Abstract
Studying the impact of local meteorological conditions and air pollution on cardiovascular disease is crucial for reducing the burden of cardiovascular disease. However, there have been few studies on the acute effects of various air pollutants on stable ischemic heart disease (SIHD), and the effects of these factors are not well defined and require further investigation. We performed a time-series study aimed at exploring the association between short-term exposure to various air pollutants and emergency department (ED) visits for SIHD during 2013–2020 in Baoshan District Renhe Hospital of Shanghai, China. The associations between air pollution (NO2, PM2.5, PM10, SO2 O3-8 h and CO) and ED visits were analyzed using quasi-Poisson regression. Subgroup and sensitivity analyses were conducted. From 2013 to 2020, a total of 18,241 ED visits for SIHD were recorded. Elevated PM2.5, PM10, NO2, SO2 and CO were significantly associated with increased ED visits for SIHD at lag (0, 5), lag 0, lag (0-4, 01-03), lag (0-3, 5, 01-03) and lag (3-5). When the concentration of O3-8 h was lower than the threshold recommended by the WHO, exposure to O3-8 h was associated with a slightly decreased risk of SIHD. Moreover, the relationship between different types of air pollution and the frequency of ED visits exhibited variations based on gender, age, and seasonality. This study suggests that short-term exposure to PM2.5, PM10, NO2, SO2 and CO might induce SIHD, especially in old females. Air pollution control measures should be encouraged to prevent the occurrence and development of SIHD.
Similar content being viewed by others
Introduction
Coronary heart disease (CHD) also called ischemic heart disease (IHD), one of the most serious cardiovascular disease1, contributing significantly to global mortality and morbidity rates2. Stable ischemic heart disease (SIHD) is a syndrome marked by stable angina, which refers to pain or pressure brought on reliably by exertion or emotion and relieved by rest or nitroglycerin3. This may or may not be associated with obstructive IDH3. SIHD is a major contributor to mortality rates in the United States and numerous other countries4. Therefore, identifying risk factors for SIHD is crucial to develop more efficient strategies for its management and prevention.
It is widely accepted that environmental factors play an important role in the occurrence and development of cardiovascular diseases. Exposure to adverse atmospheric conditions and various air pollutants is associated with an increased risk of CHD and mortality5. Both low and high air temperatures have been identified as risk factors for cardiovascular diseases6,7 and have been associated with increased mortality rates8.
In addition, there is mounting evidence that certain ambient air pollutants are linked to an elevated risk of CHD. A systematic review of 26 studies investigated the adverse effects of short-term exposure to air pollution associated with CHD and found that such exposure can increase the incidence of adverse cardiovascular events and the risk of death from cardiovascular causes9. Short-term exposure to PM2.5 has been reported to be associated with a 1~3% increase in the risk of acute cardiovascular events10, and PM10 exposure is also positively associated with the number of hospitalizations for CHD11,12. Apart from particulate pollution, short-term exposure to NO2 was also found to be positively associated with the number of hospitalizations for CHD11.
With the intensification of global climate change and industrialization, meteorological conditions and air pollution have become one of the main factors leading to the occurrence and exacerbation of cardiovascular disease. The incidence of CHD continues to rise every year in China13. Moreover, according to Shanghai Health Statistics Reports in 202114, the specific mortality rate of the cardiovascular system in Shanghai was 391.50 per 10^5, making it the leading cause of death. It is important for individuals with SIHD to take extra precautions when exposed to multiple air pollutants. Air pollution control efforts should adopt a comprehensive strategy that considers the simultaneous effects of various pollutants. In addition, implementing public health and environmental measures to reduce air pollution can help mitigate the global trend of increasing cardiovascular disease. However, few previous studies have explored the relationships between various types of air pollution and ED visits for SIHD15,16,17,18,19,20. Moreover, no research has been conducted to simultaneously investigate the relationships between six different types of air pollutants (PM2.5, PM10, NO2, SO2, CO, and O3-8h) and SIHD. Therefore, our study aimed to investigate the correlation between short-term exposure to different types of air pollution and ED visits for SIHD in Shanghai, China, from 2013 to 2020.
Methods
Study settings
This study was conducted in Shanghai, China (Fig. S1), which is located at a latitude of 31.12° N and a longitude of 121.30° E. Shanghai experiences a subtropical monsoon climate, with hot and rainy summers and cold and relatively dry winters21. Shanghai, with a population of 24.8 million in 2022, boasts the largest urban area in China. It serves as a prominent international hub for economic, financial, trade, shipping, and innovation activities within the country22.
