Abstract
Pancreatic ductal adenocarcinoma (PDAC) features a dense desmoplastic stroma, which raises the intratumoral interstitial pressure leading to vascular collapse and hypoxia, inducing angiogenesis. Vascular growth factors, such as vascular endothelial growth factor (VEGF) and angiopoietin-2 (Ang-2), increase in PDAC. A high VEGF and a high circulating Ang-2 associate with shorter survival in PDAC. In addition to the circulatory Ang-2, PDAC endothelial and epithelial cells express Ang-2. No correlation between tumor epithelial nor endothelial cell Ang-2 expression and survival has been published. We aimed to examine Ang-2 expression and survival. This study comprised PDAC surgical patients at Helsinki University Hospital in 2000–2013. Ang-2 immunohistochemistry staining was completed on 168 PDAC patient samples. Circulating Ang-2 levels were measured using ELISA in the sera of 196 patients. Ang-2 levels were assessed against clinical data and patient outcomes. A low tumor epithelial Ang-2 expression predicted shorter disease-specific survival (DSS) compared with a high expression (p = 0.003). A high serum Ang-2 associated with shorter DSS compared with a low circulating Ang-2 (p = 0.016). Ang-2 seemingly plays a dual role in PDAC survival. Further studies are needed to determine the mechanisms causing tumor cell Ang-2 expression and its positive association with survival.
Similar content being viewed by others
Introduction
Pancreatic ductal adenocarcinoma (PDAC) carries the worst prognosis among the major cancers. PDAC’s absolute numbers have been steadily increasing in the western world due to the growing number of people at risk. Some researchers predict PDAC will become the second leading cause of cancer death by 2030, falling below lung cancer1. PDAC has a notable fibro-inflammatory component. Chronic pancreatitis is one of the best-known risk factors for PDAC2,3, and a high C-reactive protein (CRP) predicts poor survival better than any other currently known serum marker4. The fibro-inflammatory reaction leads to a dense tumor desmoplasia and a high interstitial pressure leading to vascular collapse and hypoxia5. Vascular growth factors are secreted in the interplay between the stromal and epithelial cells as a response to hypoxia and inflammation6,7.
Angiopoietins are a family of growth factors that regulate vascular remodelling and angiogenesis. Angiopoietin-1 (Ang-1) is continuously secreted from perivascular cells. By binding to its receptor Tie-2, Ang-1 maintains vascular stability. Angiopoietin-2 (Ang-2), however, has far more complex effects. Inflammation and hypoxia cause endothelial cells to express Ang-2, although, depending on the context, Ang-2 can act as a Tie-2 antagonist or weak agonist, causing vessel destabilization, endothelial cell sprouting, angiogenesis, recruitment of myeloid cells, and lymphangiogenesis8. In preclinical tumor models, Ang-2 stimulated tumor angiogenesis and loosened endothelial cell-to-cell junctions enhancing metastasis9,10.
Circulating Ang-2 increases in numerous diseases associated with inflammation and angiogenesis, such as cancer8. A high serum Ang-2 appears to associate with a poor prognosis in colorectal and lung cancer11,12, whereas a high tumor endothelial Ang-2 expression associates with a poor prognosis in some but not all cancers13,14. Furthermore, a high tumor stromal Ang-2 expression in non-small cell lung carcinoma associated with a better prognosis15.
With its strong inflammatory element, it comes as no surprise that serum Ang-2 is upregulated in PDAC as well. Shultz et al. found that a high (≥ 75th percentile) serum Ang-2 associates with a shorter survival in PDAC16. It is striking that Ang-2 expression was reported not only in the endothelial cells, but also in pancreatic cancer epithelial cells16,17. While a high circulating Ang-2 level has been associated with a poorer prognosis, no association between tumor epithelial nor endothelial Ang-2 expression and survival in PDAC has been published thus far.
This study aimed to investigate the effect of Ang-2 protein in survival. We did so by comparing the associaton between circulating Ang-2 using enzyme-linked immunosorbent assay (ELISA) and the pancreatic tumor expression of Ang-2 using immunohistochemistry in both the cancer cell and endothelial expressions of Ang-2.
Results
Patient samples
The study setting consisted of 216 patients operated on at Helsinki University Hospital between 2000 and 2013. Tissue for immunohistochemistry was available from 168 patients and serum from 196 patients. We only included patients with pancreatic ductal adenocarcinoma without neoadjuvant therapy in the study. The median age at surgery was 65 years (range 39–84). Clinical data were obtained from patient records and survival data were provided by the Finnish Population Registration Center and Statistics Finland.
