Abstract
Whilst the presence of 2 subphenotypes among the heterogenous Acute Respiratory Distress Syndrome (ARDS) population is becoming clinically accepted, subphenotype-specific treatment efficacy has yet to be prospectively tested. We investigated anti-inflammatory treatment in different ARDS models in sheep, previously shown similarities to human ARDS subphenotypes, in a preclinical, randomized, blinded study. Thirty anesthetized sheep were studied up to 48 h and randomized into: (a) OA: oleic acid (n = 15) and (b) OA-LPS: oleic acid and subsequent lipopolysaccharide (n = 15) to achieve a PaO2/FiO2 ratio of < 150 mmHg. Then, animals were randomly allocated to receive treatment with methylprednisolone or erythromycin or none. Assessed outcomes were oxygenation, pulmonary mechanics, hemodynamics and survival. All animals reached ARDS. Treatment with methylprednisolone, but not erythromycin, provided the highest therapeutic benefit in Ph2 animals, leading to a significant increase in PaO2/FiO2 ratio by reducing pulmonary edema, dead space ventilation and shunt fraction. Animals treated with methylprednisolone displayed a higher survival up to 48 h than all others. In animals treated with erythromycin, there was no treatment benefit regarding assessed physiological parameters and survival in both phenotypes. Treatment with methylprednisolone improves oxygenation and survival, more so in ovine phenotype 2 which resembles the human hyperinflammatory subphenotype.
Similar content being viewed by others
Introduction
Acute Respiratory Distress Syndrome (ARDS) is a life-threatening syndrome caused by a large variety of etiologies1. Although a large body of data has characterized critical features of such syndrome2,3, its broad etiological heterogeneity and variable host-responses have impeded large improvements in patient mortality4 and morbidity rates5.
Based on the presumed predominant inflammatory pathogenesis in ARDS, treatment with corticosteroids in ARDS has been studied extensively in the past decades6, but corticosteroids are currently not recommended due to the conflicting results7,8. It has been suggested that potential beneficial effects of corticosteroids may have been offset due to its application in highly heterogenous populations. Indeed, post-hoc analyses of clinical studies revealed evidence for distinct ARDS subpenotypes: a hypoinflammatory and a hyperinflammatory subphenotype9,10,11,12,13. Briefly, the latter is characterized by a more severe inflammatory state, causing hemodynamic derangement and non-pulmonary organ failure, as well as higher mortality9,10,11,12,13. Importantly, retrospective post-hoc analyses of randomized clinical trials provided insightful suggestions on the risk of negative results when potentially beneficial treatments are applied to populations with mixed ARDS subphenotypes9,11,12,14. These retrospective findings have not been corroborated yet in prospective subphenotype-specific populations, due to the difficulties in accurately define these populations.
In this context, large animal models of ARDS subphenotypes could further elucidate benefits and harms of proposed interventions15 and inform the design of future innovative clinical studies. We previously assessed models of lung injury in sheep, and demonstrated that the double-hit ARDS model (oleic acid and lipopolysaccharides (OA-LPS)) mimics key features as observed in the human hyperinflammatory subphenotype16. Additionally, a recent report17 demonstrated comparable gene expression in tracheal aspirate among LPS animal models and human hyperinflammatory subphenotype. OA alone was chosen as the opposite ARDS lung injury model with the least systemic inflammation activation as compared to OA-LPS16.
We hypothesized that a correct selection of injury model may result in early clinical improvement in ovine ARDS. Thus, we investigated the effects of corticosteroids and macrolides on oxygenation (1° outcome) and lung edema, pulmonary mechanics, hemodynamic parameters and survival (2° outcome) in aforementioned sheep models of ARDS phenotypes.
Methods
Animal studies were conducted at the Queensland University of Technology (QUT) Medical Engineering Facility (MERF) in Brisbane. Animal ethics was approved by QUT Office of Research Ethics and Integrity (No 18-606). All experiments were performed in accordance with the Australian Code of Practice for the Care and Use of Animals for Scientific Purposes and the Animal care and Protection Act 2001 (QLD) and complied with the ARRIVE Guidelines.
Study design
This was a single-blinded, randomized, controlled preclinical trial in an ovine model (Fig. 1A). A total of 30 animals were randomized and allocated to the two injury methods: oleic acid (OA, n = 15) or oleic acid and lipopolysaccharides (OA-LPS, n = 15). For each injury model, subjects were further randomized to receive treatment either with methylprednisolone (pred: OA-LPS-pred, OA-pred; each 5 per group) or erythromycin (ery: OA-LPS-ery, OA-ery; each 5 per group) or they were randomized to the control group (ctr: OA-LPS-ctr and OA-ctr; each 5 per group). A pilot study consisting of 12 animals was conducted to confirm safety, adherence to protocol and efficacy assumptions in relation to treatment (Fig. 1A): animals were randomized to either pred or ctr per each phenotype, resulting in 3 animals per group. Randomization was performed using a random number generator.
