Abstract
This study aimed to investigate the efficacy of tranexamic acid supplemented with local infiltration analgesia in reducing blood loss in patients undergoing unicompartmental knee arthroplasty (UKA). This retrospective study was conducted on 176 individuals with a mean age of 64.27 (standard deviation [SD], 7.16) years undergoing unicompartmental cemented knee arthroplasty. The patients were divided into three groups according to patient blood management: I, patients without additional bleeding protocol (control group); II, patients intravenously administered tranexamic acid (TXA) (TXA group); and III, patients with exact TXA protocol combined with intraoperative local infiltration analgesia (LIA) (TXA + LIA group). Blood loss was measured as a substitute for blood loss by the maximal haemoglobin (Hb) drop compared with the preoperative Hb level. The mean Hb drops for the control, TXA, and TXA + LIA groups were 2.24 (16.0%), 2.14 (15.4%), and 1.81 (12.6%) g/dl, respectively. The mean hospitalisation days for patients in the control, TXA, and TXA + LIA groups were 5.91 (SD 1.24), 5.16 (SD 0.95), and 4.51 (SD 0.71) days, respectively. The combination of TXA with LIA reduces perioperative blood loss for patients after UKA.
Similar content being viewed by others
Introduction
Osteoarthritis is one of the most common causes of disability. Furthermore, treatment of the complications caused by osteoarthritis results in significant financial burden. Total knee arthroplasty (TKA), next to total hip arthroplasty (THA), is one of the most frequently performed elective orthopaedic surgeries. TKA mainly reduces pain, restores knee function, and improves patients’ quality of life. Unicompartmental knee arthroplasty (UKA) is performed on patients in whom only one knee compartment is affected by arthritis. UKA often involves the medial compartment of the knee. Compared with TKA, UKA is associated with preserving normal kinematics, translating into faster rehabilitation and quicker recovery. A simpler approach and the replacement of only one compartment are associated with minor blood loss. As UKA results in less postoperative pain, without blood transfusion, this procedure leads to shorter hospital stays and is less expensive than TKA1,2,3. The main contraindications to UKA are inflammatory arthritis, fixed varus deformity > 10°, fixed valgus deformity > 5°, range of motion < 90°, flexion contracture > 10°, contralateral meniscal damage or previous meniscectomy, tricompartmental arthritis, and grade IV patellofemoral chondropathy according to the International Cartilage Repair Society. Reducing perioperative blood loss is essential in patient blood management strategies. This approach involves evidence-based management to reduce the number of patients requiring postoperative transfusion after knee and hip replacement4. Tranexamic acid (TXA) is a fibrinolysis inhibitor that directly prevents plasminogen activation and inhibits the degradation of fibrin clots by activated plasmin. TXA promotes haemostasis and reduces the duration and quantity of blood loss5,6. Intravenous (IV) and topical TXA administration effectively reduces blood loss and risk of transfusion in patients after TKA7,8. Local infiltration analgesia (LIA) is a technique developed by Kerr and Kohan to reduce pain after TKA and THA9. It was initially assumed that ropivacaine, ketorolac, and adrenaline had infiltrated the tissues around the surgical field. LIA has been widely used for pain relief in patients undergoing total knee replacement for over 15 years. Blood loss can be evaluated either by estimating the loss or by measuring the drop in haemoglobin (Hb) and haematocrit (Hct) levels as a surrogate for blood loss10,11. This study aimed to investigate the efficacy of LIA-supplemented TXA in reducing blood loss in patients undergoing UKA.
Materials and methods
We used the Strengthening the Reporting of Observational studies in Epidemiology protocol, which is designed for retrospective observational studies12. Patients diagnosed with unicompartmental osteoarthritis who underwent unilateral primary cemented medial UKA at ZSM Hospital in Chorzów between January 2018 and July 2022 were enrolled in this study. The following inclusion criteria were established for further evaluation: (1) patients undergoing medial UKA exclusively, (2) patients operated under spinal anaesthesia, and (3) patients operated on by one of the following two surgeons: Ł.W. and B.O. Patients (1) with pre-existing coagulopathy, (2) receiving long-term anticoagulant therapy before surgery, and (3) undergoing other additional procedures, including implant removal, were excluded. We established generally accepted contraindications for UKA, as described in the Introduction section. During the study period, only four patients underwent lateral UKA. Owing to a more extensive surgical approach and an incommensurably small number of patients, we excluded them from the analysis.
