Abstract
While previous studies on navigated total hip replacement (nTHA) focused on acetabular component positioning, we compared the results of nTHA with conventional total hip replacement (cTHA) in respect of changes in leg length and hip offset. In a single-center study results radiographic parameters of patients with unilateral THA were included. Data were retrospectively analyzed from computer navigation data and radiographs. Analysis concentrated on the discrepancy in leg length (LLD) and hip offset (OSD) between the affected and unaffected hip. The effect of the procedure was defined as the difference between postoperative and preoperative LLD and OSD values in each group. 2332 patients were analyzed. Both nTHA and cTHA were effective in restoring LLD and OSD by reducing the preoperative value significantly (p < 0.001). Regarding changes in LLD, no statistical difference between nTHA and cTHA could be found. Changes in OSD nTHA was a slightly more effective than cTHA (− 2.06 ± 6.00 mm vs. − 1.50 ± 5.35 mm; p < 0.05). Both navigated and conventional THA were successful in reconstruction of leg length and hip offset, while postoperative offset discrepancy was significantly lower in the navigated group at the cost of longer operation times. If these results are clinically relevant further investigation is needed.
Similar content being viewed by others
Introduction
Destruction of the hip joint cartilage caused by osteoarthritis leads to the alternation of the physiological center of rotation (COR) of the femoral head and contributes the impairment of hip joint function. Therefore, achieving proper biomechanics by reconstruction of the COR should be the aim of all total hip arthroplasties (THA)1.
Critical to restoring the COR is proper reconstruction of leg length and hip offset2. Leg length discrepancies (LLDs) after THA have been associated with unphysiological force transmission, hip instability, ipsilateral knee pain, sciatic nerve palsy, aseptic loosening, and early revision surgery. Besides resulting in unhappy patients, LLDs are often perceived by the patient and affects functional outcome3. Unphysiological postoperative LLDs are also a main cause for malpractice liability lawsuits after THA in the United4. Failure to restore hip offset postoperatively may lead to hip instability, impingement, and polyethylene wear5,6.
Hip offset comprises two components: acetabular offset and femoral offset. Acetabular offset affects hip stability, range of motion, and soft tissue tension, while femoral offset is dictated by the configuration of the stem and affects leg length and overall limb alignment7,8.
Regarding an optimal alignment of the acetabular component Lewinnek et al.9 recommended an inclination angle of 40° ± 10° and an anteversion angle of 15° ± 10° as a safe range for acetabular alignment in THA. Freehand techniques and the use of mechanical guides have been used in the past to ensure target values, but there has been a desire for even greater accuracy.
Imageless computer navigation in THA has emerged as a potential method of restoring limb length and acetabular offset with much greater accuracy than conventional instrumentation10. With the use of computer navigation, the cup position, femoral stem position, leg length and hip offset can be tracked intraoperatively with high precision. Consequently, computer navigation has been associated with a reduced rate of revision for dislocation following THA. Furthermore, in the component combinations most commonly used with navigation there was also a reduction in the rate of all-cause revision1,11,12,13.
Previous radiological studies mainly focused on the acetabular component and the precision of the measured anteversion and inclination, while the number of studies focusing on the leg length and hip offset reconstruction in imageless computer navigated total hip arthroplasty remains low3,14,15,16. Therefore, we compared the results of navigated (nTHA) with conventional total hip replacement (cTHA) in respect to leg length and hip offset reconstruction.
Material and methods
In a retrospective single-center study collected data of patients with THA performed in 2019 and 2021 were evaluated and was approved by the institutional review board of our institution. Data were collected as a normal part of patients’ diagnosis and treatment as recorded in case notes, the departmental proprietary database, computer navigation data and radiographic images.
Two groups were reviewed, one group included all patients operated with navigated THA in 2021, and a control group of all patients operated with conventional THA operated in 2019. Due to the limited number of elective operations during the first lockdowns of CoV19-Pandemic patient data from 2020 could not be analyzed. A total of 3915 patients underwent nTHA or cTHA in the respective period of time. These operations were performed according to institutional standards; in the navigation group, surgery was performed using the Intellijoint HIP® imageless navigation device (IntellijointSurgical Inc., Kitchener, Ontario, Canada).