Animal preparation
All sheep were approved for use by the facility veterinarian after a comprehensive health check and full blood count. Prior to experimentation, all animals were fasted overnight with free access to drinking water. A four-lumen central venous catheter (CVL; Arrow Int., Reading, USA) and a venous sheath (Edwards Lifesciences, Irvine, USA) were inserted in the jugular veins via Seldinger technique and sutured in place. Cefazolin 1 g intravenously (IV) was administered for antibiotic prophylaxis. For induction of anesthesia, midazolam (0.5 mg/kg) and propofol (3–4 mg/kg) were administered IV. A cuffed endotracheal tube size 9.0 internal diameter (Mallinckrodt, USA) was inserted into the airway, and mechanical ventilation (Galileo 5, Hamilton Medical, Switzerland) was commenced after placing the animal on the operative table in supine position. Initial ventilation settings consisted of tidal volumes of 8 ml/kg, a PEEP of 5 cmH20, a respiratory rate of 12–16 breaths/min and an FiO2 of 30–50%; settings were adapted to maintain an arterial saturation of > 94% and normocapnia, defined by an end-tidal carbon dioxide (EtCO2) of 35–45 mmHg. General anesthesia was maintained and titrated to an appropriate level with continuous infusion of midazolam 0.5–0.8 mg/kg/h, fentanyl 5–20 µg/kg/h and ketamine 2.5–7.5 mg/kg/h. Basic monitoring consisted of a pulse oximeter probe attached to the tongue, a 5-lead electrocardiogram and continuous waveform capnography. A PiCCO catheter (PULSION Medical Systems, Getinge, Gothenburg, Sweden) was inserted into the femoral artery for advanced hemodynamic monitoring. A pulmonary artery catheter (Swan-Ganz CCOmbo, Edwards Lifescience, Irvine, USA) was inserted via the internal jugular sheath to monitor pulmonary artery pressure, mixed-venous saturation and core body temperature. In addition, a 14F nasogastric tube was placed and left on free drainage, and a 12F urinary catheter was inserted with closed collection. To facilitate access to the airways for bronchoscopy and decrease dead space ventilation, a surgical tracheotomy with insertion of a cuffed endotracheal tube (Size 9–10, Portex) was performed. During instrumentation, a crystalloid bolus (Hartmanns) of 250 ml was delivered to compensate for overnight fasting, then the fluids infusion rate was maintained at 1 ml/kg/h and modified as according to the hemodynamic condition. After instrumentation, the animal was positioned in prone position and rested for one hour prior to commencement of induction of ARDS (Fig. 1B).
Induction of ARDS injury models
Using the official ARDS definition for experimental models18,19, animals randomized to OA received sequential IV administration of oleic acid (0.89 g/ml; Sigma-Aldrich, Australia) in subsequent 0.03 ml/kg doses to ultimately achieve a PaO2/FiO2 < 150, as assessed via arterial blood gases test 15 min after OA infusion20. OA-LPS group received administration of OA, then after fulfilling ARDS criteria, 0.5 µg/kg of lipopolysaccharide (LPS: E. coli O55:B5, Sigma-Aldrich, Australia), dissolved in 50 ml of normal saline, was infused over 1 h.
Anti-inflammatory treatment and blinding
Animals randomized to treatment with methylprednisolone received a bolus of 100 mg IV at confirmation of ARDS diagnosis (T0) and a continuous infusion of 2 mg/kg/24 h over the course of the study (Fig. 1B). Animals randomized to treatment with erythromycin received a bolus of 100 mg IV every 6 h, starting at T0. Investigators involved in the clinical management of the study subjects were blinded to treatment allocation: all animals received two 10 ml boluses at T0 (one containing methylprednisolone 100 mg or normal saline (NS), and another containing erythromycin 100 mg or NS), followed by a continuous infusion of 2 ml/h (containing methylprednisolone 2 mg/kg/24 h or NS) and a 10 ml bolus every 6 h (containing erythromycin 100 mg or NS).
Intra-experimental monitoring and management
Arterial blood gas analysis was performed every 2 h and whenever clinically indicated to assess blood gases, glucose and electrolytes. Mixed-venous blood gas analysis and transpulmonary thermodilution using Pulse Contour Cardiac Output (PiCCO) technology was performed every 2 h (Fig. 1B). Intra-experimental monitoring and data recording are described in the Supplemental Methods.
To minimize potential confounders, strict protocols for hemodynamic management (Supplemental Fig. S1), ventilation strategy (Supplemental Fig. S2) and procedures were applied.
Animals were euthanized with 163 mg/kg of pentobarbital and organs were retrieved for tissue harvesting at the end of the study, 48 h after development of ARDS, or when animals reached the following criteria: (a) mean arterial blood pressure (MAP) persistently below 40 mmHg despite optimized support; and (b) arterial pH below 7.0 because of respiratory, metabolic or mixed acidosis and exhausted compensation strategies.
Primary and secondary outcomes
The primary outcome was oxygenation (PaO2/FiO2 ratio (PF ratio) and Oxygenation Index (OI)) throughout the 48 h assessment period among injury types and their respective treatment. As secondary outcomes, we investigated the effects of study treatment on lung edema (extravascular lung water index (EVLWI)), hemodynamic parameters, pulmonary mechanics, and survival in the respective lung injury.
Sample collection and processing
Blood samples for full blood count (Mindray Hematology analyzer BC 5000, China) and biochemistry (IDEXX laboratories Brisbane, Australia) were collected at baseline and every 12 h following T0. Postmortem collected lung tissue samples were prepared for histopathology. Quantification of pulmonary edema was determined by measuring the wet-to-dry-weight of post-mortem left and right upper and lower lung lobe: a tissue sample of 2 cm diameter and 2 cm thickness was excised and lung weight measured immediately. Dry weight was determined by placing the lung tissue in an oven at 65 °C for several days, weighing the tissue every day until the weight stopped decreasing. The wet-to-dry weight ratio was calculated by dividing the wet by the dry weight.
Inflammatory cytokines and histopathology
Arterial blood samples were collected in EDTA blood tubes, processed to plasma and stored at − 80 °C until analysis. Plasma concentration of inflammatory cytokines (e.g. interleukin (IL) -6, -8, -10, -1β) in serum were quantified by in-house ELISA’s21.
