Abstract
Cerebral hypoxia is an important cause of secondary brain injury. Improving systemic oxygenation may increase brain tissue oxygenation (PbtO2). The effects of increased positive end-expiratory pressure (PEEP) on PbtO2 and intracranial pressure (ICP) needs to be further elucidated. This is a single center retrospective cohort study (2016–2021) conducted in a 34-bed Department of Intensive Care unit. All patients with acute brain injury under mechanical ventilation who were monitored with intracranial pressure and brain tissue oxygenation (PbtO2) catheters and underwent at least one PEEP increment were included in the study. Primary outcome was the rate of PbtO2 responders (increase in PbtO2 > 20% of baseline) after PEEP increase. ΔPEEP was defined as the difference between PEEP at 1 h and PEEP at baseline; similarly ΔPbtO2 was defined as the difference between PbtO2 at 1 h after PEEP incrementation and PbtO2 at baseline. We included 112 patients who underwent 295 episodes of PEEP increase. Overall, the median PEEP increased form 6 (IQR 5–8) to 10 (IQR 8–12) cmH2O (p = 0.001), the median PbtO2 increased from 21 (IQR 16–29) mmHg to 23 (IQR 18–30) mmHg (p = 0.001), while ICP remained unchanged [from 12 (7–18) mmHg to 12 (7–17) mmHg; p = 0.42]. Of 163 episode of PEEP increments with concomitant PbtO2 monitoring, 34 (21%) were PbtO2 responders. A lower baseline PbtO2 (OR 0.83 [0.73–0.96)]) was associated with the probability of being responder. ICP increased in 142/295 episodes of PEEP increments (58%); no baseline variable was able to identify this response. In PbtO2 responders there was a moderate positive correlation between ΔPbtO2 and ΔPEEP (r = 0.459 [95% CI 0.133–0.696]. The response in PbtO2 and ICP to PEEP elevations in brain injury patients is highly variable. Lower PbtO2 values at baseline could predict a significant increase in brain oxygenation after PEEP increase.
Similar content being viewed by others
Introduction
Prevention, identification and early treatment of secondary brain injury is an important aspect of the management of acute brain injury (ABI) in order to improve outcome1. Cerebral hypoxia is an important cause of secondary brain injury and can frequently affect ABI patients with both traumatic and non-traumatic etiology2,3,4,5,6. Indeed, low brain tissue partial pressure of oxygen (PbtO2) has been associated with cerebral anaerobic metabolism, increased risk of mortality and poor functional outcome7,8,9,10,11,12,13.
PbtO2 is a focal measurement of brain oxygenation reflecting an equilibrium between oxygen delivery (i.e. cerebral blood flow, CBF, hemoglobin and arterial oxygenation), consumption (i.e. brain metabolism, mitochondrial function and body temperature) and extraction (i.e. microcirculation and mitochondrial function)14,15. Therefore, different pathophysiological mechanisms are associated with low PbtO2 after acute brain injury, such as reduced CBF and/or cerebral perfusion pressure (CPP), intracranial hypertension (IH), hypoxemia, anemia, altered microcirculation or excessive cellular metabolism16. Hypoxemia itself has also been associated with poor outcomes after traumatic brain injury17,18. Therefore, strategies aiming at improving hypoxemia may be useful in this setting.
In patient undergoing mechanical ventilation, applying a positive end-expiratory pressure (PEEP) has been shown to reduce end-expiratory alveolar collapse, maintaining alveolar recruitment and possibly reduce the incidence of ventilator-associated pneumonia and lung injury19,20,21,22. These effects are more pronounced in patients with acute respiratory distress syndrome (ARDS)23,24. By improving systemic oxygenation, increased PEEP could improve brain tissue oxygenation. However, the existing literature is scarce. Small studies have shown an increase in PbtO2 following increases in PEEP and recruitment manouvers25,26, while others have not27. Moreover, while PEEP may increase PbtO2 by increasing systemic oxygenation, it can potentially also increase ICP, by reducing cerebral venous outflow due to increased intrathoracic pressure28, or decrease mean arterial pressure (MAP), by impairing venous return to the heart27,29.
Therefore, the aim of this study was to assess the impact of increase in PEEP levels on PbtO2 and ICP in ABI patients. The secondary aim was to identify baseline factors associated with PbtO2 increase and ICP increase.
Methods
Study design
This was a single center retrospective cohort study conducted at the Intensive Care Unit (ICU) of the Hôpital Universitaire de Bruxelles (HUB), in Brussels, Belgium, from January 2016 to December 2021. The study protocol was approved by Erasme Hospital Ethics Committee (P2022/449) and the need for informed written consent was waived, because of the anonymized data collection of retrospective data. This study was carried out in accordance with the Strengthening The Reporting of Observational studies in Epidemiology (STROBE) statement30.
Study population
We screened adult (> 18 years) patients admitted to the ICU due to an acute brain injury. Inclusion criteria were: (a) traumatic brain injury (TBI) or aneurysmal subarachnoid hemorrhage (aSAH) patients under controlled mechanical ventilation; (b) the presence of ICP and PbtO2 monitoring within the first 48 h of admission and (c) patients underwent at least one increase in PEEP levels concomitantly with the use of neuromonitoring. Patients with imminent death were excluded.
