Abstract
Coronary artery disease (CAD) is one of the principal causes of death worldwide. Among several predisposing factors, inflammation and inflammatory genes play a significant role in disease pathogenesis. Inflammatory microRNAs, small noncoding RNAs involved in regulating inflammation, are promising candidates for understanding pathogenesis of CAD and developing diagnostic biomarkers. The aim of the study was to evaluate the alteration of miR-200c, miR-125b, miR-27b, miR-203 and, miR-155 in patients suffering from coronary artery stenosis and insignificant coronary artery stenosis compared to healthy subjects. In this study we compared expressions of five inflammatory miRNAs in peripheral blood mononuclear cells (PBMCs) of 72 patients suffering significant coronary artery stenosis (CAD), 74 individuals without coronary artery disease and 30 individuals with insignificant coronary artery stenosis (ICAD). After blood collection, PBMCs were isolated and RNA was extracted. Gene expression levels were assessed by SYBR green based real-time PCR. Statistical analysis was performed using R program. Expression levels of miR-200c, miR-203, and miR-155 were lower in subjects with ICAD than that in CAD patients and subjects of the control group. MiR-125b was downregulated in CAD and ICAD groups compared to the control group. PBMC miR-27b was upregulated in the CAD group as compared to the ICAD and control groups. Receiver operating characteristic curve analysis verified potential of three miRNAs in separating subjects with ICAD from CAD patients and healthy individuals. In conclusion, this original investigation suggested that altered expression of these five miRNAs may serve as a novel diagnostic biomarker discriminating clinical presentations of coronary artery diseases.
Similar content being viewed by others
Introduction
Heart diseases such as CAD are known as the most leading cause of death worldwide. CAD is divided into stable angina pectoris (SAP), unstable angina pectoris (UAP) and acute myocardial infarction (AMI) according to clinical manifestation1. This disorder is usually initiated with progressive blockage of the heart supplying major blood vessels or coronary arteries, which is called atherosclerosis. Atherosclerosis leads myocardial Perfusion defect and insults chronic inflammation with the recruitment of many inflammatory agents, such as cytokines, chemokines, and PBMCs as well as Lymphocyte and monocyte2.
PBMCs may serve as a noninvasive and powerful source for studying human health and disease diagnosis3. It has been shown that PBMCs of CAD patients exhibit a profile of inflammatory gene expression4. Recently, some reports have indicated the crucial effect of PBMCs microRNA profile in discriminating and early diagnosis of CAD3.
MicroRNAs are small non-coding RNAs that can bind to their target genes and attenuate their expression. Their alteration is found in different conditions and might serve as biomarkers5. MicroRNAs secreted from monocyte and lymphocytes can fine-tune the expression of inflammatory genes involved in atherogenesis6. The expression alteration of microRNAs is conceived in different steps of atherosclerosis and the microRNA signature may be a useful noninvasive tool in early identification of CAD7.
NF-κB (nuclear factor kappa B) is the key factor of inflammation activation which induces chemokines and cytokines production8. The Toll-like receptor 4 (TLR4)-mediated NF-κB pathway is among signaling pathways implicated in atherosclerotic-related inflammation that has attracted more attention9. TLR4 can trigger NF-κB signaling pathway to induce transcription of inflammatory genes9. Molecular mechanisms that influence the activity of NF-κB pathway have been shown to play crucial roles in modulating pathological processes in CAD. The current study was aimed at investigating the expression profile of five miRNAs that are involved in regulation of TLR/NF-κB pathways in PBMCs of patients suffering from coronary artery stenosis and insignificant coronary artery stenosis as compared to healthy subjects.
