Abstract
To compare changes in ophthalmic artery (OA) and its branches in diabetics with and without diabetic retinopathy (DR) using color duplex imaging (CDI), and to correlate these changes with the disease variables. 60 eyes of 60 diabetic patients were enrolled, divided into 3 groups: without DR (Group A), with Non-Proliferative DR (Group B) and with Proliferative DR (PDR) (Group C). Laboratory testing including HbA1c was done. Patients underwent CDI, by which OA, Central Retinal Artery (CRA) and Ciliary Arteries were identified; for each of them we measured Peak systolic velocity (PSV), End Diastolic velocity (EDV) and Resistivity Index (RI). Results were compared to clinical, laboratory and fundus examination. OA EDV was significantly lower and OA RI was found to be significantly higher in Group C (p = 0.027 and 0.025 respectively). CRA PSV and EDV were significantly lower in Group C (p = 0.017 and 0.001 respectively). PCA RI was significantly higher in Group C (p = 0.008). HbA1c was negatively correlated with CRA PSV (p = 0.041), also it was negatively correlated with CRA EDV (p = 0.0001), as well as with PCA EDV (p = 0.002). There was direct significant correlation between HbA1c and PCA RI (p = 0.012). Duration since diagnosis was negatively correlated with CRA EDV (p = 0.004). Multivariate linear regression showed that DR is an independent predictor for low OA EDV, high OA RI, low CRA EDV and high PCA RI. DR is an independent risk factor for orbital and ocular vessels flow alteration, thus can be used as a prognostic tool in diabetic patients. CDI can be reliably used in diabetics to predict early changes or progression of DR.
Similar content being viewed by others
Introduction
Till now, the actual pathogenesis behind the Diabetic Retinopathy (DR) onset and progression remains somehow unrevealed despite years and years of research. Hemodynamically, evidence has concluded that there is an early decrease in retinal blood supply even before the onset of DR1. Studying hemodynamics of retrobulbar vessels in diabetes using CDI can help in understanding the pathogenesis and can give an insight into the prospective treatment for DR. Moreover, it can guide us to predict individuals at advanced risk of developing vision threatening complications. Several studies have used CDI to analyze the circulatory changes in diabetics and found contradictory results: while some have noted a decrease in the retrobulbar blood flow velocities, others have reported an increase or no change in the same parameters1.
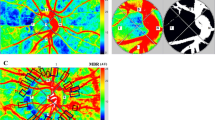
Blood supply of the retina comes from two branches of the Ophthalmic Artery (OA): the central retinal artery (CRA) and the posterior ciliary arteries (PCA)2. The CRA, running along the optic nerve, pierces the lamina cribrosa and enters the optic disc nasal to the posterior pole. It then divides into superior and inferior branches, which continue to bifurcate to supply blood to the inner retinal layers2. The CRA is an end branch of the OA and is considered as the main blood supplier to the retina. As for the outer retina, it is nourished through the PCA, which arises as a main trunk from OA then divides into short PCA and 2 long PCA that run anteriorly to supply CB and iris (Fig. 1).
The retro-ocular blood vessels that can be assessed by CDI include the OA, the PCA, CRA & CRV. CDI can also be used to study intraocular blood vessels, including the vortex veins, ocular tumors vasculature, vitreoretinal neovascular membranes as well as vessels in detached retina3. Due to its ability to analyze these vessels qualitatively and quantitatively, numerous studies have assessed changes in ocular blood flow in different eye diseases such as DR, glaucoma, CRA & CRV occlusions and have revealed significant differences compared to healthy individuals even in early disease stages4. In this study, we measured the different CDI parameters of the orbital vessels in diabetics with and without retinopathy in an attempt to detect correlations with different disease variables. DM affects roughly 15.6% of Egyptians between the ages of 20 and 60 years old5. DR affects 17.9–20% of diabetic individuals, according to some estimates6,7. CDI may be ideal for longitudinal follow up of diabetic patients for early detection of hemodynamic changes caused by ischemic retinopathy and hence early timely intervention to abort its progression. Some studies even estimated that CDI may replace fundus examination as the latter is relatively time consuming and annnoying to the patient because it needs prior dilatation of the pupil and causes blurry vision for several hours8. We do not agree with this opinion, despite our agreement that CDI may be of great use in early prediction of diabetic vasculopathy progression.