Patients’ management
We followed the current guidelines for the management of TBI31 and SAH32; invasive multimodal monitoring, including PbtO2, was implemented according to recent consensus1. PbtO2 monitoring is considered as “standard of care” for ABI patients with a Glasgow Coma Score (GCS) < 9 and requiring intracranial pressure (ICP) monitoring; PbtO2 probes were placed in the frontal region of the hemisphere at greatest risk for secondary brain injury. In TBI patients, probe was placed close < 5 cm to the most injured/contused area in TBI; in SAH patients probes were placed in the region at risk or with demonstrated delayed cerebral ischemia for aSAH). Probes were inserted through a frontal burr hole using a triple-lumen bolt. PbtO2 was monitored continuously using a specific probe and the Integra Licox® Brain Tissue Oxygen Monitoring System (IM3.ST_EU, Integra LifeSciences Corporation, Plainsboro, NJ, USA). Probe location was confirmed by a cerebral CT-scan performed within 24 h from neuromonitoring placement. The adequate functioning of the probe was tested with a 100% oxygen fraction (FiO2) test for 15 min (i.e. an increase of at least 5 mmHg of PbtO2 indicated an adequate catheter function). Intracranial pressure probes were placed either intraventricular or intraparenchymal.
PEEP trials
PEEP was increased according to the decision of the critical care team responsible for the treatment of the patient. There was no standardized protocol. However, PEEP was increased in increments of 2 mmHg for at least 1 h-aiming at improving systemic oxygenation (targeting an improvement in arterial partial pressure of oxygen and inspired fraction of oxygen ration) and respiratory mechanics while minimizing ventilator induced lung injury33 by implementing a lung protective ventilation strategy and targeting Plateau pressure < 30 mmHg and driving pressure < 15 mmHg34. If after one 1 h of PEEP incrementation there was no benefit in oxygenation or if there were deleterious effects on respiratory mechanics or persistent hemodynamic instability, PEEP was reversed to baseline setting. The decision on the amount of PEEP to incrementation was done by the respiratory therapist in agreement with the treatment treating physician. No FiO2 changes were implemented during the PEEP trial.
Data collection
Physiological variables, ICP and PbtO2 were measured in real-time and collected prospectively on a patient data monitoring system. Cerebral perfusion pressure (CPP) was calculated as the difference between MAP and ICP; MAP was zeroed at the level of the left atrium. Intracranial hypertension was defined as ICP value above 20 mmHg for at least 5 min at any time. Brain tissue hypoxia was defined as a PbtO2 < 20 mmHg for at least 5 min.
Baseline (T0) was defined as the hour immediately preceding a PEEP change and T1 was defined as the first 1 h with the new stable PEEP value. The 60-min mean of value of the following continuous variables was collected at T0 and T1: mean arterial pressure (MAP), heart rate (HR), ICP, CPP and PbtO2. ICP and PbtO2 were recorded prospectively every minute. Data was extracted from the monitoring system and the mean value of ICP and PbtO2 was calculated for every hour of monitoring.
ICP and PbtO2 changes (ΔICP and ΔPbtO2) were calculated as the difference between ICP or PbtO2 at T1 and T0. A “decrease” in ICP or PbtO2 was identified as a ΔICP/ΔPbtO2 < 0; a “stable” value as a ΔICP/ΔPbtO2 = 0 and an “increase” as a ΔICP/ΔPbtO2 > 0. Patients with a PbtO2 increase of more than 20% from baseline were considered as “responders”; a significant increase in ICP was defined as an increase of more than 20% from baseline or an increase that led to intracranial hypertension. The following ventilator parameters were recorded at T0 and T1: inspiratory pressure (Pins); tidal volume (VT), PEEP; respiratory rate (RR) and inspired fraction of oxygen (FiO2). Arterial oxygen saturation (SaO2), lactate, pH, PaCO2, PaO2 were also recorded.
We collected demographics, the presence of comorbidities, sequential organ failure assessment (SOFA)35 and the Glasgow coma scale (GCS)36 on admission. Hospital mortality and the Glasgow Outcome Scale (GOS)37 at 3 months were collected, as previously reported38. Unfavorable neurological outcome (UO) was defined as GOS of 1–3.
Study outcomes
The primary outcome was the proportion of PbtO2 responders. Secondary outcomes included: (a) the proportion of patients with an increase of ICP > 20% or an increase in ICP that resulted in intracranial hypertension after PEEP augmentation; (b) the correlation between the difference of PEEP at T1 and T0 (ΔPEEP) and ΔICP/ΔPbtO2; (c) baseline factors associated with significant increases in PbtO2 and ICP after PEEP augmentation; (d) the proportion of patients with an decrease in CPP resulting on a CPP < 60 mmHg; (e) differences between the trends in PbtO2 and ICP during PEP incrementation challenge in SAH and TBI patients.
