Abstract
Mortality is predicted by the sum of behavior-related health risk factors (BRFs: tobacco smoking, alcohol drinking, body overweight, and physical inactivity). We analyzed degrees and combinations of BRFs in their relation to mortality and adjusted for mental disorders. In a random sample of the general population in northern Germany aged 18–64, BRFs and mental disorders had been assessed in 1996–1997 by the Munich Composite International Diagnostic Interview. A sum score including eight ranks of the behavior-related health risk factors was built. Death and its causes were ascertained 2017–2018 using residents’ registration files and death certificates. Relations of the sum score and combinations of the BRFs at baseline with all-cause, cancer, and cardiovascular mortality 20 years later were analyzed. The sum score and combinations predicted all-cause, cardiovascular and cancer mortality. The odds ratio of the sum score was 1.38 (95% confidence interval 1.31–1.46) after adjustment for age, gender, and mental disorder. In addition to the BRFs, mood, anxiety or somatoform disorders were not related to mortality. We concluded that the sum score and combinations of behavior-related health risk factors predicted mortality, even after adjustment for mental disorders.
Similar content being viewed by others
Introduction
Data from controlled trials with humans and animal studies revealed that behavior-related health risk factors (BRFs) may have causal effects on health conditions1. In a general population sample, lifestyle counseling according to smoking, risky alcohol consumption, diet, and physical inactivity2 may have improved mental and physical self-reported health3 but did not seem to decrease mortality or ischemic heart disease4. Half-yearly advice to stop smoking and diet counselling over a 5-year period in a male general population sample may have added to reduced mortality from myocardial infarction5. Animal studies showed effects of diet and exercise interventions on cardiovascular conditions1,6,7. Cohort studies are limited to the analysis of potential predictors of mortality. However, different aspects of BRFs may be taken into account such as dose–response relations with mortality risk, concomitants of BRFs and their prevalence.
A dose–response relation between the number of BRFs among tobacco smoking alcohol risk drinking, poor diet, and physical inactivity and mortality exists8. A hazard ratio 0.83 (0.80–0.85) for a one-point increment in a healthy lifestyle score of 0 to 4 was found for time to death in a general population sample in the USA (n = 44,462) and almost the same hazard ratio 0.83 (0.82–0.84) in the UK (n = 399,537)8. Similar findings come from two cohorts in the USA with a mortality follow-up after more than 20 years. The data of 79,043 women and 39,544 men had been analyzed9. With each one-point increment of a healthy lifestyle score, the hazard ratio was 0.81 (0.79–0.83) for all-cause mortality among people who did not use aspirin, blood pressure or lipid lowering medication. According to meta-analysis data, a pooled hazard ratio 0.42 (CI 0.37 to 0.46) was found for cardiovascular10, and 0.48 (CI 0.42 to 0.54) for cancer mortality among persons with the most compared to those with the least healthy lifestyle11. Adherence to four lifestyle recommendations (non-smoking, low alcohol drinking, staying physically active, and maintaining a healthy diet) was related to a 70% lower hazard of death than following none of these recommendations12. In a variety of samples from America, Asia, and Europe the number of BRFs has been found to predict time to death for all-cause13, cardiovascular9,10, and cancer mortality11,14. In a sample of 35 to 70 years old residents across 21 nations including high-, medium- and low-income countries, BRFs have been shown to be related with cardiovascular events and mortality15.
Little is known about further factors that might add to the prediction of death in addition to the BRFs from general population samples. Mental disorders belong to these factors. A reason is that a relation between mental disorders and mortality has been shown. A second reason is that BRFs and mental disorders are related to each other. Third, both BRFs and mental disorders are prevalent.
Research revealed that individuals with mental disorders compared to those without have an increased mortality16. Among 148 studies reviewed, 135 found higher mortality among subjects with a mental disorder and more years of life lost than among comparison samples16. Life expectancy of people with a mental disorder was 10 years lower than in comparison samples16. Most of the evidence exists for all-cause and for cardiovascular mortality17. But also, a higher mortality was found among psychiatric patients with cancer compared to the general population with cancer18.