At study end, lung tissues were taken for histological assessment (Suppl. methods). Slides were examined by blinded, qualified veterinary pathologist. The lung injury score (LIS) was assessed as recommended by the ATS for experimental ARDS in animal models18,19: it scores neutrophils in the alveolar space (A) and in the interstitial space (B), hyaline membranes (C), proteinaceous debris filling the airspace (D) and alveolar septal thickening (E). Every item is given a score between 0 to 2, then the LIS is calculated by: ((20 × A) + (14 × B) + (7 × C) + (7 × D) + (2 × E))/number of fields × 100. This results in a score between 0 (no injury) and 1 (severe lung injury).
Twenty random high-power fields (400 × total magnification) were scored per section and the LIS was calculated per animal (mean ± SD). For the scoring, at least 50% of each field had to be filled by lung alveoli: fields consisting predominantly of the lumen of large airways or vessels were rejected. Septal thickness was not evaluated in alveolar septa directly adjacent to a blood vessel or airway (normally thickened by the collagen present in the peribroncho-vascular bundle). In addition, the following parameters were evaluated: (a) percentage of section effaced by necrosis (score/field: 0 = none or less than 10%; 1 = 10–50%; 2 = > 50%) and (b) number of thrombi within blood vessels (score/field: 0 = none; 1 = 1 thrombus; 2 = > 1 thrombus). Bacterial colonies as observed in necrotic areas or admixed with the neutrophilic aggregates and alveolar hemorrhage were marked as present or not within one animal and reported as percentage per injury type and the respective treatment group.
Statistical analysis
For the power calculation, an F-test for correction to 6 treatment groups was applied (power set at 80%, level of α at 5%, 2-tailed), assuming a treatment effect in terms of an improvement in PaO2/FiO2 ratio of 80 mmHg and a standard deviation (SD) of 40 mmHg22 over the course of the study. Conservatively assuming a Cohens d of 1.0 (medium effect size), this resulted in a total sample size of 28 animals, therefore 5 animals per group.
Categorical variables are reported as numbers and percentages, continuous data as mean ± SD or median and interquartile range (IQR), for normally or not-normally distributed parameters, respectively. Comparisons between groups were made using Kruskal–Wallis or Mann–Whitney U test and x2 test as appropriate.
Linear-mixed effects models (LMM)23 were constructed to assess the impact of parameters of oxygenation, hemodynamics, metabolic situation and respiratory mechanics over time among injury types and their treatment. Distribution of data was assessed with QQ and residual plots. Control animals were defined as the reference level, time was specified as a continuous fixed effect and the interaction between treatment and time was included. A random effect was defined for each individual to account for within-subject correlation from repeated measurements over time. Fixed effects were reported as estimates with 95% confidence intervals (CI) and p-values were estimated using Sattherwaite’s method.
The pairwise comparison of injury types (2 groups) over time was performed using averaging over time and injury type, the Kenward-Roger method was applied for the degrees of freedom.
A shared parameter joint model24 for assessment of longitudinal and time-to-event data (death) and the associated treatment effect was estimated under a Bayesian framework. The model uses observed longitudinal measurement (trajectories) to determine the posterior probability for event (death) and treatment effect for each of the assessed parameter. Data were reported as hazard ratio (HR) and 95% credible intervals.
All statistical analyses were performed with R Version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria). The minimal reproducible code for the LMM and Bayesian model is reported in the Supplemental Methods.
Results
Studied population
A total of 30 female non-pregnant Merino-Dorset crossbreed ewes, aged 1–3 years, mean weight 51 ± 5 kg, were included in the final analysis (Fig. 1A). Baseline characteristics of animals are shown in Supplemental Table S1.
All animals reached ARDS criteria within 2–3 h, median PF ratio at T0 was 138 (IQR 120–149). ARDS was achieved through a median dose of OA of 0.14 ml/kg (IQR 0.012–0.18 ml/kg) with no significant difference among the six groups.
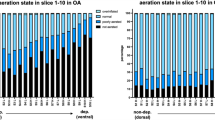
In terms of inflammatory reaction, OA-LPS groups showed higher levels of IL-6, IL-8, IL-10 and IFNy as compared to OA groups early after ARDS induction with a peak at 2 to 6 h (Fig. 2). However, there was no systematic difference over time among the treatment groups in both injury types.
Cytokine levels among all OA-LPS and OA animals in plasma. P values denotes interaction of treatment group over time from linear-mixed effect model. Abbreviations: ctr: control; ery: erythromycin; IFNy: interferon gamma; IL: interleukin; OA: Oleic Acid; OA-LPS: Oleic Acid and lipopolysaccharides; pred: methylprednisolone.
Primary outcome
Treatment with methylprednisolone resulted in a higher PF ratio and a significantly lower OI, while animals treated with erythromycin displayed worse oxygenation than control animals (p for interaction (IA) treatment:time < 0.05) (Fig. 3A; Table 1). Clustering between injury type and treatment confirmed a significantly improved PF ratio and OI among OA-LPS in animals treated with methylprednisolone (p for IA treatment:time < 0.001) and a worse oxygenation in animals treated with erythromycin as compared to controls (Fig. 3B; Table 1). Among OA, no significant difference between treatment groups over time were seen (p for IA ns) (Fig. 3C, Table 1). Analyzing OA and OA-LPS independently of treatment (ctr, pred and ery combined), PF ratio and OI did not differ between injury models (Supplemental Fig. S3 and Supplemental Table S2).
Oxygenation and pulmonary derangement among (A) treatment groups (injury types combined) (B) treatment among OA-LPS and (C) treatment among OA; displayed in mean over time of observation. Curve smoothened by using the LOESS method (locally estimated scatterplot smoothing), p-values for interaction of treatment group over time. Abbreviations: ctr: control; ery: erythromycin; OA: Oleic Acid; OA-LPS: Oleic Acid and lipopolysaccharides; pred: methylprednisolone; Qs/Qt: shunt.