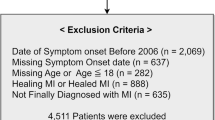
Emergency department (ED) visit data
ED visit records were extracted from the computerized medical database of Renhe Hospital in Baoshan District, Shanghai, China, from January 1, 2013, to December 31, 2020. This hospital is a comprehensive hospital in Shanghai equipped with 360 beds and catering to over 0.7 million outpatients each year. Detailed patient information, such as visit dates, age, gender, and clinical diagnoses, was collected for analysis. The diagnoses of all patients in our study according to the tenth edition of the International Classification of Disease (ICD-10) and then documented on ED discharge records. I25 and I20 except I20.0 was selected to identify SIHD cases as a previous study reported23.
Air pollution and meteorological data
Daily average concentrations for particulate matter (PM)2.5 (fine particulate matter with aerodynamic diameter ≤ 2.5 μm), PM10 (fine particulate matter with aerodynamic diameter ≤ 10 μm), sulfur dioxide (SO2), nitrogen dioxide (NO2), carbon monoxide (CO), and 8-h maximum levels of O3 (O3-8 h) from January 1, 2013, to December 31, 2020, were obtained from the air quality sharing platform of China. This platform is administered by China’s Ministry of Environmental Protection and displays real-time concentrations of criteria air pollutants in all national air quality monitoring sites around China24,25. We utilized the average air pollutant concentrations obtained from all the available air pollution monitoring stations across Shanghai city as a proxy for measuring air pollution exposure. Daily meteorological data, such as daily mean temperature (°C) and relative humidity (%), were collected from the National Weather Data Sharing System of China (http://data.cma.cn)24.
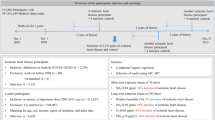
Statistical analysis
We conducted a comprehensive analysis to investigate the links between short-term exposure to various air pollutants and the frequency of ED visits for SIHD24. Considering that the daily ED visits exhibited a quasi-Poisson distribution, we employed an overdispersed generalized additive model (GAM) to analyze the data. The model included the average temperature for the current day (the degree of freedom, df = 6), relative humidity for the current day (df = 3), calendar time (df = 8/year), and adjustment for day of the week (DOW) and public holiday (PH)24,26. The main model is described as follow:
where E(Yt) represents the expected ED visits for CHD on day t, Zt refers to various air pollutants concentration on day t, time refers to calendar time which was used to control unmeasured long-term trend, temperature and relative humidity refers to average temperature and relative humidity of the current day, respectively, DOW and PH are dummy variables, β is the coefficient for Zt, ns refers to a natural cubic smooth function, df refers to the degree of freedom, and α is the intercept. We can calculate the Relative Risk by taking logarithm of β.
The main model investigated both single-day lags from the current day (lag0) to five days before (lag5), as well as moving average exposure from the current day to the previous 1 to 3 days (lag01 to lag03). The optimal lag periods were determined based on the maximum estimates and minimum values of p27. The estimates were reported as excess risk (ER) with a corresponding 95% confidence interval (95% CI). These values represent the percentage change in morbidity associated with a 10-unit increase in different air pollutants28.
Afterwards, we excluded the extremely concentrations of air pollutants and then the association between different concentrations of air pollutants and the number of ED visits for SIHD was illustrated using an exposure-response curve. This curve was plotted using a methodology previously reported24,29. In the sensitivity analyses, we utilized the raw data to reconstruct the curve.
Subgroup analyses were performed by categorizing the ED visits according to age groups (<50, 50–59, 60–69, 70–79, and ≥80 years), gender (male and female) and season (warm season: April to September; cold season: October to March). In the sensitivity analyses, we varied the df for calendar time from 4 to 16, for average temperature from 4 to 8, and for relative humidity from 3 to 5. Additionally, we conducted two-pollutant models by incorporating air pollutants that had a Spearman's correlation coefficient below 0.7 (Tables S1–S6) in the main model separately. To control a longer time period of ambient temperature, we used the moving average temperature of the current day to the three previous days (temp03), the seven previous days (temp07), and the fourteen previous days (temp014) as substitutes for the average temperature of the present day in the analysis24.
R software (version 4.2.3) was used for all analyses, and an association was considered statistically significant when two-sided p < 0.05.
Ethical approval
This study was approved by the Ethics Committee of Shanghai University, all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research/review board (IRB)-IRB Number: ECSHU 2023-018. Study participation only required verbal consent, which was obtained from all subjects who participated in this study and was approved by the ethics committee.
Results
Description of the study population
The time-series analysis of ED visits revealed that there were small fluctuations in the number of ED visits for SIHD throughout the study period, with a weak seasonal trend (Fig. S2). A total of 18,241 ED visits for SIHD were included (Table 1). The median number of daily ED visits for SIHD varied across different age groups, genders, and seasons (P < 0.001). Patients aged 50 years and older accounted for 95.5% of the visits, with females outnumbering males (11,680 females vs. 6561 males). Additionally, more SIHD patients were visited during the cold season (52.1%).