BRFs and mental disorders are related to each other. BRFs may add to the evolvement and maintenance of a mental disorder or may accrue when maturing out of it. Dietary factors and lack of physical activity have been shown to be associated with depressive19,20 and with anxiety disorders21,22. Mood and anxiety disorders may add to BRFs in the risk of death23. However, there is a lack of general population data.
Both BRFs and mental disorders are prevalent. In the United States of America, in a general population sample 47.3% had two or three among three health risk behaviors (smoking, poor diet, physical inactivity)24. Among men at age 18 to 44, there were 17% current smokers, 68% overweight or obese, and 54% did not meet activity recommendations25. According to general population data from Great Britain, considerable proportions of the study participants did not meet the criteria for health behavior due to smoking (45.2%), risky alcohol consumption (37.0%), overweight or obesity (66.7%) or physical inactivity (66.7%)8. Among an adult general population sample in Germany, 51.5% of the female and 61.9% of the male respondents had two or more of four BRFs (tobacco smoking, risky alcohol consumption, overweight or obesity, physical inactivity)26. According to mental disorders, pooled survey data from 85 studies and 39 countries revealed a proportion of 29.2% in general population samples with a mental disorder in lifetime before27. Among the population aged 18 to 65 in European countries, 27.1% have been estimated to suffer each year from a mental disorder such as anxiety, depressive, somatoform or substance use disorder28. General population data from the United States revealed that 13.2% had a major depressive disorder and 17.2% an anxiety disorder in their lifetime before29.
Limitations of the knowledge so far include, first, that hardly anything is known about the prediction of mortality by BRFs and mental disorders in one prediction model with mental disorders being assessed according to international standards. Symptoms of depressive disorders have been analyzed15,30. However, the assessment was limited by using a screening instrument15,30. Second, a lack of evidence exists concerning associations between BRFs and mental disorders among general population samples. Third, a variety of studies just considered whether single BRFs were present or absent10. Three or more ranks of each single BRF and sum scores of these ranks may be expected to provide more information on dose–response relations of BRFs with mortality. Fourth, little evidence exists about specific combinations of single BRFs and mortality31.
The aim of the present study was, first, to analyze the mortality risks among a sample of working aged adult residents based on degrees of tobacco smoking, alcohol drinking, body overweight, physical inactivity and prevalent mental disorders that had been assessed 20 years before according the Diagnostic and Statistical Manual of the American Psychiatric Association32. Second, more than four ranks among tobacco smoking, alcohol drinking, body overweight, and physical inactivity and the combinations of these BRFs were to be included.
Methods
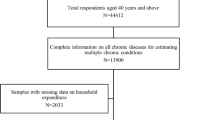
Sample
A random adult population sample aged 18 to 64 years was used33. Among the 5,829 individuals eligible for the baseline study, 4,093 (70.2%) interviews had been completed July 1996 to March 1997, and 4,075 were analyzed33. A mortality follow-up was conducted from April 2017 until April 2018. Among the 4,075 baseline study participants, vital statistics data could not be proved for 4734. For 4,028 (98.8% of 4,075) study participants, we received the data. This is our final sample for the reported data analysis.