Statistical analysis
Descriptive statistics were computed for all variables. Categorical variables were described as proportions (%) and compared using Chi square or Fisher’s exact test. Normality was assessed using the Kolmogorov–Smirnov test. Normally distributed variables were expressed as mean (± SD) and compared using Student t test while non-gaussian continuous variables were described median [IQRs] and compared using Mann–Whitney test (independent variables) or Wilcoxon test (repeated measures of related variables). A Spearman correlation was computed between ΔPEEP, ΔPbtO2, ΔICP, ΔCPP and ΔPaO2. As a sensitivity analysis we also considered just the first PEEP increment of each patient to calculate the correlation between ΔPEEP, ΔPbtO2, ΔICP, ΔCPP and ΔPaO2. To account for multiple measures per patient a generalized mixed model with logit link was used to identify baseline variables which were independently associated with a PbtO2 responder and a significant increase in ICP after PEEP increment; baseline variables with a p value < 0.1 in the univariate analysis were included in the multivariable analysis. Odds ratios (ORs) with 95% confidence intervals (CIs) were computed for all variables. The independence of errors, presence of multicollinearity and of influential outlier assumptions were checked; none were violated. A receiver operator curve was designed to assess the sensitivity and specificity of baseline PbtO2 to identify responders. The area under the curve (AUROC) and CI 95% were computed. Youden’s test was used to identify the cut-off with the best sensitivity and specificity. We used a similar model to identify variables associated with an absolute increase in PbtO2 and ICP after PEEP increments. All statistical analyses were performed using SPSS 27.0 for MacIntosh. A p value < 0.05 was considered significant.
Ethics approval and consent to participate
The study protocol was approved by local ethics Committees (Erasme Hospital: P2022/449) and informed written consent was waived. All methods were carried out in accordance with relevant scientific and ethical guidelines and regulations.
Results
Study population
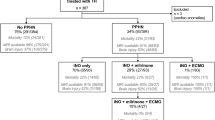
Over a total of 237 patients monitored with ICP and PbtO2 during the study period, 112 patients (TBI, n = 47 [42%]; SAH, n = 65 [58%]) had an increase in PEEP values under controlled mechanical ventilation (a total of 295 PEEP increase for ICP and 163 for PbtO2, as in some patients PbtO2 catheter was removed). The characteristics of the population are shown in Table 1. Mean age and median GCS on admission were 51(± 15) years and 5 (3–9), respectively. During the ICU stay, intracranial hypertension occurred in 89/112 patients (79%) and brain tissue hypoxia occurred in 94/112 (84%). A total of 59 (53%) of patients died in the hospital and 97 (87%) had unfavorable outcome. Table 2 shows ventilatory parameters and physiological variables at T0 and T1; PEEP was increased from 6 (5–8) to 10 (8–12) cmH2O (p = 0.001); PbtO2 significantly increased from 21 (16–29) to 23 (18–30) mmHg (p = 0.001), while ICP remained stable over time, varying from 12 (7–18) to 12 (7–17) mmHg (p = 0.42), as shown in Fig. 1. During the same time-period, MAP and CPP remained unchanged.
Variations of intracranial hypertension and of brain tissue oxygenation (PbtO2) before (T0) and after (T1) increments in positive end expiratory pressure (PEEP). PEEP changed from 6 cmH2O (5–8) to 10 cmH2O (8–12), p = 0.001. ICP varied from 12 mmHg (7–18) to 12 mmHg (7–17), p = 0.42. PbtO2 changed from 21 mmHg (16–29) to 23 mmHg (18–30), p = 0.001.
PEEP augmentation and PbtO2 values
There was an absolute increase in PbtO2 in 102/163 (63%) episodes of PEEP augmentation; in 30 (18%) episodes, there were no changes in PbtO2, while in 31 (19%) episodes there was a decrease in PbtO2. Baseline PbtO2 was below 20 mmHg in 63/163 (39%) episodes. Higher baseline PaO2 (OR 1.02 [95% CI 1.01–1.03]) and lower baseline PbtO2 (OR 0.92 [95% CI 0.91–0.94]) were independently associated with any increase in PbtO2 after PEEP augmentation (Supplemental Tables S1 and S2).
There was no correlation between ΔPEEP and ΔPbtO2 (r = 0.084 [95% CI − 0.075 to 0.24], Supplemental Fig. S1A), even when we considered only the first measure per patient (r = 0.197 [95% CI − 0.100 to 0.425], Supplemental Fig. S1B). Considering all measurements, there was a weak correlation between ΔPbtO2 and ΔPaO2 (r = 0.223 [95% CI 0.030 to 0.400]); considering only the first measure per patient, a weak correlation between ΔPbtO2 and ΔPaO2 was observed (r = 0.275 [95% CI 0.0254 to 0.530]).
PbtO2 responders
We identified 34/163 (21%) PbtO2 responders after PEEP incrementation; lower levels of baseline PbtO2 were associated with being a responder (Table 3: OR 0.83 95% CI 0.73–0.95, p = 0.009). Baseline PbtO2 had an AUROC of 0.83 (0.76–0.89) to predict PbtO2 responder after PEEP augmentation (Fig. 2); the baseline PbtO2 cut-off with the best sensitivity (91.2%) and specificity (66.7%) was 21 mmHg.