Immunohistochemical staining
Ang-2 was expressed both in the cytoplasm of pancreatic cancer epithelial cells and in the endothelial cells (Fig. 1A).
Both tumor epithelial and endothelial cells, as well as lymphocytes stained positive for Ang-2. (A) Tumor epithelial (black arrows in left column) and endothelial (black arrows in right column) staining of Ang-2 with staining intensity ranging from negative (0) to strong (3). (B) Double stainings of consecutive tissue slides show Ang-2 expression in blood vessel coating endothelial cells (CD31, black arrow head) and lymphocytes (CD45, red circle).
Tumor epithelial Ang-2 expression
Of the 168 tissue microarray (TMA) samples, 158 (94.0%) contained sufficient representative tumor tissue to allow for the evaluation of Ang-2 epithelial staining (Fig. 1A). Nearly half of the patients (77 patients, 48.7%) showed a moderate expression of Ang-2. Scores were dichotomized based on their Ang-2 expression. Negative to low scores (< 2) were categorized as low expression and moderate to strong (≥ 2) scores were categorized as high expression (Fig. 1A). Only two out of the 158 stained tumors were completely Ang-2 negative in their epithelium (1.3%). An additional two tumors had one section with negative Ang-2 expression, but expressed Ang-2 in other parts of the tumor epithelium (see Supplementary Table 1).
Association between tumor epithelial Ang-2 expression and clinicopathological variables
The intensity of the tumor epithelial Ang-2 expression was not significantly associated with age, sex, stage, lymph node metastasis, grade, tumor size, perineural, or perivascular infiltration (Table 1).
The epithelial Ang-2 intensity negatively correlated with carbohydrate antigen 19-9 (CA19-9) (p = 0.001, Spearman’s rho − 0.261). There was no statistically significant correlation between epithelial Ang-2 expression with either CRP or carcinoembryonic antigen (CEA) (p = 0.958, Spearman’s rho -0.005 and p = 0.227, Spearman’s rho − 0.099).
Endothelial Ang-2 expression
Of the 168 TMA samples, 159 (94.6%) contained sufficient representative tissue to allow for the evaluation of the Ang-2 endothelial staining. Ang-2 was expressed in the endothelial cells of pancreatic tumors (Fig. 1A). To confirm the cell type as endothelial cells, we performed double staining of consecutive slides using endothelial marker CD31 (Fig. 1B).
In accordance with the tumor Ang-2 expression, nearly half of the patients (73 patients, 45.9%) showed a moderate endothelial expression of Ang-2 (Table 2). We dichotomized the scores with negative to low scores (< 2) as a low expression and moderate to strong (≥ 2) scores were categorized as a high expression (Fig. 1A). None of the patients had a negative Ang-2 expression in their endothelium (Supplementary Table 2).
In addition to the previously described tumor epithelial and endothelial, we noticed in a small proportion of tumors the presence of a population of Ang-2 expressing lymphocyte-like cells (Fig. 2Ac.), which were confirmed as lymphocytes in double staining using common lymphocyte marker CD45 (Fig. 1B).
Histologically normal pancreatic tissue stains positive for Ang-2. Whole block slides of (A). PDAC tissue (a.) with adjacent ductal and acinar (b.) structures of the normal pancreas. Endothelial cells of a vessel with surrounding lymphocytes are shown in c. (B) normal pancreatic tissue adjacent to neuroendocrine tumor with endothelial (a.), ductal (b.) and acinar (c.) cells staining positive for Ang-2. Black arrows points at acinar structures and red arrow at ductal.
Association between endothelial Ang-2 expression and clinicopathological variables
The intensity of the endothelial Ang-2 expression did not significantly associate with age, sex, stage, lymph node metastasis, grade, tumor size, perineural, or perivascular infiltration (Table 1).
In contrast to the epithelial Ang-2 expression, endothelial Ang-2 intensity correlated positively with CA19-9 (p = 0.012, Spearman’s rho 0.218). There was no statistically significant correlation with either CRP or CEA (p = 0.349, Spearman’s rho − 0.166 and p = 0.160, Spearman’s rho 0.124). The tumor epithelial and endothelial expressions of Ang-2 showed a positive correlation (p = 0.017, Spearman’s rho 0.240).