MiR-200c, miR-203, and miR-155 are the regulator of genes involved in inflammation and play roles in the NF-κB pathway. MiR-200c is involved in TLR4 signaling and can reduce NF-κB receptor activity10. It also inhibits IL-6, CXCL9, and TNF-α expression in THP-1 cells10. MiR-203 can suppress interlukin8 which induces NF-κB activation11,12. In addition, it can inactivate the NF-κB pathway through IKKα inhibition13. MiR-203 inactivates MEF2C expression that participates in heart development. Also, MEF2c can suppress inflammation through modulating the NF-κB pathway in endothelial cells14. MiR-155 is a controversial key regulator of the inflammatory processes and immune responses involved in pro-inflammatory cytokines induction15. In endothelial cells, miR-155 activated by TNF-α targets NF-κB, P65 and this negative feedback inhibits atherogenesis by TNF-α suppression16. MiR-125b targets TNF-α and TNF receptor-associated factor 6 (TRAF6) in the mouse heart and participates in the NF-kB pathway. Induction of its expression in the mouse heart ceases NF-kB pathway activation through TRAF6 and results in ischemia prevention17. MiR-27b belongs to the mir-27 family and is involved in the different biological pathways. In inflammatory processes TLR stimulation drives miR-27b expression in an NF-κB pathway18.
In the present study, we aimed to compare the PBMC expression of miR-200c, miR-203, miR-155, miR-125b, and miR-27b in subjects with significant or insignificant stenosis of coronary arteries and healthy subjects.
Materials and methods
Study population
As previously explained19, the case–control study population consisted of 176 subjects from Shahid Modarres hospital (Tehran, Iran). This included 102 and 74 subjects in the case and control groups, respectively. The case group was comprised of 72 patients suffering significant coronary stenosis [i.e., the CAD group, defined as ≥ 50% stenosis in at-least one coronary artery diagnosed by angiography20] and 30 participants with insignificant coronary stenosis [i.e., the ICAD group, < 50% coronary stenosis20]. The CAD subgroup was comprised of 32 subjects with unstable angina pectoris (UAP), 20 subjects with stable angina pectoris (SAP) and 20 subjects with acute myocardial infarction (AMI). Patients with a history of any CAD influential disorders as well as heart, liver, renal and infectious disease and neoplasia were excluded from the study. The Gensini score was computed for the evaluation of intensity and location of arteries obstruction. Same hospital clients with normal ECG and stress test sex- and age-matched with case group, randomly selected and compromised our control group and people with previously described exclusion criteria excluded from the control group19. Demographic data and clinical characteristics were collected from all groups. Informed consent was acquired from all project attendants. This study was supported by a grant (grant number: 62308) from clinical research development unit, Shohada hospital, Tabriz University of Medical Sciences (Tabriz, Iran) and had been performed in accordance with the Declaration of Helsinki. In addition, this study was approved by the ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1397.977).
PBMC isolation and RNA extraction
After collecting ~ 7 ml peripheral blood in EDTA-containing tubes, bloods were diluted with the same volume of the PBS solution. Afterwards, the PBMC isolation was accomplished by adding blood on Ficoll-Paque PLUS (Amersham Pharmacia Biotech, Sweden) and carrying out a centrifuge with 800 g for 20 min. The miRNeasy Mini Kit (Qiagen, Germany) was used for extraction of total RNA including small RNAs21. concentration and quality detection of microRNA were carried out by nanodrop. RNA measurement was conducted by measuring ultraviolet absorbance at 260 nm and 280 nm.
cDNA synthesis and qPCR assays
Each 10 µl reverse transcription reaction mix contained 500 ng RNA. The cDNA synthesis of all miRNAs (Table1) and their reference genes (i.e., RNU48, RNU44, and RNU24) was performed using the standard stem loop RT-qPCR primers and Strand cDNA Synthesis Kit (Clontech, Takara Bio, Japan) according to the its guidelines. the following program was used: 16 °C for 30 min, 42 °C for 30 min, and 5 min at 82 °C. The SYBR green based qPCR reactions were done in duplicates using the Light Cycler 96 instrument (Roche Diagnostics, Mannheim, Germany) for evaluating all gene expressions in 40 cycles at a 95 °C denaturation for 12 min, 60 °C annealing for 30 s and 95 °C extension for 10 s. Each 10 µL qPCR reaction contained 2 µL HOT FIREPol EvaGreen qPCR Mix Plus, 1 µL cDNA, 1 µL of each primer (5 pmol/µL), and 5 µL nuclease‐free water. The melt curve analysis evaluated the specificity of each reaction. The amplification efficiency of each reaction was more than 80%. Cq values and the processed fluorescence information were extracted from Light Cycler 96 software. The R software was applied for analyzing qPCR reactions efficiencies and calculating relative quantities (RQs). ΔCq and normalized relative quantity (NRQ) were computed as explained elsewhere21,22.