The time-series patterns of various air pollutants during the study period are displayed in Fig. S3, while the concentrations of different air pollutants, temperature, and relative humidity are presented in Table 2. Generally, all air pollutants exhibit noticeable seasonal trends. The concentration trends of O3-8 h were higher in the warm season, while other air pollutants showed higher concentrations in the cold season. The daily mean concentrations of NO2, PM2.5, PM10, SO2, O3-8 h and CO were 41.40 μg/m3 (SD =19.27; range: 5.24 to 140.08 μg/m3), 44.15 μg/m3 (SD = 32.33; range: 5.33 to 460.98 μg/ m3), 61.77 μg/m3 (SD =39.22; range: 6.96 to 487.96 μg/m3), 13.12 μg/m3 (SD = 9.97; range: 4.00 to 106.90 μg/m3), 93.12 μg/ m3 (SD = 43.15; range: 6.18 to 280.00 μg/m3) and 0.78 mg/ m3 (SD = 0.88; range: 0.31 to 19.92 mg/m3), respectively. The daily average concentrations of NO2, PM2.5 and PM10 exceeded the concentration limits set by the “WHO Air quality guidelines”30. In addition, the average daily temperature was 17.52 °C (SD = 8.66; range: -6.10 to 35.00 °C), and the relative humidity was 73.08% (SD = 12.60%; range: 28.00 to 99.00%).
Correlation between air pollution and meteorology
Spearman’s correlations among air pollutants and meteorological factors are presented in Fig. S4 and Table S7. PM2.5 was strongly associated with PM10 (Spearman correlation coefficient, r = 0.88, p < 0.001); NO2 exhibited a moderate association with PM2.5 (r = 0.62, p = 0.004), PM10 (r =0.60, p = 0.008), SO2 (r = 0.44, p = 0.021) and mean temperature (r = 0.42, p = 0.004). SO2 demonstrated a moderate association with PM2.5 (r = 0.68, p = 0.001), PM10 (r =0.66, p = 0.002) and mean temperature (r = 0.36, p = 0.01). Mean temperature exhibited a weak association with PM2.5 (r = 0.29, p = 0.011) and PM10 (r = 0.24, p = 0.034). Meanwhile, the associations between O3-8 h, CO, relative humidity, and other air pollutants, as well as daily mean temperature, were found to be insignificant.
Relationship between air pollutants and SIHD
The associations between different ambient air pollutants and ED visits for SIHD are presented in Fig. 1. Overall, our findings suggest that there is an elevated risk of ED visits for SIHD with 10 units increase in various ambient air pollutants, such as PM2.5, PM10, NO2, SO2, and CO, as well as a decrease in the concentration of O3-8 h. We observed significant associations between PM2.5 and the number of ED visits for SIHD at lag0, with an ER of 0.58% (95% CI: 0.01%, 1.14%) for every 10 μg/m3 increase in PM2.5. PM10 was also significantly associated with the number of ED visits for SIHD at lag0 and lag5, and the estimates were larger at lag0, with an ER for PM10 of 0.50% (95% CI 0.02%, 0.98%) for every 10 μg/m3 increase. NO2 showed significant positive associations with the number of ED visits for SIHD at lag0 to lag3, lag5, and lag01 to lag03, with the largest effect observed at lag03. The ER for NO2 was 2.82% (95% CI 1.47%, 4.18%) for every 10 μg/m3 increase at lag03. Similarly, significant positive associations were found between SO2 and SIHD at lag0 to lag2, lag5, and lag01 to lag03, with the largest effect observed at lag03. The ER for SO2 was 5.02% (95% CI 2.23%, 7.88%) for every 10 μg/m3 increase. CO was significantly associated with the number of ED visits for SIHD at lag 3 to lag 5, with the largest effect observed at lag 4. The ER for CO was 25.50% (95% CI 6.36%, 48.08%) for each 10 mg/m3 increase at lag 4. However, O3-8 h showed a significant association with the number of ED visits for SIHD only at lag4, with an ER of -0.48% (95% CI − 0.95%, 0.00%) for every 10 μg/m3 decrease in O3-8 h. Therefore, in our subsequent analyses, we focused on the effects of PM2.5 (lag0), PM10 (lag0), NO2 (lag03), SO2 (lag03), CO (lag4) and O3-8 h (lag4).
ER (%) and 95% CI of ED visits for SIHD were analyzed in relation to each 10 units increase in various ambient air pollutants. (a) PM2.5 (μg/m3); (b) PM10 (μg/m3); (c) NO2 (μg/m3); (d) SO2 (μg/m3); (e) O3-8 h (μg/m3); (f) CO (mg/m3).The ER and corresponding 95% CI were derived from an overdispersed generalized additive model, with calendar time, weather conditions, day of the week (DOW) and public holiday (PH) controlled. #indicates that excess risk (%) and 95% CI of ED visits with SIHD were associated with a 10 mg/m3 increase in CO concentrations.
