Abstract
Prostate Cancer (PC) is the most common male nonskin tumour in the world, and most diagnosed patients are over 65 years old. The main treatment for PC includes surgical treatment and nonsurgical treatment. Currently, for nonsurgically treated elderly patients, few studies have evaluated their prognostic factors. Our aim was to construct a nomogram that could predict cancer-specific survival (CSS) in nonsurgically treated elderly PC patients to assess their prognosis-related independent risk factors. Patient information was obtained from the Surveillance, Epidemiology and End Results (SEER) database, and our target population was nonsurgically treated PC patients who were over 65 years old. Independent risk factors were determined using both univariate and multivariate Cox regression models. A nomogram was built using a multivariate Cox regression model. The accuracy and discrimination of the prediction model were tested using the consistency index (C-index), the area under the subject operating characteristic curve (AUC), and the calibration curve. Decision curve analysis (DCA) was used to examine the potential clinical value of this model. A total of 87,831 elderly PC patients with nonsurgical treatment in 2010–2018 were included in the study and were randomly assigned to the training set (N = 61,595) and the validation set (N = 26,236). Univariate and multivariate Cox regression model analyses showed that age, race, marital status, TNM stage, chemotherapy, radiotherapy modality, PSA and GS were independent risk factors for predicting CSS in nonsurgically treated elderly PC patients. The C-index of the training set and the validation set was 0.894 (95% CI 0.888–0.900) and 0.897 (95% CI 0.887–0.907), respectively, indicating the good discrimination ability of the nomogram. The AUC and the calibration curves also show good accuracy and discriminability. We developed a new nomogram to predict CSS in elderly PC patients with nonsurgical treatment. The model is internally validated with good accuracy and reliability, as well as potential clinical value, and can be used for clinical aid in decision-making.
Similar content being viewed by others
Introduction
Since the U. S. Preventive Services Task Force (USPSTF) recommended using serum prostate specific antigen (PSA) for prostate cancer (PC) screening1. PSA screening has led to a significant increase in the diagnosis of low- and intermediate-risk prostate cancer worldwide. At present, the incidence of PC ranks first among nonskin tumours in males2,3. PC ranks fourth in total incidence by 7.4%, but in males, it is second only to lung cancer4.
Nonsurgical treatment of PC includes active surveillance (AS), androgen deprivation therapy (ADT), radiotherapy (RT), ablative therapy, chemotherapy, and emerging immunotherapy. AS is a therapeutic observation through regular monitoring of serum PSA, DRE results, serial biopsies, and diagnostic imaging (especially prostate magnetic resonance imaging (MRI)). Patients with clinically low-risk PC and some selected patients with moderate-risk disease frequently choose AS5. AS programs have been shown to be safe and effective6 in the treatment of low-risk PC. Men with localized or metastatic high-risk PC usually receive radiotherapy, while chemotherapy7,8 is recommended for patients with recurrent or metastatic, castration-sensitive, or drug-resistant PC. ADT is commonly used in locally advanced or advanced PC not suitable for surgery and is also considered the primary adjuvant regimen after prostate surgery. However, despite the survival benefits, ADT is associated with significant adverse effects, mainly including9 sexual dysfunction, gynaecomastia, anaemia, osteoporosis, and cardiovascular disease. Alternatively, ablation therapy can be used as the primary treatment for low- and medium-risk disease or as salvage therapy for7 clinical local disease with radiotherapy failure.
The prognosis of PC patients receiving different treatment modalities varies greatly. Although some patients adopt active surgical treatment, many patients also receive nonsurgical treatment. However, current clinical trials focus more on the prognosis of patients treated with surgery, especially those undergoing radical prostatectomy (RP)10,11,12. There are also many investigators comparing the prognosis of13,14,15 patients undergoing surgical treatment and AS. However, few studies have evaluated the relevant factors that affect the prognosis of nonsurgically treated PC patients.