Statistical analysis
R software (version 3.5.1) was applied for data analysis. For testing quantitative variables normality, the Shapiro–Wilk test was used. In order to compare quantitative variable or categorical variable among study groups, Student’s t-test or Mann–Whitney U test and chi-squared tests were used respectively. The Welch’s ANOVA with the Games-Howell post hoc test or One-way ANOVA F test with Tukey’s HSD post hoc test was applied for gene expression comparison between more than two groups whenever expression values were distributed normally. In order to evaluate gene expression comparison between more than two groups without normally-distributed expression values, the Kruskal–Wallis one-way ANOVA with the Conover-Iman test were used. The ROC curve analysis estimated discrimination power of miRNAs and Youden’s method selected suitable threshold.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical principles and the national standards for conducting medical research in Iran and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by Research Ethics Committees of Tabriz University of Medical Sciences (Approval ID: IR.TBZMED.REC.1397.977).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Results
The study population was matched in terms of gender, mean age, the proportion of smoking individuals, or the proportion of participants suffering from diabetes, dyslipidemia, obesity, or hypertension (Table 2). Out of 72 patients with significant stenosis, 25 subjects had one vessel disease (i.e., only one vessel with stenosis), 15 subjects had two vessel disease and 32 subjects had three vessel diseases. Furthermore, the CAD group were comprised of 32 UAP, 20 AMI, and 20 SAP patients.
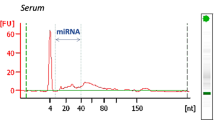
MicroRNA concentration and quality detection
The ratio of ultraviolet absorbance at 260 nm/280 nm for all samples was about 2 and they all have suitable purity.
The PBMC gene expression levels
There was no significant difference between subjects of the CAD and the control group in terms of the expression levels of miR-200c, miR-155 and miR-203 (all P values > 0.05, Fig. 1). Downregulation of miR-203, miR-200c and, miR-155 was found in insignificant CAD patients as compared to subjects of the CAD and the control group (miR-155: CAD vs. ICAD P: 0.004, ICAD vs. controls P: 0.004, miR-203: CAD vs. ICAD P < 0.001, ICAD vs. controls P < 0.001, miR-200c: CAD vs. ICAD P: 0.01, ICAD vs. controls P: 0.001, Fig. 1). Subjects of the control group had significantly higher expression levels of PBMC miR-125b than subjects of the CAD or ICAD group and CAD patients had higher levels of this miRNA as compared to the ICAD group (Fig. 1, miR-125b: CAD vs. ICAD P: 0.005, CAD vs controls P: 0.004). The PBMC level of miR-27b was lower in the ICAD group and control subjects as compared to the subjects of the CAD group (Fig. 1, miR-27b: CAD vs. ICAD P: 0.002, CAD vs. controls P < 0.001).
The comparison of the PBMC level of miR-200c (A), miR-125b (B), miR-27b (C), miR-155 (D), and miR-203 (E) in CAD, insignificant stenosis and the control group. Although no prominent difference was detected between subgroups of the CAD group (i.e., AMI, UAP, and SAP) (all P > 0.05), all subtypes had significant increase in terms of the levels of miR-200c, miR-155 and miR-203 compared to subjects of the ICAD group (Fig. 2).