Specifically, there were appropriately linear associations between air pollution (PM2.5, PM10, NO2 and SO2) and the number of ED visits for SIHD, indicating that higher concentrations of these pollutants corresponded to a greater number of ED visits. No discernible thresholds were observed as the concentrations of these pollutants increased. Regarding O3-8 h and CO, we observed a slight initial increase in the number of ED visits for SIHD, reaching a peak at specific air pollution concentrations (O3-8 h = 118.94 μg/m3, CO = 0.76 mg/m3), followed by a subsequent decline (Fig. 2). However, in sensitivity analyses, the dose-exposure plot of PM10 and CO exhibits a noticeable change in trend, which may be due to extremely high concentrations of certain air pollutants (Fig. S5).
Exposure-response curve for the association between various ambient air pollutants and ED visits for SIHD (Excluding extreme values). The line represents the point estimates, and the shading indicates corresponding 95% CIs, which were derived from an overdispersed generalized additive model, with calendar time, weather conditions, day of the week (DOW) and public holiday (PH) controlled. (a) PM2.5 (lag0); (b) PM10 (lag0); (c) NO2 (lag03); (d) SO2 (lag03); (e) O3-8 h (lag4); (f) CO (lag4).
Stratified analyses of the association of various ambient air pollutants and SIHD
The results of the stratified analyses are summarized in Table 3. When the data were divided by gender, it was observed that the associations between air pollutants and SIHD were weaker in females than in males. In the age-specific analyses, it was predominantly observed that significant relationships between various air pollutants and SIHD were present in patients aged 60-69 years. In the season-stratified analysis, we observed that the effects of air pollutants on PM2.5 and O3-8 h remained almost unchanged. The effect estimates were significantly higher during the warm period when analyzing NO2, SO2 and CO, but the effect was found to be insignificant for CO. In contrast, the effect estimates of PM10 were larger during the cold period, but we were unable to detect significant effects during the warm period. For example, the ERs with 95% CIs for the associations of each 10 μg/m3 increase in SO2 in the warm season and cold season were 14.73% (95% CI 5.44%, 24.84%) and 3.67% (95% CI 0.47%, 6.98%), respectively.
Sensitivity analyses
Tables S1–S6 show robust results in the two-pollutant models of various air pollutants. Generally, the ER for associations between air pollution (PM2.5 and PM10) and the number of ED visits for SIHD increased and remained significant only when O3-8 h was added in the mode. The ER for associations between air pollution (NO2, SO2 and CO) and the number of ED visits for SIHD remained significant even after adjusting for other pollutants. However, the results became insignificant for O3-8 h. For example, the estimates for the ERs of each 10 μg/m3 increase in NO2 slightly decreased to 2.73% (95% CI 1.20%, 4.29%), 2.77% (95% CI 1.22%, 4.34%) and 2.61% (95% CI 1.21%, 4.03%) when PM2.5, PM10 and SO2 were adjusted, respectively. However, they increased to 2.99% (95% CI 1.63%, 4.36%) and 3.02% (95% CI 1.66%, 4.41%) when O3-8 h and CO were adjusted, respectively.
When the df of calendar time (from 4 to 16) and temperature (from 4 to 8) were changed, the estimates showed slight variations (Tables S8, 9). For NO2, SO2 and CO, the results remained robust when the relative humidity (from 3 to 5) was changed or when a longer time period of ambient temperature was controlled (Tables S10, S11). However, because the raw values were already close to the critical value, the results became insignificant for PM2.5, PM10 and O3-8 h (Tables S10, S11).
Discussion
To the best of our knowledge, this is the first study to simultaneously explore the associations of six types of air pollution (PM2.5, PM10, NO2, SO2, CO and O3-8 h) with SIHD. Our results revealed significant variations in these associations depending on the type of air pollutant, with the strongest effects observed for CO, followed by SO2 and NO2. PM2.5, PM10 and O3-8 h showed weak associations with SIHD. Furthermore, the association between various air pollutants and the morbidity of acute SIHD exhibited variations depending on gender, age, and season. Taken together, our results may contribute to a better understanding of the short-term effects of various types of air pollution on acute SIHD.
Few previous studies have explored the relationships between various types of air pollution and ED visits for SIHD15,16,17,18,19,20. We found that the association between air pollution and SIHD varied greatly depending on the specific type of air pollution. For instance, a time-series study conducted in Lima, Peru revealed a significant association between elevated PM2.5 levels and an increase in the number of ED visits for IHD at lag020. Similarly, a study in Shanghai, China, which included five clinical subtypes of CHD, reported that a 10 μg/m3 increase in present-day PM10 concentrations was associated with a respective increase of 0.80% (95% CI 0.22%, 1.37%) in ED visits for ischemic cardiomyopathy18. However, other studies have shown a positive correlation between PM10 concentration and the number of ED visits for IHD, but the effect was not statistically significant15,19. Our study supported the positive association between particulate air pollutants (PM2.5, PM10) and the number of ED visits for SIHD. Particulate air pollution has been associated with adverse cardiac effects through various biological mechanisms, including enhanced coagulation/thrombosis, a propensity for arrhythmias, acute arterial vasoconstriction, systemic inflammatory responses, and the chronic promotion of atherosclerosis31.