In PbtO2 responders, there was a moderate positive correlation between ΔPbtO2 and ΔPEEP (r = 0.459 [95% CI 0.133 to 0.696]), ΔPbtO2 and ΔPaO2 (r = 0.382 [95% CI 0.001 to 0.672]), while no correlation between ΔPbtO2 and ΔCPP was found (r = − 0.027 [95% CI − 0.371 to 0.324]), as shown in Fig. 3A. In non-responders, there was a weak correlation between ΔPbtO2 and ΔCPP (r = 0.196 [95% CI 0.019 to 0.361]), ΔPbtO2 and ΔPaO2 (r = 0.213 [95% CI 0.012 to 0.418]), while no correlation between ΔPbtO2 and ΔPEEP was observed (r = 0.002 [95% CI − 0.176 to 0.180]—Fig. 3B).
PEEP augmentation and ICP values
In 142/295 (48%) episodes of PEEP augmentation, there was an absolute increase in ICP. Baseline ICP was above 20 mmHg in 49/295 episodes (17%). No baseline factors were associated with an absolute ICP increase after PEEP augmentation (Supplemental Tables S3). There was no correlation between ΔPEEP and ΔICP (r = − 0.07 [95% CI − 0.18 to 0.05], Supplemental Fig. S1A), while a moderate inverse correlation between ΔICP and ΔCPP (r = − 0.310 [95% CI − 0.413 to − 0.200]) was observed. When only the first measure per patient was considered, no correlation between ΔPEEP and ΔICP was found (r = − 0.112 [95% − 0.297 to 0.080), while there was a moderate inverse correlation between ΔICP and ΔCPP (r = − 0.403[95% − 0.552 to − 0.230], Supplemental Fig. S1B).
Patients with significant ICP increase
A significant increase in ICP was observed in 109/295 (37%) episodes of PEEP incrementation. In 23/109 (21%) episodes of significant ICP increase there was an ICP increase > 20% resulting in an ICP > 20 mmHg at T1. No baseline factors were associated with a significant ICP increase (Table 4). In patients with a significant increase in ICP (Supplemental Fig. S2A), no correlation between ΔPEEP and ΔICP (r = − 0.063 [95% CI − 0.53 to 0.132) was observed, but there was a weak inverse correlation between ΔICP and ΔCPP (r = − 0.239 [95% CI − 0.413 to − 0.047). In the other patients (Supplemental Fig. S2B), no correlation between ΔPEEP and ΔICP (r = − 0.039 [95% CI − 0.186 to 0.109) was observed, but there was a weak inverse correlation between ΔICP and ΔCPP (r = − 0.195[95% CI − 0.334 to − 0.049).
Of note, in only 4/295 (1.4%) episodes of PEEP incrementation resulted in a CPP of < 60 mmHg.
A significant CPP reduction (T1 CPP < 60 mmhg) was observed in /295.
Subarachnoid hemorrhage and TBI
In TBI patients (n = 48) PEEP was increased from 5 (5–8) to 10 (8–12) cmH2O (p = 0.001); PbtO2 significantly increased from 20 (15–25) to 22 (18–28) mmHg (p = 0.001), while ICP did not vary significantly over [from 13 (7–18) to 12 (7–16) mmHg (p = 0.56)]. CPP also remained stable over time [ from 86 (78–95) to 85 (74–95) mmHg (p = 0.50]. There was an absolute increase in PbtO2 in 42/59 (71%) episodes of PEEP augmentation; however, only in 13 (22%) episodes there was a significant increase in PbtO2 (PbtO2 responders). In 11 (17%) episodes, there were no changes in PbtO2 while in 6 (10%) episodes there was a decrease in PbtO2. In 52/122 (43%) episodes of PEEP augmentation in TBI patients, there was an absolute increase in ICP, while a significant increase in ICP was observed in 38/122 (31%) episodes.
In SAH patients (n = 65) PEEP was increased from 6 (5–8) to 10 (8–12) cmH2O (p = 0.001); PbtO2 significantly increased from 23 (16–32) to 24 (18–32) mmHg (p = 0.001), while ICP did not vary significantly over [from 12 (7–18) to 12 (7–18) mmHg (p = 0.24)]. CPP also remained stable over time [from 96 (82–110) to 96 (79–110) mmHg (p = 0.73]. There was an absolute increase in PbtO2 in 60/104 (58%) episodes of PEEP augmentation; however, we identified only in 21/104 (20%) PbtO2 responders. In 19/104 (18%) episodes, there were no changes in PbtO2 while in 25/104 (24%) episodes there was a decrease in PbtO2. In 52/173 (31%) episodes of PEEP augmentation in SAH patients, there was an absolute increase in ICP, while a significant increase in ICP was observed in 54/122 (26%) episodes.
Patient with TBI and SAH had similar trends regarding PbtO2 and ICP variation of time after PEEP challenges as shown in Supplemental Fig. S3.
Discussion
In this study, we observed a significant elevation in PbtO2 in 35% of episodes following an increase in PEEP; a lower baseline PbtO2 was found to be associated with a significant increase in brain oxygenation. We determined that a baseline PbtO2 cut-off of 21 mmHg was optimal for identifying PbtO2 responders to PEEP. Additionally, we observed a moderate correlation between changes in PEEP and changes in PbtO2, specifically within the group of PbtO2 responders. Interestingly, we did not identify any baseline factors associated with a significant increase in ICP, which was observed in 37% cases following PEEP augmentation.