Patients and methods
This is a cross sectional study on diabetic patients at the ophthalmology outpatient clinic of Kasr Alainy hospital, Cairo University, between November 2020 to July 2021. All patients received a thorough explanation of the study design and aims. An informed consent was obtained from all patients. The study protocol was revised and approved by the Research Ethics Committee, Faculty of Medicine, Cairo University (Code:MS-454-2020) and followed the tenets of the Helsinki declaration.
Study population
Inclusion criteria
Diabetic patients with more than 5-years duration were included. Only 1 eye per subject was selected in the study, the eye with more diabetic changes was chosen in case of patients with retinopathy, while in diabetics with no fundus changes, it was randomly selected.
Exclusion criteria
We excluded patients with vascular retinopathies other than DR (e.g., hypertensive retinopathy, retinal artery or vein occlusion, hereditary systemic angiopathy); patients with glaucoma, laser photocoagulation, previous intravitreal injections, recent eye trauma or surgery, congenital anomalies, any inflammatory process involving the eye and globe. Patients suspected to have hypoglycemic coma or diabetic keto acidosis, patients with any other hormonal disturbance rather than DM, cardiovascular patients and chronically ill (e.g., nephropathy) patients were also excluded. Also, patients who take any medications affecting the circulation hemodynamics such as lowering blood lipids and preventing platelet aggregation, were excluded.
Data collection
Patients had their demographics (age and gender) recorded, and a review of their medical history including personal history, history and duration of systemic diseases, history of ocular diseases. All patients underwent random blood sugar and glycosylated hemoglobin level (HbA1c) testing and the duration of diabetes mellitus (DM) was noted. All patients had comprehensive ophthalmological examination, including Best Corrected Visual Acuity (BCVA) using Snellen’s chart, slit lamp examination, assessment of intraocular pressure by Goldmann’s applanation tonometry, and dilated fundus examination by binocular indirect slit-lamp biomicroscopy. In patients with retinopathy, Fundus Fluorescein Angiography (FFA) was done to detect possible proliferation if not seen clinically. Patients were divided into 3 groups. Group A: without diabetic retinopathy, Group B: with Non-Proliferative Diabetic Retinopathy (NPDR), and Group C: with PDR. All selected patients had no previous treatment.
Color duplex imaging
CDI scan was performed to all patients using the same machine by a single experienced operator. The operator was blind to the clinical and fundus examination findings of the patients. The study was performed using the ultrasound and Color duplex machine (TOSHIBA TUS A-500, Toshiba medical systems corporation, JAPAN) using linear array probe (L11-13 MHZ). Patients were placed in supine decubitus, instructed to keep their eyes straight ahead while closing their lids. A good amount of acoustic coupling gel was applied to the closed upper eyelid and the probe was gently positioned, avoiding exerting excessive pressure on the eye and the hand of the operator rested either on the patient’s forehead or cheek for fine manipulation of the probe. We used the preset for small parts which allowed detection of low flow with low pulse repetition frequency, low filter and high gain. First, we identified the eye globe using the B- mode image, then the optic nerve was identified at the posterior aspect of the eye globe as the hypo-echoic structure, and used as a landmark and depth was adjusted to visualize the apex of the orbit then the overall gain, time gain compensation and focus were adjusted to visualize the whole orbital cavity and its contents clearly. Next, Color mode was applied, adjusting velocity scale to 7–15 cm/second using low filter setting and increasing color gain till noise appears then slightly decreasing the gain to just below the noise floor.
Central Retinal Artery (CRA) was identified running within the optic nerve together with the Central Retinal Vein (CRV) (Fig. 2), while Ciliary Arteries (CA) (Nasal or Temporal were identified on either both sides of the optic nerve and Ophthalmic Artery (OA) was identified arising at the apex of the orbit temporally and crossing nasally over (or below) the optic nerve (Fig. 3). Regarding CA, they arise as nasal and temporal trunks from the OA, then they divide into short and long branches. We scanned PCA at the main trunk before their division. Since the angle can't be fixed at zero in advance, the cursor was kept parallel or near parallel the direction of blood flow (according to the vessel direction), usually at an angle minor than 60°. For each artery, we measured Peak Systolic Velocity (PSV), End Diastolic Velocity (EDV), and Resistivity Index (RI) while adjusting sample volume to 1 mm, angle at zero and CDI filter at 70 Hz (low filter setting) and again the gain was increased until the noise appeared in the CDI spectrum then decreased again just below the noise floor.