Ang-2 expression in histologially benign pancreatic tissue
We found that Ang-2 expression was not limited to the tumor tissue alone (Fig. 2A). To investigate this further we stained PDAC whole block slides with Ang-2 (n = 5). We found that in addition to the PDAC tumor tissue (Fig. 2Aa), histologically benign pancreatic ductal and acinar (Fig. 2Ab.) tissue also showed positive Ang-2 staining. To determine whether it was due to the closely located PDAC (and subsequent inflammation), we stained whole block slides from neuroendocrine tumors with Ang-2 (n = 5) (Fig. 2B). Again, histologically benign pancreatic ductal (Fig. 2Bb.) and acinar (Fig. 2Bc.) tissue stained positive for Ang-2. Also endothelial cells of vessels within the histologically normal pancreatic tissue (Fig. 2Ac., Bd.) stained positive for Ang-2.
ELISA
The optimal cut-off of 2.83 ng/ml for serum Ang-2 was found through a time-dependent receiver operating curve (ROC) analysis. The median circulating Ang-2 level in patients with PDAC was 2.72 (range 0.36–26.88). Only three patients had Ang-2 expression levels exceeding 10 ng/ml. We found no significant correlation between the serum Ang-2 and the Ang-2 level in the tumor epithelial (p = 0.330, Spearman’s rho − 0.079) or endothelial (p = 0.600, Spearman’s rho − 0.041) immunohistochemistry (IHC) staining.
Association between serum Ang-2 expression and clinicopathological variables
A high lymph node ratio (ratio above 20%) was more common in patients with higher levels of circulating Ang-2 (33% versus 17%, p = 0.01). The level of circulating Ang-2 did not significantly associate with age, sex, tumor stage, grade, size, number of lymph node metastasis, perivascular infiltration, or perineural infiltration (Table 1).
The serum Ang-2 expression correlated positively with CEA (p = 0.005, Spearman’s rho 0.205) and CRP (p < 0.001, Spearman’s rho 0.286). The circulating Ang-2 showed no statistically significant correlation with CA19-9 (p = 0.106, Spearman’s rho 0.118).
Schultz et al.9 previously reported that a serum Ang-2 exceeding the 75th percentile associated with a higher degree of lymph node metastasis. While in our series the serum Ang-2 did not significantly associate with the lymph node metastasis ratio directly, we separately examined high versus low serum Ang-2 expressions. We found a positive correlation between a > 20% lymph node ratio (LNR) and serum Ang-2 levels exceeding the 50th (p = 0.41, Spearman’s rho 0.149) and 75th (p = 0.005, Spearman’s rho 0.203) percentile. An LNR < 20% was found in 19% versus 39.1% of patients with lower than versus higher than 75th percentile serum Ang-2 expression levels (p = 0.010).
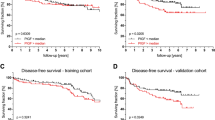
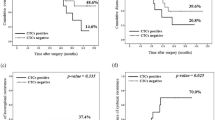
Survival analysis
In a univariate analysis, a stronger Ang-2 tumor epithelial expression associated with a better prognosis (lower hazard ratio [HR]; Table 2). Furthermore, this result persisted in a multivariate analysis (low versus high Ang-2 expression; HR = 0.49; 95% confidence interval [CI] 0.31–0.78; p = 0.003) adjusted for age, sex, stage, adjuvant therapy, radical (R0) surgery, and tumor markers CA19-9, CRP, and CEA (Table 3). We detected a shorter disease specific survival (DSS) in patients with a low tumor epithelial Ang-2 expression (median 1.33; 95% CI 0.50–2.16) when compared with those with an intermediate to high expression (median 2.40; 95% CI 1.86–2.94; p = 0.003; Fig. 3A).
No statistically significant association was found between the endothelial Ang-2 expression and prognosis in univariate analysis (p = 0.66; Table 2; Fig. 3B).
A high serum Ang-2 expression associated with a poorer prognosis according to a univariable analysis (p = 0.016; HR = 1.45; 95% CI 1.07–1.97; Table 2). A multivariable analysis (Ang-2 expression: HR = 1.48; 95% CI 1.08–2.04; p = 0.015), adjusted for age, sex, stage, adjuvant therapy, and radical (R0) surgery, was significant. Yet, when CA19-9, CRP, and CEA were added to the model, the multivariable analysis was not significant (p = 0.081). In addition, a high serum Ang-2 expression associated with a shorter DSS (median 1.63; 95% CI 1.37–1.89 years) when compared with patients with a lower serum Ang-2 expression (median 2.74; 95% CI 2.33–3.16; p = 0.016; Fig. 4).