Biomarker potential of PBMC expressions
The ROC curve analysis demonstrated that PBMC miR-200c, miR-203 and, miR-155 expression levels may discriminate subjects with insignificant stenosis (i.e., participants of the ICAD group) from patients with significant stenosis with reasonable specificity and sensitivity (miR-203: AUC [95%CI]: 0.75 [0.65 to 0.85], sensitivity: 0.63, specificity: 0.86, miR-155: AUC [95%CI]: 0.74 [0.64 to 0.84], sensitivity: 0.69, specificity: 0.79, miR-200C: AUC [95%CI]: 0.78 [0.69 to 0.87], sensitivity: 0.68, specificity: 0.89). The ROC curve analysis yielded an AUC of 0.68 (95% CI 0.6–0.77) for PBMC levels of miR-27b in discriminating CAD patients from healthy subjects (sensitivity: 0.5, specificity: 0.85). The figure for miR-125b was AUC of 0.64 (95% CI 0.55–0.73, sensitivity: 0.70, specificity: 0.58). PBMC miR-125 and miR-27b levels were also able to discriminate among subjects of CAD and ICAD groups with AUC of 0.69 (miR-125b 95% CI 0.58–0.80, sensitivity: 0.54, specificity; 0.82; miR-27b 95% CI 0.58–0.79, sensitivity: 0.55, specificity: 0.82). Moreover, PBMC levels of miR-200c, miR-203 and miR-155 could distinguish ICAD from AMI, UAP, SAP with acceptable sensitivity and specificity (Table 3).
Discussion
Cardiovascular diseases have the most burden of morbidity and mortality worldwide and CAD as a chronic inflammatory disease covers a large part of them1. In this investigation, we studied the PBMC expression levels of miR-200c, miR-203, miR-155, miR-125b, miR-27b in CAD, ICAD and healthy subjects. Downregulation of miR-203, miR-200c and, miR-155 was found in insignificant CAD patients while their expression was the same in CAD patients and, healthy controls. Although AMI, UAP and, SAP had higher expression levels than ICAD, there was no significant difference in expression of the three miRNAs between these subtypes. Furthermore, downregulation of miR-125b in ICAD compared with CAD and healthy group was confirmed. Mir-27b showed the highest expression level in CAD and its level were higher in ICAD compared to the controls. The ROC curve analysis suggested that the expression levels of miR-200c, mir-203 and, miR-155 can discriminate ICAD from other groups with acceptable specificity and sensitivity. Furthermore, miR-27b could discriminate CAD patients from controls and ICAD. Also, discriminating among CAD and ICAD groups could be effective with PBMC levels of miR-125b.
Satoh et al. evaluated TLR4-responsive miRNAs such as miR-200 in CAD patients and control groups plasma. Although microarray screening indicated mir-200c downregulation in CAD compared to non-CAD but real-time PCR adoption didn’t show any significant alteration of mir-200c in these groups23. miR-200 cluster upregulation suppresses not only inflammatory genes expression including IL-2, IL-4, IL-5, IL-10, IL-13, GM-CSF, INF-γ and, TNF-α but also an angiogenic promoting gene, VEGF-A in MDA-MB231 cells24. In another study, on the A549 and HUVEC cell lines, Shi, Liangliang et al. declared miR-200c influences VEGFR-2 expression and elevates the radiosensitivity of cancer cells. Therefore miR-200c inhibition results in angiogenesis increase25,26. Kemal Marc Akat et al.27 acclaimed miR-203 downregulation in heart failure. However, E.A.Polyakova et al.28 noticed miRNA-203 overexpression in serum and cardiomyocytes of patients with multiple coronary artery stenosis compared to controls. Zhi and colleagues have reported the increased levels of miR-203 in the rat heart under hypoxia29. Given that, VEGF-A and HIF‐1α are miR-203 targets involved in angiogenesis, miR‐203 hinders angiogenesis and, interferes with neo-angiogenic disorders as well as ischemic heart disease30,31. In addition, Liu F and his colleagues informed miR-203 can play role in fine-tuning of placental blood vessels formation by targeting VEGFA and VEGFR233. Julien Faccini et al.32 indicated, circulating MiR-155 downregulation is related to CAD. Guo-Fu Zhu et al.33 presented miR-155 downturn in PBMC and plasma of CAD patients compared to controls and the low levels of mir-155 are extended in patients with severe