In terms of NO2, a previous study conducted in Montreal, Canada reported that it contributes to an increased number of ED visits for IHD, with an ER of 5.9% (95% CI 2.1–9.9)16. In contrast, a study by Juan Xie et al.18 found that there was no significant association between NO2 exposure and the number of ED visits for IHD. Our study provided evidence supporting a positive correlation between NO2 levels and the number of ED visits for SIHD. The reason for this difference remains uncertain, but it may be attributed to variations in ambient air quality across different regions.
Previous studies have indicated a potential relationship between IHD mortality and CO exposure32,33. The study by M. Szyszkowicz 16 showed that higher levels of CO were associated with an increased number of ED visits for IHD, with an ER of 5.4% (95% CI 2.3–8.5). Similarly, two previous studies have also reported a positive association between CO and ED visits for IHD, demonstrating a statistically significant effect15,17. In our study, we also demonstrated a significant positive association between CO exposure and the number of ED visits for SIHD. The mechanism may involve CO replacing oxygen in the bloodstream, which could potentially impact cardiovascular disease.
Notably, in previous studies, a significant association was found between SO215,18 concentrations and ED visits for IHD. However, the effects were not statistically significant. Our study demonstrated a significant association between elevated SO2 levels and the number of ED visits for SIHD. It is imperative to conduct more research to better understand which pathways may be responsible for the effect of SO2 on SIHD.
Interestingly, a previous study has found a positive correlation between O315 levels and ED visits for IHD with no significant. On the contrary, we found a negative correlation between elevated O3-8 h levels and the number of ED visits for SIHD. Except for regional differences, this discrepancy is potentially linked to O3-8 h levels well below the air quality standards recommended by the WHO in our study.
The observed association between various air pollutants and cardiovascular events may be partially explained by biological mechanisms. First, we used ED visits, as the outcome primarily reflects acute attacks or exacerbations of SIHD. It is worth noting that SIHD is a leading cause of death in the United States and many other countries4. Second, several researchers have investigated the association between PMs and CHD, as well as the underlying mechanisms. They found that exposure to PM2.5 can damage vascular endothelial cells (ECs), activate inflammatory responses, lead to disseminated intravascular coagulation (DIC), and induce lipid metabolic disorders34,35,36. Moreover, previous studies have demonstrated that various air pollutants, including PM2.5, PM10, NO2, SO2, O3, and CO, can contribute to oxidative stress pathways and cardiac outcomes. These outcomes may include endothelial dysfunction, atherosclerosis, procoagulant changes, hypertension, and cardiac dysfunction, either independently or through interpollutant interactions37. However, the specific mechanisms underlying the impact of various air pollutants on SIHD are still not fully understood. Further research is necessary to gain a better understanding of the potential pathways through which air pollutants affect SIHD. This knowledge will be valuable in guiding the development of effective public health policies.
Certain populations appear to be particularly susceptible to the detrimental effects of air pollution. Haikerwal, A. et al. study38 conducted a study that revealed that older adults (aged ≥65 years) and females have a higher risk of IHD. The results were similar to our study, in which over 95% of patients with SIHD were over 50 years old and more than half of them were female. A review also reported that both females and older individuals appear to be more susceptible to the effects of environmental stressors39. Given that atherosclerosis (often asymptomatic) is a common comorbidity in older individuals, exposure to high levels of air pollution may increase the risk of coronary episodes. In addition, females typically have a longer lifespan than males and constitute a majority of the aging population40.
Our results indicated that a higher number of ED visits for SIHD occurred during the cold season, aligning with previous studies32,41,42. This can be attributed to the potential that cold temperatures to raise both systolic and diastolic blood pressure, leading to increased oxygen consumption by the heart41. In addition, the subgroup analysis indicated a more pronounced effect of PM10 on SIHD during the cold season, which was in general accordance with previous studies12,18. Contrary to previous studies15,18,43, our findings indicated that the impact of NO2, SO2, and CO on SIHD was more pronounced in the warm season. The increased risk of cardiovascular disease can be attributed to a combination of factors, including extreme high or low temperatures6,7, variations in air pollution mixtures and levels, and population exposure patterns in different seasons. Further investigations are needed to explore the influence of meteorological factors on the relationship between air pollution and SIHD, as well as the underlying mechanisms involved. Moreover, it is crucial to pay more attention to the high levels of PM10 during the cold season and the elevated levels of NO2, SO2, and CO during the warm season in Shanghai.