Discussion
In this study, we found that tumor epithelial Ang-2 expression strongly and significantly associates with PDAC survival whereby a higher tumor expression of Ang-2 predicts a better survival. By contrast, a higher serum Ang-2 level predicts a poorer survival.
In concordance with our findings, one previous study has found higher serum Ang-2 levels to be associated with poorer prognosis (and a higher number of lymph node metastases in PDAC)9. However, in that study, the association was found in serum Ang-2 levels over the 75th percentile. In our patient samples series, the levels of serum Ang-2 were generally lower than those reported by Schulz et al., and neither the 75th percentile of our sample nor the cut-off used in the Schultz et al. study predicted survival in our cohort9. The ratio of positive lymph node metastases was, however, higher in patients with a higher than 50th and 75th percentile serum Ang-2, which agrees with Schultz et al.’s findings.
The association between serum Ang-2 and tumor (epithelial and endothelial) Ang-2 expression was inverse in our study, as discussed later. This inverse relationship suggests that the serum Ang-2 is secreted from sources outside the tumor; most probably from the systemic vasculature. The exact origin of the serum Ang-2 can, however, not be answered by the means of this study. Alternatively, epithelial Ang2 staining might in theory represent Ang2 bound to a cell surface receptor in epithelial cells.
Schultz et al. found that Ang-2 was transcriptionally active only in transformed ductal cells, but not in the cells of a normal pancreas9. Indeed, Ang-2 expression is known to be enhanced in KRAS mutated cancers through transcriptional upregulation mediated by FOXC2 transcription factor18. In our study, however, also histologically normal pancreatic epithelium expressed Ang-2. Further, in the Human Protein Atlas, the glandular cells in a normal exocrine pancreas express Ang-2 at moderate levels19.
While previous studies have confirmed that Ang-2 is expressed in the epithelial cells of PDAC tumors, to our knowledge this is the first time the association between Ang-2 expression and survival has been examined. Surprisingly, we found that the relationship between tumor epithelial Ang-2 and survival was opposite of that of serum Ang-2 and survival.
Commercial pancreatic cell lines such as Mia Paca-2, PANC-1, and AsPC-1 have been shown to express Ang-2 mRNA9,20, and their aggressiveness is associated, and can be induced by upregulation of Ang-29,20. Further, downregulation of Ang-2 has been shown to suppress invasion and colony formation of pancreatic cell lines in vitro20. In addition, both Ang-2 silencing in pancreatic cancer cells and intratumoral injection of miR-145 (causing downregulation of presumably both tumor epithelial and endothelial Ang-2) slowed the growth of pancreatic xenografts in nude mice20,21,22. Based on our results, it seems that the effect of tumor epithelial Ang-2 on prognosis is, however, far more complicated in PDAC patients than suggested by preclinical models. Indeed, albeit promising preclinical results, Ang-2 inhibitors have showed limited effect in clinical trials23,24.
It needs to be noted that in addition to of the Ang-2 Tie-2 signaling pathway, Ang-2 is also known activate integrins signaling25,26. The integrin signaling of Ang-2 is known to be involved in the autocrine signaling between PDAC epithelial cells9 and regulate tumor matrix metalloproteinase (MMP) expression27,28. Clinical trials modifying tumor extracellular matrix in PDAC, such as the HALO-trial, have taught us that the results of such modifications are not always straightforward29.
In addition, Ang-2 is known to affect the immune cell environment of the tumor30,31. The most promising results from Ang-2 inhibitors have been gained from combination treatment with either immunotherapy or other anti-angiogenic drugs9. Whereas many of the prior studies have been conducted in immunodeficient mice, Schmittnaegel et al. showed that in immunocompetent models combined Ang2 and VEGF blocking antibody therapy relied on cytotoxic T cells32. Further research is needed to explore the role of immune cells in the prognosis associated with Ang-2 expression.Overall, the underlying mechanism (and cellular components involved) leading to the better prognosis in Ang-2 expressing tumor epithelial cells is of importance and should be addressed in future studies. Most importantly, this should be investigated before considering the use of anti-Ang-2 therapies in PDAC patients.