Secondary outcomes
Animals treated with methylprednisolone displayed a lower shunt fraction, dead space ventilation (Vd/Vt) and plateau pressure (Pplat) (all p for IA pred:time < 0.05) than animals treated with erythromycin or controls which showed similar values over time (Fig. 3A, Table 1). The differences remained significant in OA-LPS treated with methylprednisolone for Vd/Vt, Pplat and additionally EVLWI (all p for IA pred:time < 0.05) while erythromycin was shown a trend towards worse values that did not reach statistical significance except for Pplat (Fig. 3B; Table 1). In OA, parameters were largely comparable among treatment groups and controls except for a significantly lower Pplat and shunt fraction in OA-pred (Fig. 3C, Table 1) There was no significant difference among injury model alone when assessed independently of treatment (ctr, pred and ery combined) (Supplemental Fig. S3, Supplemental Table S2).
Hemodynamic status
MAP, heart rate, SVRI, VDI and lactate clearance displayed better values in animals treated with methylprednisolone when compared to controls (p for IA pred:time < 0.05) while these parameters were shown worse values over time in animals treated with erythromycin as compared to controls (Fig. 4A, Table 1). In both, OA-LPS and OA, treatment with methylprednisolone resulted in a significantly lower VDI and a higher SVRI (p for IA pred:time < 0.05) as compared to controls, while only in OA, HR and lactate displayed statistically significant better values while treated with methylprednisolone as compared to controls (p for IA pred:time < 0.05) (Fig. 4, Table 1). Among injury types, independently of treatment, no difference was observed for all parameters displayed (Supplemental Fig. S3 and Supplemental Table S2).
Hemodynamic parameters among (A) treatment groups (injury types combined), (B) treatment among OA-LPS and (C) treatment among OA; displayed in mean over time of observation. Curve smoothened by using the LOESS method (locally estimated scatterplot smoothing), p-values for interaction of treatment group over time. Abbreviations: ctr: control; ery: erythromycin; OA: Oleic Acid; OA-LPS: Oleic Acid and lipopolysaccharides intravenously; pred: methylprednisolone.
Pulmonary mechanics, fluid balance and metabolic situation
A lower total fluid balance, a higher urinary output with an increased BE was seen in animals treated with methylprednisolone as compared to controls and erythromycin (Supplemental Fig. S5, Supplemental Table S4). Treatment with methylprednisolone facilitated a lower minute ventilation (MV) at a higher compliance and resulted in lower PaCO2 values (Supplemental Fig. S6, Supplemental Table S3). No difference was observed among injury models independently of treatment groups (Supplemental Fig. S3 and Supplemental Table S2).
Results of full blood count and biochemistry are shown in Supplemental Fig. S7.
Wet-dry ratio and lung injury score
There was no systematic difference among injury models and their respective treatment groups in median wet-dry ratio of the lungs (Fig. 5).
All animals displayed severely damaged lungs in histology assessment. Among OA, the highest LIS was observed in animals treated with erythromycin and the necrosis score was highest among all treated animals (Fig. 5). Among OA-LPS, the LIS, necrosis and thrombosis score was comparable among treatment groups. A higher percentage of bacterial colonies was seen in OA-ctr and -pred as well as OA-LPS-ctr and -ery than in all other groups (Fig. 5).
Cumulative survival up to 48 h
Crude survival rates for every animal among treatment groups are shown in Supplemental Fig. S4. Animals treated with methylprednisolone were shown a survival benefit at 48 h (log rank 0.02) (Supplemental Fig. S8A). Among OA-LPS but not OA, control animals displayed a significantly lower survival at 24 h than treated ones (log rank 0.024) (Supplemental Fig. S8B and C.
Deceased animals displayed no difference in the LIS but a trend towards higher necrosis score and more bacterial colonies in histology assessment of the lungs (Supplemental Fig. S9).
Predictors of survival and treatment effect
In the Bayesian model, the strongest predictors of survival were compliance, MAP, BE and PF ratio, in ctr vs ery as well as in ctr vs pred in OA-LPS and OA. The strongest predictor for death was lactate, Vd/Vt, mPAP, ventilatory ratio and Pdriv (Supplemental Fig. S10A). Analyzing the treatment effect showed that while pred improved most parameters in comparison with ctr, comparison between ctr and ery did not confirm any benefit associated with the use of erythromycin, specifically in OA animals (Supplemental Fig. S10B, Supplemental Table S4).
Discussion
This is an evaluation of anti-inflammatory treatment in two different ovine ARDS injury models—OA-LPS, mimicking features of human hyperinflammatory ARDS, and OA alone, as the opposite model—aimed to improve the early course of the disease. We have shown that only in hyperinflammatory ovine ARDS (OA-LPS), treatment with low-dose corticosteroids improved oxygenation significantly as compared to erythromycin and controls. In addition, all animals treated with methylprednisolone, independently of the lung injury type, had a survival benefit up to 48 h, while erythromycin was associated with increased mortality.
Strengths of this study include two different lung injury models with a different inflammatory response but similar clinical presentation, a randomized controlled study design comparing the treatment effect to placebo using an adequate sample size, allocation concealment and blinding. Additionally, an observation period up to 48 h in an ICU setting with rigorous continuous monitoring and the assessment of a variety of clinical parameters (pulmonary mechanics, lung edema, hemodynamics, metabolic situation, fluid balance) are to name.