In these patients AP pelvic radiographs were performed before surgery and six weeks after in standard manner, with a marker of known diameter to account for magnification while postoperative radiographs were corrected for magnification using the acetabular liner diameter. The patients were supine position with x-ray beam centered over pubic symphysis with lower limbs placed in internal rotation with the big toes touching each other and patella facing forward. In this view the femoral neck could be viewed in full profile.
In the analysis only patients with unilateral hip disease were included. Excluded were patients with bilateral hip osteoarthritis, bilateral THA, inadequate pelvic radiographs, and revision surgeries as well as additional inserted implants such as cables and plates. All these patients had pre- and postoperative standard AP pelvic radiographs according to the institutional standard protocol.
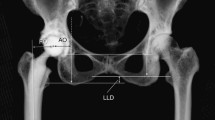
To calculate leg length (LL) the Ranawat technique was used10,17,18 (Fig. 1). The trans teardrop line was defined as the standard line. The perpendicular distance from this horizontal line to the apex of the lesser trochanter was measured and displayed in the Picture Archiving Communications System PACS templating system. The difference in between the affected und the contralateral unaffected hip was termed hip length discrepancy (HLD), which was determined in each patient pre- and postoperatively.
Leg length (LL) was measured with the Ranawat technique and hip offset (OS) was calculated as the sum of femoral and acetabular offset. Analysis of radiologic images concentrated on the discrepancy in leg length (LLD) and hip offset (OSD) between the affected and unaffected hip. (O: femoral offset, A: acetabular offset, Diff: LLD).
Hip offset (OS) was calculated as the sum of femoral and acetabular offsets10 Fig. 1). Femoral offset was defined as the perpendicular distance from the center of rotation of the femoral head to the line of action of the abductor muscles. Acetabular offset is the perpendicular distance from the center of rotation of the femoral head to the vertical trans-teardrop line. The difference in OS between the affected und the contralateral unaffected hip was termed offset discrepancy (OSD), which was determined in each patient pre- and postoperatively.
Radiographic cup anteversion was determined in shoot-through lateral radiographs by measuring the angle between the transverse axis and the acetabular opening10,19. For technical reasons shoot-through lateral radiographs were only taken in 861 patients. Therefore, anteversion was only determined in 454 patients with cTHA and 407 patients with nTHA.
All radiographs were accessed on Kodak PACS (Eastman Kodak Company, 10.1_SP1, 2006). All the radiographic measurements were performed retrospectively by a single author, who was not involved in patient care or surgery, using Orthoview Digital Planning Software system (Orthoview LLC) on PACS. To account inter-rater and intra-rater reliability 60 radiographs were randomly selected and the author (RL) measured them twice 2 weeks apart and they were also measured by another author independently (AO).
For statistical analysis continuous variables were reported as mean and standard deviation and categorial variables frequency and proportion. Cohorts were compared using Welch two sample t test for continuous data and Pearson Chi squared for categorical data. Levene's test using median as the center was used to compare variances between cohorts. Multivariable linear regression was conducted to investigate association of LLD and Offset discrepancy at postop with BMI and operative time. Significance was established at alpha 0.05.
The Institutional Review Board of the Hospital for Special Surgery approved the study protocol before data collection was started (IRB Number: 2022–0126).
All patients gave consent to treatment according to institutional guidelines and to anonymized assessment of clinical data and treatment outcome. This was a retrospective trial. Therefore, the Institutional Review Board waived the requirement to obtain distinct written informed consent from the patients.
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the institutional review board of the Hospital for Special Surgery (IRB Number: 2022-0126).
Informed consent
All patients gave consent to treatment according to institutional guidelines and to anonymized assessment of clinical data and treatment outcome. This was a retrospective trial. Therefore, the Institutional Review Board of the Hospital of Special Surgery waived the requirement to obtain distinct written informed consent from the patients.
Results
Our final analysis included 2332 patients: 1174 patients with cTHA and 1158 patients with nTHA (Table 1). A total of 1583 patients were excluded due to the predefined exclusion criteria.
Due These two groups did not differ significantly in respect of BMI and Charlson Comorbidity index. However, in the nTHA group there were significantly more male patients than in the cTHA group (49.8% vs. 44.5; p = 0.012) and nTHA patients were also significantly younger (61.65 ± 9.79 vs. 63.04 ± 10.37; p = 000.9) Based on their ASA scores, patients of the nTHA appeared less medically compromised than patients with cTHA; ASA 3–4: cTHA n = 182 (15.3%) vs. nTHA143 (12.2%), p < 0.05.
