Abstract
Mortality related to femoral neck fractures remains a challenging health issue, with a high mortality rate at 1 year of follow-up. Three modifiable factors appear to be under control of the surgeon: the choice of the implant, the use of cement and the timing before surgery. The aim of this research project was to study the impact on mortality each of these risk factors play during the management of femoral neck fractures. A large retrospective epidemiological study was performed using a national database of the public healthcare system. The inclusion criteria were patients who underwent joint replacement surgery after femoral neck fracture during the years 2015 to 2017. All data points were available for at least 2 years after the fracture. The primary outcome was mortality within 2 years following the surgery. We evaluated the association between mortality and the type of the implant hemiarthroplasty (HA) versus total hip arthroplasty (THA), cemented versus non cemented femoral stem as well as the timing from fracture to surgical procedure. A multivariate analysis was performed including age, gender, comorbidities/autonomy scores, social category, and obesity. We identified 96,184 patients who matched the inclusion criteria between 2015 and 2017. 64,106 (66%) patients underwent HA and 32,078 (33.4%) underwent THA. After multivariate analysis including age and comorbidities, patients who underwent surgery after 72 h intra-hospital had a higher risk of mortality: Hazard Ratio (HR) = 1.119 (1.056–1.185) p = 0.0001 compared to the group who underwent surgery within 24 h. THA was found to be a protective factor HR = 0.762 (0.731–0.795) p < 0.0001. The use of cement was correlated with higher mortality rate: HR = 1.107 (1.067–1.149) p < 0.0001. Three key points are highlighted by our study in the reduction of mortality related to femoral neck fracture: the use of hemiarthroplasty a surgery performed after 48 h and the use of cement for femoral stem fixation adversely affect mortality risk.
Similar content being viewed by others
Introduction
Femoral neck fractures are a frequent pathology seen in the elderly population1,2. This group of patients, often presents with multiple co-morbidities, complex social requirements and prolonged length of hospital stay, leading to an associated high mortality rate and a major healthcare cost3. All these factors have been pointed out in national database studies like Macaulay et al.3 reviewing 350,000 cases in the US population in 2006 and Bandhari et al.4 280,000 for the same country in 2005. Nikitovic et al.5 published the cost of managing a single patient in Ontario with a femoral neck fracture as being 39,479 dollars the first year and 10,347 dollars the second year. The mortality rate after femoral neck fracture is around 30% in the 1st year following the fracture6.
The timing from fracture to surgery appears to be a key point in reducing mortality. In. 2010, Simunovic et al.7 reported a significantly lower mortality and morbidity rate in their study if surgery was performed early. The most recent study evaluating this question is Hip Attack in the Lancet in 20208 which described a comparable mortality rate if the surgery was performed during the first 6 h after the trauma or twenty 4 h after.
There is strong evidence in the literature to support the use of Total Hip Arthroplasty (THA) to provide better patients reported outcomes measures (PROM’s) compared to hemiarthroplasty (HA)9,10,11,12,13,14. There is ongoing debate regarding the influence of the choice of the implant on the mortality rate. Wang et al.15 found a lower mortality rate in the THA group compared to the HA group in patients with displaced neck of femur fractures. Lewis et al.16 performed a meta-analysis including 1364 patients in which there was no difference in mortality rate between the two implant options. The lower mortality rate found in some studies17 when utilizing a THA may be explained by lower pre-operative co-morbidities levels.
Finally, the literature does not provide strong evidence on the use of cemented versus uncemented stems in femoral neck fracture surgery18,19,20,21. Kumar et al.22 did not find any difference in their meta-analysis which included 18 studies with 2819 patients, whereas Richardson et al.23 described a higher mortality rate for uncemented stems due to a higher reoperation rate.
The purpose of this study was to identify key points in the management of femoral neck fracture which could be “game changers” to reduce mortality16,17. The primary outcome was the mortality rate at 2 years of follow up after arthroplasty for femoral neck fracture. The modifiable risk factors associated to the primary outcome were analyzed: timing to surgery, the choice of implant: THA versus HA and the use of cemented or cementless femoral stems.
Methods
A population-based cohort study was performed using the French national hospital database (Programme de Médicalisation des Systèmes d’Information or PMSI) covering currently 98.8% of the country population24. The PMSI contains anonymized information prospectively collected from all public and private hospitals in France for acute (PMSI-MCO) and psychiatric (PMSI-PSY) hospitalizations. Inpatient stays are converted into single diagnosis-related groups (DRGs) based on standard discharge abstracts containing administrative and clinical information: primary/secondary diagnoses, using the International Classification of Diseases, Tenth Revision (ICD-10), as well as procedural codes associated with the care provided25,26.