Assessments
Baseline
Four BRFs were assessed by self-statements: tobacco smoking, alcohol drinking, body overweight, and leisure time physical inactivity. Tobacco smoking was part of a standardized interview. Alcohol drinking, body overweight and physical inactivity were assessed using standardized questionnaires which were filled in by the study participants as part of the interview. Tobacco smoking included smoking status (never or ever less than daily smoker, former daily smoker, current daily smoker less than 20 cigarettes per day, current daily smoker 20 or more cigarettes per day). Never smokers were those who answered “No” to the question whether they ever had smoked tobacco by cigarette, cigar or pipe in their life before. Ever less than daily smokers reported a history of smoking but not daily over a time period longer than 4 weeks in their life. Former daily smokers were smokers who had disclosed daily tobacco smoking over a time period of more than 4 weeks but not during the last 12 months prior to the baseline interview. Current daily smokers had smoked daily during the last 12 months prior to the interview. Alcohol drinking during the last 12 months prior to the interview was assessed by the Alcohol Use Disorders Identification Test, first three questions (Alcohol Use Disorders Identification Test Consumption, AUDIT-C35,36): “1. How often did you have an alcoholic drink in the past 12 months?” (0: never, 1: once a month or less, 2: 2 to 4 times a month, 3: 2 to 3 times a week, 4: 4 times a week or more often). Those who had an alcohol drink in the last 12 months received questions 2 and 3: “2. If you have an alcoholic drink, how many glasses do you typically drink at 1 day?” (a small glass or a bottle of beer, a small glass of wine or sparkling wine, Spirits or liquor; 0: 1–2, 1: 3–4, 2: 5–6, 3: 7–9, 4: 10 or more), “3. How often did you drink 6 or more glasses in a row?” (0: never, 1: less than once a month, 2: once a month, 3: once a week, 4: daily or almost daily). The sum of the three item scores is the AUDIT-C sum score. Body overweight was estimated using the body mass index (BMI) as weight in kilograms divided by height in meters squared. Physical inactivity was assessed by a score with the value range 5 to 20 based on five questions about single areas of leisure time physical activity: ride a bicycle; practice gymnastics, aerobics or dancing; playing sports such as soccer, volleyball, handball, tennis; hiking or going on longer walks; working in house or garden. For each of these activities the respondent was asked to indicate how often s/he practiced the activity. We collapsed the answer categories into four: daily or almost daily, several times per week, once a week, less than once a week or never. We used a score of 1 to 4. It was the higher the less frequently the activity was practiced.
Mental disorders included mood disorders, anxiety disorders, and somatoform disorders34. These had been assessed for the lifetime before baseline according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, American Psychiatric Association32. The Composite International Diagnostic Interview (M-CIDI)33,37 had been used.
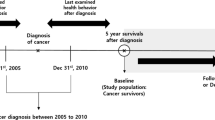
Mortality follow-up
Vital statistics data were retrieved from the residents` registration files at the place of the last residence for all-cause mortality. For cardiovascular and for cancer mortality, we used the death certificate information. Based on the information of the residents’ registration office about the date of death, we received the death certificates from the local health authorities at the place of residence of the individual. The death certificates included health disorders which inferred death, disorders which were a main cause of, and disorders which may have contributed to death. A maximum of 15 disorders and 11 disorders as found by autopsy could be documented by the certificating physician. We used cardiovascular disorders and cancer among the disorders that inferred or were a main cause of death based on the International Classification of the Diseases, version 1038.
Data analysis
The data analysis was performed in three steps: First, we determined the ranks of the four single BRF variables. We started with four ranks per variable. We collapsed the four values each of body overweight and physical inactivity into three based on the number of death cases per group. A score 0 to 3 for each of tobacco smoking and alcohol drinking and a score 0 to 2 for body mass index and for physical inactivity turned out. The four ranks of tobacco smoking were: 0 never or ever less than daily smoker, 1 former daily smoker, 2 current daily smoker less than 20 cigarettes per day, 3 current daily smoker 20 or more cigarettes per day. Alcohol drinking included: 0 AUDIT-C = 1–4, 1 AUDIT-C = 5–7, 2 AUDIT-C alcohol abstinent, 3 AUDIT-C = 8–12. The ranks of body overweight were: 0 BMI < 27, 1 BMI 27- < 32, 2 BMI 32 or higher. Physical inactivity had the ranks: 0 physical inactivity score 16 or lower, 1 physical inactivity score 17–19, 2 physical inactivity score 20.
Second, the BRF sum score was constructed as the sum of the values of the four single variables (0 to 10). The values 7 to 10 included 117 persons only and were collapsed to one group. Thus, the final BRF sum score had eight ranks (0–7). We built the 16 combinations of the four BRFs after dichotomizing tobacco smoking into never daily smokers vs. ever daily smokers, alcohol drinking into low risk (AUDIT-C: 1—4) vs. high risk drinking (AUDIT-C: 5–12) or alcohol abstinence in the last 12 months prior to the interview. We used alcohol abstinence and AUDIT-C 5–12 as one group because evidence had shown that alcohol abstinence included former problem drinkers and had been related to death in a similar way as high alcohol consumption39. Body overweight was used as normal weight (BMI lower than 27) vs. overweight (BMI 27 or higher), and physical inactivity as physically active (physical inactivity score: lower than 17) vs. physically inactive (physical inactivity score: 17 or higher).