The prognosis evaluation of PC in addition to the traditional TNM stage, PSA and Gleason score (GS) is also very important. The nomogram combines various clinicopathological factors, including PSA and GS, to predict cancer-specific survival (CSS) in PC patients, and there are already some nomograms for the prognosis of PC16,17. As a high incidence group of PC, approximately 60% of PC currently occurs in elderly men over 65 years of age and 80% of these cases are clinically localized cancers, although most patients receive active treatment18. However, considering the risks of excessive treatment, including the cardiopulmonary burden of anaesthesia and surgical and postoperative complications, many patients still take AS and other nonsurgical treatment modalities. However, for elderly patients who undergo nonsurgical treatment, the prognostic factors remain to be explored. However, there have been a number of risk assessment studies on the nonsurgical treatment of prostate cancer. Examples include Choi SY, Cooperberg MR, and studies by Hu et al. on the prostate19,20. However, these studies are limited to ADT treatment, and there is a lack of ADT data in the SEER database, so the present study focuses more attention on nonsurgical treatment, including radiotherapy and chemotherapy. To our knowledge, no predictive model can accurately predict the prognosis of elderly nonsurgically treated prostate cancer patients. We therefore aimed to develop a nomogram for nonsurgically treated elderly PC patients who can be accurately used to predict patient CSS to help clinicians and patients make decisions while avoiding overtreatment.
Patients and methods
Data source and data extraction
Information on PC patients over 65 years old undergoing non-surgical treatment between 2010 and 2018 was extracted from the SEER database. The SEER database serves as a national cancer database registers data from 18 cancer medical centers, covering approximately 30% of the population. Since the data in the SEER database are publicly available and the patient information is hidden, ethical approval and patient informed consent are not required. We followed the research guideline book published in the SEER database for the study.
The variables we obtained from the SEER database including age, race, marital status, year of diagnosis, tumor grade, TNM stage, radiotherapy method, chemotherapy, PSA, GS, and patient follow-up outcomes, including survival status, cause of death, and survival time. The race of the patients was classified as white, black, and other types. Inclusion criteria: (1) patients aged 65 years and older; (2) a pathological diagnosis of PC; and (3) patients receiving non-surgical treatment. Exclusion criteria: (1) patients younger than 65 years old; (2) unknown tumor grade; (3) unknown TNM stage; (4) patients undergoing surgical treatment or patients with unknown surgical treatment; (5) unknown GS; (6) PSA unknown; (7) survival time less than 1 month or survival time unknown. A flowchart of patient inclusion and exclusion is shown in Fig. 1.
Development and validation of the nomogram
All patients obtained between 2010 and 2018 were randomized to training set (70%) and validation set (30%) for nomogram development and internal validation. Independent risk factors for patients in the training set were identified using both univariate and multivariate Cox proportional regression models. A nomogram was established based on the results of the multivariate Cox regression analysis to predict CSS at 3-, 5-, and 8-years in non-surgical treated elderly PC patients. In addition, we calibrated the nomogram for 3-, 5-, and 8-years using 1000 autonomous samples. The consistency index (c-index) and the area under the subject operating characteristic curve (AUC) were used to test the accuracy and discrimination of the model.
Clinical application
DCA is a new algorithm to calculate the net gain of the model at different thresholds. We used DCA to examine the potential clinical value of the nomogram predictive model. We also calculated the risk for each patient from the nomogram. Using the subject operating characteristic curve (ROC) as the cut-off value, all patients were divided into high-risk and low-risk groups. Differences in survival between patients at high-risk and low-risk groups were examined using the Log-rank test and Kaplan–Meier (K–M) curves. In addition, we analyzed differences of RT and chemotherapy in high-risk and low-risk groups. When analyzing the difference in chemotherapy between the high risk and low risk groups, we also performed a 1:1 propensity matching (PSM), which made the comparison cohort more reliable. The propensity-matched cohorts were counterbalanced by age, race, marriage, year of diagnosis, tumor grade, TNM stage, RT, PSA, and GS.