Right sided THA operations were performed in 606 patients (52.3%) of nTHA group and in 643 patients (54.8%) of cTHA group (p = 0.255). Duration of operation in the nTHA group was significantly longer than in cTHA group (89.21 ± 24.63 min vs. 79.88 ± 23.29 min; p < 0.001).
Results of the analysis of the pelvic radiographs of the two groups are listed in Table 2. Both groups did not differ significantly in respect of pre- and postoperative LLD and preoperative OSD. Postoperative OSD was significantly lower in the nTHA group (− 0.92 ± 4.58 vs. − 0.07 ± 4.19; p < 0.0001). Inclination (40.47 ± 4.95 vs. 40.95 ± 5.28 degrees) and anteversion (19.41 ± 4.05 vs. 20.18 ± 4.95 degrees) of the acetabular cup were slightly but significantly (p < 0.05) lower in the nTHA group.
Both nTHA and cTHA were effective in restoring LLD and OSD by reducing the preoperative value significantly (p < 0.001). Regarding changes in LLD no statistical difference between nTHA and cTHA could be found. Regarding OSD, nTHA was slightly more effective than cTHA (− 2.06 ± 6.00 vs. − 1.50 ± 5.35; p < 0.05).
Testing for variance revealed no significant differences between the two groups for LLD post-operative (F = 2.6186, p = 0.1058), offset discrepancy postoperative (F = 0.4785, p = 0.4892) and inclination (F = 2.0801, p = 0.1494). Anteversion in cTHA had a significantly higher variance than in nTHA (F = 13.452, p < 0.001).
Linear regression analysis was performed to study factors associated with LLD postoperatively (Table 3). Navigated Operation (p = 0.186) and operative time (p = 0.103) had no influence, BMI showed a trending significant association with LLD postoperatively (p = 0.070). Linear regression analysis was also performed to study factors associated with OSD postoperatively (Table 4). BMI showed no significant association (p = 0.142), while significant associations were found for nTHA (p < 0.001) and operative time (p = 0.006).
Discussion
We retrospectively analyzed radiographs of patients who underwent cTHA in 2019 and nTHA 2021 in our institution. We are aware of the fact that no randomization was performed. Patients with cTHA were older, more often female and had higher ASA scores than patients with nTHA. All these limitations must be considered, when the two groups are compared.
These limitations do not however compromise the finding of this study that navigated hip arthroplasties need longer operation times with a mean prolongation of 10 min when navigation is used. This has been well documented by others1,20,21,22,23,24. While newer observations suggest that with a reasonable learning curve and improved workflow no added operative time in imageless navigation THA can be achieved25, we found no such change with increased use of navigation. In addition to the longer operative times, the higher costs of the navigated operation must be considered1 but was not the focus of this study.
We found that in both groups the operations were successful in restoring leg length and hip offset discrepancy. While postoperative LLD was not associated with the mode of operation or operative time, there was a trend of increased LLD with increased BMI. Computed tomography measurements have shown that measurements of inclination and anteversion were affected by the thickness of the soft tissue overlying the anterior superior iliac spine and pubic tubercles26. It is reasonable that our observation is due to different thicknesses of soft tissue. Interestingly, in contrast to published data, we could not document significantly higher decreases in leg length discrepancies postoperatively with computer navigation versus conventional THA21,24. Our results show, that in restoring hip offset discrepancy nTHA was statistically more effective than cTHA as it was associated with lower OSD values. Whether this discrepancy difference which was less than 1 mm is clinically relevant is unclear.
Navigated THA is advocated for improved placement of the acetabular component within the Lewinnek safe zone defined by a cup inclination of 40° ± 10° and a cup anteversion of 15° ± 10°9,20,27,28,29,30,31,32 Although cup placement within this zone has not been shown to significantly reduce dislocation rates, it is still a clinically relevant measure (32, 33). Regarding acetabular cup inclination and anteversion our results show that both surgical approaches resulted in acetabular positions which are well within Lewinnek safe zone9,33. The slightly but significant lower values in the nTHA group are noteworthy. The significantly higher variance of anteversion in cTHA is implicates that statistically nTHA is more precise than cTHA. Also, recent research demonstrates in vivo that an imageless, non-invasive navigation system is a reliable tool for intra-operative leg length and offset when compared to standard practice of plain film radiographs34.