Mechanical ventilation is often required for patients with severe TBI and poor-grade SAH due to various factors, such as coma, compromised airway protection, risk of aspiration, seizures, elevated ICP, pulmonary dysfunction, and respiratory failure resulting from pre-existing conditions or new complications37. The use of PEEP is a crucial component of ventilation strategies in this context. Recent consensus guidelines38 suggest that in acute brain injury patients without acute respiratory failure, PEEP levels should be similar to those used in patients without brain injury, and lung protective ventilation strategies can be employed. In patients with both respiratory failure and acute brain injury, lung protective ventilation and higher levels of PEEP may be utilized, as long as clinically significant increases in ICP are not observed. However, there are currently no specific recommendations provided for patients with acute brain injury, respiratory failure and intracranial hypertension38.
These consensus guidelines have also recommended targeting a PaO2 range of 80–120 mmHg to avoid both hypoxemia and hyperoxia38. Positive end-expiratory pressure plays a crucial role in increasing lung functional residual capacity, preventing alveolar de-recruitment, and improving oxygenation37. Therefore, increasing PEEP can be a strategy to enhance oxygenation in these patients. Another important consideration in setting PEEP is PbtO2, as avoiding cerebral hypoxia, in addition to systemic hypoxemia, is crucial in preventing secondary brain injury in neurocritical care. Additionally, acute lung injury has been associated with brain tissue hypoxia39. However, there is limited research on the impact of PEEP on brain oxygenation.
One study involving 20 TBI patients with ARDS demonstrated that increasing PEEP from 5 to 10 to 15 cmH2O resulted in significant increases in PbtO2 and oxygen saturation, without affecting ICP or CPP in patients without baseline intracranial hypertension25. Another study with 10 SAH patients showed that applying PEEP of 20 cmH2O resulted in a decrease in PbtO2 due to a simultaneous decrease in CPP and cerebral blood flow, which was reversed upon restoration of MAP27. Furthermore, a study involving a mixed population of SAH and TBI patients with ARDS demonstrated that recruitment maneuvers and high levels of PEEP significantly improved both systemic and brain tissue oxygenation, leading to reduced oxygen requirements26. In our study, increasing PEEP improved PbtO2, particularly in patients with low baseline PbtO2. Similar responses have been observed with other strategies aimed at enhancing interstitial oxygen availability in acute brain injury patients, such as red blood cell transfusion40.
The application of PEEP can have an impact on cardiovascular physiology by increasing intrathoracic pressure; this can potentially decrease venous return, reduce cardiac output, and lead to hypotension, particularly in hypovolemic patients41. Hypotension is a significant cause of secondary brain injury, as it can reduce CPP and induce ischemia42,43. Previous studies that reported negative effects of PEEP on CPP are typically associated with decreased mean arterial pressure27,28,44,45,46. In our study, both MAP and CPP remained unchanged. It is important to note that increased intrathoracic pressure can lead to decreased cerebral venous drainage, which may elevate ICP28. Additionally, higher levels of PEEP and low tidal volumes can result in increased arterial carbon dioxide levels, potentially causing cerebral vasodilation and a subsequent increase in ICP47. Consequently, numerous studies have investigated the effects of PEEP on ICP and cerebral hemodynamics.
Wolf et al. demonstrated that employing an open lung strategy with PEEP appears to be safe in patients with acute brain injury and concomitant ARDS, as evidenced by no significant changes in ICP in a small case series (n = 11)48. Boone et al. showed minimal effects of PEEP on ICP in patients without severe lung injury, and even in severe lung injury patients, the increase in ICP due to PEEP was considered clinically irrelevant44. Other studies conducted in patients with ischemic stroke and TBI have also indicated that the response of ICP to PEEP, although variable, is moderate at best and lacks clinical impact, suggesting that PEEP can be safely utilized in acute brain injury patients when indicated27,29,45,49,50,51,52. These findings are consistent with our study. However, an older study reported a significant increase in ICP after increments in PEEP among head-injured patients, which had neurological repercussions and necessitated immediate reduction in PEEP28.
The impact of PEEP on ICP appears to be influenced by the presence of baseline intracranial hypertension. One study that analyzed changes in ICP after incremental increases in PEEP found that in patients with baseline intracranial hypertension, higher PEEP levels did not affect ICP, while in patients with normal ICP, PEEP levels of 10 and 15 cmH2O resulted in increases in ICP without clinical relevance, as CPP remained stable and above 60 mmHg50. Other studies have shown that in patients with ICP > 20 mmHg, ICP decreased or remained stable after PEEP increments, while CPP remained unchanged or even increased in some cases45,52. In our study, significant increases in ICP due to PEEP increments were observed in 37% (109/295) of episodes, with an ICP exceeding 20 mmHg in 34% (37/109) of episodes. However, baseline ICP was not found to be an independent factor associated with ICP increases following PEEP increments. We were unable to identify any baseline factors that could predict changes in ICP in response to PEEP. Similarly, a recent study also failed to identify baseline factors that could help identify patients at higher risk for ICP increases following PEEP changes46.