After considering the above criteria, 176 individuals were included for further analysis. The patients were divided into three groups based on patient blood management: I, patients without additional bleeding protocol (control group); II, patients intravenously administered 1.0 g of TXA 30 min before skin incision and 3 h later (TXA group); and III, patients with exact TXA protocol combined with intraoperative LIA (ropivacaine [100 mg] and epinephrine [0.25 mg] in a 50-ml solution) (TXA + LIA group). The differences in the number of individuals among the groups resulted from restrictions related to coronavirus disease 2019 during the study period and the growing number of UKA.
According to the Polish guidelines for preventing and treating venous thromboembolism, each patient received a dose of low-molecular-weight heparin (LMWH) 12 h before surgery (40 mg Clexane, Sanofi, Paris, France), and LMWH was continued postoperatively for 14 days. To assess blood loss, the Hb level before surgery was compared with the lowest Hb level during the hospital stay. Laboratory tests were performed on the day of hospital admission, the second postoperative day, and the day preceding discharge.
Follow-up for the included patients was extended to 1 month after discharge to assess the early readmission rate.
Surgical technique
The surgeries were performed by two surgeons (Ł.W. and B.O.). A standard medial parapatellar approach was used in all the patients. Only one type of prosthesis was used in our study, JOURNEY™ UNI (Smith & Nephew, Cordova, USA). Surgical procedures were performed without a tourniquet, and thorough haemostasis was achieved. A drain was not used in all groups. The cement-receiving bone surfaces were cleaned using a pulse lavage system to remove fat residue, bone debris, marrow, and blood. The LIA solution contained 100 mg of ropivacaine and 0.25 mg of epinephrine in a 50-ml volume. According to the assumed intra-hospital protocol, half of the dose was used for TKA. The solution was sterile and prepared using a 50-ml syringe: 15 ml solution for the posteromedial joint capsule, 10 ml medial collateral ligament, 10 ml supracondylar soft tissue, and 15 ml subcutaneous tissue (Fig. 1). The joint capsule was tightly sutured using STRATAFIX Symmetric PDS Plus 1–0 (ETHICON, Johnson & Johnson, Germany). After the surgery, a compression dressing was applied to the operated limb. A standard rehabilitation programme was implemented on the first postoperative day. We present an example of a patient who underwent a medial UKA in Fig. 2.
This study was approved by the Bioethics Committee of Silesian Medical Chamber in Katowice, Poland (ŚIL.KB.1011.2022). All procedures in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Ethics approval and consent to participate
This study was approved by the Bioethics Committee of Silesian Medical Chamber in Katowice, Poland (ŚIL.KB.1011.2022). Informed consent was not required owing to the retrospective nature of the study.
Results
A total of 176 (control group, 59; TXA group, 45; TXA + LIA group, 72) individuals were included in the analysis. All groups were homogeneous in terms of sex, with a female predominance (control group, 72.88%; TXA group, 75.55%; TXA + LIA group, 68.05%). The mean age of all patients was 64.27 (standard deviation [SD], 7.16) years. The mean body mass index (BMI) of all patients was 27.1 (SD, 1.88) kg/m2. Table 1 presents an overview of the study groups. In all groups, the overall blood transfusion rate after the primary UKA was 0%. We did not observe a drop in Hb < 9 g/dl in any patient.
Statistical analyses
For statistical analyses, analysis of variance (ANOVA) parametric tests with Tukey’s post-test for unequal samples were used to assess the Hb drop, and the Kruskal–Wallis ANOVA test with Dun’s post hoc test was used to assess the length of hospitalisation. Spearman’s rho coefficients were used to determine correlations. All statistical tests were performed at p = 0.05.
