthy controls selected from the general population via advertisement and local association networks, no objective sleepiness on the MSLT (mean sleep latency > 8 min), no medication use, and no other significant psychiatric, neurologic, or medical disorders.
The study was approved by the Ethics Committee of The Second Hospital of Shandong University, and all participants signed written informed consent prior to participation. This study was conducted in accordance with the Declaration of Helsinki.
Exclusion criteria
Exclusion criteria were as follows: (1) medical history of central nervous system demyelinating disease, central nervous system infection, and intracranial tumors; (2) patients with a history of metabolic illness(e.g. autoimmune liver disease, viral hepatitis, diabetes, and hypertension) were excluded; (3) patients with a history of 131I treatment for hyperthyroidism, neck radiotherapy, thyroidectomy were excluded; (4) Exclusion of participants with comorbid other forms of sleep disorders (e.g. OSA, RLS); (5) Comorbid psychiatric disorders were excluded20.
Research methods
Collecting general information
To assess the subjects’ EDS symptoms, the Epworth sleepiness scale (ESS) was used by professional physicians21.
Laboratory assessment
After an overnight fast of 8 h, venous blood samples were collected from all subjects and serum free thyroxine (FT4), free triiodothyronine (FT3) and thyroid stimulating hormone (TSH) levels were assessed according to standard operating procedures, the Architect i2000SR automated immunoassay system was used to measure FT4, FT3 and TSH20. We used the 125I radioimmunoassay kit (Phoenix Pharmaceuticals, Belmont, CA, USA) to muesure the cerebrospinal fluid (CSF) hypocretin-1 levels.
Clinical and neuropsychological assessment
To measure the sleep quality, the Pittsburgh sleep quality index (PSQI) was used20,22. To measue the anxiety, the 14-item Hamilton Anxiety Scale (HAMA14) was used20. While, to measure the depression symptoms of narcoelpsy patients, the 24-item Hamilton depression rating scale (HAMD24) were used20,23.
Statistical analysis
All analyses were performed using SPSS 24.0 computer software20. The mean ± standard deviation (SD) was uesed to reprent the continuous variables. The interquartile range (M, P25, P75) was used to present non-normally distributed data, which was tested by the student’s t test. Mann–Whitney U test was used to test the normality of the data. To compare the groups, we used the Chi-square test or Fisher’s exact test. Categorical data were expressed in amount (%)20. Spearman or Pearson for correlation analysis20. A P value of less than 0.05 was considered statistically significant.
Ethics statement
The study was approved by the Ethics Committee of The Second Hospital of Shandong University (No.2021141), and all participants signed written informed consent prior to participation. This study was conducted in accordance with the Declaration of Helsinki..
Results
Demographics and clinical characteristics
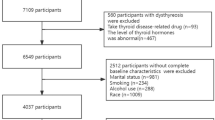
A total of 40 patients with NT1 were included in the study according to the inclusion and exclusion criteria (Fig. 1). Biochemical characteristics and demographic data characteristics of the participants are presented in Table 1.
Comparison of thyroid hormones of NT1 patients and healthy subjects
The levels of FT4 in serum (p < 0.001) were significantly lower in patients with NT1 compared to the HC group. However, no differences were found between TSH (p = 0.906) or FT3 (p = 0.274) levels (Table 2).
The number of subjects in NT1 patients categorized by thyroid hormones
Table 3 shows the number of subjects in the NT1 group classified by FT4, FT3 and TSH levels. 4 (10%) patients had higher than normal TSH levels. 0 (0%) and 4 (10%) subjects had lower than normal FT3 and FT4 levels. No patient was diagnosed with primary hypothyroidism, compared to 4 (10%) subjects who were diagnosed with subclinical hypothyroidism. No hyperthyroidism was found in our study.