The endothelial Ang-2 expression did not, in our study, correlate with PDAC survival. Immunohistochemical analysis of endothelial Ang2 in other cancer types has shown variable correlation with survival, for example13 showed that high endothelial Ang2 in RCC correlated with better prognosis, whereas33 showed that high Ang2 correlated with poor prognosis in glioblastoma. Nasarre et al. have showed using preclinical models that endothelial Ang-2 is vital during the early stages of tumorigenesis, and both sarcoma and melanoma tumor cells grew slower into tumors in Ang-2 deficient mice. However, the tumor growth during later stages were unchanged between Ang-2 deficient and wild type mice34. The blockade of Ang-2 can also induce vascular normalization, rather than vascular depletion8. The balance of decreasing delivery of nutrients and thereby inhibiting tumor growth—but not impairing the routes cytostatic drugs to enter the tumor is, again, not straighforward.
Regardless of the underlying mechanism, our findings suggest that the local inflammatory (tumor Ang-2 expression) state associates with a better prognosis, while the systemic inflammation (serum Ang-2) associates with a poorer prognosis. This agrees with previous findings in PDAC as well as in other cancers whereby local inflammatory responses appear beneficial to patient survival, while systemic inflammation is disadvantageous35.
Another interesting finding from this study was the cytosolic Ang-2 expression in intratumoral lymphocytes. Monocytes and macrophages are known to express Tie-2. To the best of our knowledge, the expression of Ang-2 within lymphocytes has not previously been described in the literature. However, many of the stromal cells reportedly expressing Ang-2 are lymphocytes, based on images in an article by Andersen et al.15. In addition, the Single Cell Expression Atlas shows Ang-2 expressing lymphocytes in glioblastoma36, while chronic lymphocytic leukemia cells also show immunoreactivity to Ang-237. The Human Protein Atlas also shows Ang-2 expression in immune cells, such as basophils19. Perhaps, the cytosolic Ang-2 staining in fact results from its expression within lymphocytes. However, further studies are required to confirm this supposition.
The strength of this study lies in the large cohorts we analyzed with long follow-up times and reliable clinical data. Since patients were recruited to the study when awaiting pancreatic surgery, the number of stage IV patients remained rather low in our series (n = 8). This does not reflect the general PDAC population, > 80% of whom present with inoperable tumors. Further studies are needed to determine how high serum Ang-2 levels are in widely metastasized PDAC and how it predicts survival in such patients. It would also be interesting to determine whether Ang-2 expression is detectable in the metastatic sites of PDAC, given that histological samples from PDAC metastases are rarely available. The optimal cut-off for serum Ang-2 was found through a time-dependent ROC analysis. Using this cut-off, the Kaplan–Meier as well as the Cox regression analyses were significant, as was the multivariable model. However, the serum Ang-2 results should be interpreted carefully, since this cut-off value has not been employed in a different cohort.
In summary, we identify here an interesting potential dual role of Ang-2 in PDAC: the local beneficial effect of tumor epithelial Ang-2 and the role of serum Ang-2 as a predictor of a poor prognosis. Further studies are needed to identify the mechanisms causing tumor epithelial Ang-2 and normal pancreatic expression, along with the positive association with survival.
Methods
Ethical approval
The Surgical Ethics Committee of Helsinki University Hospital (Dnro HUS 226/E6/06, extension TMK02 §66 17.4.2013) and the National Supervisory Authority of Health and Welfare (Valvira Dnro 10041/06.01.03.01/2012) approved the study. Patients provided their written informed consent upon inclusion in the study Patient information, samples and data were handled and stored in accordance with the Declaration of Helsinki and other local regulations.
Preparation of tumor tissue microarrays and immunohistochemistry
We collected paraffin-embedded surgical samples from the archives of the Department of Pathology, Helsinki University Hospital. The histopathological diagnosis of PDAC was re-evaluated by two experienced pathologists. Representative regions of a tumor were marked on haematoxylin & eosin-stained slides. Tissue microarray blocks were prepared and six 1.0-mm punches from each tumor sample were cut using a semiautomatic tissue microarrayer (Tissue Arrayer 1, Beecher Instruments Inc., Silver Spring, MD, USA). TMA blocks were cut into 4-μm sections, deparaffinized, rehydrated, and incubated in a Tris–HCl buffer at 98 ºC for 20 min. TMA slides were stained in an Autostainer 480 (Lab Vision Corp., Fremont, CA, USA) using the Dako REAL EnVision Detection system. We used goat polyclonal antibodies to human Angiopoietin-2 (Serial number AF623, amino acid residues Asp68-Phe496, 1:800, 0.2 mg/ml, R&D Systems, Minneapolis, MN, USA). Samples of colon tissue and normal lymph nodes served as positive controls in each staining series. To increase the representativeness, a total of six spots were examined per patient. These spots were from different areas of a PDAC tumor.