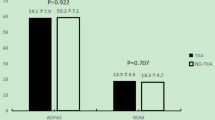
The TXA group had less Hb drop (M = 2.14 [15.4%]) than the control group (M = 2.24 [16.0%]), but the difference was not statistically significant (p = 0.749). In the TXA + LIA group, the decrease in Hb level was significantly (p = 0.001) lower (M = 1.81 [12.6%]) than that in the control group (M = 2.24 [16.0%]) and significantly lower (p = 0.043) than that in the TXA group (M = 2.14 [15.4%]). The mean values with 95% confidence interval are shown in Fig. 3. The length of hospitalisation was shorter (ME = 5) in the TXA group than in the control group (ME = 6), and the difference was statistically significant (p = 0.004). Moreover, the length of hospitalisation was significantly shorter (p < 0.001) in the TXA + LIA group (ME = 4.51) than in the control (ME = 6) and TXA (p = 0.005) groups. Figure 4 presents the statistics of the median, lower, and upper quartiles and minimum–maximum days of hospitalisation depending on the examined group. Based on Spearman’s rho correlation tests, sex and age were not significantly associated with a decrease in Hb levels. For the TXA (rho = 0.708, p < 0.001) and TXA + LIA (rho = 0.660, p < 0.001) groups, we observed a more significant decrease in Hb levels in patients with higher BMI than in those with lower BMI.
Discussion
Different from TKA, UKA is not a surgical procedure related to an increased blood transfusion risk. The transfusion rates for patients undergoing UKA range from 0 to 7.4%10,13,14,15. Less blood loss in UKA is mainly due to the less invasive approach, limited bone cuts to a single compartment, and lack of the need for extensive soft tissue balancing. IV and topical TXA administration effectively reduces blood loss and transfusion risk in patients after TKA7,8,16. The benefits of TXA in decreasing blood loss in UKA have yet to be fully validated. Topical TXA reduces perioperative blood loss in patients undergoing UKA without associated complications17,18. However, there have been concerns regarding the chondrotoxicity of TXA in UKA, where native cartilage is still present in the knee after surgery19,20. Therefore, some researchers do not recommend using TXA in UKA20. Pongcharoen et al.21, on a group of 120 knees, demonstrated that using IV TXA in UKA resulted in lower blood loss than not using IV TXA in UKA, but the differences were not significant. Similarly, in our study, the TXA group had less Hb drop than the control group, but the difference was not statistically significant (p = 0.749). Our study is the first to determine the effects of combining TXA with LIA on blood loss after UKA. The decrease in Hb level was significantly lower (p = 0.001) in the TXA + LIA group than in the control and TXA (p = 0.043) groups.
We have started using LIA routinely in TKA and UKA since January 2021. Contrary to most recommendations, we used a volume of 100 ml for TKA and 50 ml for UKA because high LIA volumes may increase the risk of prolonged wound drainage or leaking9,22. Patients in the LIA group had significantly lower pain scores according to the visual analogue scale, especially in the first 2 postoperative days, compared with other patients. However, this detailed assessment differs from the purpose of the present study. We did not use a drain for any of the UKA groups. Surgical drainage increases postoperative blood loss23,24.
Several authors have assessed the risk factors for morphological decrease after TKA and THA to identify patients at risk for blood transfusion25,26. Preoperative anaemia is the most significant risk factor for blood transfusion after TKA27.
None of the patients in our study required a transfusion. According to in-hospital guidelines, surgery is delayed in patients with anaemia until their Hb values are equalised. BMI, female sex, and age are significant predictors of transfusion in patients undergoing elective TKA28,29,30. According to our analysis, based on Spearman’s rho correlation tests, sex and age were not preoperative predictors of higher blood loss rates. For the TXA (rho = 0.708, p < 0.001) and TXA + LIA (rho = 0.660, p < 0.001) groups, we observed a more significant decrease in Hb levels in patients with higher BMI than in those with lower BMI. In recent years, outpatient and fast-track UKA pathways have gained increasing attention31,32,33. Sephton et al.34, in line with the results of our study, reported a transfusion rate of 0% in patients after UKA. However, the average hospitalisation time in their study was shorter (3.3 days) than that of our study. We did not follow fast-track UKA in our study. The length of hospitalisation was shorter in the TXA (p = 0.004) and TXA + LIA groups (p < 0.001) than in the control group. Moreover, Sephton et al. concluded that postoperative control of Hb and Hct was unnecessary and could be omitted in postoperative procedures.
Although patients undergoing knee replacement routinely receive prophylactic anticoagulants, venous thromboembolic events continue to occur. In our study, we used a double dose of 1.0 g TXA, administered 30 min before skin incision and 3 h later, and we did not observe any case of deep venous thrombosis or pulmonary embolism.
The strength of our study is the homogeneity of the comparison groups. Based on the data analysis, we confirmed the synergistic effect of TXA and LIA in reducing perioperative blood loss. However, this study has some limitations. The main limitation of this study was its retrospective design. Furthermore, we did not evaluate perioperative blood loss.