Another factor that appears to influence ICP responses to variations in PEEP is lung compliance. In patients with low compliance, as is often the case in ARDS patients, higher levels of PEEP had no impact on CPP, ICP or cerebral blood flow53. Conversely, in patients with normal compliance, there was a decrease in CPP and cerebral blood flow, but no changes in ICP45. A recent study has demonstrated that changes in ICP are inversely correlated with lung recruitability after PEEP application and recruitment maneuvers, suggesting that patients who would benefit from higher PEEP levels will have minimal side effects on intracranial pressure46. This can be explained by the fact that the detrimental effects of PEEP are related to alveolar hyperinflation, leading to a significant increase in arterial carbon dioxide and intrathoracic pressure. Conversely, when PEEP leads to alveolar recruitment, improved lung gas distribution, and optimization of ventilation/perfusion matching, ICP remains unchanged46. In our study, PaCO2 remained stable and within the normal range, which may explain why overall ICP remained unchanged.
Our study has several limitations that should be acknowledged. Firstly, we did not perform a formal sample size calculation, which may have limited the power of our study and prevented us from drawing definitive conclusions. Additionally, this was a single-center study, and therefore, the generalizability of our findings to other centers may be limited. Due to the limited number of events, we were unable to conduct further subgroup analyses, such as comparing patients with baseline tissue hypoxia, baseline intracranial hypertension or differentiating those with ARDS from those without ARDS, which could provide valuable insights into specific patient populations. Another limitation is that we did not specifically assess the correlation between increases in PbtO2 after PEEP increments and functional outcomes. Moreover, the retrospective design of our study prevents us from ruling out the potential influence of other concurrent interventions, sedation, or vasopressor therapy, which may have contributed to the observed changes in PbtO2 following PEEP increments. Additionally, we lack information on the specific reasons for PEEP changes, as these were determined by the clinical care team. Importantly, we were unable to assess change in respiratory mechanics (such as lung compliance) and correlate them to PbtO2 and ICP due to the retrospective nature of this study. Furthermore, the magnitude of PEEP changes in our study was generally small, which could have impacted our results. Moreover, due to how the data was collected (1 h mean) we were unable to perform a time series analysis of the impact of PEEP incrementation on physiological variables. It is also important to note that while PbtO2 may assess interstitial oxygen availability, its influence on cellular oxygenation in the brain remains uncertain. Lastly, our findings are not conclusive, as the heterogeneity of our study cohort, which included both traumatic and non-traumatic brain injury patients, and the placement of the probe in hypo perfused cerebral areas (which are more sensitive to interventions aiming to improve oxygen delivery), as well as the use of regional rather than global oxygen monitoring, raise significant issues that should be addressed in future studies on this topic.
Conclusions
In this study, implementing PEEP to enhance PbtO2 could be a viable approach in patients with acute brain injury, particularly those presenting with baseline tissue hypoxia. However, it is crucial to closely monitor ICP and systemic hemodynamics to ensure the safe and appropriate administration of PEEP.
Data availability
Due to ethical restrictions, the datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
LeRoux, P. et al. Consensus summary statement of the international multidisciplinary consensus conference on multimodality monitoring in neurocritical care: A statement for healthcare professionals from the neurocritical care society and the European society of intensive care medicine. Intensive Care Med. 40, 1189–1209. https://doi.org/10.1007/s00134-014-3369-6 (2014).
Lazaridis, C., Rusin, C. G. & Robertson, C. S. Secondary brain injury: Predicting and preventing insults. Neuropharmacology 145, 145–152. https://doi.org/10.1016/j.neuropharm.2018.06.005 (2019).
O’Leary, R. A. & Nichol, A. D. Pathophysiology of severe traumatic brain injury. J. Neurosurg. Sci. 62, 542–548. https://doi.org/10.23736/s0390-5616.18.04501-0 (2018).
Taufique, Z. et al. Predictors of poor quality of life 1 year after subarachnoid hemorrhage. Neurosurgery 78, 256–264. https://doi.org/10.1227/neu.0000000000001042 (2016).
Lazaridis, C. & Robertson, C. S. The role of multimodal invasive monitoring in acute traumatic brain injury. Neurosurg. Clin. N. Am. 27, 509–517. https://doi.org/10.1016/j.nec.2016.05.010 (2016).
Rosengart, A. J., Schultheiss, K. E., Tolentino, J. & Macdonald, R. L. Prognostic factors for outcome in patients with aneurysmal subarachnoid hemorrhage. Stroke 38, 2315–2321. https://doi.org/10.1161/strokeaha.107.484360 (2007).
Oddo, M. et al. Brain hypoxia is associated with short-term outcome after severe traumatic brain injury independently of intracranial hypertension and low cerebral perfusion pressure. Neurosurgery 69, 1037–1045. https://doi.org/10.1227/NEU.0b013e3182287ca7 (2011) (Discussion 1045).
Bardt, T. F. et al. Monitoring of brain tissue PO2 in traumatic brain injury: Effect of cerebral hypoxia on outcome. Acta Neurochir. Suppl. 71, 153–156 (1998).
van den Brink, W. A. et al. Brain oxygen tension in severe head injury. Neurosurgery 46, 868–876. https://doi.org/10.1097/00006123-200004000-00018 (2000) (Discussion 876–868).
Maloney-Wilensky, E. et al. Brain tissue oxygen and outcome after severe traumatic brain injury: A systematic review. Crit. Care Med. 37, 2057–2063. https://doi.org/10.1097/CCM.0b013e3181a009f8 (2009).