CDI of the left eye of a diabetic patient showing the Doppler spectral waveform of CRA and CRV. The flow velocity waveform in the CRA is of low amplitude and typical peaks for systolic and diastolic velocities are seen above the zero line. The flow velocity waveform in the CRV (almost monophasic) presents below the zero line.
Outcome measures
-
1.
Comparing CDI parameters (PSV, EDV and RI) of OA, CRA and PCA between Groups A, B and C.
-
2.
Correlation between measured CDI parameters (PSV, EDV and RI) and disease variables including age, duration of DM, HbA1c level, and presence of retinopathy.
-
3.
Multivariate Linear Regression Analysis was performed with different dependent variables (OA EDV, OA RI, CRA PSV, CRA EDV and PCA RI) and independent variables such as age, sex, duration of diabetes and DR.
Statistical analysis
Statistical analysis was conducted using SPSS 22nd edition, numeric variables were presented in mean ± standard deviation and were compared using Mann Whitney u test between 2 groups and Kruskal Wallis test between > 2 groups after normality testing. Categorical variables were presented in frequency and percentage and were compared using Chi2 test. Spearman correlation test was used to assess the correlation between 2 numeric variables. Any p value < 0.05 was considered significant.
Results
We have included 60 diabetic patients in our study with a mean age of 53 ± 12 years and 32 (53.8%) were males. The mean duration of diabetes was 13 ± 6 years, and the HbA1c was 7.5 ± 0.7 gm/dL. Based on fundus examination and FFA, we had 13 patients (21.7%) with normal fundus (Group A), 12 (20%) had NPDR (Group B) and 35 (58.3%) had PDR (Group C). Patients in Group C were significantly older than patients of the other 2 groups. Group C patients also had significantly longer disease duration higher HbA1c level (Table 1). Figure 4 shows the HbA1c level distribution between the 3 groups.
Comparing CDI parameters between Groups A, B and C
OA EDV was significantly higher in Group A with p value 0.027, OA RI was significantly higher in Groups B and C compared to Group A with p value 0.025. CRA PSV as well as CRA EDV were significantly lower among Group C patients with p value 0.017 and 0.001 respectively. PCA RI was significantly higher among Group C patients when compared to Groups A and B, with p value 0.008 (Table 2). A post hoc pairwise comparison table was done and also showed significant differences between CDI parameters in different arteries upon comparing each 2 of the 3 groups together (Table 3).
Correlation between CDI parameters and disease variables
Interesting correlations between duration of diabetes, HbA1c and CDI findings were found and are shown in Table 4, Figs. 5, 6. HbA1c was negatively correlated with CRA PSV (p: 0.041), with CRA EDV (p: 0.0001), as well as with PCA EDV (p: 0.002). On the other hand, there was direct significant correlation between HbA1c and PCA RI (p: 0.012). Disease duration was negatively correlated with CRA EDV (p: 0.004).
Multivariate linear regression models
Multivariate linear regression model was performed with different dependent variables (OA EDV, OA RI, CRA PSV, CRA EDV and PCA RI) and independent variables such as age, sex, duration of diabetes and DR. Results showed that DR is an independent predictor for low OA EDV, high OA RI, low CRA EDV and high PCA RI with p values < 0.05 after adjusting for age, gender and duration of diabetes.
Discussion
Demographics
In our study, it was noted that patients with higher degree of DR (PDR, Group C) had significantly older age, higher HbA1c, and longer DM duration than the other 2 groups. This is expected with the disease timely progression and in agreement with other studies that reported that aging and higher HbA1c were risk factors for developing DR, and that longer disease duration was consistently found among patients with PDR9,10,11,12.
CDI parameters
Orbital CDI indices analysis showed that the OA EDV was significantly lower and OA RI was significantly higher among Group C compared to the other 2 groups. These results are consistent with those reported by Divya et al., who studied 100 diabetic patients, 50 without DR and 50 with DR. They concluded that severe DR was significantly associated with higher OA RI compared to mild DR and diabetics without DR1.