Statistical analysis
Mean and standard deviation were used to describe continuous variables (age), and frequency (%) was used to describe other categorical variables (race, marriage, tumor grade, TNM stage, PSA, GS, RT and chemotherapy).Differences between groups were compared using chi-square or non-parametric U-test. The patient prognostic factors were analyzed by the Cox regression model, and the patient survival differences were analyzed by the log-rank test and the K–M curve. Statistical analyses were performed using R software version 4.1.0 and SPSS26.0. The R package includes "survival", "matching", "ggDCA", "DynNom", and "RMS". P values less than 0.05 were considered statistically significant.
Informed consent
This study is accordance with relevant guidelines and regulations. All the data in our study were obtained from the SEER database. This is a publicly open database and does not require informed consent from the subjects and/or their legal guardians.
Result
Clinical features
A total of 87,831 PC patients information between 2010 and 2018 was obtained from the SEER database, all patients received non-surgical treatment and were over 65 years of age. Patients were randomized into the training set (N = 61,595) and the validation set (N = 26,236). The mean age of all patients was 72.4 ± 5.69 years, with 77.6% white and 63.3% married. The tumor grade was mainly by grade II (39.8%) and grade III (41.3%). Most patients were T1 and T2, accounting for 64.2% and 30.5%, respectively. All patients were mainly N0 (96.6%) and M0 (94.5%). 98.8% of patients did not receive chemotherapy. RT included beam radiation (42.8%), radioactive implants or isotopes (7.23%), combined with radiation (5.43%), and no radiation (44.5%). The GS were divided into GS ≤ 6 (33.5%), 7 (39.8%), and GS ≥ 8 (26.7%), respectively. Patient PSA was < 10 ng/ml (63.3%), PSA 10–20 ng/ml (20.8%), and PSA > 20 ng/ml (15.9%).There was no significant statistical bias in the clinical characteristics of both groups, and the results are shown in Table 1.
Univariate and multivariate COX regression analysis
Univariate Cox regression models were used to analyze and screen for influencing factors associated with survival in the training set.The results showed that age, race, marriage, Grade tumor grade, TNM stage, chemotherapy, RT, PSA, and GS were all prognostic factors affecting patient survival.Then, independent risk factors associated with patient survival were screened by multivariate Cox regression analysis. Results found that age, race, marriage, TNM stage, RT method, chemotherapy, PSA and GS were independent risk factors for CSS, and tumor stage was not an independent risk factor for CSS.All of the results are shown in Table 2.
Development and validation of the nomograms
We constructed a new nomogram based on the multivariate Cox regression analysis model to predict CSS at 3, 5, and 8 years in non-surgical treated elderly PC patients (Fig. 2). The nomogram showed that PSA, GS, radiotherapy mode and TNM stage were the most critical factors affecting CSS in elderly PC treated patients. In addition, age, marriage, race, and chemotherapy also had some influence on CSS.
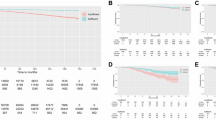
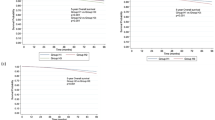
Internal cross-validation was used to verify the accuracy and discriminability of the model. The C-index for the training and validation set is 0.894 (95% CI 0.888–0.900) and 0.897 (95% CI 0.887–0.907), respectively, indicating that the prediction model has good recognition ability. The calibration curve indicates that the nomogram has good accuracy, and the results show that the predicted values of the nomogram are highly consistent with the actual observed values (Fig. 3). In the training set, the AUC at 3-, 5-, and 8-years was 91.7, 90.1, and 87.3, respectively, and in the validation set, the AUC was 91.7, 90.3, and 87.4 at 3-, 5-, and 8-years (Fig. 4), showing good discrimination of the nomogram.