Third, we analyzed the prediction of all-cause, cardiovascular and cancer mortality by the single BRFs, the BRF sum score, and the BRF combinations. For Cox Proportional Hazards models the proportional hazards assumption was tested using Schoenfeld residuals40,41. The Cox Proportional Hazards assumption was not fulfilled in one or more variables in each of the models that have been calculated. Therefore, we used logistic regression analysis. Odds ratios (ORs) with 95% confidence intervals (CIs) are presented. With respect to the single BRFs (Table 3), we analyzed three models. Model 1 included each single BRF adjusted for age and sex. Model 2 was adjusted for age and sex and the three further BRFs. Model 3 in addition was adjusted for mental disorders. The BRF sum score and combinations (Table 4) were analyzed by two models. Model 1 was adjusted for age and sex. Model 2 was adjusted for age, sex, and mental disorders. We used three groups of mental disorders in the data analysis: mood, anxiety, and somatoform disorders. Mood disorders included major depression, dysthymia, bipolar disorders, and mood disorders based on a medical condition. Anxiety disorders were panic disorders, phobias, anxiety disorders not further specified, compulsive disorders, posttraumatic stress disorder, and anxiety disorder on grounds of a medical condition. Somatoform disorders included somatization disorder, conversion disorder, pain disorder, and hypochondriasis.
Missing values were found in the number of cigarettes per day among the current daily smokers (14; 0.35% of 4028) and in the alcohol drinking (35; 0.87% of 4028), body overweight (30; 0.74% of 4028), and physical inactivity variables (40; 0.99% of 4028). The missing values were replaced by the means of 5-year age groups among females and males each. For sex, age and mental disorders no values were missing due to the rules of the computer-assisted interview. They included that the study participant was recontacted if any information in the interview was missing and could not be provided by answers to other questions in the interview37. The datasets used and analyzed during the current study are available from the corresponding author on reasonable request. All methods were performed in accordance with the relevant guidelines and regulations. All data were analyzed using Stata 17.042.
Ethics approval and consent to participate
The ethics committee of the University Medicine Greifswald gave approval for the study (BB 044/13). All study participants had been invited to participate in the study and informed that participation is on their own choice and that they were free to withdraw at any time. All study participants gave informed consent to the scientific use of their data including analysis and publication. They had been informed to withdraw their consent at any time.
Results
At baseline, 49.90% of the final sample had a BRF sum score 3 or greater (2010 study participants; Table 1). The likelihood of a mental disorder was higher for all BRF sum score ranks compared to no BRF. The data revealed an OR 1.86 (1.32–2.63) for a mental disorder among the persons with two BRFs who were daily smokers and alcohol high risk drinkers. Among the study participants with three BRFs, those who were daily smokers, alcohol high risk drinkers and physically inactive had an OR 2.38 (1.74–3.25) for a mental disorder. The BRFs were associated with each other except tobacco smoking with body overweight (Table 2).
All-cause mortality was predicted by each of the single BRFs after adjustment for age, sex, and the other three BRFs (Table 3). The OR per rank was 1.47 (1.35–1.60) for tobacco smoking and 1.45 (1.30–1.62) for alcohol drinking in model 2. For cardiovascular mortality, the data revealed increased ORs for all four BRFs. The highest rank of alcohol drinking had an OR 4.78 (2.43–9.41) in model 2.