The access to the SNIIRAM is regulated and requires approval from the IDS, Institute of health data and the CNIL, the French data protection commission27. The study was declared for ethical considerations to the French National Data Protection Commission in accordance with the previous declaration of compliance with the reference methodology MR005- N°: 2203797.
Outcomes
Our primary outcome was the mortality rate after arthroplasty surgery for femoral neck fracture. The mortality rate considered was the in-hospital mortality at a minimum of 2 years follow up.
Three modifiable risk factors associated to the mortality were considered:
-
The time between femoral neck fracture and arthroplasty was separated in four categories: Group I for the surgery performed during the first 24 h in hospital, group II between 24 and 48 h, group III between 48 and 72 h and group IV for the patients who underwent the surgery after 72 h in hospital8.
-
The choice of the implant: total hip arthroplasty or hemiarthroplasty28,29.
-
The use of cemented or cementless implant for the femoral stem23.
The following non-modifiable risk factors of mortality were included in the multivariate analysis:
-
Age
-
Gender
-
Comorbidities Scores30
-
Type of hospital: Public/Private
-
Obesity
-
Social deprivation index31
Study population
The inclusion criteria were patients hospitalized between 2015 and 2017 in France, suffering from an intracapsular femoral neck fracture according to the ICD-10 code S720 and who had undergone prosthetic surgery either with hemiarthroplasty (HA) or total hip arthroplasty (THA). Specific codes from the List of Reimbursable Products and Services (LRPS) were used to identify THA and HA and the use of cemented implants. These codes are displayed in Appendix.
The exclusion criteria were patients who suffered a contralateral femoral neck fracture within the last 2 years, patients for which it was impossible to distinguish cemented versus non-cemented implants and patients who underwent osteosynthesis.
Population characteristics
The following demographic and clinical patients’ characteristics were extracted and computed from the database: age; gender; social deprivation assessed by the FDep09 index validated on French data32 categorized according to quartiles, from the least (Q1) to the most deprived areas (Q4); year of surgery; comorbidities assessed using the Elixhauser score30 (computed from ICD-10 codes recorded as primary or secondary diagnoses over the period of the last 12 months preceding the surgery) and obesity (from ICD 10 codes E66.x).
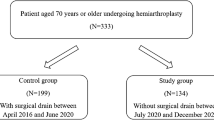
As a result, 96,184 patients were included during the 3 years investigated by our study. A total of 64,106 patients underwent hemiarthroplasty (66.6%) and 32,078 underwent total hip arthroplasty (33.4%) (Fig. 1). The number of women was higher than the number of men: 71,114 women (73.9%) and 25,070 men (26.1%). The HA group included 48,065 (74.9%) women and 16,041 (25.1%) men. The THA group included 23,049 (71.8%) women and 9029 (28.2%) men. The mean age was 84.7 ± 8.2 in the HA group and 76.8 ± 11.6 in the THA group. The mean number of days in hospital was 10.6 ± 6.8 in the HA group and 8.35 ± 6.02 in the THA group. The mean Charlson score was 1.27 ± 1.91. The mean Elixhauser score was 5.76 ± 7.45, and 3.71% of our population was considered as obese (BMI > 30) (Table 1).
Statistical analysis
All the data contained a minimal period of 2 years after the femoral neck fracture at the time of data collection. Comparisons between the HA Group vs the THA Group was performed according to socio-demographics data using the Chi2 test for categorical data and the t test for comparison of means for quantitative variables.
Risk factors associated with 2-years mortality were then analyzed: We performed univariate and multivariable survival analysis using the frailty Cox model using the hospital as a random effect. Data was censored at 2 years following surgery.
Multivariate analysis was adjusted on the following variables: age (categorized), gender, Elixhauser comorbidity score (Appendix), type of hospital (academic, non-academic but public, private), obesity, year of surgery, type of implant, cemented vs non cemented implant, deprivation index, delay of surgery (categorized). No stepwise selection of variables was performed.
For each model, p < 0.05 was considered as statistically significant corresponding to an alpha risk α = 0.05. Analyses were performed using the SAS software ® (V9.4), SAS Institute, Cary, North Carolina, United-States.
Ethical approval
The study was declared for ethical considerations to the French National Data Protection Commission in accordance with the previous declaration of compliance with the reference methodology MR005- N°: 2203797.