Clinical application of the nomogram
The DCA can assess the potential clinical value of the nomogram, and the results show a good clinical potential value in both the training group and the validation set (Fig. 5). Furthermore, we calculated the risk values for each patient based on the nomogram, and the ROC curve was used to calculate the optimal cut-off value. Patients were divided by cut-off into high risk (total score > 153.78) and low risk (total score < 153.78).The K–M curves of both the training and validation sets showed that the survival rate of the patients in the low-risk group was significantly higher than that in the high-risk group (Fig. 6). In the high-risk group, the 3-, 5-, and 8-year CSS were 92.2%, 87.7%, and 81.0%, respectively.In the low-risk group, the 3-year, 5-year, and 8-year CSS were 99.6%, 99.1%, and 97.9%, respectively.The K–M curve analysis of RT showed that among the patients in the high-risk group, patients treated with radioactive implants or isotope and combined with radiotherapy had the best prognosis, and there was no significant survival difference between the two radiotherapy methods, followed by patients receiving beam radiation, while patients without radiotherapy had the worst prognosis; and there was no significant difference in survival between any of the four RT modalities in the low-risk group (Fig. 7). We also conducted a K–M curve analysis of chemotherapy methods, and found that the survival rate of the high-risk and low-risk groups was lower than those without chemotherapy, and too few people considered chemotherapy, resulting in outcome bias.Therefore, we matched patients 1:1 and further analyzed the survival differences of chemotherapy. The results showed that after PSM, in the high-risk group, there was no significant difference between the survival rate of chemotherapy and no chemotherapy, while in the low-risk group, the survival rate of patients receiving chemotherapy was still lower, considering the reason that most low-risk patients can achieve better treatment effect without chemotherapy, and the side effects of chemotherapy lead to worse prognosis (Fig. 8).
DCA of the nomogram in the training set (A) and the validation set (B). The Y-axis represents a net benefit, and the X-axis represents threshold probability. The green line means no patients died, and the dark green line means all patients died. When the threshold probability is between 0 and 100%, the net benefit of the model exceeds all deaths or none.
Discussion
PC is the most common noncutaneous malignancy in men in the United States and its incidence is only increasing, with 268,490 new patients expected in the United States by 2022 and an expected 34,500 deaths from PC in the United States21. Worldwide, PC accounts for 37% of malignant solid tumours in males, and an estimated 19.3 million new cancer cases were reported worldwide in 2020. Treatment modalities for PC patients include surgical treatment and nonsurgical treatment. With the popularity of serum PSA screening, the proportion of early PC diagnoses has gradually increased, and the median age at diagnosis of PC has gradually advanced from 72 years old to 66 years old22. The proportion of nonsurgical treatment is also increasing1. PC has a high incidence in the elderly population, so this study used the SEER database to establish a new nomogram to predict CSS in nonsurgically treated elderly PC patients, and our results showed that age, race, marriage, PSA, GS, RT mode, chemotherapy and TNM stage are independent risk factors for elderly prostate patients 3 and 8 years.
With PC as the most common malignancy in developed countries, most patients have an age of diagnosis of over 65 years of age23. Regarding the effect of age on malignant potential, several malignancies show different characteristics between older and younger patients. In gastric cancer as well as colon cancer, younger patients have a worse prognosis than older patients24,25. However, a meta-analysis showed a 5-year OS of 62.1% in PC patients aged 56–65 years old, compared with 59.8% aged 66–75 years old, indicating that elderly PC patients have a worse prognosis26. Our study also showed that age is an important factor in CSS in PC.
Previous literature has reported that the risk of PC varies between ethnic groups, with increased risk in African men and reduced27 risk in Asian men. PC risk factors in Asian men may differ significantly from those in white men, and subtypes may also vary in28 by ethnicity. Our predictive model suggests that race in aged nonsurgically treated PC patients is also an independent risk factor, and nomograms indicate that Black patients have the worst prognosis, followed by White, and Asian and other ethnic groups have the best prognosis. Alternatively, marriage is a protective factor for many cancer patients, for example, breast cancer and bladder cancer29,30. Considering the financial support and psychological comfort of marriage, some studies have also shown that marital status is closely related to the prognosis of PC31, which is consistent with our results.