Correlation analysis of thyroid hormones and clinical characteristics of NT1
A statistically significant negative correlation was found between serum TSH levels and HAMD24 score (r = − 0.807, P-value ˂0.001), and ESS score (r = − 0.317, P-value = 0.046). The serum FT4 levels was positively correlated with HAMA14 score(r = − 0.343, P-value = 0.030) by Pearson correlation analysis (Table 4).
Discussion
NT1 and thyroid function
Kok et al.11 reported that the serum levels of TSH were lower in patients with NT1. Szakacs et al.24 considered that the median TSH was decreased in NT1 patients with cataplexy. Our results also suggested that the FT4 was significantly decreased in NT1 patients. However, Chabas et al.25 found no different in serum TSH and FT4 levels. In addition, there was no difference in FT3 and TSH levels between NT1 patients and the control group. Moreover, in an autopsy study, the thyrotropin releasing hormone-expressing neurons were unaffected in paraventricular nucleus (PVN) of patients with NT126. Thyroid hormone changes in patients with NT1 remain unknown due to the small number of studies and conflicting results. CG-3703, a thyroid-releasing hormone (TRH) analog can increase wakefulness, suppressed both REM sleep, slow-wave sleep, and significantly reduce cataplexy in canine NT127,28. However, there were four (10.0%) subjects with subclinical hypothyroidism in our study. Hypocretin can regulate the HPT axis, which could provide insights into the understanding of the broad symptom spectrum of NT1. Martinez-Orozco et al.29 found an increased prevalence of autoimmune thyroid disease in NT1 patients, which may provide a valuable starting point for basic and applied research into the disease. However, autoimmune thyroid disease was not seen in our present study.
Orexin system and HPT axis
Several animal experiments have already demonstrated that the hypocretin system can be able to modulate the HPT axis in rodents. Kaufman et al.30 found that the levels of thyroid hormone were lower in rats with LHA lesions. Besides, Suzuki et al.31 found that the administration of TRH in the LHA can significantly enhance the anorexia effect. In addition, studies have demonstrated that peripheral administration of hypocretin-1 can inhibit the TRH release from the hypothalamus in rats32. Different mechanisms for the causal relationship between thyroid function and NT1 were suggested. The PVN can receive hypocretin input signals33, which is also the central point of the regulation of the HPT axis34. Hypophysiotropic neurons of the PVN of the hypothalamus expressing TRH project to the portal system, via which it reaches the thyrotropin-producing cells of the anterior pituitary35. Thyroid hormone secretion is suppressed during starvation, while preprohypocretin mRNA is upregulated in the LHA36. We hypothesized that hypocretin neural circuits can modulate the HPT axis. Despite the evolving understanding of the hypocretin system, its role on the HPT axis in NT1 seems to remain unclear.
Thyroid dysfunction and depression
The neuroendocrine dysfunction theory of the pathogenesis of depression mainly includes abnormalities of the hypothalamic–pituitary–adrenal axis and the HPA axis10. The relationship between thyroid function and depression has been of great interest to scholars, and it has been suggested that there are alterations in the function of the hypothalamic pituitary thyroid (HPT) axis in patients with depression, and it has been reported that disturbances in the level of thyroid hormones not only affects the patient's emotional response, but also serves as a marker of sensitivity in some patients with depression15. Studies have indicated that FT3 and FT4 may be the hallmark markers for predicting the degree of depression, and thyroid-related tests may be considered as routine examinations for adolescents with depression16. Hypothyroidism can induce depression and inattention, while mood disorders also be able to modulate the function of HPT axis16. Some researchers have proposed that thyroid hormones have an antidepressant effect in depression37. The serum TSH level of patients with NT1 was linked with the more severe subjective sleepiness symptoms, and the worse depression. In addition, we found that the serum FT4 levels was positively correlated with HAMA14 score. Hypocretin deficiency can induce the cholinergic monoaminergic imbalance, which may be involved in the pathophysiological process of depression18. However, although previous studies have found that thyroid hormones are involved in the pathogenesis of depression, the exact mechanism of the HPT axis in depression remains unclear.