Kett-White, R. et al. Adverse cerebral events detected after subarachnoid hemorrhage using brain oxygen and microdialysis probes. Neurosurgery 50, 1213–1221. https://doi.org/10.1097/00006123-200206000-00008 (2002) (Discussion 1221–1212).
Vath, A., Kunze, E., Roosen, K. & Meixensberger, J. Therapeutic aspects of brain tissue PO2 monitoring after subarachnoid hemorrhage. Acta Neurochir. Suppl. 81, 307–309 (2002).
Chen, H. I. et al. Detection of cerebral compromise with multimodality monitoring in patients with subarachnoid hemorrhage. Neurosurgery 69, 53–63. https://doi.org/10.1227/NEU.0b013e3182191451 (2011) (Discussion 63).
Rose, J. C., Neill, T. A. & Hemphill, J. C. 3rd. Continuous monitoring of the microcirculation in neurocritical care: An update on brain tissue oxygenation. Curr. Opin. Crit. Care 12, 97–102. https://doi.org/10.1097/01.ccx.0000216574.26686.e9 (2006).
Soehle, M., Jaeger, M. & Meixensberger, J. Online assessment of brain tissue oxygen autoregulation in traumatic brain injury and subarachnoid hemorrhage. Neurol. Res. 25, 411–417. https://doi.org/10.1179/016164103101201580 (2003).
Haitsma, I. K. & Maas, A. I. Advanced monitoring in the intensive care unit: brain tissue oxygen tension. Curr. Opin. Crit. Care 8, 115–120. https://doi.org/10.1097/00075198-200204000-00005 (2002).
Chesnut, R. M. et al. The role of secondary brain injury in determining outcome from severe head injury. J. Trauma 34, 216–222. https://doi.org/10.1097/00005373-199302000-00006 (1993).
Manley, G. et al. Hypotension, hypoxia, and head injury: Frequency, duration, and consequences. Arch. Surg. 136, 1118–1123. https://doi.org/10.1001/archsurg.136.10.1118 (2001).
Manzano, F. et al. Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients. Crit. Care Med. 36, 2225–2231. https://doi.org/10.1097/CCM.0b013e31817b8a92 (2008).
Neto, A. S. et al. Epidemiological characteristics, practice of ventilation, and clinical outcome in patients at risk of acute respiratory distress syndrome in intensive care units from 16 countries (PRoVENT): An international, multicentre, prospective study. Lancet Respir. Med. 4, 882–893. https://doi.org/10.1016/S2213-2600(16)30305-8 (2016).
Yi, H. et al. Higher PEEP versus lower PEEP strategies for patients in ICU without acute respiratory distress syndrome: A systematic review and meta-analysis. J. Crit. Care 67, 72–78. https://doi.org/10.1016/j.jcrc.2021.09.026 (2022).
Acute Respiratory Distress Syndrome et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 342, 1301–1308. https://doi.org/10.1056/NEJM200005043421801 (2000).
Mercat, A. et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: A randomized controlled trial. JAMA 299, 646–655. https://doi.org/10.1001/jama.299.6.646 (2008).
Meade, M. O. et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: A randomized controlled trial. JAMA 299, 637–645. https://doi.org/10.1001/jama.299.6.637 (2008).
Nemer, S. N. et al. Effects of positive end-expiratory pressure on brain tissue oxygen pressure of severe traumatic brain injury patients with acute respiratory distress syndrome: A pilot study. J. Crit. Care 30, 1263–1266. https://doi.org/10.1016/j.jcrc.2015.07.019 (2015).
Wolf, S., Plev, D. V., Trost, H. A. & Lumenta, C. B. Open lung ventilation in neurosurgery: An update on brain tissue oxygenation. Acta Neurochir. Suppl. 95, 103–105. https://doi.org/10.1007/3-211-32318-x_22 (2005).
Muench, E. et al. Effects of positive end-expiratory pressure on regional cerebral blood flow, intracranial pressure, and brain tissue oxygenation. Crit. Care Med. 33, 2367–2372. https://doi.org/10.1097/01.ccm.0000181732.37319.df (2005).
Shapiro, H. M. & Marshall, L. F. Intracranial pressure responses to PEEP in head-injured patients. J. Trauma 18, 254–256. https://doi.org/10.1097/00005373-197804000-00005 (1978).
Georgiadis, D., Schwarz, S., Baumgartner, R. W., Veltkamp, R. & Schwab, S. Influence of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure in patients with acute stroke. Stroke 32, 2088–2092. https://doi.org/10.1161/hs0901.095406 (2001).
Vandenbroucke, J. P. et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. PLoS Med. 4, e297. https://doi.org/10.1371/journal.pmed.0040297 (2007).
Carney, N. et al. Guidelines for the management of severe traumatic brain injury. Neurosurgery 80, 6–15. https://doi.org/10.1227/NEU.0000000000001432 (2017).
Connolly, E. S. Jr. et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: A guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke 43, 1711–1737. https://doi.org/10.1161/STR.0b013e3182587839 (2012).
Vincent, J. L. et al. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure on behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med. 22, 707–710 (1996).
Teasdale, G. & Jennett, B. Assessment of coma and impaired consciousness. A practical scale. Lancet 2, 81–84 (1974).
Jennett, B. & Bond, M. Assessment of outcome after severe brain damage. Lancet 1, 480–484. https://doi.org/10.1016/s0140-6736(75)92830-5 (1975).