Our nomogram shows that TNM stage is also an independent risk factor for CSS in elderly nonsurgical PC patients, and patients with distant as well as lymph node metastases have worse outcomes than nonmetastases and higher T stage, which is consistent with previous studies32. It is well known that PSA is an important factor affecting patient prognosis. Our prediction model shows that the level of PSA is also an independent risk factor affecting the CSS of PC. The results show that most elderly nonsurgical PC patients have low PSA levels, mostly below 10, and patients with PSA < 10 have a much higher prognosis than those with PSA 10–20 and above 20. In 1974, Gleason and Mellinger proposed the GS scoring system, where GS remains the most powerful predictor of PC prognosis33 compared to other clinicopathological factors and molecular markers. Although different GS groups were used in clinical practice, most researchers grouped GS by GS ≤ 6, GS7, and GS ≥ 8, and most studies showed higher GS and worse patient prognosis34,35,36. Our results showed that most GS of elderly nonsurgically treated PC patients were GS ≤ 6, which is consistent with previous literature.
RT provides a treatment for localized PC without major surgery and is the preferred treatment in many men37. Approximately 30% of PC patients receive RT each year38. PC patients with adverse pathological features after prostatectomy may benefit from postoperative RT39. RT for PC mainly includes external beam radiotherapy (EBRT), in which radiation beams produced by in vitro machines are exposed to cancer cells, brachytherapy, where radioactive substances and other isotopes are placed near cancer cells in the body, or EBRT and brachytherapy combined40. PSA has been introduced as a screening tool and is now also used as a marker of response to RT. Although it has been shown that serum PSA can appear as temporary and benign "PSA rebound" in the early stages after RT, it does not necessarily indicate PC treatment failure. PSA rebound can occur after external beam or brachytherapy and occurs in 30–40% of successfully treated men41. A randomized trial conducted by Christopher et al. showed that RT, although it improved asymptomatic survival in unselected patients with newly diagnosed metastatic PC, did not improve overall survival. However, for patients with a low metastatic burden, RT improved 3-year overall survival and failure-free survival42. The results of a phase 3 randomized trial conducted by Linda et al. showed that external irradiation radiation does not improve the CSS and OS of PC43. However, this conclusion is controversial. Freddie et al. showed that by targeting localized PC, RT significantly reduced disease progression and metastasis incidence44. The randomized trial conducted by Lars Holmberg et al. showed that RT significantly reduced mortality in PC45. Our findings suggest that patients who receive RT have better outcomes than those who do not. Moreover, we also found that among the patients receiving RT, the patients receiving external beam irradiation had the worst prognosis, while the internal implantation and combination treatment were better, with no significant difference between the two groups.
Since the 1940s, androgen ablation therapy has been the mainstay of treatment for prostate cancer, but drug resistance has developed over time. Thus, between the 1950s and 1970s, a number of small trials using alkylating agents were conducted, which was the original chemotherapy for prostate cancer. However, the initial chemotherapy results were not significant. In 1972, the National Prostate Cancer Project (NPCP) began a series of randomized single-agent and phase III combination studies called "hormone resistance" but later created "castration-resistant" PCa patients. Chemotherapy is not the primary treatment for prostate cancer, but docetaxel has improved overall survival in metastatic castration-resistant prostate cancer (mCRPC); however, combination chemotherapy or any drug added to docetaxel has failed to produce more benefit46. The recent proposal of the combination of ADT + androgen receptor-targeted agents (ARTA) or ADT + ARTA + docetaxel for mHSPC patients overcomes this clinical situation. B. A. Maiorano et al. also supported the combination of ARTA with docetaxel and ADT in patients with mHSPC47. Our nomogram showed that chemotherapy is also an independent risk factor for prognosis, and our K‒M curve analysis revealed that survival was lower in high-risk and low-risk groups than in patients without chemotherapy, and we considered too few people receiving chemotherapy to cause outcome bias. Therefore, we further analysed the survival difference of chemotherapy methods after the 1:1 PSM of patients. The results showed that after PSM, there was no significant difference between chemotherapy and without chemotherapy in the high-risk group, while in the low-risk group, the CSS of patients receiving chemotherapy was still lower, possibly because most low-risk patients can obtain better treatment effects without chemotherapy, and the side effects of chemotherapy lead to worse prognosis.