Limitations and recommendations
Firstly, subjects should be followed up periodically to assess their clinical characteristics as well as thyroid function, further illustrating the changes in thyroid hormones in patients with NT1. In addition, our results remain weak due to the sample size; our study subjects represent only NT1 patients with cataplexy.
Conclusion
Hypocretin deficiency may be associated with the regulation of thyroid hormones in NT1 patients. The serum thyroid hormones may affect the severity and neuropsychological functions of NT1 patients. The exact relationship between thyroid hormones and NT1 should be validated in multi-center, and large-sample clinical studies in the future.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Bassetti, C. L. A. et al. Narcolepsy—Clinical spectrum, aetiopathophysiology, diagnosis and treatment. Nat. Rev. Neurol. 15(9), 519–539 (2019).
Ebrahim, I. O. et al. Hypocretin (orexin) deficiency in narcolepsy and primary hypersomnia. J. Neurol. Neurosurg. Psychiatry 74(1), 127–130 (2003).
Luo, G., Yogeshwar, S., Lin, L. & Mignot, E. J. T cell reactivity to regulatory factor X4 in type 1 narcolepsy. Sci. Rep. 11(1), 7841 (2021).
Andlauer, O. et al. Predictors of hypocretin (orexin) deficiency in narcolepsy without cataplexy. Sleep 35(9), 1247-1255F (2012).
Liblau, R. S., Vassalli, A., Seifinejad, A. & Tafti, M. Hypocretin (orexin) biology and the pathophysiology of narcolepsy with cataplexy. Lancet Neurol. 14(3), 318–328 (2015).
Geng, C., Yang, Z., Xu, P. & Zhang, H. Psychological status and serum uric acid levels in narcolepsy with type 1: A case-control study. J. Clin. Neurosci. 97, 17–20 (2022).
Kachooei-Mohaghegh-Yaghoobi, L., Rezaei-Rad, F., Sadeghniiat-Haghighi, K. & Zamani, M. The impact of the HLA DQB1 gene and amino acids on the development of narcolepsy. Int. J. Neurosci. https://doi.org/10.1080/00207454.2020.1835903 (2020).
Bourgin, P., Zeitzer, J. M. & Mignot, E. CSF hypocretin-1 assessment in sleep and neurological disorders. Lancet Neurol. 7(7), 649–662 (2008).
Kornum, B. R., Faraco, J. & Mignot, E. Narcolepsy with hypocretin/orexin deficiency, infections and autoimmunity of the brain. Curr. Opin. Neurobiol. 21(6), 897–903 (2011).
Cohen, A., Mandrekar, J., St Louis, E. K., Silber, M. H. & Kotagal, S. Comorbidities in a community sample of narcolepsy. Sleep Med. 43, 14–18 (2018).
Kok, S. W. et al. Altered setting of the pituitary-thyroid ensemble in hypocretin-deficient narcoleptic men. Am. J. Physiol. Endocrinol. Metab. 288(5), E892-899 (2005).
Sobol, D. L. & Spector, A. R. Levothyroxine improves subjective sleepiness in a euthyroid patient with narcolepsy without cataplexy. J. Clin. Sleep Med. 10(11), 1231–1232 (2014).
Li, H. et al. Increased hypocretin (orexin) plasma level in depression, bipolar disorder patients. Front. Psychiatry 12, 676336 (2021).
Messina, A. et al. Role of the orexin system on the hypothalamus-pituitary-thyroid axis. Front. Neural Circuits 10, 66 (2016).
Lopez, M., Tena-Sempere, M. & Dieguez, C. Cross-talk between orexins (hypocretins) and the neuroendocrine axes (hypothalamic-pituitary axes). Front. Neuroendocrinol. 31(2), 113–127 (2010).
Wang, X. et al. Relationship of free thyroxine and triiodothyronine on recurrence in maintenance therapy for bipolar depression. Asian J. Psychiatr. 71, 103086 (2022).