Immunohistochemistry staining was conducted on 159 PDAC patient samples. We chose five whole PDAC tissue blocks to evaluate Ang-2 expression in tumor-adjacent tissue. Double staining of Ang-2 together with endothelial marker CD31 and common lymphocyte marker CD45 were done on four of these whole tissue blocks to confirm the cell types of Ang-2 expressing cells. An additional five sections of a normal pancreas were obtained from surgeries removing local pancreatic neuroendocrine tumors.
Evaluation of staining
Cytoplasmic staining of Ang-2 in both pancreatic tumor cells as well as tumor endothelial cells were blindly scored by two examiners (MJ and JH), the second of whom is an experienced pathologist. The staining intensity was categorized as negative (0), weakly positive (1), moderately positive (2), and strongly positive (3) (Fig. 1A). The investigators were blinded to each other’s scores as well as to the clinical data. In the event that the intensity was scored differently between investigators, a consensus score was determined through discussion. A median score for each sample was calculated.
ELISA
ELISA were performed on 196 patient serum samples. The assay was performed on an MTX LabSystems Multiskan EX reader (MTX LabSystems, Bradenton, FL, USA). We used the DuoSet methodology ELISA (DANG20, R&D Systems, Biotechne, Minneapolis, MN, USA) assay to measure circulating Ang-2 levels in patient sera. Samples were quantified by converting optical density values to concentrations (pg/ml) using a standard curve calculated in accordance with the manufacturer’s instructions. In this assay, the quantification limit was 46.9 pg/ml and the detection limit was 8.29 pg/mL. None of the samples showed concentrations lower than the quantification or detection limits. This method was described in greater detail elsewhere38. The optimal cut-off point was selected based on the Youden index and set to 2.83 ng/ml. Time-dependent ROC curve is shown in Supplementary Fig. 1.
Statistical analysis
Associations between Ang-2 and clinical data and patient characteristics were assessed using the Fisher’s exact test or the Cochran–Armitage test. Descriptive survival analysis was performed using the Kaplan–Meier method and groups were compared using the log-rank test. DSS was calculated from the day of surgery until death from PDAC or until the end of the follow-up period. The time-dependent receiver operating curve (ROC) was constructed for DSS at one year follow-up and the cut-off value for the serum Ang-2 was obtained by maximizing the Youden index, granting equal weight to sensitivity and specificity. Uni- and multivariable survival analyses were calculated using the Cox regression analysis. The Cox regression assumption of a constant hazard ratio over time was assessed by plotting the Schoenfeld residuals over time, and testing for a trend. No significant deviations from the proportional hazards assumptions were identified. Interactions were considered in the multivariable models, but no statistically significant interactions were detected after applying the Bonferroni correction for multiple testing. The non-parametric Spearman’s correlation coefficient (rho) was used to assess correlations between variables. We considered p ≤ 0.05 as stastistically significant, and all tests were two-sided. All statistical analyses were performed using SPSS version 27.0 (IBM SPSS Statistics version 27.0 for Mac; SPSS Inc., Chicago, IL, USA, an IBM Company) and R version 4.0.3 (Foundation for Statistical Computing, Vienna, Austria).
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Petersen, G. M. Familial pancreatic cancer. Semin. Oncol. 43(5), 548–553. https://doi.org/10.1053/J.SEMINONCOL.2016.09.002 (2016).
Kirkegård, J., Mortensen, F. V. & Cronin-Fenton, D. Chronic pancreatitis and pancreatic cancer risk: A systematic review and meta-analysis. Am. J. Gastroenterol. https://doi.org/10.1038/ajg.2017.218 (2017).
Lowenfels, A. B. et al. Pancreatitis and the risk of pancreatic cancer. International Pancreatitis Study Group. N. Engl. J. Med. 328(20), 1433–1437 (1993).
Salmiheimo, A. et al. Systemic inflammatory response and elevated tumour markers predict worse survival in resectable pancreatic ductal adenocarcinoma. PLoS One https://doi.org/10.1371/journal.pone.0163064 (2016).
Provenzano, P. P. et al. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell. 21(3), 418–429. https://doi.org/10.1016/J.CCR.2012.01.007 (2012).