Our study has several limitations. It is a retrospective, non-randomized analysis of groups of patients, that were treated in different time periods, with different implants. These groups differed statistically in respect of age, sex, and ASA-Scores. Therefore, all radiological outcome parameters must be interpreted with caution. We can only speculate that the radiologically observed differences between the two groups lead to clinically relevant differences in the follow up. However, sparce data on long term results imply that these differences do not achieve clinical relevance30.
In summary our results on the one hand confirm published data that the navigated approach to total hip arthroplasty offers higher precision in cup placement and off set at the cost of longer operation times, while, on the other hand, we were able to demonstrate no radiographically superiority of navigation with regard to leg length reconstruction.
If these results are clinically relevant or affect long term clinical outcomes, needs further investigations.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bostrom, M. P. G. & Haddad, F. S. The hip society supplement 2019. Bone Joint J. 101(6), 1 (2019).
Konyves, A. & Bannister, G. C. The importance of leg length discrepancy after total hip arthroplasty. J. Bone Joint Surg. Br. 87(2), 155 (2005).
Kubota, Y., Kaku, N., Tabata, T., Tagomori, H. & Tsumura, H. Efficacy of computed tomography-based navigation for cup placement in revision total hip arthroplasty. Clin. Orthop. Surg. 11(1), 43 (2019).
Patterson, D. C., Grelsamer, R. P., Bronson, M. J. & Moucha, C. S. Lawsuits after primary and revision total hip arthroplasties: A malpractice claims analysis. J. Arthroplast. 32(10), 2958 (2017).
Sakalkale, D. P., Sharkey, P. F., Eng, K., Hozack, W. J. & Rothman, R. H. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin. Orthop. Relat. Res. 388, 125–134 (2001).
Spalding, T. J. Effect of femoral offset on motion and abductor muscle strength after total hip arthroplasty. J. Bone Joint Surg. Br. 78(6), 997 (1996).
Flecher, X., Ollivier, M. & Argenson, J. N. Lower limb length and offset in total hip arthroplasty. Orthop. Traumatol. Surg. Res. 102(1 Suppl), S9 (2016).
Avram, G. M. et al. Acetabular cup placement and offset control in robotic total hip arthroplasty performed through the modified anterolateral approach. Int. Orthop. 47(9), 2265 (2023).
Lewinnek, G. E., Lewis, J. L., Tarr, R., Compere, C. L. & Zimmerman, J. R. Dislocations after total hip-replacement arthroplasties. J. Bone Joint Surg. Am. 60(2), 217 (1978).
Dastane, M., Dorr, L. D., Tarwala, R. & Wan, Z. Hip offset in total hip arthroplasty: Quantitative measurement with navigation. Clin. Orthop. Relat. Res. 469(2), 429 (2011).
Agarwal, S. et al. The use of computer navigation in total hip arthroplasty is associated with a reduced rate of revision for dislocation: A study of 6,912 navigated THA procedures from the Australian Orthopaedic Association National Joint Replacement Registry. J. Bone Joint Surg. Am. 103(20), 2021 (1900).
Bohl, D. D. et al. Computer-assisted navigation is associated with reductions in the rates of dislocation and acetabular component revision following primary total hip arthroplasty. J. Bone Joint Surg. Am. 101(3), 250 (2019).
Davis, E. T., McKinney, K. D., Kamali, A., Kuljaca, S. & Pagkalos, J. Reduced risk of revision with computer-guided versus non-computer-guided THA: An analysis of manufacturer-specific data from the National Joint Registry of England, Wales, Northern Ireland and the Isle of Man. JB JS Open Access 6(3), 6 (2021).
Rajpaul, J. & Rasool, M. N. Leg length correction in computer assisted primary total hip arthroplasty: A collective review of the literature. J. Orthop. 15(2), 442 (2018).
Tetsunaga, T. et al. Comparison of the accuracy of CT- and accelerometer-based navigation systems for cup orientation in total hip arthroplasty. Hip. Int. 31(5), 603 (2021).
Renkawitz, T., Meyer, M., Vollner, F. & Weber, M. Intraoperative assessment of pelvic tilt and cup position in total hip arthroplasty: The relevance of navigation and robotics. Orthopade 49(10), 893 (2020).
Ranawat, C. S., Rao, R. R., Rodriguez, J. A. & Bhende, H. S. Correction of limb-length inequality during total hip arthroplasty. J. Arthroplast. 16(6), 715 (2001).