Esposito, S., Prange, A. J. Jr. & Golden, R. N. The thyroid axis and mood disorders: Overview and future prospects. Psychopharmacol. Bull. 33(2), 205–217 (1997).
Li, X. et al. Prevalence of depression or depressive symptoms in patients with narcolepsy: A systematic review and meta-analysis. Neuropsychol. Rev. 31(1), 89–102 (2021).
Sateia, M. J. International classification of sleep disorders-third edition: Highlights and modifications. Chest 146(5), 1387–1394 (2014).
Geng, C., Yang, Z., Kong, X., Xu, P. & Zhang, H. Association between thyroid function and disease severity in restless legs syndrome. Front. Neurol. 13, 974229 (2022).
Johns, M. W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 14(6), 540–545 (1991).
Buysse, D. J., Reynolds, C. F. 3rd., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 28(2), 193–213 (1989).
Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62 (1960).
Szakacs, A. et al. Endocrine and metabolic aspects of narcolepsy type 1 in children. Eur. J. Paediatr. Neurol. 33, 68–74 (2021).
Chabas, D. et al. Eating disorder and metabolism in narcoleptic patients. Sleep 30(10), 1267–1273 (2007).
Shan, L., Balesar, R., Swaab, D. F., Lammers, G. J. & Fronczek, R. Reduced numbers of corticotropin-releasing hormone neurons in narcolepsy type 1. Ann. Neurol. 91(2), 282–288 (2022).
Zaharna, M., Dimitriu, A. & Guilleminault, C. Expert opinion on pharmacotherapy of narcolepsy. Expert Opin. Pharmacother. 11(10), 1633–1645 (2010).
Riehl, J. et al. Chronic oral administration of CG-3703, a thyrotropin releasing hormone analog, increases wake and decreases cataplexy in canine narcolepsy. Neuropsychopharmacology 23(1), 34–45 (2000).
Martinez-Orozco, F. J. et al. Narcolepsy with cataplexy and comorbid immunopathological diseases. J. Sleep Res. 23(4), 414–419 (2014).
Kaufman, L. N., Corbett, S. W. & Keesey, R. E. Relationship of thyroid hormones and norepinephrine to the lateral hypothalamic syndrome. Metabolism 35(9), 847–851 (1986).
Suzuki, T., Kohno, H., Sakurada, T., Tadano, T. & Kisara, K. Intracranial injection of thyrotropin releasing hormone (TRH) suppresses starvation-induced feeding and drinking in rats. Pharmacol. Biochem. Behav. 17(2), 249–253 (1982).
Mitsuma, T. et al. Effects of orexin A on thyrotropin-releasing hormone and thyrotropin secretion in rats. Horm. Metab. Res. 31(11), 606–609 (1999).
Date, Y. et al. Orexins, orexigenic hypothalamic peptides, interact with autonomic, neuroendocrine and neuroregulatory systems. Proc. Natl. Acad. Sci. U.S.A. 96(2), 748–753 (1999).
Lechan, R. M. & Jackson, I. M. Immunohistochemical localization of thyrotropin-releasing hormone in the rat hypothalamus and pituitary. Endocrinology 111(1), 55–65 (1982).
Alkemade, A. Thyroid hormone and the developing hypothalamus. Front. Neuroanat. 9, 15 (2015).
Sakurai, T. Roles of orexins in the regulation of body weight homeostasis. Obes. Res. Clin. Pract. 8(5), e414-420 (2014).
Zhao, S. et al. Comparison of thyroid function in different emotional states of drug-naive patients with bipolar disorder. BMC Endocr. Disord. 21(1), 210 (2021).
Author information
Authors and Affiliations
Contributions
W.-H.L. wrote first draft and statistics; J.-M.R. conceptualization, resources and supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, H., Jia, M. Analysis of thyroid function and related factors in narcolepsy patients. Sci Rep 13, 18494 (2023). https://doi.org/10.1038/s41598-023-45321-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45321-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.