stenosis. However, in Leistner et al.34 study there are higher levels of mir-155 in trans coronary of patients with increased vulnerable plaques. MiR-155 is involved in HIF1α-mediated angiogenesis. Under the hypoxia condition, MIR-155 is upregulated and drives HIF-1α to fell45. VEGF motivates miR-155 expression leading to endothelial cells angiogenesis35. Albeit to the above description, some evidences exhibit the antiangiogenic function of mir-155. miR-155 reduces vascular inflammation arrests angiogenesis in endothelial cells of the mouse brain36,37. Caballero-Garrido and his colleagues suggested Mir-155 restriction can impede the generation of new vascular and angiogenesis38. Angiogenesis impression of miR-155 is specific considering to a cell-type39, so it can rationalize our results. Downregulation of miR-125b is found in myocardial tissues of mice with heart failure40. Plasma Downregulation of miR-125b compared with noncoronary heart disease is reported in Ding et al.41 research. Furthermore, they found a remarkable negative association between Gensini score and the level of miR-125b and miR-125b overexpression is related to Gensini score increase. Chen et al. showed overexpression of miR-125b leads to upregulation of many mitochondria fatty acid metabolism proteins and it is related to cardiac hypertrophy in mice too42. Mir-125b could serve as a biomarker in heart defects. This microRNA is a vascular regulator and its increased levels are reported in myocardial ischemia and leads to cardiac self-protection mechanisms activation43. After the Heart injury miR-125b level is increased due to myocardial restore44. miR-27b is a lipid metabolism regulator and takes apart in atherosclerotic development, inflammation and TGF-β signaling pathway regulation45,46. Its elevation was shown in the mice with cardiac hypertrophy and in a heart of a mouse model with a transverse aortic constriction (TAC)-induced cardiac hypertrophy respectively47,48. Moreover patients with left ventricular hypertrophy showed high expression of miR-27b in their serum49. Furthermore Mir-27b increase was found in patients with adverse paraclinical symptoms of heart failure and it could estimate cardiovascular death50.
In conclusion, in this investigation, we reported the variable expression levels of miR-200c, miR-203, miR-155, miR-125b and miR-27b in patients with ICAD. As we described in the introduction, all of these microRNAs participate in NF-kB signaling and are related to inflammation. However, miR-200c, miR-203, miR-155 and miR-125b are involved in angiogenesis. When atherosclerosis is initiated, angiogenesis and novel vessel development are formed to compensate for blood deficiency to the heart muscle. We reported a similar role for mir-196a in ICAD elsewhere19. The small plaque of individuals with insignificant coronary stenosis may deteriorate after 18–24 months and cause disabilities51. Therefore, the early diagnosis of ICAD is crucial20,51. About 30 percent of individuals referred to angiography are diagnosed with ICAD and less than 50 percent of their arteries are blocked51. Because of ischemia compensation, angiogenesis and numerous arteries formation is augmented in the early stages of CAD52. Accordingly, the expression profile of genes involved in this process is divergent to CAD and healthy controls. It worth mentioning that, to the best of our knowledge, this study is the first inquiry that investigates miR-203, miR-200c, miR-155, miR-125b and miR-27b in PBMCS of ICAD. We hope our findings facilitate the development off noninvasive diagnostic biomarkers. The discrepancy in results of different studies may accentuate the significance of evaluating gene expression profile based on specific cell type and further research is required to unravel the accurate molecular mechanism of these microRNAs, their accompanying components and, details of related pathways in PBMCs of patients with CAD.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Malakar, A. K. et al. A review on coronary artery disease, its risk factors, and therapeutics. J. Cell. Physiol. 234(10), 16812–16823 (2019).