Informed consent
The study was based only on publicly available anonymized data of the public healthcare insurance and thus no informed consent was required because these data are routinely collected, and no experimental study was made on the patients. The Institutional Review Board confirmed the absence of need for informed consent of the participant. The reference number of the IRB is MR005- N°: 2203797.
Results
Mortality rate
The in-hospital mortality rate was studied at 2 years of follow up: 16,238 (16.88%) patients were deceased and 79,946 (83.12%) were still alive. During the first stay, in hospital mortality associated with the femoral neck fracture was seen in 2608 (2.71%) patients (Fig. 2).
Timing to surgery
Group I considered those undergoing surgery for a fractured neck of femur in less than 24 h, with 10,758 patients (11.2% of total population). In this group, the 2-year mortality rate was 14.91% which was considered as the reference in the multivariate analysis. Group II looked at those undergoing surgery within 24 and 48 h, including 37,840 patients (39.3% of total population) with a mortality rate of 14.47%. Group III considered those undergoing surgery within 48 and 72 h, including 19,655 patients (20.4% of our population). In Group III the mortality rate was 16.67%. Group IV patients had surgery after 72 h, including 27,931 patients (29.1% of population) with a mortality rate of 21.06% (Fig. 3, Table 2).
The univariate analysis found the following results: Group I: Reference, group II: HR = 0.99 (0.936–1.046) p = 0.7171, group III: HR = 1.109 (1.045–1.177) p = 0.0007, group IV: HR = 1.335 (1.263–1.411) p < 0.0001 (Table 3).
The multivariate analysis including age and comorbidities only identified the Group IV to be an independent and statistically significant risk factor of mortality: HR = 1.119 (1.056–1.185) p = 0.0001 (Table 4).
Total hip arthroplasty versus hemiarthroplasty
The HA group included 64,106 patients. At 2 years of follow-up, 12,247 (19.1%) patients were deceased and 51,859 (80.9%) were still alive. The THA group included 32,078 patients. At 2 years of follow up, 3991 (12.4%) patients were deceased and 28,087 (87.6%) were still alive (Table 2).
The univariate analysis found a Hazard Ratio (HR) = 0.628 (0.606–0651) p < 0.0001 for THA as a protective factor of mortality (Table 3). This was confirmed by the multivariate analysis including age and comorbidities: THA was found to be a protective factor of mortality. HR = 0.762 (0.731–0.795) p < 0.0001 (Table 4).
Cement versus cementless stem
The use of cement for the femoral stem fixation was also investigated. Out of the entire cohort, 65,914 hip arthroplasties were uncemented and 30,270 were cemented. The use of cement was more frequent in the THA group: 22,911 (71.4%) versus 9167 (28.6%). In the HA group, the use of cement was also more frequent: 43,003 (67.1%) versus 21,103 (32.9). In the cemented group, 5587 (18.5%) patients were deceased at 2 years of follow up and 24,683 were still alive (81.5%) (Table 2). In the uncemented group, 10,651 (16.2%) patients were deceased at 2 years of follow up and 55,263 (83.8%) were still alive.
The univariate analysis found the following results: the use of cement was an independent risk factor of mortality at 2 years of follow up: HR = 1.108 (1.073–1.145) p < 0.0001 (Table 3). The multivariate analysis including age and comorbidities confirmed cement to be an independent and statistically significant risk factor of mortality: HR = 1.107 (1.067–1.149) p < 0.0001 (Table 4).
Discussion
Our study highlights three crucial points in the management of femoral neck fractures: The timing from emergency admission to surgery, the choice between hemi- and total hip arthroplasty and the use of cemented or uncemented femoral stem. It appears that the right surgeon decision concerning these factors could reduce mortality. Thus, based on this large database study it appears that performing a total hip arthroplasty for femoral neck fracture with an uncemented femoral stem within 72 h after admission looks a protective attitude to reduce mortality rate.
Concerning the timing from fracture to surgery, Simunovic et al.7 published in their meta-analysis, an obvious reduction of mortality risk if the timing from fracture to surgery was reduced. Lewis and Waddel33 performed a review of the literature and found that a delay in surgery up to 48 h in ASA 1 or 2 patients did not adversely affect patient outcomes. A large randomized controlled trial was published by the Hip Attack group in the Lancet in 2020 comparing 1487 patients undergoing early surgery within 6 h after entering the hospital and 1483 patients undergoing surgery within 24 h. They did not find any significant reduction of mortality between the two groups. Our study highlights the fact that mortality really increases after 72 h as seen in Group IV: HR = 1.119 (1.056–1.185) p = 0.0001. This hazard ratio suggests that for every thousand surgeries for femoral neck fractures, 119 patients may die due to a prolonged delay of surgery. Another explanation for increased mortality after 72 h could be related to the taking of anti-coagulants medication creating a bias in a more vulnerable population with cardiac disease. Patients undergoing surgery in more than 72 h would be a different sub-population.