The higher the BRF sum score was, the higher were the proportions of deceased persons (Table 4). Among the study participants who had no BRF, 7.91%, among the study participants who had seven to ten BRFs, 34.19% had been deceased. The data revealed 38% higher odds of all-cause mortality for each of the ranks, the study participants who had none of the BRFs being the reference. For persons with a sum score 3 or higher, the ORs were significantly increased compared to the persons who had no BRF. After adjustment for mental disorders in addition to age and sex, the OR per sum score rank was 1.38 (1.31–1.46) and 8.09 (4.66–14.02) for the sum score rank 7 to 10. Mood, anxiety and somatoform disorders were not related with an increased mortality risk.
For the combinations of the single BRFs, the study participants who had no BRFs were the reference group. Among the person groups with two or more BRFs, all ORs for all-cause mortality were significantly increased. Among the participants with two BRFs, ever daily smokers and alcohol high risk drinkers had the highest OR (2.91; 1.80–4.70) after adjustment for age, sex, and mental disorders. The lowest OR was found in the group that had neither a tobacco- nor an alcohol-related BRF. Among the persons with three BRFs, those with ever daily smoking, alcohol high risk drinking and physical inactivity had the highest OR (4.79; 3.08–7.43). All ORs that were statistically significant after adjustment for age and sex remained to be significant after additional adjustment for mental disorders (model 2).
According to cardiovascular mortality, in both models increased ORs of the BRF sum score were found compared to persons without BRFs. The data revealed 49% higher odds of mortality for each of the ranks with the study participants who had none of the BRFs as the reference (model 1). The data of the combinations revealed that among persons who had three or four BRFs all combinations showed significantly increased ORs.
According to cancer mortality, in model 1 increased ORs were found for the BRF sum score (1.35; 1.25–1.46). Persons with any mood, anxiety or somatoform disorder did not have an increased risk of cancer death. For the combinations of the BRFs, the data revealed eight increased ORs. Among these, seven included ever daily smoking. Ever daily smokers turned out to be the only subgroup with an increased OR among the study participants with one BRF. The highest OR (4.14; 2.04–8.40) was found for those who had four BRFs.
Discussion
This study has four main findings. First, the BRF sum score turned out to be related with mortality risk in a dose-dependent manner. Second, among the specific combinations of the single BRFs alcohol drinking and tobacco smoking seem to strongly contribute to the prediction of mortality. Third, cardiovascular mortality was predicted by the BRFs in a particularly strong manner. Fourth, mental disorders did not change the findings considerably.
The BRF sum score predicted mortality. The score turned out to have three advantages. First, it gave evidence for the dose-dependent relation with mortality. Each of the seven ranks indicated a 38% higher likelihood to die within the 20 years. This finding gives evidence on a dose-relation between BRFs and mortality risk. Many of the studies before had been limited to BRFs as being present or absent8,9,43. Second, the sum score may provide more information about risk of death than single BRFs because of covering four behavior-related health risk factors and eight ranks. Third, the data revealed rank 3 of the sum score as the lowest one that indicates an increased risk of death. This finding seems to be particularly important for public health. Among all 4028 study participants, 49.90% had a BRF sum score 3 or higher.
According to specific combinations, the findings suggest that alcohol consumption might be of particularly strong influence. Persons with high risk alcohol drinking had seven ORs greater than 2 for all-cause mortality. This was the largest number of ORs greater than 2 among all BRFs. High risk alcohol drinking was also involved in all three combinations of the BRFs with an OR larger than 3.
According to cardiovascular mortality, the BRF sum score turned out to be related with the risk of death in a particularly high dose manner. Each rank of the sum score was 48% higher compared to the respective lower rank after adjustment for age, sex and mental disorders. Nine combinations of BRFs had an OR larger than 2. Among them, the most frequent BRF was alcohol high risk drinking. Persons with high risk drinking were involved in seven of the nine ORs larger than 2. According to cancer mortality, the BRF sum score was also in a linear relation to the mortality risk with a 35% higher risk per rank after adjustment for age and sex. Daily tobacco smoking was included in seven out of eight BRF combinations that predicted cancer mortality. Tobacco smoking was the only BRF that predicted mortality among persons with one BRF. This lends support to the assumption that in cancer mortality tobacco smoking might have a particularly strong influence among the four BRFs.