We also found that CRA PSV and EDV in Group A patients were significantly higher than Group B and C. This agrees well with what has been reported by Dimitrova et al. and MacKinnon et al., who reported that decreased EDV and increased RI in CRA were consistent with background DR compared to controls3,13. But in our case, despite the significant decrease in the CRA flow velocities in DR groups, the increase in RI was not statistically significant. This has been previously concluded in other studies and could be explained by the simultaneous and proportionate decrease of both PSV and EDV in patients with DR1.
We also found PCA EDV to be significantly higher in group A, while the PCA RI was significantly highest among Group C compared to Group B, which in its turn was siginifcantly higher compared to Group A. These results agree partially with the results of Divya and his team who stated that PCA EDV and PSV were significantly different between diabetics with and without DR, but their results did not witness any significance regarding RI1. The findings of decreased EDV in PCA has been previously explained as a possible result of choroidal blood flow affection in the early stages of DR. An outstanding study by Laser Doppler flowmetry has shown a foveal reduction in choroidal blood flow in early DR14. Another study analyzing the Choroidal vascularity index (CVI) using by optical coherence tomography (OCT) has also concluded a decreased CVI in patients with mild/moderate NPDR , which proofs the early choroidal vascular affection15. Last but not least, histopathological studies have reported a much more chorio-capillaries loss in diabetic eyes compared to normal eyes1.
Since It has been postulated that only 10% or less of the total ocular blood supply from OA flows to the retina while the majority remainder is directed to the ciliary circulation to supply the choroid due to the high metabolic need of photoreceptors16, thus our result of increased RI in the OA in PDR group can be attributed to the statistically significant reduction in EDV observed in diabetic subjects caused by distal downstream vascular changes in the choroid mainly and maybe the retina, since significant differences were found in only one CRA parameter between groups. Thus, we believe that the OA hemodynamic alterations in our study mainly represent alteration in choroidal flow, with a minimal affection of retinal blood flow. Other studies found that choroidal flow affection is the main factor in hemodynamic changes and did not find any significant differences in CRA parameters1.
Although it is not easy to propose a contributing link, it can be assumed that changes in choroidal circulation (as reflected by high OA RI) lead to upregulation of VEGF (vascular endothelial growth factor) and downregulation of antiangiogenic PEDF (pigment epithelial-derived factor) and hence contributing to DR progression. Variable secretion and expression of these growth factors derived from the retinal pigment epithelium can lead to non-proliferative and proliferative DR17.
Correlations and multivariate analysis
HbA1c was found to be negatively correlated with CRA PSV, CRA EDV, and with PCA EDV. HbA1c also showed significant correlation with PCA RI. These results confirm the direct relationship between poor diabetic control and the hemodynamic alterations in CRA and PCA; and the latter hemodynamic changes were mentioned above to be significantly correlated with the development and severity of DR. This agrees with a previous correlating study stating that duration of diabetes as well as HbA1c levels, were found to be correlating negatively with EDV of CRA1. So poorly controlled diabetic patients are more likely to develop DR and to develop hemodynamically significant alteration in orbital arteries. It has been noted in the multivariate linear regression model that we conducted, that DR is an independent predictor for low OA EDV, high OA RI, low CRA EDV and high PCA RI with p values < 0.05 after adjusting for age, gender and duration of diabetes.
Limitations
Our study had limitations, first the relatively small sample which was a reflection of the decreased flow of patients in the Covid-19 period during which this study was conducted. In addition, in the multivariate regression analysis, we used DR as one of the independent variables, but we did not assess the degree of DR as another more detailed variable. Nevertheless, DR was proved to be an independent predictor for some of the CDI parameteric changes in orbital vessels.
In conclusion, DR is an independent predictor for low OA EDV, high OA RI, low CRA EDV, and high PCA RI. CDI can be a useful tool for detecting retrobulbar vascular affection caused by DR. Since alterations in resistivity indices and arterial velocities of the orbital arteries were significantly correlated to DR and HbA1c levels, it thus has the potential to be used as a rapid affordable prognostic screenig tool for the development or the progression of DR by noticing individual changes in flow parameters. We do recommend conducting a larger prospective studies including patients with different grades of DR and to follow them up to assess changes over time, in order to validate and to standardize a protocol to predict the onset or the early progression of DR using CDI.