A significant reduction of mortality was found after total hip arthroplasty compared to hemiarthroplasty. This finding is consistent with two studies analyzing national data. Hansson et al.17 looked at a cohort of patients from the Swedish Hip Registry who found a reduction of mortality linked to THA in a population of 5815 patients. The second study was published by Wang et al.15 based on 70,242 American patients. They found a reduction of mortality at 2 years of follow up in a multivariate analysis: HR 1.67 (1.59–1.92). The most likely reason to explain this reduction of mortality is the increase of function after THA compared to HA11,34,35,36. Mariconda et al.37 described an increase of the autonomy score in the elderly after THA compared to HA. Based on these studies, it can be postulated that an arthroplasty associated with higher functional scores allows better return to autonomous living and reduced mortality. In our study the Hazard Ratio of 0.762 means that 238 patients are protected from death for every thousand surgeries if the surgeon chooses a total hip arthroplasty. Even though the population of THA and HA are difficult to compare because HA group is older and present more comorbidities than THA group. The multivariate analysis allows us to get rid of the bias concerning the differences in the populations.
There is no consensus in the literature concerning the use of cement for femoral stem fixation19,21,23,38. Nantha Kumar et al.22 performed a meta-analysis of 18 studies including 2819 patients comparing cemented versus cementless stem fixation. They found a reduced risk of intra- and post-operative peri-prosthetic fracture in the cemented arthroplasty group but no difference in terms of mortality. In comparison, Richardson et al.23 described an increased risk of mortality linked to the use of cementless femoral stem. In this study, they found an increased incidence of revision surgery in the cementless stem group which was associated with a higher rate of mortality. The literature review published by Chen et al.21 in 2018 explains that the choice of using cement or not must be based on bone quality, comorbidity profile, and age. Based on our findings, there is an increased risk of mortality with cemented stem fixation: for every thousand surgeries performed, 107 patients would potentially be saved if they have cementless fixation. Two reasons could explain the higher mortality rate associated with cement: first the physiological reaction induced by cement39 including hypersensitivity and lung reaction could cause death. Second, the surgeon could choose to use cement due to poor bone quality. A low bone quality could be associated with decrease overall condition. This could create a selection bias.
One potential limitation of the study stands in the only “in-hospital” mortality rate: the percentage of mortality in our series of 17% at 2 years of follow up does not includepatients who died at their home. This is why the percentage is below the results displayed in the literature of 30% of mortality at 1 year2,6,40. Berggren et al.40 published a mortality rate of 40% at 3 years of follow up after femoral neck fractures and Giummarra et al.6 considered 30% at 1 year, which is the most accepted percentage in the scientific community. The French National Institute of Statistics published the following results concerning places of death in 2016: 59% in-hospital mortality, 26% at home, 14% in retirement home and 1% on the roads41. This variation of percentage does not change the statistics and conclusions of our study even though the percentage is reduced because both groups are concerned.
The strength of the study is based on the large number of participants analyzed from a national database. The collected dataset allowed performing a powerful multivariate analysis including age and comorbidities to identify the risks factors associated to mortality following femoral neck fracture. This can bring new knowledge on the optimal timing and type of arthroplasty treatment for femoral neck fracture affecting a growing elderly population.
Data availability
All data used for the study are available and have been uploaded on the submission platform as a filed called RESULTATSv3.docx.
References
Avery, P. P. et al. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: A seven- to ten-year follow-up report of a prospective randomised controlled trial. J. Bone Joint Surg. Br. 93, 1045–1048 (2011).
Levi, N. Early mortality after cervical hip fractures. Injury 27, 565–567 (1996).
Macaulay, W., Pagnotto, M. R., Iorio, R., Mont, M. A. & Saleh, K. J. Displaced femoral neck fractures in the elderly: hemiarthroplasty versus total hip arthroplasty. J. Am. Acad. Orthop. Surg. 14, 287–293 (2006).
Bhandari, M. et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J. Bone Joint Surg. Am. 87, 2122–2130 (2005).