First and foremost, an early and consistent improvement in oxygenation, as reflected by PF ratio and OI was only shown in the OA-LPS-pred group. A possible pathophysiological explanation for this result is the significantly lower amount of pulmonary edema (as quantified by EVLWI) and dead space ventilation early on after starting treatment. As there was no significant difference in the amount of pulmonary edema (EVLWI and wet-dry ratio) at study end, subsidence of the methylprednisolone effect over time or an additional injury like ventilation-induced damage might be held accountable. Additionally, lower plateau pressures, higher compliance and lower PaCO2 were displayed in both injury types treated with methylprednisolone, indicating less pulmonary derangement. These observations are likely related to the specific anti-inflammatory effects of methylprednisolone: amongst corticosteroids as the most potent anti-inflammatory substances, methylprednisolone was chosen for its larger volume of distribution and longer mean residence time, as well as a greater retention in the epithelial lining fluid of the alveoli25.
Mechanistically, the pleiotropic effects of corticosteroids are driven by the activation of the glucocorticoid-receptor (GCR) that enables multiple signaling pathways and affects genomic and non-genomic mechanisms26. In particular, the proinflammatory pathway via nuclear factor-κB (NF-κB) plays a crucial role in the dysregulation of systemic and pulmonary inflammation in ARDS27,28. The GCR inhibits the NF-κB signal pathway26 and activator protein-1, inhibiting NF-κB dependent proinflammatory gene expression and the transcription of proinflammatory cytokines29. Since LPS but not OA, is known to activate NF-κB30,31, part of the beneficial effects of methylprednisolone in our OA-LPS ARDS model might be explained by the inhibition of the NF-κB signalling pathway through the GCR. However, given that corticosteroids interact with the inflammatory cascade on several levels, this mechanism does not explain all observed improvements. In septic shock, corticosteroids reduce levels of pro-inflammatory cytokines IL-6 and -832. In ARDS associated with septic shock, IL-6 decreases over time in treated patients with relative adrenal insufficiency33. In our study, we observed the highest plasma IL-6 levels in OA-LPS animals, with levels already decreasing six hours into the study in OA-LPS-pred and OA-LPS-ery, potentially indicating a higher anti-inflammatory effect. There was however no systematic difference in cytokine levels among treatment groups over the whole observation time. Possible explanations are that the treatment benefit regarding oxygenation and hemodynamics is not captured by an effect of pred on cytokine levels or that the granularity of data points with cytokine measurements every 6 h is not matching.
Methylprednisolone was associated with improved hemodynamic stability in comparison with controls or erythromycin. This persisted in OA-LPS-pred and OA-pred, which were both characterized by higher blood pressure and systemic vascular resistance, as well as a lower heart rate and vasoactive need than all other groups. Paired with a lower total fluid balance and a higher base excess in OA-LPS-/OA-pred animals, this indicates a more stable metabolic milieu. The positive effect of methylprednisolone on the hemodynamic parameters could be due to a reversion of a relative or complete adrenal insufficiency in OA-LPS and OA. An indicator for this mechanism is the higher urinary output in OA-LPS-pred and OA-pred, as glucocorticoids suppress the secretion of vasopressin via the neuroendocrinological hypothalamic-pituitary axis34. Considering the known effect of corticosteroids on hemodynamic parameters in septic shock32, our findings are in line with previous ones.
It is highly likely that the improved hemodynamic and metabolic stability contributed to the improved survival with methylprednisolone throughout the 48 h assessment period in OA-LPS-pred and OA-pred. In the Bayesian model, major differences were observed in treatment effects: comparing controls and methylprednisolone, treatment was shown beneficial for most parameters (in OA-LPS and OA equally), whereas in the comparison of controls and erythromycin, the treatment effect was negative for survival in most parameters, even more so in OA-LPS animals. Yet, our study was likely underpowered to identify any difference in survival between OA and OA-LPS during corticosteroid treatment.
Erythromycin was tested as a second treatment option as it has proven beneficial in chronic inflammatory lung diseases such as chronic obstructive pulmonary disease and bronchiectasis35,36 as well as ARDS37,38,39 because of its immunomodulatory effects. Macrolides exhibit multifactorial anti-inflammatory mechanisms by inhibiting chemotaxis, infiltration and activation of neutrophils as well as the production of inflammatory cytokines. In our study, treatment with erythromycin did not provide benefits in any study groups but was associated with a higher risk of death as compared to controls. There are several possible explanations for these results. First, the applied dose, while consistent with previous studies39,40, might have been insufficient in the settings of our OA model characterized by life-threating pulmonary inflammation. Second, the 48 h assessment period may have been too short to detect erythromycin-related immunomodulatory effects. Finally, characterization of ARDS subgroups is highly complex and likely not only confined to the inflammatory status, in this context macrolides might have not influenced critical biological pathways. As our understanding of the pathophysiological pathways leading to human hypo- and hyperinflammatory subphenotypes is still imperfect, the likely complex intertwining of general and subphenotypic specific effects cannot be untangled.
Histology overall assessment did not explain the positive treatment response in terms of oxygenation as all animals displayed severe lung injury (LIS) without a systematic difference among type of lung injury or applied treatment. Set in relation with mortality, surviving animals were shown a trend towards lower necrosis score and fewer bacterial colonies in the lung. This remained true for the OA-LPS-pred but not the OA-pred, the two groups with the highest survival rate up to 48 h.