Although the nomogram established based on the SEER database has good accuracy, there are some potential limitations simultaneously, including the lack of some important clinicopathological variables, such as smoking, alcohol consumption, and haemoglobin. In addition, AS and ADT are also the main nonsurgical treatments for nonsurgical PC patients. Meanwhile, ADT, as one of the nonsurgical treatment options for patients with prostate cancer, is usually used for high-risk local or systemic advanced PC that is not suitable for radical surgery. Although ADT was explored in Beebe-Dimmer and Muralidhar et al. in the SEER-based study48,49. However, their ADT data are all from the SEER-Medicare database, and the SEER-Medicare database database is only open to Americans. We cannot obtain relevant access rights, so we cannot obtain relevant data for research. However, the SEER database lacks data related to AS and ADT, so our model also lacks the relationship between AS and ADT and prognosis. Furthermore, database-based studies are all retrospective, which may confer a risk of unavoidable selection bias. Future prospective studies with large and multicentre samples are needed for further validation of the nomogram. Finally, although our nomogram could not include all prognostic-related variables, such as BMI, smoking, and drinking, we still included most of the key clinical factors and conducted internal verification, so there would not be a large deviation in the results.
Conclusion
Our study developed a predictive model for nonsurgically treated elderly PC patients with all data from the SEER database, and we found that age, race, marriage, TNM stage, PSA, GS, RT modality, and chemotherapy were independent risk factors affecting patient CSS. The model has been internally validated with good accuracy and reliability and can be used for adjuvant decision-making in elderly prostate cancer patients.
Data availability
The SEER data analyzed in this study is available at https://seer.Cancer.gov/.
References
Stamey, T. A. et al. The prostate specific antigen era in the United States is over for prostate cancer: What happened in the last 20 years?. J. Urol. 172(4 Pt 1), 1297–1301 (2004).
American Cancer Society (2019).
Canadian Cancer Society (2019).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Chen, R. C. et al. Active surveillance for the management of localized prostate cancer (cancer care ontario guideline): American society of clinical oncology clinical practice guideline endorsement. J. Clin. Oncol. 34(18), 2182–2190 (2016).
Klotz, L. et al. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J. Clin. Oncol. 33(3), 272–277 (2015).
Gravis, G. et al. Chemotherapy in hormone-sensitive metastatic prostate cancer: Evidences and uncertainties from the literature. Cancer Treat Rev. 55, 211–217 (2017).
Cornford, P. et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part II: Treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur. Urol. 71(4), 630–642 (2017).
Muniyan, S. et al. Cardiovascular risks and toxicity: The Achilles heel of androgen deprivation therapy in prostate cancer patients. Biochim. Biophys. Acta Rev. Cancer 1874(1), 188383 (2020).
Carrie, C. et al. Short-term androgen deprivation therapy combined with radiotherapy as salvage treatment after radical prostatectomy for prostate cancer (GETUG-AFU 16): A 112-month follow-up of a phase 3, randomised trial. Lancet Oncol. 20(12), 1740–1749 (2019).
Eastham, J. A. et al. Cancer and leukemia group B 90203 (alliance): Radical prostatectomy with or without neoadjuvant chemohormonal therapy in localized, high-risk prostate cancer. J. Clin. Oncol. 38(26), 3042–3050 (2020).
Parker, C. C. et al. Timing of radiotherapy after radical prostatectomy (RADICALS-RT): A randomised, controlled phase 3 trial. Lancet 396(10260), 1413–1421 (2020).
Bill-Axelson, A. et al. Radical prostatectomy or watchful waiting in prostate cancer: 29-year follow-up. N. Engl. J. Med. 379(24), 2319–2329 (2018).
Bill-Axelson, A. et al. Radical prostatectomy or watchful waiting in early prostate cancer. N. Engl. J. Med. 370(10), 932–942 (2014).
Wilt, T. J. et al. Radical prostatectomy versus observation for localized prostate cancer. N. Engl. J. Med. 367(3), 203–213 (2012).