Mood, anxiety or somatoform disorders did not add to the prediction of mortality by BRFs. Our findings at first view seem to contradict findings of a higher mortality among subjects with a mental disorder than among healthy comparison samples16. One reason might be that our sample had been drawn from the general population. The study participants with a mental disorder in their majority included those who had not utilized psychiatric treatment. Among them, there might be those with a low severity of the disorder. Persons with a mental disorder but no treatment survived longer than those with a treated mental disorder34.
Strengths of our study include that a sum score with the potential of ten ranks has been used. This provides the opportunity to detect more detailed dose-relations between BRFs and mortality. Second, 15 combinations of the BRFs in addition to no BRF turned out to add information to the relations between BRFs and mortality. Subgroups of persons at particularly high risk among the general population and combinations of single BRFs that might be more important than others in the prediction of mortality have been detected. Third, we assessed mental disorders using an internationally standardized interview and the diagnostic criteria of the American Psychiatric Association. Our study added findings about BRFs, mental disorders, all-cause, cardiovascular, and cancer mortality in the time frame of 20 years. Limitations of our study include that we had self-report data only. Reporting bias is likely. This particularly might be the case for alcohol consumption. But for the other BRFs also, underreporting may have taken place. It seems plausible that residents with high ranks of BRFs might be particularly prone to underreport BRFs. Feelings of guilt and shame might be responsible for that. Our study was limited to four BRFs. More may be relevant for death. BRFs may have evolved or been discontinued during the 20 years. We reported a considerable number of statistical test results. Problems of multiple testing should be kept in mind.
Conclusions
The findings of this 20-year mortality follow-up study suggest that the eight ranks of the sum score of behavior-related health risk factors are related to risk of death in a dose-dependent manner. This was found for all-cause, cardiovascular and cancer mortality. The study results provide evidence that especially alcohol high risk drinking and tobacco smoking might have a robust influence on mortality. Cardiovascular mortality was predicted by the BRFs in a particularly strong manner. Lifetime mood, anxiety or somatoform disorders might not have an effect on mortality in addition to the behavior-related health risk factors.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Veiga, E. C. A. et al. Exercise training and experimental myocardial ischemia and reperfusion: A systematic review and meta-analysis. Int. J. Cardiol. Heart Vasc. 46, 101214. https://doi.org/10.1016/j.ijcha.2023.101214 (2023).
Jorgensen, T. et al. A randomized non-pharmacological intervention study for prevention of ischaemic heart disease: Baseline results Inter99. Eur. J. Cardiovasc. Prev. Rehabil. 10, 377–386. https://doi.org/10.1097/01.hjr.0000096541.30533.82 (2003).
Pisinger, C. et al. Five years of lifestyle intervention improved self-reported mental and physical health in a general population: The Inter99 study. Prev. Med. 49, 424–428. https://doi.org/10.1016/j.ypmed.2009.07.020 (2009).
Jorgensen, T. et al. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. BMJ 348, g3617. https://doi.org/10.1136/bmj.g3617 (2014).
Holme, I., Retterstol, K., Norum, K. R. & Hjermann, I. Lifelong benefits on myocardial infarction mortality: 40-year follow-up of the randomized Oslo diet and antismoking study. J. Intern. Med. 280, 221–227. https://doi.org/10.1111/joim.12485 (2016).
Cardoso, J. C. et al. A high-fat diet induces cardiac damage in obesity-resistant rodents with reduction in metabolic health. Cell. Physiol. Biochem. 57, 264–278. https://doi.org/10.33594/000000642 (2023).
Veiga, E. C. A. et al. Prior exercise training and experimental myocardial infarction: A systematic review and meta-analysis. Clinics 75, e1293. https://doi.org/10.6061/clinics/2020/e1293 (2020).
Zhang, Y. B. et al. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: Two prospective cohort studies. BMJ 373, n604. https://doi.org/10.1136/bmj.n604 (2021).
Wang, K. et al. Healthy lifestyle for prevention of premature death among users and nonusers of common preventive medications: A prospective study in 2 US cohorts. J. Am. Heart Assoc. 9, e016692. https://doi.org/10.1161/JAHA.119.016692 (2020).