As mentioned above, cardiovascular disease, especially CHD, imposes a significant burden on both health and society. A modeling study conducted in Australia highlighted the potential benefits of preventing new cases of CHD. If achieved during the 2020–2029 period, it could save over 8000 years of life and gain 104,000 ‘productivity-adjusted life years’, equivalent to a gain of nearly $14.8 billion in GDP44. Our study further emphasized the detrimental effects of various air pollutants (PM2.5, PM10, SO2, NO2, and CO) on SIHD, underscoring the importance of implementing preventive measures to mitigate SIHD. Firstly, this finding underscores the importance of controlling air pollution. We discovered a positive correlation between air pollutant concentrations and the number of ED visits for SIHD (Fig. 2). Secondly, based on our findings, we recommend implementing specific measures during periods of high air pollution, such as wearing masks and reducing outdoor activities, especially for individuals with SIHD in severe weather conditions.
Our study has several limitations. First, there is the presence of ecological bias inherent in time-series studies. We relied on average values of air pollution data from fixed air-quality monitors instead of individual exposure measurements. This approach may introduce a bias known as the ecological fallacy in the assessment of air pollution exposure. However, previous studies have consistently shown that this type of measurement error tends to underestimate the true risk and lead to conservative estimates of the association45,46. Qiu et al.’s study47 has shown that this type of misclassification has minimal impact on the results. Second, our study was conducted at a single center and focused on a localized population, which may limit the generalizability of our findings. To address this limitation, we conducted a series of sensitivity analyses over a longer period to enhance the reliability of our findings.
Conclusion
Our study suggests that short-term exposure to various air pollutants (NO2, PM2.5, PM10, SO2 and CO) may act as triggers for inducing SIHD. When the concentration of O3-8 h was lower than the threshold recommended by the WHO, exposure to O3-8 h was associated with a slightly decreased risk of SIHD. We observed varying associations between different air pollutants and the number of ED visits for SIHD, with variations based on gender, age, and season. By identifying the specific thresholds for each pollutant and understanding their corresponding health effects, appropriate measures can be implemented to mitigate the risks associated with air pollution and promote better cardiovascular health.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files. The raw data that supporting the findings of this study are available on GitHub at https://github.com/Zhangzhengrenhe163/SIHD.
References
Qi, J., Han, W., Zhong, N., Gou, Q. & Sun, C. Integrated analysis of miRNA-mRNA regulatory network and functional verification of miR-338-3p in coronary heart disease. Funct. Integr. Genom. 23, 16. https://doi.org/10.1007/s10142-022-00941-w (2022).
Shaya, G. E., Leucker, T. M., Jones, S. R., Martin, S. S. & Toth, P. P. Coronary heart disease risk: Low-density lipoprotein and beyond. Trends Cardiovasc. Med. 32, 181–194. https://doi.org/10.1016/j.tcm.2021.04.002 (2022).
Katz, D. H. & Gavin, M. C. Handbook of Inpatient Cardiology 19–39 (Springer International Publishing, 2020).
Katz, D. & Gavin, M. C. Stable ischemic heart disease. Ann. Intern. Med. 171, Itc17–Itc32. https://doi.org/10.7326/aitc201908060 (2019).
Pope, C. A. 3rd. et al. Ischemic heart disease events triggered by short-term exposure to fine particulate air pollution. Circulation 114, 2443–2448. https://doi.org/10.1161/CIRCULATIONAHA.106.636977 (2006).
Luan, G., Yin, P., Li, T., Wang, L. & Zhou, M. The years of life lost on cardiovascular disease attributable to ambient temperature in China. Sci. Rep. 7, 13531. https://doi.org/10.1038/s41598-017-13225-2 (2017).
Han, J. et al. The impact of temperature extremes on mortality: A time-series study in Jinan China. BMJ Open 7, e014741. https://doi.org/10.1136/bmjopen-2016-014741 (2017).
Gonçalves, F. L., Braun, S., Dias, P. L. & Sharovsky, R. Influences of the weather and air pollutants on cardiovascular disease in the metropolitan area of São Paulo. Environ. Res. 104, 275–281. https://doi.org/10.1016/j.envres.2007.01.004 (2007).
Bourdrel, T., Bind, M. A., Béjot, Y., Morel, O. & Argacha, J. F. Cardiovascular effects of air pollution. Arch. Cardiovasc. Dis. 110, 634–642. https://doi.org/10.1016/j.acvd.2017.05.003 (2017).
Rajagopalan, S., Al-Kindi, S. G. & Brook, R. D. Air pollution and cardiovascular disease: JACC state-of-the-art review. J. Am. Coll. Cardiol. 72, 2054–2070. https://doi.org/10.1016/j.jacc.2018.07.099 (2018).