Further analysis is required to understand the effects of combining TXA with LIA in reducing perioperative blood loss and blood transfusion rate after unicompartmental knee replacement. Assessing the predictive risk factors for UKA is difficult because of the low transfusion rate and requires a large cohort of patients to reach meaningful conclusions.
Conclusions
The combination of TXA and LIA reduces perioperative blood loss in patients after UKA. The use of LIA in the perioperative protocol does not increase the risk of local wound healing complications. The use of TXA with LIA results in shorter length of hospitalisation compared with the use of isolated TXA.
Data availability
The data generated and analyzed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- BMI:
-
Body mass index
- Hb:
-
Haemoglobin
- Hct:
-
Haematocrit
- LMWH:
-
Low-molecular-weight heparin
- SD:
-
Standard deviation
- THA:
-
Total hip arthroplasty
- TKA:
-
Total knee arthroplasty
- TXA:
-
Tranexamic acid
- UKA:
-
Unicompartmental knee arthroplasty
References
Zuiderbaan, H. A. et al. Unicompartmental knee arthroplasty versus total knee arthroplasty: Which type of artificial joint do patients forget?. Knee Surg. Sports Traumatol. Arthrosc. 25, 681–686 (2017).
Lum, Z. C. et al. Early outcomes of twin-peg mobile-bearing unicompartmental knee arthroplasty compared with primary total knee arthroplasty. Bone Jt. J. 98, 28–33 (2016).
Siman, H. et al. Unicompartmental knee arthroplasty vs total knee arthroplasty for medial compartment arthritis in patients older than 75 years: Comparable reoperation, revision, and complication rates. J. Arthroplast. 32, 1792–1797 (2017).
Khanna, A., Gougoulias, N., Longo, U. G. & Maffulli, N. Minimally invasive total knee arthroplasty: A systematic review. Orthop. Clin. N. Am. 40, 479–489 (2009).
Tengborn, L., Blomback, M. & Berntorp, E. Tranexamic acid: An old drug still going strong and making a revival. Thromb. Res. 135(2), 231–242 (2015).
Eubanks, J. D. Antifibrinolytics in major orthopaedic surgery. J. Am. Acad. Orthop. Surg. 18, 132–138 (2010).
Hourlier, H., Reina, N. & Fennema, P. Single dose intravenous tranexamic acid as effective as continuous infusion in primary total knee arthroplasty: A randomised clinical trial. Arch. Orthop. Trauma Surg. 135, 465–471 (2015).
Lin, S. Y. et al. The efficacy of combined use of intraarticular and intravenous tranexamic acid on reducing blood loss and transfusion rate in total knee arthroplasty. J. Arthroplast. 30(5), 776–780 (2015).
Kerr, D. R. & Kohan, L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: A case study of 325 patients. Acta Orthop. 79, 174–178 (2008).
Schwab, P. E., Lavand’homme, P., Yombi, J. C. & Thienpont, E. Lower blood loss after unicompartmental than total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 23(12), 3494–3500 (2015).
Spahn, D. R. Anemia and patient blood management in hip and knee surgery: A systematic review of the literature. Anesthesiology 113, 482–495 (2010).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 370, 1453–1457 (2007).
Lombardi, A. V. Jr., Berend, K. R., Walter, C. A., Aziz-Jacobo, J. & Cheney, N. A. Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty?. Clin. Orthop. Relat. Res. 467, 1450–1457 (2009).
Yang, K. Y., Wang, M. C., Yeo, S. J. & Lo, N. N. Minimally invasive unicondylar versus total condylar knee arthroplasty-early results of a matched-pair comparison. Singap. Med. J. 44, 559–662 (2003).
Alshryda, S. et al. Tranexamic acid in total knee replacement: A systematic review and meta-analysis. J. Bone Jt. Surg. Br. 93, 1577–1585 (2011).
Tai, T. W., Yang, C. Y., Jou, I. M., Lai, K. A. & Chen, C. H. Temporary drainage clamping after total knee arthroplasty: A meta-analysis of randomized controlled trials. J. Arthroplast. 25, 1240–1245 (2010).
Parker, M. J., Roberts, C. P. & Hay, D. Closed suction drainage for hip and knee arthroplasty: A meta-analysis. J. Bone Jt. Surg. 86, 1146–1152 (2004).