Nikitovic, M., Wodchis, W. P., Krahn, M. D. & Cadarette, S. M. Direct health-care costs attributed to hip fractures among seniors: A matched cohort study. Osteoporos. Int. J. Establ. Result Coop. Eur. Found. Osteoporos. Natl. Osteoporos. Found. USA 24, 659–669 (2013).
Giummarra, M. J. et al. Twelve month mortality rates and independent living in people aged 65 years or older after isolated hip fracture: A prospective registry-based study. Injury https://doi.org/10.1016/j.injury.2019.11.034 (2019).
Simunovic, N. et al. Effect of early surgery after hip fracture on mortality and complications: Systematic review and meta-analysis. CMAJ Can. Med. Assoc. J. J. Assoc. Medicale Can. 182, 1609–1616 (2010).
HIP Attack Investigators. Accelerated surgery versus standard care in hip fracture (HIP ATTACK): An international, randomised, controlled trial. Lancet Lond. Engl. 395, 698–708 (2020).
Hopley, C., Stengel, D., Ekkernkamp, A. & Wich, M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: Systematic review. BMJ 340, c2332–c2332 (2010).
Ossendorf, C., Scheyerer, M. J., Wanner, G. A., Simmen, H.-P. & Werner, C. M. Treatment of femoral neck fractures in elderly patients over 60 years of age—Which is the ideal modality of primary joint replacement?. Patient Saf. Surg. 4, 16 (2010).
Hedbeck, C. J. et al. Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: A concise four-year follow-up of a randomized trial. J. Bone Joint Surg. Am. 93, 445–450 (2011).
Baker, R. P., Squires, B., Gargan, M. F. & Bannister, G. C. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J. Bone Joint Surg. Am. 88, 2583–2589 (2006).
Blomfeldt, R. et al. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J. Bone Joint Surg. Br. 89, 160–165 (2007).
Farey, J. E., Cuthbert, A. R., Adie, S. & Harris, I. A. Revision risk after unipolar or bipolar hemiarthroplasty for femoral neck fractures: An instrumental variable analysis of 62,875 procedures from the Australian Orthopaedic Association National Joint Replacement Registry. J. Bone Joint Surg. Am. 103, 195–204 (2021).
Wang, Z. & Bhattacharyya, T. Outcomes of hemiarthroplasty and total hip arthroplasty for femoral neck fracture: A medicare cohort study. J. Orthop. Trauma 31, 260–263 (2017).
Lewis, D. P., Wæver, D., Thorninger, R. & Donnelly, W. J. Hemiarthroplasty vs total hip arthroplasty for the management of displaced neck of femur fractures: A systematic review and meta-analysis. J. Arthroplasty 34, 1837-1843.e2 (2019).
Hansson, S., Bülow, E., Garland, A., Kärrholm, J. & Rogmark, C. More hip complications after total hip arthroplasty than after hemi-arthroplasty as hip fracture treatment: Analysis of 5,815 matched pairs in the Swedish Hip Arthroplasty Register. Acta Orthop. https://doi.org/10.1080/17453674.2019.1690339 (2019).
Dorr, L. D., Glousman, R., Hoy, A. L., Vanis, R. & Chandler, R. Treatment of femoral neck fractures with total hip replacement versus cemented and noncemented hemiarthroplasty. J. Arthroplasty 1, 21–28 (1986).
Corten, K., Bourne, R. B., Charron, K. D., Au, K. & Rorabeck, C. H. What works best, a cemented or cementless primary total hip arthroplasty?: Minimum 17-year followup of a randomized controlled trial. Clin. Orthop. 469, 209–217 (2011).
Parker, M. J. & Cawley, S. Cemented or uncemented hemiarthroplasty for displaced intracapsular fractures of the hip: A randomized trial of 400 patients. Bone Jt. J. 102-B, 11–16 (2020).
Chen, K. K. et al. Cemented compared with uncemented femoral fixation in the arthroplasty treatment of displaced femoral neck fractures: A critical analysis review. JBJS Rev. 6, e6 (2018).
Nantha Kumar, N. et al. Effectiveness and safety of cemented and uncemented hemiarthroplasty in the treatment of intracapsular hip fractures. Bone Jt. J. 102-B, 1113–1121 (2020).
Richardson, C. G., Lethbridge, L. N. & Dunbar, M. J. Increased mortality with the use of cementless fixation for femoral neck fractures: Analysis of 5883 hip arthroplasty cases. J. Arthroplasty https://doi.org/10.1016/j.arth.2020.07.006 (2020).