Soleimani, Z., Darvishi Boloorani, A., Khalifeh, R., Griffin, D. W. & Mesdaghinia, A. Short-term effects of ambient air pollution and cardiovascular events in Shiraz, Iran, 2009 to 2015. Environ. Sci. Pollut. Res. Int. 26, 6359–6367. https://doi.org/10.1007/s11356-018-3952-4 (2019).
Ye, X. et al. Acute effects of particulate air pollution on the incidence of coronary heart disease in Shanghai, China. PLoS One 11, e0151119. https://doi.org/10.1371/journal.pone.0151119 (2016).
Pan, F., Xu, W., Li, J., Huang, Z. & Shu, Q. Trends in the disease burden of congenital heart disease in China over the past three decades. Zhejiang Da Xue Xue Bao Yi Xue Ban 51, 267–277. https://doi.org/10.3724/zdxbyxb-2022-0072 (2022).
https://wsjkw.sh.gov.cn/tjsj2/20220704/a540b90305ae4c54bf870b3804c6f84c.html. (Accessed 31 May 2023).
Lin, C. A. et al. Association between air pollution and ischemic cardiovascular emergency room visits. Environ. Res. 92, 57–63. https://doi.org/10.1016/s0013-9351(02)00054-3 (2003).
Szyszkowicz, M. Air pollution and emergency department visits for ischemic heart disease in Montreal, Canada. Int. J. Occup. Med. Environ. Health 20, 167–173. https://doi.org/10.2478/v10001-007-0015-3 (2007).
Bell, M. L., Peng, R. D., Dominici, F. & Samet, J. M. Emergency hospital admissions for cardiovascular diseases and ambient levels of carbon monoxide: Results for 126 United States urban counties, 1999–2005. Circulation 120, 949–955. https://doi.org/10.1161/circulationaha.109.851113 (2009).
Xie, J., He, M. & Zhu, W. Acute effects of outdoor air pollution on emergency department visits due to five clinical subtypes of coronary heart diseases in shanghai, China. J. Epidemiol. 24, 452–459. https://doi.org/10.2188/jea.je20140044 (2014).
Sohn, J. et al. Susceptibility to ambient particulate matter on emergency care utilization for ischemic heart disease in Seoul, Korea. Environ. Sci. Pollut. Res. Int. 23, 19432–19439. https://doi.org/10.1007/s11356-016-7144-9 (2016).
Tapia, V. et al. Time-series analysis of ambient PM(2.5) and cardiorespiratory emergency room visits in Lima, Peru during 2010–2016. J. Expo. Sci. Environ. Epidemiol. 30, 680–688. https://doi.org/10.1038/s41370-019-0189-3 (2020).
Jiang, Y., Jiang, S. & Shi, T. Comparative study on the cooling effects of green space patterns in waterfront build-up blocks: An experience from Shanghai. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17228684 (2020).
Lai, Z. et al. Exploring the spatial heterogeneity of residents’ marginal willingness to pay for clean air in Shanghai. Front. Public Health https://doi.org/10.3389/fpubh.2021.791575 (2021).
Wang, X. et al. Association between air temperature and the incidence of acute coronary heart disease in Northeast China. Clin. Interv. Aging 15, 47–52. https://doi.org/10.2147/CIA.S235941 (2020).
Guo, H. et al. Short-term exposure to nitrogen dioxide and outpatient visits for cause-specific conjunctivitis: A time-series study in Jinan, China. Atmos. Environ. 247, 118211. https://doi.org/10.1016/j.atmosenv.2021.118211 (2021).
Han, T. et al. Baosteel emission control significantly benefited air quality in Shanghai. J. Environ. Sci. (China) 71, 127–135. https://doi.org/10.1016/j.jes.2018.01.014 (2018).
Song, J. et al. Short-term exposure to nitrogen dioxide pollution and the risk of eye and adnexa diseases in Xinxiang, China. Atmos. Environ. 218, 117001 (2019).
Fu, Q. et al. Air pollution and outpatient visits for conjunctivitis: A case-crossover study in Hangzhou, China. Environ. Pollut. 231, 1344–1350. https://doi.org/10.1016/j.envpol.2017.08.109 (2017).
Ai, S. et al. Hourly associations between ambient air pollution and emergency ambulance calls in one central Chinese city: Implications for hourly air quality standards. Sci. Total Environ. 696, 133956. https://doi.org/10.1016/j.scitotenv.2019.133956 (2019).
Zeng, Q. et al. The association between inhalable particulate matter and YLL caused by COPD in a typical city in northern China. Atmos. Environ. 172, 26–31 (2018).
World Health Organization. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. Geneva: World Health Organization (2021).
Brook, R. D. et al. Air pollution and cardiovascular disease: A statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 109, 2655–2671. https://doi.org/10.1161/01.Cir.0000128587.30041.C8 (2004).