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Divya, K. et al. Evaluation of retrobulbar circulation in type 2 diabetic patients using color Doppler imaging. Indian J. Ophthalmol. 68(6), 1108–1114 (2020).
Remington LA. Retina. Clinical Anatomy and Physiology of the Visual System. 3rd ed. St. Louis, MO: Elsevier/Butterworth Heinemann;2012:87–8.
Dimitrova, G. & Kato, S. Color Doppler imaging of retinal diseases. Surv. Ophthalmol. 55(3), 193–214 (2010).
Bittner, M. et al. Color Doppler analysis of ophthalmic vessels in the diagnosis of carotic artery and retinal vein occlusion, diabetic retinopathy and glaucoma: systematic review of test accuracy studies. BMC Ophthalmol. 16(1), 214. https://doi.org/10.1186/s12886-016-0384-0 (2016).
Hegazi, R., El-Gamal, M., Abdel-Hady, N. & Hamdy, O. Epidemiology of and risk factors for type 2 diabetes in Egypt. Ann. Glob. Health 81(6), 814–820 (2015).
AlSawahli, H. et al. Population-based cross-sectional prevalence survey of diabetes and diabetic retinopathy in Sohag—Egypt. BMJ Open. 11(6), e047757 (2021).
Macky, T. A., Khater, N., Al-Zamil, M. A., El Fishawy, H. & Soliman, M. Epidemiology of diabetic retinopathy in Egypt: a hospital-based study. Ophthalmic Res. 45(2), 73–78 (2010).
Venturini, M. et al. Early increase in retinal arterial and venous blood flow velocities on color Doppler ultrasound after acupuncture. Ultraschall der Med.-Eur. J. Ultrasound https://doi.org/10.1055/a-1342-6789 (2021).
Leley, S. P., Ciulla, T. A. & Bhatwadekar, A. D. diabetic retinopathy in the aging population: A perspective of pathogenesis and treatment. Clin. Interv. Aging 16, 1367. https://doi.org/10.2147/CIA.S297494 (2021).
Zhang, X. et al. Prevalence of diabetic retinopathy in the United States, 2005–2008. JAMA 304(6), 649–656 (2010).
Stępień, E., Kabłak-Ziembicka, A., Czyż, J., Przewłocki, T. & Małecki, M. Microparticles, not only markers but also a therapeutic target in the early stage of diabetic retinopathy and vascular aging. Expert Opin. Ther. Targets 16(7), 677–688 (2012).
Hahn, P., Acquah, K., Cousins, S. W., Lee, P. P. & Sloan, F. A. Ten-year incidence of age-related macular degeneration according to diabetic retinopathy classification among medicare beneficiaries. Retina 33(5), 911 (2013).
MacKinnon, J. R. et al. Color Doppler imaging of the ocular circulation in diabetic retinopathy. Acta Ophthalmol Scand. 78(4), 386–389 (2000).
Nagaoka, T. et al. Alteration of choroidal circulation in the foveal region in patients with type 2 diabetes. Br. J. Ophthalmol. 88, 1060–1063 (2004).
Kim, M., Ha, M. J., Choi, S. Y. & Park, Y. H. Choroidal vascularity index in type-2 diabetes analyzed by swept-source optical coherence tomography. Sci. Rep. 8, 70 (2018).
Cioffi, G. A., Granstam, E. & Alm, A. Ocular circulation. In Adler’s Physiology of the Eye 10th edn (eds Kaufman, P. L. & Alm, A.) 747–773 (Mosby, 2003).
Witmer, A. N., Vrensen, G. F., Van Noorden, C. J. & Schlingemann, R. O. Vascular endothelial growth factors and angiogenesis in eye disease. Prog. Retin. Eye Res. 22, 1–29 (2003).
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research did not receive any grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [Alia Noureldine], [Abo Elmagd ElBohy] and [Aya Montasser]. The first draft of the manuscript was written by [Hisham Mostafa]and revised by [Tamer Macky]. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Noureldine, A.M., Abdelmaksoud, A.M.S., Mostafa, H.A.A.F. et al. Orbital blood vessels changes on color duplex imaging in diabetics with and without diabetic retinopathy. Sci Rep 13, 17115 (2023). https://doi.org/10.1038/s41598-023-43838-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43838-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.