Gafita, A. et al. Nomograms to predict outcomes after (177)Lu-PSMA therapy in men with metastatic castration-resistant prostate cancer: An international, multicentre, retrospective study. Lancet Oncol. 22(8), 1115–1125 (2021).
Zhu, X., Gou, X. & Zhou, M. Nomograms predict survival advantages of gleason score 3+4 over 4+3 for prostate cancer: A SEER-based study. Front. Oncol. 9, 646 (2019).
Meltzer, D., Egleston, B. & Abdalla, I. Patterns of prostate cancer treatment by clinical stage and age. Am. J. Public Health 91(1), 126–128 (2001).
Cooperberg, M. R. et al. Risk assessment among prostate cancer patients receiving primary androgen deprivation therapy. J. Clin. Oncol. 27(26), 4306–4313 (2009).
Hu, M. B. et al. Prognostic factors in Chinese patients with prostate cancer receiving primary androgen deprivation therapy: Validation of Japan Cancer of the Prostate Risk Assessment (J-CAPRA) score and impacts of pre-existing obesity and diabetes mellitus. Int. J. Clin. Oncol. 23(3), 591–598 (2018).
Siegel, R. L. et al. Cancer statistics, 2022. CA Cancer J. Clin. 72(1), 7–33 (2022).
Droz, J. P. et al. Management of prostate cancer in elderly patients: Recommendations of a task force of the international society of geriatric oncology. Eur. Urol. 72(4), 521–531 (2017).
Arnold, M. et al. Recent trends in incidence of five common cancers in 26 European countries since 1988: Analysis of the European cancer observatory. Eur. J. Cancer 51(9), 1164–1187 (2015).
Kong, X. et al. Comparison of the clinicopathological characteristics of young and elderly patients with gastric carcinoma: A meta analysis. J. Surg. Oncol. 106(3), 346–352 (2012).
Al-Barrak, J. & Gill, S. Presentation and outcomes of patients aged 30 years and younger with colorectal cancer: A 20-year retrospective review. Med. Oncol. 28(4), 1058–1061 (2011).
Kimura, T. et al. Validation of the prognostic grouping of the seventh edition of the tumor-nodes-metastasis classification using a large-scale prospective cohort study database of prostate cancer treated with primary androgen deprivation therapy. Int. J. Urol. 20(9), 880–888 (2013).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer Statistics, 2017. CA Cancer J. Clin. 67(1), 7–30 (2017).
Freedland, S. Prostate cancer: Race and prostate cancer personalized medicine: The future. Nat. Rev. Urol. 15(4), 207–208 (2018).
Zhai, Z. et al. Effects of marital status on breast cancer survival by age, race, and hormone receptor status: A population-based Study. Cancer Med. 8(10), 4906–4917 (2019).
Tao, L. et al. Marital status and prognostic nomogram for bladder cancer with distant metastasis: A SEER-based study. Front. Oncol. 10, 586458 (2020).
Ellis, L. et al. Racial and ethnic disparities in cancer survival: The contribution of tumor, sociodemographic, institutional, and neighborhood characteristics. J. Clin. Oncol. 36(1), 25–33 (2018).
van der Poel, H. et al. Imaging and T category for prostate cancer in the 8th edition of the union for international cancer control TNM classification. Eur. Urol. Oncol. 3(5), 563–564 (2020).
Epstein, J. I. An update of the Gleason grading system. J. Urol. 183(2), 433–440 (2010).
Ham, W. S. et al. New prostate cancer grading system predicts long-term survival following surgery for gleason score 8–10 prostate cancer. Eur. Urol. 71(6), 907–912 (2017).
Hollemans, E. et al. Cribriform architecture in radical prostatectomies predicts oncological outcome in Gleason score 8 prostate cancer patients. Mod. Pathol. 34(1), 184–193 (2021).
Kane, C. J. et al. Variability in outcomes for patients with intermediate-risk prostate cancer (Gleason score 7, international society of urological pathology Gleason group 2–3) and implications for risk stratification: A systematic review. Eur. Urol. Focus 3(4–5), 487–497 (2017).