Crucial questions in human ARDS subphenotyping remain to be answered before the translatability of animal models can be fully understood: (A) Is inflammation activation the true differentiating factor among ARDS subphenotypes or is it another yet undiscovered underlying biological process? The answer will determine which treatable traits are the most promising as potential treatment targets. (B) Is the host-response, as measured by clinical parameters and biomarkers in circulation, truly reflecting the biological process in the lung compartment41 and in ARDS? Or is it rather an expression of disease severity than specific pathophysiological processes in ARDS, therefore potentially also transmittable to other critical care diseases42,43? The immunological processes happening in ARDS might be confined to the lungs, therefore true subphenotypes and possibly ARDS endotypes might only be identified by studying the local compartment.
The present study has several limitations to be addressed: First, the observation period was limited to 48 h, therefore we cannot predict the further course of the assessed parameters. Some clinical and laboratory markers displayed a clear trend and may be even more accentuated in a longer observation period. Second, the limited availability of species-specific research reagents restricts the measurement of several biomarkers as described in the human ARDS population. Third, due to a limited sample size per group, the results regarding survival benefits are likely underpowered. Fourth, blood cultures or other microbiological sampling were not performed, hence we do not know if these animals developed infections, potentially as a side effect of corticosteroids, that might have impacted the inflammatory status or treatment effect.
Due to its pathophysiological complexities, animal models have been crucial to ARDS research: key concepts in ARDS44 were originally discovered in large animal models before successful application in human2. As preclinical models can not fully reproduce human ARDS in all its complexity, by narrowing the complexity of the disease to more homogenous subgroups, the chances of identification of treatable traits increase45. Likely this is the gap where translational models could be valuable: to reproduce a specific treatable trait and test targeted treatment. Our ovine model offers opportunities to investigate OA-LPS, which resembles in many features the human hyperinflammatory subphenotype16 as similar pathways of inflammation are activated15,17. A comparison of omics data among preclinical models and human ARDS subphenotypes could inform about the true extent of comparability.
Conclusion
Early and persistent improvement in oxygenation was seen only in hyperinflammatory ovine ARDS treated with methylprednisolone, while hemodynamic situation and survival was improved in both injury models and corticosteroid treatment. Erythromycin did not offer any benefit regarding all assessed outcomes.
Data availability
The dataset generated and analysed during the current study are not publicly available due to being part of a PhD project but are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute Respiratory Distress Syndrome
- ATS:
-
American Thoracic Society
- BAL:
-
Bronchoalveolar lavage
- BE:
-
Base excess
- CI:
-
Confidence interval
- CVL:
-
Central venous line
- ELISA:
-
Enzyme-linked immunoassay
- EtCO2 :
-
End-tidal carbon dioxide
- EVLWI:
-
Extravascular lung water index
- FiO2 :
-
Inspired oxygen fraction
- GCR:
-
Glucocorticoid receptor
- GEDI:
-
Global end-diastolic index
- HR:
-
Heart rate
- IFNγ:
-
Interferon gamma
- IL:
-
Interleukin
- IQR:
-
Interquartile range
- IV:
-
Intravenously
- LIS:
-
Lung injury score
- LMM:
-
Linear-mixed effects models
- LPS:
-
Lipopolysaccharide
- MAP:
-
Mean arterial pressure
- mPAP:
-
Mean pulmonary artery pressure
- NS:
-
Normal saline
- OA:
-
Oleic acid
- OA-ctr:
-
Oleic acid control
- OA-pred:
-
Oleic acid treated with methylprednisolone
- OA-ery:
-
Oleic acid treated with erythromycin
- OA-LPS:
-
Oleic acid and LPS intravenously
- OA-LPS-ctr:
-
Oleic acid and LPS intravenously control
- OA-LPS-pred:
-
Oleic acid and LPS intravenously treated with methylprednisolone
- OA-LPS-ery:
-
Oleic acid and LPS intravenously treated with erythromycin
- OI:
-
Oxygenation index
- Pdriv:
-
Driving pressure
- PF ratio:
-
PaO2/FiO2 ratio
- PEEP:
-
Positive end-expiratory pressure
- Pplat:
-
Plateau pressure
- PiCCO:
-
Pulse contour cardiac output
- PPV:
-
Pulse pressure variation
- QUT:
-
Queensland University of Technology
- SD:
-
Standard deviation
- SpO2 :
-
Oxygen saturation
- SVV:
-
Stroke volume variation
- Vd/Vt:
-
Dead space ventilation
References
Ashbaugh, D. G., Bigelow, D. B., Petty, T. L. & Levine, B. E. Acute respiratory distress in adults. Lancet 2, 319–323 (1967).
Brower, R. G. et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 342, 1301–1308 (2000).
Brower, R. G. et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N. Engl. J. Med. 351, 327–336 (2004).
Bellani, G. et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. J. Am. Med. Assoc. 315, 788–800 (2016).
Herridge, M. S. et al. Functional disability 5 years after acute respiratory distress syndrome. N. Eng. J. Med. 364, 1293–1304 (2011).
Meduri, G. U. et al. Pharmacological principles guiding prolonged glucocorticoid treatment in ARDS. Int. Care Med. https://doi.org/10.1007/s00134-020-06289-8 (2020).
Villar, J. et al. Dexamethasone treatment for the acute respiratory distress syndrome: A multicentre, randomised controlled trial. Lancet Respir. Med. 8, 267–276 (2020).
Meduri, G. U., Siemieniuk, R. A. C., Ness, R. A. & Seyler, S. J. Prolonged low-dose methylprednisolone treatment is highly effective in reducing duration of mechanical ventilation and mortality in patients with ARDS. J. Intensive Care 6, 1–7 (2018).
Calfee, C. S. et al. Latent class analysis of ARDS subphenotypes: Analysis of data from two randomized controlled trials. Lancet Respir. Med. 2, 611–620 (2014).
Bos, L. D. et al. Identification and validation of distinct biological phenotypes in patients with acute respiratory distress syndrome by cluster analysis. Thorax 72, 876–883 (2017).