Geovanini, G. R. & Libby, P. Atherosclerosis and inflammation: Overview and updates. Clin. Sci. 132(12), 1243–52 (2018).
Hoekstra, M. et al. The peripheral blood mononuclear cell microRNA signature of coronary artery disease. Biochem. Biophys. Res. Commun. 394, 792–797 (2010).
Jönsson, S., Lundberg, A. K., Chung, R. W. S. & Jonasson, L. Glucocorticoid sensitivity and inflammatory status of peripheral blood mononuclear cells in patients with coronary artery disease. Ann. Med. 50(3), 260–268 (2018).
Ehtesham, N., Mosallaei, M., Karimzadeh, M.R., Moradikazerouni, H. & Sharifi, M. microRNAs: key modulators of disease-modifying therapies in multiple sclerosis. Int. Rev. Immunol. (2020).
Duroux-Richard, I., Robin, M., Peillex, C. & Apparailly, F. MicroRNAs: Fine tuners of monocyte heterogeneity. Front. Immunol. 10, 2145 (2019).
Nariman-saleh-fam, Z. et al. Expression pattern of miR-21, miR-25 and PTEN in peripheral blood mononuclear cells of patients with significant or insignificant coronary stenosis. Gene. 698, 170–178 (2019).
Hong, L. et al. MicroRNA-200c Represses IL-6, IL-8, and CCL-5 Expression and enhances osteogenic differentiation. PLOS ONE. 11(8), e0160915 (2016).
Tang, Y. L. et al. TLR4/NF-κB signaling contributes to chronic unpredictable mild stress-induced atherosclerosis in ApoE-/- mice. PLoS One. 10(4), e0123685 (2015).
Wendlandt, E. B., Graff, J. W., Gioannini, T. L., McCaffrey, A. P. & Wilson, M. E. The role of microRNAs miR-200b and miR-200c in TLR4 signaling and NF-κB activation. Innate. Immun. 18(6), 846–855 (2012).
Manna, S. K. & Ramesh, G. T. Interleukin-8 induces nuclear transcription factor-kappaB through a TRAF6-dependent pathway. J. Boil. Chem. 280(8), 7010–7021 (2005).
Wei, T. et al. Interleukin-8 is regulated by miR-203 at the posttranscriptional level in primary human keratinocytes. Eur. J. Dermatol. EJD. https://doi.org/10.1684/ejd.2013.1997 (2013).
Ma, X., Becker Buscaglia, L. E., Barker, J. R. & Li, Y. MicroRNAs in NF-kappaB signaling. J. Mol. Cell. Biol. 3(3), 159–166 (2011).
Yu, Q., Zhao, M.-W. & Yang, P. LncRNA UCA1 suppresses the inflammation via modulating miR-203-mediated regulation of MEF2C/NF-κB signaling pathway in epilepsy. Neurochem. Res. 45(4), 783–795 (2020).
Chen, C. et al. NF-kB-regulated exosomal miR-155 promotes the inflammation associated with arsenite carcinogenesis. Cancer Lett. 388, 21–33 (2017).
Tahamtan, A., Teymoori-Rad, M., Nakstad, B. & Salimi, V. Anti-inflammatory MicroRNAs and their potential for inflammatory diseases treatment. Front. Immunol. 9, 1377 (2018).
Yang, K., Liu, X., Lin, W., Zhang, Y. & Peng, C. Upregulation of MicroRNA-125b leads to the resistance to inflammatory injury in endothelial progenitor cells. Cardiol. Res. Practice. 2020, 6210847 (2020).
He, X., Jing, Z. & Cheng, G. MicroRNAs: New regulators of toll-like receptor signalling pathways. BioMed Res. Int. 2014, 945169 (2014).
Saadatian, Z. et al. Peripheral blood mononuclear cells expression levels of miR-196a and miR-100 in coronary artery disease patients. Immunol. Investigat. 50(8), 914–24 (2020).