Zhang, Y. B. et al. Combined lifestyle factors, all-cause mortality and cardiovascular disease: A systematic review and meta-analysis of prospective cohort studies. J. Epidemiol. Community Health 75, 92–99. https://doi.org/10.1136/jech-2020-214050 (2021).
Zhang, Y. B. et al. Combined lifestyle factors, incident cancer, and cancer mortality: A systematic review and meta-analysis of prospective cohort studies. Br. J. Cancer 122, 1085–1093. https://doi.org/10.1038/s41416-020-0741-x (2020).
Ibsen, D. B. et al. Modifiable lifestyle recommendations and mortality in denmark: A cohort study. Am. J. Prev. Med. 60, 792–801. https://doi.org/10.1016/j.amepre.2021.01.003 (2021).
Han, Y. et al. Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. Eur. Heart J. 42, 3374–3384. https://doi.org/10.1093/eurheartj/ehab413 (2021).
Troeschel, A. N. et al. A novel evolutionary-concordance lifestyle score is inversely associated with all-cause, all-cancer, and all-cardiovascular disease mortality risk. Eur. J. Nutr. 60, 3485–3497. https://doi.org/10.1007/s00394-021-02529-9 (2021).
Yusuf, S. et al. Modifiable risk factors, cardiovascular disease, and mortality in 155,722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet 395, 795–808. https://doi.org/10.1016/S0140-6736(19)32008-2 (2020).
Walker, E. R., McGee, R. E. & Druss, B. G. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry 72, 334–341. https://doi.org/10.1001/jamapsychiatry.2014.2502 (2015).
Penninx, B. & Lange, S. M. M. Metabolic syndrome in psychiatric patients: Overview, mechanisms, and implications. Dialogues Clin. Neurosci. 20, 63–73 (2018).
Kisely, S., Forsyth, S. & Lawrence, D. Why do psychiatric patients have higher cancer mortality rates when cancer incidence is the same or lower?. Aust. N. Z. J. Psychiatry 50, 254–263. https://doi.org/10.1177/0004867415577979 (2016).
Cao, B. et al. Interventions targeting comorbid depression and overweight/obesity: A systematic review. J. Affect. Disord. 314, 222–232. https://doi.org/10.1016/j.jad.2022.07.027 (2022).
Zhou, Q., Guo, C., Yang, X. & He, N. Dose-response association of total sedentary behaviour and television watching with risk of depression in adults: A systematic review and meta-analysis. J. Affect. Disord. 324, 652–659. https://doi.org/10.1016/j.jad.2022.12.098 (2023).
Aucoin, M. et al. Diet and anxiety: A scoping review. Nutrients 13, 4418. https://doi.org/10.3390/nu13124418 (2021).
Allen, M. S., Walter, E. E. & Swann, C. Sedentary behaviour and risk of anxiety: A systematic review and meta-analysis. J. Affect. Disord. 242, 5–13. https://doi.org/10.1016/j.jad.2018.08.081 (2019).
Zaman, R., Hankir, A. & Jemni, M. Lifestyle factors and mental health. Psychiatr. Danub. 31, 217–220 (2019).
Ford, E. S., Bergmann, M. M., Boeing, H., Li, C. & Capewell, S. Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Prev. Med. 55, 23–27. https://doi.org/10.1016/j.ypmed.2012.04.016 (2012).
Deierlein, A. L., Sun, Y., Prado, G. & Stein, C. R. Socioeconomic characteristics, lifestyle behaviors, and health conditions among males of reproductive age with and without disabilities, NHANES 2013–2018. Am. J. Mens Health 17, 15579883221138190. https://doi.org/10.1177/15579883221138190 (2023).
John, U., Hanke, M. & Freyer-Adam, J. Health risk behavior patterns in a national adult population survey. Int. J. Environ. Res. Public Health 15, 873 (2018).
Steel, Z. et al. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 43, 476–493. https://doi.org/10.1093/ije/dyu038 (2014).
Wittchen, H. U. et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 21, 655–679. https://doi.org/10.1016/j.euroneuro.2011.07.018 (2011).