Famous, K. R. et al. Acute respiratory distress syndrome subphenotypes respond differently to randomized fluid management strategy. Am. J. Respir. Crit. Care Med. 195, 331–338 (2017).
Calfee, C. S. et al. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: Secondary analysis of a randomised controlled trial. Lancet Respir. Med. 0, 1–8 (2018).
Sinha, P. et al. Latent class analysis of ARDS subphenotypes: A secondary analysis of the statins for acutely injured lungs from sepsis (SAILS) study. Int. Care Med. 44, 1859–1869 (2018).
Sinha, P. et al. Latent class analysis reveals COVID-19-related acute respiratory distress syndrome subgroups with differential responses to corticosteroids. Am. J. Respir. Crit. Care Med. 204, 1274–1285 (2021).
Enkhbaatar, P. et al. Comparison of gene expression by sheep and human blood stimulated with the TLR4 agonists lipopolysaccharide and monophosphoryl lipid A. PLoS ONE 10, e0144345 (2015).
Millar, J. E. et al. Characterizing preclinical sub-phenotypic models of acute respiratory distress syndrome: An experimental ovine study. Physiol. Rep. https://doi.org/10.14814/phy2.15048 (2021).
Sarma, A. et al. Hyperinflammatory ARDS is characterized by interferon-stimulated gene expression, T-cell activation, and an altered metatranscriptome in tracheal aspirates. Prepr. medRxiv https://doi.org/10.1101/2022.03.31.22272425 (2022).
Matute-Bello, G. et al. An official American Thoracic Society Workshop Report: Features and measurements of experimental acute lung injury in animals. Am. J. Resp. Cell. Mol. Biol. 44, 725–738 (2011).
Kulkarni, H. S. et al. Update on the features and measurements of experimental acute lung injury in animals: An official American Thoracic Society workshop report. Am. J. Respir. Cell Mol. Biol. 66, e1–e14 (2022).
Luecke, T. et al. Oleic acid vs saline solution lung lavage-induced acute lung injury. Chest 130, 392–401 (2006).
Bouquet, M. et al. Development and validation of ELISAs for the quantitation of interleukin (IL)-1β, IL-6, IL-8 and IL-10 in ovine plasma. J. Immunol. Methods 486, 112835 (2020).
Asmussen, S. et al. Human mesenchymal stem cells reduce the severity of acute lung injury in a sheep model of bacterial pneumonia. Thorax 69, 819–825 (2014).
Casals, M., Girabent-Farrés, M. & Carrasco, J. L. Methodological quality and reporting of generalized linear mixed models in clinical medicine (2000–2012): A systematic review. PLoS ONE 9, 1–10 (2014).
McGlothlin, A. E. & Viele, K. Bayesian hierarchical models. J. Am. Med. Assoc. 320, 2365–2366 (2018).
Greos, L. S. et al. Methylprednisolone achieves greater concentrations in the lung than prednisolone: A pharmacokinetic analysis. Am. Rev. Respir. Dis. 144, 586–592 (1991).
Rhen, T. & Cidlowski, J. A. Antiinflammatory action of glucocorticoids—new mechanisms for old drugs. N. Engl. J. Med. 353, 1711–1723 (2005).
Meduri, G. U., Muthiah, M. P., Carratù, P., Eltorky, M. & Chrousos, G. P. Nuclear factor-ĸB- and glucocorticoid receptor α-mediated mechanisms in the regulation of systemic and pulmonary inflammation during sepsis and acute respiratory distress syndrome. Neuroimmunomodulation 12, 321–338 (2005).
Umberto Meduri, G., Tolley, E. A., Chrousos, G. P. & Stentz, F. Prolonged methylprednisolone treatment suppresses systemic inflammation in patients with unresolving acute respiratory distress syndrome: Evidence for inadequate endogenous glucocorticoid secretion and inflammation-induced immune cell resistance to glucocorticoids. Am. J. Respir. Crit. Care Med. 165, 983–991 (2002).
Jantz, M. A. & Sahn, S. A. Corticosteroids in acute respiratory failure. Am. J. Respir. Crit. Care Med. 160, 1079–1100 (1999).
Chen, H., Bai, C. & Wang, X. The value of the lipopolysaccharide-induced acute lung injury model in respiratory medicine. Expert Rev. Respir. Med. 4, 773–783 (2010).
Moine, P. et al. NF-κB regulatory mechanisms in alveolar macrophages from patients with acute respiratory distress syndrome. Shock 13, 85–91 (2000).
Keh, D. et al. Immunologic and hemodynamic effects of ‘low-dose’ hydrocortisone in septic shock: A double-blind, randomized, placebo-controlled, crossover study. Am. J. Respir. Crit. Care Med. 167, 512–520 (2003).
Annane, D., Sébille, V. & Bellissant, E. Effect of low doses of corticosteroids in septic shock patients with or without early acute respiratory distress syndrome. Crit. Care Med. 34, 22–30 (2006).
Erkut, Z. A., Pool, C. & Swaab, D. F. Glucocorticoids suppress corticotropin-releasing hormone and vasopressin expression in human hypothalamic neurons 1. J. Clin. Endocrinol. Metab. 83, 2066–2073 (1998).
Kadota, J. et al. Long-term efficacy and safety of clarithromycin treatment in patients with diffuse panbronchiolitis. Respir. Med. 97, 844–850 (2003).
Equi, A., Balfour-Lynn, I. M., Bush, A. & Rosenthal, M. Long term azithromycin in children with cystic fibrosis: A randomised, placebo-controlled crossover trial. Lancet 360, 978–984 (2002).