Tavella, R. et al. Natural history of patients with insignificant coronary artery disease. Eur. Heart J. Qual. Care Clin. Outcomes 2(2), 117–124 (2016).
Saadatian, Z. et al. Dysregulated expression of STAT1, miR-150, and miR-223 in peripheral blood mononuclear cells of coronary artery disease patients with significant or insignificant stenosis. J. Cell. Biochem. 120(12), 19810–19824 (2019).
Rieu, I. & Powers, S. J. Real-time quantitative RT-PCR: Design, calculations, and statistics. Plant Cell 21(4), 1031–1033 (2009).
Satoh, M. et al. Circulating Toll-like receptor 4-responsive microRNA panel in patients with coronary artery disease: Results from prospective and randomized study of treatment with renin–angiotensin system blockade. Clin. Sci. 128(8), 483–491 (2014).
Choi, S. K. et al. Overexpression of the miR-141/200c cluster promotes the migratory and invasive ability of triple-negative breast cancer cells through the activation of the FAK and PI3K/AKT signaling pathways by secreting VEGF-A. BMC Cancer 16, 570 (2016).
Gallach, S., Calabuig-Fariñas, S., Jantus-Lewintre, E. & Camps, C. MicroRNAs: Promising new antiangiogenic targets in cancer. BioMed. Res. Int. 2014, 878450 (2014).
Shi, L. et al. MiR-200c increases the radiosensitivity of non-small-cell lung cancer cell line A549 by targeting VEGF-VEGFR2 pathway. PLOS ONE 8(10), e78344 (2013).
Akat, K. M. et al. Comparative RNA-sequencing analysis of myocardial and circulating small RNAs in human heart failure and their utility as biomarkers. Proc. Natl. Acad. Sci. U S A 111(30), 11151–6 (2014).
Polyakova, E. A. et al. Association of myocardial and serum miRNA expression patterns with the presence and extent of coronary artery disease: A cross-sectional study. Int. J. Cardiol. 322, 9–15 (2020).
Zhi, F. et al. δ-Opioid receptor activation and microRNA expression in the rat heart under prolonged hypoxia. Cell. Physiol. Biochem. 39(3), 1118–1128 (2016).
Zhu, X. et al. miR-203 suppresses tumor growth and angiogenesis by targeting VEGFA in cervical cancer. Cell. Physiol. Biochem. Int. J. Exper. Cell. Physiol. Biochem. Pharmacol. 32(1), 64–73 (2013).
Han, N., Xu, H., Yu, N., Wu, Y. & Yu, L. MiR-203a-3p inhibits retinal angiogenesis and alleviates proliferative diabetic retinopathy in oxygen-induced retinopathy (OIR) rat model via targeting VEGFA and HIF-1α. Clin. Exper. Pharmacol. Physiol. 47(1), 85–94 (2019).
Faccini, J. et al. Circulating miR-155, miR-145 and let-7c as diagnostic biomarkers of the coronary artery disease. Sci. Rep. 7, 42916 (2017).
Zhu, G. F. et al. microRNA-155 is inversely associated with severity of coronary stenotic lesions calculated by the Gensini score. Coronary Artery Dis. 25(4), 304–310 (2014).
Leistner, D. M. et al. Transcoronary gradients of vascular miRNAs and coronary atherosclerotic plaque characteristics. Eur. Heart J. 37(22), 1738–1749 (2016).
Yang, D., Wang, J., Xiao, M., Zhou, T. & Shi, X. Role of Mir-155 in controlling HIF-1α level and promoting endothelial cell maturation. Sci. Rep. 6, 35316 (2016).
Sun, H. X. et al. Essential role of microRNA-155 in regulating endothelium-dependent vasorelaxation by targeting endothelial nitric oxide synthase. Hypertension 60(6), 1407–14 (2012).
Roitbak, T., Bragina, O., Padilla, J. L. & Pickett, G. G. The role of microRNAs in neural stem cell-supported endothelial morphogenesis. Vasc. Cell. 3, 25 (2011).