Hasin, D. S. & Grant, B. F. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Waves 1 and 2: Review and summary of findings. Soc. Psychiatry Psychiatr. Epidemiol. 50, 1609–1640. https://doi.org/10.1007/s00127-015-1088-0 (2015).
Rajan, S. et al. Association of symptoms of depression with cardiovascular disease and mortality in low-, middle-, and high-income countries. JAMA Psychiatry 77, 1052–1063. https://doi.org/10.1001/jamapsychiatry.2020.1351 (2020).
Freyer-Adam, J. et al. Behavioral health risk factor profiles in general hospital patients: Identifiying the need for screening and brief intervention. BMC Public Health 19, 1594 (2019).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (American Psychiatric Association, 2000).
Meyer, C., Rumpf, H.-J., Hapke, U., Dilling, H. & John, U. Prevalence of alcohol consumption, abuse and dependence in a country with high per capita consumption: Findings from the German TACOS study. Soc. Psychiatry Psychiatr. Epidemiol. 35, 539–547. https://doi.org/10.1007/s001270050277 (2000).
John, U., Rumpf, H. J., Hanke, M. & Meyer, C. Mental disorders and total mortality after 20 years in an adult general population sample. Eur. Psychiatry 63, e30. https://doi.org/10.1192/j.eurpsy.2020.27 (2020).
Bradley, K. A. et al. The AUDIT alcohol consumption questions: Reliability, validity, and responsiveness to change in older male primary care patients. Alcohol. Clin. Exp. Res. 22, 1842–1849. https://doi.org/10.1111/j.1530-0277.1998.tb03991.x (1998).
Babor, T. F. & Robaina, K. The alcohol use disorders identification test (AUDIT): A review of graded severity algorithms and national adaptations. Int. J. Alcohol Drug Res. 5, 17–24. https://doi.org/10.7895/ijadr.v5i2.222 (2016).
Meyer, C., Rumpf, H.-J., Hapke, U. & John, U. The Composite International Diagnostic Interview: Feasibility and necessity of editing and interviewer training in general population surveys. Int. J. Methods Psychiatr. Res. 9, 32–42 (2000).
World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision (World Health Organization, 2019).
John, U., Rumpf, H. J., Hanke, M. & Meyer, C. Alcohol abstinence and mortality in a general-population sample of adults in Germany: A cohort study. PLoS Med. 18, e1003819. https://doi.org/10.1371/journal.pmed.1003819 (2021).
Flynn, R. Survival analysis. J. Clin. Nurs. 21, 2789–2797. https://doi.org/10.1111/j.1365-2702.2011.04023.x (2012).
Bellera, C. A. et al. Variables with time-varying effects and the Cox model: Some statistical concepts illustrated with a prognostic factor study in breast cancer. BMC Med. Res. Methodol. 10, 20. https://doi.org/10.1186/1471-2288-10-20 (2010).
StataCorp, L. P. Stata 17.0 (StataCorp LP, 2021).
Li, Y. et al. Impact of healthy lifestyle factors on life expectancies in the US population. Circulation 138, 345–355. https://doi.org/10.1161/CIRCULATIONAHA.117.032047 (2018).
Funding
Open Access funding enabled and organized by Projekt DEAL. This research has been funded by grants from the German Federal Ministry for Education and Research (grant number: 01 EB 9406) and the German Research Foundation (DFG; grant numbers: JO 150/11-1; ME 3180/4-1; RU 1570/3-1).
Author information
Authors and Affiliations
Contributions
U.J. applied for two of the grants, provided the data analysis, and wrote the paper. H.-J.R. applied for one of the grants, prepared the data, and collaborated in the writing of the paper. M.H. prepared the data and collaborated in the writing of the paper. C.M. applied for one of the grants, prepared the data, provided parts of the data analysis, and collaborated in the writing of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
John, U., Rumpf, HJ., Hanke, M. et al. Behavior-related health risk factors, mental disorders and mortality after 20 years in a working aged general population sample. Sci Rep 13, 16764 (2023). https://doi.org/10.1038/s41598-023-43669-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43669-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.