Loughead, J. M., Chesney, D., Holland, J. P. & McCaskie, A. W. Comparison of offset in Birmingham hip resurfacing and hybrid total hip arthroplasty. J Bone Joint Surg. Br. 87(2), 163 (2005).
Jolles, B. M., Zangger, P. & Leyvraz, P. F. Factors predisposing to dislocation after primary total hip arthroplasty: A multivariate analysis. J. Arthroplast. 17(3), 282 (2002).
Li, Y. L. et al. Evidence-based computer-navigated total hip arthroplasty: An updated analysis of randomized controlled trials. Eur. J. Orthop. Surg. Traumatol. 24(4), 531 (2014).
Migliorini, F. et al. Imageless navigation for primary total hip arthroplasty: A meta-analysis study. J. Orthop. Traumatol. 23(1), 21 (2022).
Reininga, I. H. et al. Minimally invasive and computer-navigated total hip arthroplasty: A qualitative and systematic review of the literature. BMC Musculoskelet. Disord. 11, 92 (2010).
Shigemura, T. et al. Is a portable accelerometer-based navigation system useful in total hip arthroplasty?: A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 107(1), 102742 (2021).
Xu, K. et al. Computer navigation in total hip arthroplasty: A meta-analysis of randomized controlled trials. Int. J. Surg. 12(5), 528 (2014).
Valsamis, E. M., Ricketts, D., Hussain, A. & Jenabzadeh, A. R. Imageless navigation total hip arthroplasty: An evaluation of operative time. SICOT J. 4, 18 (2018).
Ybinger, T. et al. Accuracy of navigation-assisted acetabular component positioning studied by computed tomography measurements: Methods and results. J. Arthroplast. 22(6), 812 (2007).
Hohmann, E., Bryant, A. & Tetsworth, K. A comparison between imageless navigated and manual freehand technique acetabular cup placement in total hip arthroplasty. J. Arthroplast. 26(7), 1078 (2011).
Kalteis, T. et al. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: Is it as accurate as CT-based navigation?. J. Bone Joint Surg. Br. 88(2), 163 (2006).
Kumar, M. A., Shetty, M. S., Kiran, K. G. & Kini, A. R. Validation of navigation assisted cup placement in total hip arthroplasty. Int. Orthop. 36(1), 17 (2012).
Lass, R. et al. Total hip arthroplasty using imageless computer-assisted navigation-2-year follow-up of a prospective randomized study. J. Clin. Med. 9(6), 1620 (2020).
Moskal, J. T. & Capps, S. G. Acetabular component positioning in total hip arthroplasty: An evidence-based analysis. J. Arthroplast. 26(8), 1432 (2011).
Lass, R. et al. Total hip arthroplasty using imageless computer-assisted hip navigation: A prospective randomized study. J. Arthroplast. 29(4), 786 (2014).
Tezuka, T., Heckmann, N. D., Bodner, R. J. & Dorr, L. D. Functional safe zone is superior to the Lewinnek safe zone for total hip arthroplasty: Why the Lewinnek safe zone is not always predictive of stability. J. Arthroplast. 34(1), 3 (2019).
Lambers, A. P., Marley, M. A., Jennings, R. & Bucknill, A. Accuracy of leg length and offset measurements during total hip arthroplasty using an imageless navigation system. Cureus 15(5), e38689 (2023).
Acknowledgements
We express our gratitude to Agnes D. Cororaton for performing the statistical analysis.
Author information
Authors and Affiliations
Contributions
Conceptualization, R.L. and M.B. Data curation, R.L., Formal analysis R.L.; Methodology, R.L.; Supervision, M.B. and R.W.; Validation; R.L., A.O. and M.B. Writing—original draft: R.L. Writing—review & editing: M.B., R.W. All authors have read and agreed to the published version of the manuscript. All authors have approved the manuscript and agree with its submission.
Corresponding author
Ethics declarations
Competing interests
Author M.B.: Royalties from a company or supplier: Smith&Nephew, Research support from a company or supplier as a Principal Investigator: Ines Mandl Research Foundation, Smith & Nephew, Medical/Orthopaedic publications editorial/governing board: Journal of Orthopaedic Research. The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laggner, R., Oktarina, A., Windhager, R. et al. Changes in leg length and hip offset in navigated imageless vs. conventional total hip arthroplasty. Sci Rep 13, 17161 (2023). https://doi.org/10.1038/s41598-023-44009-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-44009-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.