Caballero-Garrido, E. et al. In vivo inhibition of miR-155 promotes recovery after experimental mouse stroke. J. Neurosci. Off. J. Soc. Neurosci. 35(36), 12446–12464 (2015).
Pankratz, F. et al. MicroRNA-155 exerts cell-specific antiangiogenic but proarteriogenic effects during adaptive neovascularization. Circulation 131(18), 1575–1589 (2015).
Zhang, B. et al. MiR-125b inhibits cardiomyocyte apoptosis by targeting BAK1 in heart failure. Mol. Med. 27(1), 72 (2021).
Ding, X.-Q. et al. Interaction between microRNA expression and classical risk factors in the risk of coronary heart disease. Sci. Rep. 5(1), 14925 (2015).
Chen, C.-Y. et al. Cardiac-specific microRNA-125b deficiency induces perinatal death and cardiac hypertrophy. Sci. Rep. 11(1), 2377 (2021).
Szabó, M. et al. Hypercholesterolemia interferes with induction of miR-125b-1-3p in preconditioned hearts. Int. J. Mol. Sci. 21, 3744 (2020).
Nagpal, V. et al. MiR-125b is critical for fibroblast-to-myofibroblast transition and cardiac fibrosis. Circulation 133(3), 291–301 (2015).
Vickers, K. C. et al. MicroRNA-27b is a regulatory hub in lipid metabolism and is altered in dyslipidemia. Hepatology. 57(2), 533–542 (2013).
Rong, X. et al. miR-27b suppresses endothelial cell proliferation and migration by targeting Smad7 in Kawasaki disease. Cell. Physiol. Biochem. 48(4), 1804–1814 (2018).
Wang, J. et al. Cardiomyocyte overexpression of miR-27b induces cardiac hypertrophy and dysfunction in mice. Cell Res. 22(3), 516–527 (2012).
Li, G. et al. MicroRNA-27b-3p down-regulates FGF1 and aggravates pathological cardiac remodelling. Cardiovasc. Res. 118(9), 2139–2151 (2021).
Wang, Y., Chen, S., Gao, Y. & Zhang, S. Serum MicroRNA-27b as a screening biomarker for left ventricular hypertrophy. Texas Heart Inst. J. 44(6), 385–389 (2017).
Rincón, L. M. et al. Serum microRNAs are key predictors of long-term heart failure and cardiovascular death after myocardial infarction. ESC Heart Fail. https://doi.org/10.1002/ehf2.13919 (2022).
Lavoie, A. J. et al. Plaque progression in coronary arteries with minimal luminal obstruction in intravascular ultrasound atherosclerosis trials. Am. J. Cardiol. 105(12), 1679–1683 (2010).
Wu, W. et al. The role of angiogenesis in coronary artery disease: A double-edged sword: Intraplaque angiogenesis in physiopathology and therapeutic angiogenesis for treatment. Curr. Pharm. Des. 24(4), 451–464 (2018).
Funding
This study was funded by clinical research development unit, Shohada hospital, Tabriz University of Medical Sciences (Grant No.: 62308).
Author information
Authors and Affiliations
Contributions
Z.S. and Z.N.S.F. designed the study. Z.S. and Y.M. contributed to sample preparation. Z.N.S.F., A.D. and S.Z.V. carried out the experiment. S.N. and L.N.S.F. processed the experimental data and performed the analysis. Z.S. and Y.M. aided in interpreting the results. Z.S. and Y.M. wrote the manuscript with support from A.D. and S.Z.V., L.N.S.F. and Z.N.S.F. revised the first draft. All authors discussed the results and commented on the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saadatian, Z., Mansoori, Y., Nariman-Saleh-Fam, L. et al. Peripheral blood mononuclear cells expression of miR-200c, miR-125b, miR-27b, miR-203, and miR-155 in patients with significant or insignificant coronary artery stenosis. Sci Rep 13, 18438 (2023). https://doi.org/10.1038/s41598-023-45146-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45146-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.