Walkey, A. J. & Wiener, R. S. Macrolide antibiotics and survival in patients with acute lung injury. Chest 141, 1153–1159 (2012).
Tamaoki, J. et al. Effect of erythromycin on endotoxin-induced microvascular leakage in the rat trachea and lungs. Am. J. Respir. Crit. Care Med. 151, 1582–1588 (1995).
Simonis, F. D. et al. Macrolide therapy is associated with reduced mortality in acute respiratory distress syndrome (ARDS) patients. Ann. Transl. Med. 6, 24–31 (2018).
Tamaoki, J., Kadota, J. & Takizawa, H. Clinical implications of the immunomodulatory effects of macrolides. Am. J. Med. Suppl. 117, 5–11 (2004).
Conway Morris, A., Rynne, J. & Shankar-Hari, M. Compartmentalisation of immune responses in critical illness: Does it matter?. Intensive Care Med. https://doi.org/10.1007/s00134-022-06871-2 (2022).
Reddy, K. et al. Subphenotypes in critical care: Translation into clinical practice. Lancet Resp. Med. 8, 631–643 (2020).
Neyton, L. P. A. et al. Molecular patterns in acute pancreatitis reflect generalizable endotypes of the host response to systemic injury in humans. Ann. Surg. 275(2), e453–e462 (2020).
Tsuno, K., Prato, P. & Kolobow, T. Acute lung injury from mechanical ventilation at moderately high airway pressures. J. Appl. Physiol. 69, 956–961 (1990).
Bos, L. D. J. et al. Towards a biological definition of ARDS: Are treatable traits the solution?. Intensive Care Med. Exp. https://doi.org/10.1186/s40635-022-00435-w (2022).
Acknowledgements
We thank Prof. Adrian Barnett for expert statistical advice. Additionally, we would like to thank Prof. Balasubramian Venkatesh and Prof. Carolyn Calfee for critical review of the manuscript. Karin Wildi, John Fraser, Jacky Suen and Gianluigi Li Bassi take full responsibility for the content of the manuscript, including the data and analysis.
Author information
Authors and Affiliations
Contributions
Conception and design of work: K.W., G.L.B., J.S., J.F. Acquisition of data: K.W., S.L., C.A., S.M.C., S.H., N.S., K.S., M.B., E.W., G.A., M.P., K.H., K.L., X.W., C.P., L.S.H., J.S.J., K.K.; C.M., G.L.B., J.S., J.F. Analysis and interpretation of data: K.W., C.P., G.L.B., J.S., J.F. Drafting the work or revising it critically for important intellectual content: K.W., S.L., C.A., S.M.C., S.H., N.S., K.S., M.B., E.W., G.A., M.P., K.H., K.L., X.W., C.P., L.S.H., J.S.J., K.K., C.M., J.L., PP, G.L.B., J.S., J.F. Final approval of the version submitted for publication: K.W., S.L., C.A., S.M.C., S.H., N.S., K.S., M.B., E.W., G.A., M.P., K.H., K.L., X.W., C.P., L.S.H., J.S.J., K.K., C.M., PP, G.L.B., J.L., J.S., J.F. Agreement to be accountable for all aspects of the submitted work: K.W., S.L., C.A., S.M.C., S.H., N.S., K.S., M.B., E.W., G.A., M.P., K.H., K.L., X.W., C.P., L.S.H., J.S.J., K.K., C.M., J.L., PP, G.L.B., J.S., J.F. K.W., J.S. and J.F. take full responsibility for the content of the manuscript, including the data and analysis.
Corresponding author
Ethics declarations
Competing interests
This study was funded by the Wesley Medical Research Foundation (2020CR25) and an innovation grant by the Prince Charles Hospital Foundation (INN2018-101) (all KW). The funders had no role in the design of the study, data collection, analysis and interpretation as well as in writing the manuscript.
Dr. Karin Wildi has received research funding from the Gottfried and Julia Bangerter-Rhyner Foundation, the University of Basel, the Wesley Medical Research Foundation and the Prince Charles Hospital Foundation. In addition, she received a PhD scholarship from the University of Queensland (UQ). Samantha Livingstone received a PhD scholarship from the Prince Charles Hospital Foundation. Keibun Liu received a research grant from Senko Medical Instrument Mfg. Co., Ltd and the Prince Charles Hospital Foundation. Silver Heinsar and Kei Sato received a PhD scholarship from the University of Queensland. Christian Mueller received research support from the Swiss National Science Foundation, the Swiss Heart Foundation, the KTI, the University Hospital Basel, the University of Basel, Abbott, Beckman Coulter, Idorsia, Novartis, Ortho Clinical Diagnostics, Quidel, Roche, Siemens, as well as speaker honoraria/consulting honoraria from Amgen, Astra Zeneca, Bayer, Boehringer Ingelheim, BMS, Daiichi Sankyo, Idorsia, Novartis, Osler, Roche, and Sanofi, outside the submitted work. Jacky Suen received an Advance Queensland Industry Research Fellowship. Gianluigi Li Bassi acknowledges receipt of a “BITRECS” fellowship; the “BITRECS” project has received funding from the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement no. 754550 and from the “La Caixa” Foundation (ID 100010434), under the agreement LCF/PR/GN18/50310006. Gianluigi Li Bassi also received research grants from Fisher& Paykel through his affiliated research institution. All other authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wildi, K., Livingstone, S., Ainola, C. et al. Application of anti-inflammatory treatment in two different ovine Acute Respiratory Distress Syndrome injury models: a preclinical randomized intervention study. Sci Rep 13, 17986 (2023). https://doi.org/10.1038/s41598-023-45081-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45081-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.