Holmes, J. A. et al. Is primary prostate cancer treatment influenced by likelihood of extraprostatic disease? A surveillance, epidemiology and end results patterns of care study. Int. J. Radiat. Oncol. Biol. Phys. 84(1), 88–94 (2012).
Cancer Research UK (2019).
Wiegel, T. et al. Phase III postoperative adjuvant radiotherapy after radical prostatectomy compared with radical prostatectomy alone in pT3 prostate cancer with postoperative undetectable prostate-specific antigen: ARO 96–02/AUO AP 09/95. J. Clin. Oncol. 27(18), 2924–2930 (2009).
Pugh, T. J. et al. Radiation therapy modalities in prostate cancer. J. Natl. Compr. Cancer Netw. 11(4), 414–421 (2013).
Naghavi, A. O. et al. Clinical implications of a prostate-specific antigen bounce after radiation therapy for prostate cancer. Int. J. Clin. Oncol. 20(3), 598–604 (2015).
Parker, C. C. et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): A randomised controlled phase 3 trial. Lancet 392(10162), 2353–2366 (2018).
Kerkmeijer, L. G. W. et al. Focal boost to the intraprostatic tumor in external beam radiotherapy for patients with localized prostate cancer: Results from the FLAME randomized phase III trial. J. Clin. Oncol. 39(7), 787–796 (2021).
Hamdy, F. C. et al. 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N. Engl. J. Med. 375(15), 1415–1424 (2016).
Holmberg, L. et al. A randomized trial comparing radical prostatectomy with watchful waiting in early prostate cancer. N. Engl. J. Med. 347(11), 781–789 (2002).
Nader, R., El Amm, J. & Aragon-Ching, J. B. Role of chemotherapy in prostate cancer. Asian J. Androl. 20(3), 221–229 (2018).
Maiorano, B. A. et al. Addition of androgen receptor-targeted agents to androgen-deprivation therapy and docetaxel in metastatic hormone-sensitive prostate cancer: A systematic review and meta-analysis. ESMO Open 7(5), 100575 (2022).
Beebe-Dimmer, J. L. et al. Patterns of bicalutamide use in prostate cancer treatment: A U. S. real-world analysis using the SEER-medicare database. Adv. Ther. 35(9), 1438–1451 (2018).
Muralidhar, V. et al. Variation in national use of long-term ADT by disease aggressiveness among men with unfavorable-risk prostate cancer. J. Natl. Compr. Cancer Netw. JNCCN 14(4), 421–428 (2016).
Funding
This study was supported by Yunnan Education Department of Science Research Fund (No. 2023 J0295), Kunming City Health Science and Technology Talent “1000” training Project (No. 2020-SW (Reserve)-112), Kunming Health and Health Commission Health Research Project (No. 2020-0201-001), Joint project of Science and Technology Department of Yunnan Province and Kunming Medical University (202301AY070001-108), Kunming Medical Joint Project of Yunnan Science and Technology Department (No. 202001 AY070001-271), and Open Research Fund of Clinical Research Center for Children's Health and Diseases of Yunnan Province (2022-ETYY-YJ-03).The funding bodies played no role in the study's design and collection, analysis and interpretation of data, and writing the manuscript.
Author information
Authors and Affiliations
Contributions
Z.X.Z. and C.H.Z.H. designed the study; Z.X.Z., J.K.W., Z.G.Y., F.M.J. collected and analyzed the data; Z.X.Z. and C.H.Z.H. drafted the initial manuscript; C.H.Z.H., Y.H., J.M., H.C.J. and B.Y. revised the article critically; C.H.Z.H., Z.X.Z. and Q.C. reviewed and edited the article. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Z., Cai, Q., Wang, J. et al. Development and validation of a nomogram to predict cancer-specific survival in nonsurgically treated elderly patients with prostate cancer. Sci Rep 13, 17719 (2023). https://doi.org/10.1038/s41598-023-44911-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-44911-z
This article is cited by
-
Individualized detection of TMPRSS2-ERG fusion status in prostate cancer: a rank-based qualitative transcriptome signature
World Journal of Surgical Oncology (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.