Gouvea Bogossian, E. et al. Time course of outcome in poor grade subarachnoid hemorrhage patients: A longitudinal retrospective study. BMC Neurol. 21, 196. https://doi.org/10.1186/s12883-021-02229-1 (2021).
Stevens, R. D., Lazaridis, C. & Chalela, J. A. The role of mechanical ventilation in acute brain injury. Neurol. Clin. 26, 543–563. https://doi.org/10.1016/j.ncl.2008.03.014 (2008).
Robba, C. et al. Mechanical ventilation in patients with acute brain injury: Recommendations of the European Society of Intensive Care Medicine consensus. Intensive Care Med. 46, 2397–2410. https://doi.org/10.1007/s00134-020-06283-0 (2020).
Oddo, M. et al. Acute lung injury is an independent risk factor for brain hypoxia after severe traumatic brain injury. Neurosurgery 67, 338–344. https://doi.org/10.1227/01.NEU.0000371979.48809.D9 (2010).
Gouvea Bogossian, E. et al. Factors associated with brain tissue oxygenation changes after RBC transfusion in acute brain injury patients. Crit. Care Med. 50, e539–e547. https://doi.org/10.1097/CCM.0000000000005460 (2022).
Pinsky, M. R. Cardiovascular issues in respiratory care. Chest 128, 592S-597S. https://doi.org/10.1378/chest.128.5_suppl_2.592S (2005).
Chesnut, R. M. et al. Early and late systemic hypotension as a frequent and fundamental source of cerebral ischemia following severe brain injury in the Traumatic Coma Data Bank. Acta Neurochir. Suppl. 59, 121–125. https://doi.org/10.1007/978-3-7091-9302-0_21 (1993).
Berthiaume, L. & Zygun, D. Non-neurologic organ dysfunction in acute brain injury. Crit. Care Clin. 22, 753–766. https://doi.org/10.1016/j.ccc.2006.09.002 (2006).
Boone, M. D. et al. The effect of positive end-expiratory pressure on intracranial pressure and cerebral hemodynamics. Neurocrit. Care 26, 174–181. https://doi.org/10.1007/s12028-016-0328-9 (2017).
Videtta, W. et al. Effects of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure. Acta Neurochir. Suppl. 81, 93–97. https://doi.org/10.1007/978-3-7091-6738-0_25 (2002).
Robba, C. et al. Effects of positive end-expiratory pressure on lung recruitment, respiratory mechanics, and intracranial pressure in mechanically ventilated brain-injured patients. Front. Physiol. 12, 711273. https://doi.org/10.3389/fphys.2021.711273 (2021).
Feihl, F. & Perret, C. Permissive hypercapnia: How permissive should we be?. Am. J. Respir. Crit. Care Med. 150, 1722–1737. https://doi.org/10.1164/ajrccm.150.6.7952641 (1994).
Wolf, S., Schurer, L., Trost, H. A. & Lumenta, C. B. The safety of the open lung approach in neurosurgical patients. Acta Neurochir. Suppl. 81, 99–101. https://doi.org/10.1007/978-3-7091-6738-0_26 (2002).
Huynh, T. et al. Positive end-expiratory pressure alters intracranial and cerebral perfusion pressure in severe traumatic brain injury. J. Trauma 53, 488–492. https://doi.org/10.1097/00005373-200209000-00016 (2002) (Discussion 492–483).
McGuire, G., Crossley, D., Richards, J. & Wong, D. Effects of varying levels of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure. Crit. Care Med. 25, 1059–1062. https://doi.org/10.1097/00003246-199706000-00025 (1997).
Frost, E. A. Effects of positive end-expiratory pressure on intracranial pressure and compliance in brain-injured patients. J. Neurosurg. 47, 195–200. https://doi.org/10.3171/jns.1977.47.2.0195 (1977).
Cooper, K. R., Boswell, P. A. & Choi, S. C. Safe use of PEEP in patients with severe head injury. J. Neurosurg. 63, 552–555. https://doi.org/10.3171/jns.1985.63.4.0552 (1985).
Burchiel, K. J., Steege, T. D. & Wyler, A. R. Intracranial pressure changes in brain-injured patients requiring positive end-expiratory pressure ventilation. Neurosurgery 8, 443–449. https://doi.org/10.1227/00006123-198104000-00007 (1981).
Funding
No funding was obtained to this study. EGB was supported by a post doctorate research mandate from Fonds National de la Recherche Scientifique, Belgium (Grant No. 33409).
Author information
Authors and Affiliations
Contributions
E.G.B. and F.S.T. conceived the study; E.G.B., J.C., A.F., G.C., A.D. and F.O.G. selected the population and collected the data; E.G.B., H.N., M.A., conducted the statistical analysis. E.G.B., A.F. and J.C. wrote the first draft of the paper; F.S.T., M.S., M.A., S.S., L.N., C.R. revised the text for intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gouvea Bogossian, E., Cantos, J., Farinella, A. et al. The effect of increased positive end expiratory pressure on brain tissue oxygenation and intracranial pressure in acute brain injury patients. Sci Rep 13, 16657 (2023). https://doi.org/10.1038/s41598-023-43703-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43703-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.