Zanobetti, A. & Schwartz, J. Air pollution and emergency admissions in Boston, MA. J. Epidemiol. Community Health 60, 890–895. https://doi.org/10.1136/jech.2005.039834 (2006).
Koskela, R. S., Mutanen, P., Sorsa, J. A. & Klockars, M. Factors predictive of ischemic heart disease mortality in foundry workers exposed to carbon monoxide. Am. J. Epidemiol. 152, 628–632. https://doi.org/10.1093/aje/152.7.628 (2000).
Yang, L. et al. Adverse effects of PM (2.5) on cardiovascular diseases. Rev. Environ. Health 37, 71–80. https://doi.org/10.1515/reveh-2020-0155 (2022).
Liang, S. et al. The critical role of endothelial function in fine particulate matter-induced atherosclerosis. Part. Fibre Toxicol. 17, 61. https://doi.org/10.1186/s12989-020-00391-x (2020).
Miller, M. R. The role of oxidative stress in the cardiovascular actions of particulate air pollution. Biochem. Soc. Trans. 42, 1006–1011. https://doi.org/10.1042/bst20140090 (2014).
Kelly, F. J. & Fussell, J. C. Role of oxidative stress in cardiovascular disease outcomes following exposure to ambient air pollution. Free Radic. Biol. Med. 110, 345–367. https://doi.org/10.1016/j.freeradbiomed.2017.06.019 (2017).
Ge, E. et al. Differential effects of size-specific particulate matter on emergency department visits for respiratory and cardiovascular diseases in Guangzhou, China. Environ. Pollut. 243, 336–345. https://doi.org/10.1016/j.envpol.2018.08.068 (2018).
Bruno, R. M. et al. Environmental factors and hypertension. Curr. Pharm. Des. 23, 3239–3246. https://doi.org/10.2174/1381612823666170321162233 (2017).
Tsang, T. S., Barnes, M. E., Gersh, B. J. & Hayes, S. N. Risks of coronary heart disease in women: Current understanding and evolving concepts. Mayo Clin. Proc. 75, 1289–1303. https://doi.org/10.4065/75.12.1289 (2000).
Pell, J. P. & Cobbe, S. M. Seasonal variations in coronary heart disease. QJM 92, 689–696. https://doi.org/10.1093/qjmed/92.12.689 (1999).
Zanobetti, A. & Schwartz, J. The effect of particulate air pollution on emergency admissions for myocardial infarction: A multicity case-crossover analysis. Environ. Health Perspect. 113, 978–982. https://doi.org/10.1289/ehp.7550 (2005).
Feng, W. et al. Short-term PM(10) and emergency department admissions for selective cardiovascular and respiratory diseases in Beijing, China. Sci. Total Environ. 657, 213–221. https://doi.org/10.1016/j.scitotenv.2018.12.066 (2019).
Savira, F. et al. The impact of coronary heart disease prevention on work productivity: A 10-year analysis. Eur. J. Prev. Cardiol. 28, 418–425. https://doi.org/10.1093/eurjpc/zwaa037 (2021).
Dominici, F., Zeger, S. L. & Samet, J. M. A measurement error model for time-series studies of air pollution and mortality. Biostatistics 1, 157–175. https://doi.org/10.1093/biostatistics/1.2.157 (2000).
Szyszkowicz, M., Kousha, T. & Castner, J. Air pollution and emergency department visits for conjunctivitis: A case-crossover study. Int. J. Occup. Med. Environ. Health 29, 381–393. https://doi.org/10.13075/ijomeh.1896.00442 (2016).
Qiu, H., Pun, V. C. & Tian, L. Short-term effects of fine and coarse particles on deaths in Hong Kong elderly population: An analysis of mortality displacement. Environ. Pollut. 241, 148–154. https://doi.org/10.1016/j.envpol.2018.05.056 (2018).
Acknowledgements
We thank the staff members at Baoshan District Renhe Hospital for assisting with the field data collection.
Funding
This work was supported by the Young and Middle-aged Excellent Talent Training Program of Renhe Hospital in Baoshan District, Shanghai [grant No. BSRHYX-2020-04].
Author information
Authors and Affiliations
Contributions
Y.Z.: Conceptualization, methodology, investigation, writing—original draft, formal analysis. Y.J.: Formal analysis, investigation, writing—review & editing. Z.Z.: Investigation, Resources, Funding acquisition, Writing—review &editing. All authors contributed to the review and revision, approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, Y., Jin, Y. & Zhang, Z. Short-term exposure to various ambient air pollutants and emergency department visits for cause-stable ischemic heart disease: a time-series study in Shanghai, China. Sci Rep 13, 16989 (2023). https://doi.org/10.1038/s41598-023-44321-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-44321-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.