McDonald, D. M. Angiogenesis and vascular remodeling in inflammation and cancer: Biology and architecture of the vasculature. In Angiogenesis: An Integrative Approach From Science to Medicine. https://doi.org/10.1007/978-0-387-71518-6_2 (2008).
Longo, V. et al. Angiogenesis in pancreatic ductal adenocarcinoma: A controversial issue. Oncotarget 7(36), 58649–58658. https://doi.org/10.18632/ONCOTARGET.10765 (2016).
Saharinen, P., Eklund, L. & Alitalo, K. Therapeutic targeting of the angiopoietin-TIE pathway. Nat. Rev. Drug. Discov. 16(9), 635–661. https://doi.org/10.1038/NRD.2016.278 (2017).
Schulz, P. et al. Angiopoietin-2 drives lymphatic metastasis of pancreatic cancer. FASEB J. 25(10), 3325–3335. https://doi.org/10.1096/FJ.11-182287 (2011).
Holopainen, T. et al. Effects of angiopoietin-2-blocking antibody on endothelial cell–cell junctions and lung metastasis. J. Natl. Cancer Inst. 104(6), 461–475. https://doi.org/10.1093/JNCI/DJS009 (2012).
Jary, M. et al. Molecular description of ANGPT2 associated colorectal carcinoma. Int. J. Cancer 147(7), 2007–2018. https://doi.org/10.1002/IJC.32993 (2020).
Xu, Y. et al. The role of serum angiopoietin-2 levels in progression and prognosis of lung cancer: A meta-analysis. Medicine https://doi.org/10.1097/MD.0000000000008063 (2017).
Lampinen, A. M. et al. Novel angiogenesis markers as long-term prognostic factors in patients with renal cell Cancer. Clin. Genitourin. Cancer 15(1), e15–e24. https://doi.org/10.1016/J.CLGC.2016.07.008 (2017).
Dong, Z. et al. Ang-2 promotes lung cancer metastasis by increasing epithelial-mesenchymal transition. Oncotarget 9(16), 12705–12717. https://doi.org/10.18632/ONCOTARGET.24061 (2018).
Andersen, S. et al. Prognostic impacts of angiopoietins in NSCLC tumor cells and stroma: VEGF-A impact is strongly associated with Ang-2. PLoS One https://doi.org/10.1371/JOURNAL.PONE.0019773 (2011).
Schulz, P. et al. Angiopoietin-2 drives lymphatic metastasis of pancreatic cancer. FASEB J. https://doi.org/10.1096/fj.11-182287 (2011).
Durkin, A. J. et al. Differential expression of the Tie-2 receptor and its ligands in human pancreatic tumors. J. Am. Coll. Surg. https://doi.org/10.1016/j.jamcollsurg.2004.07.021 (2004).
Hosaka, K. et al. KRAS mutation-driven angiopoietin 2 bestows anti-VEGF resistance in epithelial carcinomas. Proc. Natl. Acad. Sci. U. S. A. https://doi.org/10.1073/PNAS.2303740120 (2023).
Pontèn, F., Jirström, K. & Uhlén, M. The human protein atlas—a tool for pathology. J. Pathol. 216(4), 387–393 (2008).
Wang, H. et al. MiR-145 functions as a tumor suppressor via regulating angiopoietin-2 in pancreatic cancer cells. Cancer Cell. Int. https://doi.org/10.1186/S12935-016-0331-4 (2016).
Zhou, J. et al. Anti-angiogenesis by lentivirus-mediated small interfering RNA silencing of angiopoietin-2 gene in pancreatic carcinoma. Technol. Cancer Res. Treat. https://doi.org/10.7785/tcrt.2012.500213 (2011).
Chen, H. M., Tsai, C. H. & Hung, W. C. Foretinib inhibits angiogenesis, lymphangiogenesis and tumor growth of pancreatic cancer in vivo by decreasing VEGFR-2/3 and TIE-2 signaling. Oncotarget https://doi.org/10.18632/oncotarget.3613 (2015).
Hyman, D. M. et al. Phase I study of MEDI3617, a selective angiopoietin-2 inhibitor alone and combined with carboplatin/paclitaxel, paclitaxel, or bevacizumab for advanced solid tumors. Clin. Cancer Res. 24(12), 2749–2757. https://doi.org/10.1158/1078-0432.CCR-17-1775 (2018).