Fan, L. et al. The comparison of local infiltration analgesia with peripheral nerve block following total knee arthroplasty (TKA): A systematic review with meta-analysis. J. Arthroplast. 30(9), 1664–1671 (2015).
Pongcharoen, B. & Ruetiwarangkoon, C. Does tranexamic acid reduce blood loss and transfusion rates in unicompartmental knee arthroplasty?. J. Orthop. Sci. 21(2), 211–215 (2016).
Moo, I. H., Chen, J. Y. Q., Pagkaliwaga, E. H., Tan, S. W. & Poon, K. B. Bone wax is effective in reducing blood loss after total knee arthroplasty. J. Arthroplast. 32(5), 1483–1487 (2017).
Wu, J. et al. Intra-articular injection of tranexamic acid on perioperative blood loss during unicompartmental knee arthroplasty. Med. Sci. Monit. 25, 5068–5074 (2019).
Waddell, B. S., Zahoor, T., Meyer, M., Ochsner, L. & Chimento, G. Topical tranexamic acid use in knee periprosthetic joint infection is safe and effective. J. Knee Surg. 29(5), 423–429 (2016).
Parker, J. D., Lim, K. S., Kieser, D. C., Woodfield, T. B. F. & Hooper, G. J. Is tranexamic acid toxic to articular cartilage when administered topically? What is the safe dose?. Bone Jt. J. 100(3), 404–412 (2018).
Jacob, B. et al. Tranexamic acid is toxic on human chondrocytes, in vitro. J. Orthop. 20, 1–5 (2020).
To, J. et al. Predicting perioperative transfusion in elective hip and knee arthroplasty: A validated predictive model. Anesthesiology 127, 317–325 (2017).
Slover, J. et al. Incidence and risk factors for blood transfusion in total joint arthroplasty: Analysis of a statewide database. J. Arthroplast. 32, 2684–2687 (2017).
Kasivisvanathan, R., Ramesh, V., Rao Baikady, R. & Nadaraja, S. Preoperative anaemia is associated with increased allogeneic pack red cell transfusion in revision hip and knee joint arthroplasty: A retrospective analysis of 5387 patients over a 10-year period at a single high volume centre. Transfus Med. 26, 271–277 (2016).
Feagan, B. G. et al. Transfusion practice in elective orthopaedic surgery. Transfus Med. 11, 87–95 (2001).
Rosencher, N. et al. Orthopedic surgery transfusion hemoglobin European overview (OSTHEO) study: Blood management in elective knee and hip arthroplasty in Europe. Transfusion 43, 459–469 (2003).
Maempel, J., Wickramasinghe, N., Clement, N., Brenkel, I. & Walmsley, P. The preoperative levels of haemoglobin in the blood can be used to predict the risk of allogenic blood transfusion after total knee arthroplasty. Bone Jt. J. 98, 490–497 (2016).
Kehlet, H. & Thienpont, E. Fast-track knee arthroplasty: Status and future challenges. Knee 20(Suppl. 1), S29-33 (2013).
Cross, M. B. & Berger, R. Feasibility and safety of performing outpatient unicompartmental knee arthroplasty. Int. Orthop. 38, 443–447 (2014).
Gondusky, J. S. et al. Day of surgery discharge after unicompartmental knee arthroplasty: An effective perioperative pathway. J. Arthroplast. 29, 516–519 (2014).
Sephton, B. M., Edwards, T. C., Bakhshayesh, P. & Nathwani, D. Should we routinely perform a post-operative hemoglobin check following unicompartmental knee arthroplasty?. Knee 27(1), 249–256 (2020).
Funding
This paper was not funded. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Contributions
Ł.W. designed the study and drafted the manuscript. Ł.W. collected data. Ł.W., B.O. and M.D. conducted the data analysis. Ł.W. prepared the final version of the manuscript. Ł.W. B.O. and M.D. critically reviewed and edited the manuscript. All authors have read and agreed to the published version of the manuscript. Informed consent was not required owing to the retrospective nature of the study and approved by the Bioethics Committee of Silesian Medical Chamber in Katowice, Poland.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wiktor, Ł., Osadnik, B. & Damps, M. Efficacy of tranexamic acid supplemented with local infiltration analgesia in reducing blood loss in patients undergoing unicompartmental knee arthroplasty. Sci Rep 13, 17304 (2023). https://doi.org/10.1038/s41598-023-44651-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-44651-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.