Scailteux, L.-M. et al. French administrative health care database (SNDS): The value of its enrichment. Therapie 74, 215–223 (2019).
Tuppin, P. et al. Value of a national administrative database to guide public decisions: From the système national d’information interrégimes de l’Assurance Maladie (SNIIRAM) to the système national des données de santé (SNDS) in France. Rev. Epidemiol. Sante Publique 65(Suppl 4), S149–S167 (2017).
Tuppin, P., de Roquefeuil, L., Weill, A., Ricordeau, P. & Merlière, Y. French national health insurance information system and the permanent beneficiaries sample. Rev. Epidemiol. Sante Publique 58, 286–290 (2010).
Goldberg, M. et al. The opening of the French national health database: Opportunities and difficulties. The experience of the Gazel and Constances cohorts. Rev. Epidemiol. Sante Publique 64, 313–320 (2016).
Suarez, J. C. et al. Hemiarthroplasty vs total hip arthroplasty for femoral neck fractures: 2010–2017 trends in complication rates. J. Arthroplasty 35, S262–S267 (2020).
Rodriguez-Buitrago, A. et al. Hemiarthroplasty for femoral neck fracture. JBJS Essent. Surg. Tech. 9, e13 (2019).
Austin, S. R., Wong, Y.-N., Uzzo, R. G., Beck, J. R. & Egleston, B. L. Why summary comorbidity measures such as the Charlson comorbidity index and Elixhauser score work. Med. Care 53, e65-72 (2015).
Roussel, A. et al. A comparison of individual and ecological indicators of social deprivation and their association with hospital efficiency in the context of infectious diseases in two French general paediatric departments. Int. Health https://doi.org/10.1093/inthealth/ihz102 (2020).
Rey, G., Jougla, E., Fouillet, A. & Hémon, D. Ecological association between a deprivation index and mortality in France over the period 1997–2001: Variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health 9, 33 (2009).
Lewis, P. M. & Waddell, J. P. When is the ideal time to operate on a patient with a fracture of the hip? A review of the available literature. Bone Jt. J. 98, 1573–1581 (2016).
Squires, B. & Bannister, G. Displaced intracapsular neck of femur fractures in mobile independent patients: total hip replacement or hemiarthroplasty?. Injury 30, 345–348 (1999).
Keating, J. F., Grant, A., Masson, M., Scott, N. W. & Forbes, J. F. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J. Bone Joint Surg. Am. 88, 249–260 (2006).
Fokter, S. K. & Fokter, N. Hip fracture in the elderly: Partial or total arthroplasty? in Recent Advances in Hip and Knee Arthroplasty (ed. Fokter, S.) (InTech, 2012). https://doi.org/10.5772/31279.
Mariconda, M. et al. Ambulatory ability and personal independence after hemiarthroplasty and total arthroplasty for intracapsular hip fracture: A prospective comparative study. J. Arthroplasty 32, 447–452 (2017).
DeRogatis, M. J., Piatek, A. Z., Jacob, R., Kelly, S. C. & Issack, P. S. Hemiarthroplasty for femoral neck fractures in the elderly: A comparison of cemented and uncemented femoral Stems. JBJS Rev. 8, e1900192 (2020).
Bonfait, H. et al. Bone cement implantation syndrome in hip arthroplasty: Frequency, severity and prevention. Orthop. Traumatol. Surg. Res. OTSR 108, 103139 (2022).
Berggren, M., Stenvall, M., Englund, U., Olofsson, B. & Gustafson, Y. Co-morbidities, complications and causes of death among people with femoral neck fracture—A three-year follow-up study. BMC Geriatr. 16, 120 (2016).
Bellamy V. « Les décès en 2016 », Insee Résultats, octobre 2017.
Acknowledgements
The authors want to thank the public teaching hospital of Marseille for the funding of the study and the team of the public healthcare service for their technical supply in statistical analysis and data collection.
Funding
All funds required for the study were sponsored by the Public Hospitals of Marseille France.
Author information
Authors and Affiliations
Contributions
C.P.: data collection, design of the study, writing. C.J.: design of the study. V.P.: statistical analysis. V.O.: statistical analysis. L.B.: design of the study. R.K.: English native speaker correction. J.N.A.: design of the study. M.O.: design of the study, writing corrections. All authors consent to publish the submitted work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pangaud, C., Pauly, V., Jacquet, C. et al. Reduced mortality associated to cementless total hip arthroplasty in femoral neck fracture. Sci Rep 13, 16849 (2023). https://doi.org/10.1038/s41598-023-43790-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43790-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.