Papadopoulos, K. P. et al. A phase I first-in-human study of nesvacumab (REGN910), a fully human anti-angiopoietin-2 (Ang2) monoclonal antibody, in patients with advanced solid tumors. Clin. Cancer Res. 22(6), 1348–1355. https://doi.org/10.1158/1078-0432.CCR-15-1221 (2016).
Felcht, M. et al. Angiopoietin-2 differentially regulates angiogenesis through TIE2 and integrin signaling. J. Clin. Invest. 122(6), 1991–2005. https://doi.org/10.1172/JCI58832 (2012).
Hakanpaa, L. et al. Endothelial destabilization by angiopoietin-2 via integrin β1 activation. Nat. Commun. https://doi.org/10.1038/NCOMMS6962 (2015).
Zhang, Z. X. et al. Knockdown of angiopoietin-2 suppresses metastasis in human pancreatic carcinoma by reduced matrix metalloproteinase-2. Mol. Biotechnol. 53(3), 336–344. https://doi.org/10.1007/S12033-012-9532-9 (2013).
Yu, X. & Ye, F. Role of angiopoietins in development of cancer and neoplasia associated with viral infection. Cells https://doi.org/10.3390/CELLS9020457 (2020).
Hakim, N., Patel, R., Devoe, C. & Saif, M. W. Why HALO 301 failed and implications for treatment of pancreatic cancer. Pancreas (Fairfax) 3(1), e1–e4. https://doi.org/10.17140/POJ-3-E010 (2019).
Scholz, A. et al. Angiopoietin-2 promotes myeloid cell infiltration in a β2-integrin-dependent manner. Blood 118(18), 5050–5059. https://doi.org/10.1182/BLOOD-2011-03-343293 (2011).
Coffelt, S. B. et al. Angiopoietin 2 stimulates TIE2-expressing monocytes to suppress T cell activation and to promote regulatory T cell expansion. J. Immunol. 186(7), 4183–4190. https://doi.org/10.4049/JIMMUNOL.1002802 (2011).
Schmittnaegel, M. et al. Dual angiopoietin-2 and VEGFA inhibition elicits antitumor immunity that is enhanced by PD-1 checkpoint blockade. Sci. Transl. Med. https://doi.org/10.1126/SCITRANSLMED.AAK9670 (2017).
Scholz, A. et al. Endothelial cell-derived angiopoietin-2 is a therapeutic target in treatment-naive and bevacizumab-resistant glioblastoma. EMBO Mol. Med. 8(1), 39–57. https://doi.org/10.15252/EMMM.201505505 (2016).
Nasarre, P. et al. Host-derived angiopoietin-2 affects early stages of tumor development and vessel maturation but is dispensable for later stages of tumor growth. Cancer Res. 69(4), 1324–1333. https://doi.org/10.1158/0008-5472.CAN-08-3030 (2009).
Imrie, C. W. Host systemic inflammatory response influences outcome in pancreatic cancer. Pancreatology 15(4), 327–330. https://doi.org/10.1016/J.PAN.2015.04.004 (2015).
Darmanis, S. et al. Single-cell RNA-seq analysis of infiltrating neoplastic cells at the migrating front of human glioblastoma. Cell Rep. 21(5), 1399–1410. https://doi.org/10.1016/J.CELREP.2017.10.030 (2017).
Maffei, R. et al. Angiopoietin-2 plasma dosage predicts time to first treatment and overall survival in chronic lymphocytic leukemia. Blood 116(4), 584–592. https://doi.org/10.1182/BLOOD-2009-11-252494 (2010).
Lukasz, A. et al. Circulating angiopoietin-1 and angiopoietin-2 in critically ill patients: Development and clinical application of two new immunoassays. Crit. Care https://doi.org/10.1186/CC6966 (2008).
Acknowledgements
We thank Pia Saarinen for her indispensable technical assistance.
Author information
Authors and Affiliations
Contributions
Conception: M.R., H.S., P.S., and C.H. Data curation: M.R., T.K., H.M., J.H., and J.H. Analysis of data: H.M., T.K., M.R., H.S., and C.H. Preparation of the manuscript: M.R., T.K., H.M., H.S., P.S., and C.H. Revision for important intellectual content: All authors. Supervision: H.S. and C.H.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roos-Mattila, M., Kaprio, T., Mustonen, H. et al. The possible dual role of Ang-2 in the prognosis of pancreatic cancer. Sci Rep 13, 18725 (2023). https://doi.org/10.1038/s41598-023-45194-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45194-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.