Abstract
Human brucellosis cases are rare in non-endemic countries, such as Germany, where infections are predominantly caused by Brucella melitensis. The German National Reference Laboratory for Bovine, Porcine, Ovine and Caprine Brucellosis received a suspected Brucella sp. isolate from a patient for identification. Bacteriological tests and PCR-based diagnostics showed the isolate to be B. suis, but did not yield cohesive results regarding the biovar. Whole genome sequencing and subsequent genotyping was employed for a detailed characterization of the isolate and elucidating the reason for failure of the diagnostic PCR to correctly identify the biovar. The isolate was found to be B. suis bv. 5, a rare biovar with limited geographical distribution primarily found in the Northern Caucasus. Due to a deletion in one of the target regions of the diagnostic PCR, the isolate could not be correctly typed. Based on in silico genotyping it could be excluded that the isolate was identical to one of the B. suis bv. 5 reference strains. Here, we report a rare case of a B. suis bv. 5 field isolate. Furthermore, by reporting this finding, we want to make practitioners aware of possible misinterpretation of PCR results, as it cannot be excluded that the detected deletion is common among the B. suis bv. 5 community, as there is currently a lack of field isolates.
Similar content being viewed by others
Introduction
Brucellosis is a zoonotic disease that has had many names over the centuries, such as Malta fever or Mediterranean fever, before its causative agent was discovered in 1887 by the British microbiologist David Bruce, after whom it was later named Brucella, and the disease was called “brucellosis”1,2. The primary hosts for the pathogen are animals, and there is a preference of the various Brucella spp. for specific animal species. However, close contact with infected animals can lead to infection of non-primary host species, like humans. Especially in endemic regions, like the Mediterranean Basin3, the risk of contracting brucellosis can be quite high. Contact with animal abortion material, handling of carcasses, consumption of contaminated, raw animal products such as unpasteurized milk, as well as laboratory work are the main sources of infection. Thus, veterinarians, hunters, cooks and laboratory workers are some of the occupational groups with an increased risk of a Brucella infection4,5,6. The identification of the disease as brucellosis is often difficult due to unspecific symptoms, e.g. usually fever, sweat, headache, arthralgia and weight loss, which may occur episodically for months or even years after the infection5,6,7,8,9. Therapeutically, diagnosis is followed by a long antibiotic treatment and relapses are frequent, especially in endemic, rural areas where medical care often cannot be sufficiently ensured7,10,11.
The global number of human infections per year can hardly be estimated reliably, as brucellosis is often underreported12. In the literature, 500,000 cases per year is the most cited number, however, it was pointed out, that this number is not reliable and a product of incorrect citation throughout brucellosis literature1. Based on statistical modelling using international healthcare data, a conservative estimate gives an annual incidence of 2.1 million13. Since 2017, a decline of confirmed human brucellosis cases is observed in the European Union (EU), from 0.09 confirmed cases per 100,000 population in 2017 to 0.03 in 202114, e.g. in 2019, 310 human brucellosis infections have been reported in the EU, which accounts for a notification rate of 0.06 cases per 100,000 population15.
With regard to human brucellosis, B. melitensis, B. abortus and B. suis are the most commonly identified species. B. melitensis has the highest potential for causing brucellosis in humans and is the most frequently isolated species from brucellosis patients in the EU15,16,17. On the contrary, reports on human infections with B. suis in the EU are rare. In the period of 2006 to 2018, the vast majority (91%) of notified human brucellosis cases in Germany were caused by B. melitensis, whereas only a single infection with B. suis was reported5. In the latter case, B. suis bv. 1 was identified as the causative agent and the infection resulted most likely from consumption of contaminated meat, possibly from Argentina7.
The species B. suis is divided into five biovars based on phenotypic properties. They also exhibit different host preferences and regional prevalences. The biovars 1, 2 and 3 are commonly found in wild boars and domestic pigs, with the former two biovars also infecting hares4,18,19,20,21. Biovar 2 is the most frequently reported biovar of B. suis in Europe. Infections with B. suis bv. 4 have occurred mainly in northern America affecting reindeers and caribous22. In contrast, B. suis bv. 5 has exclusively been reported from the Northern Caucasus and South West Siberia, where it primarily infects rodents23,24. In Germany, B. suis bv. 2 is the only biovar that circulates among animals, as it is frequently reported in wild boars and domestic pigs, also from neighbouring countries25,26,27,28.
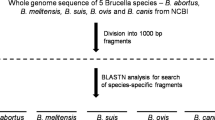
Although different serological tests for brucellosis diagnosis are available, the isolation of the bacterium from the patient gives the only conclusive evidence. For the quick identification of Brucella species directly from Brucella suspected specimen, PCR assays have been developed. The most widely used approaches are AMOS and Bruce-ladder PCR. With the former, Brucella abortus biovars 1, 2, and 4, Brucella melitensis, Brucella ovis, and Brucella suis bv. 1 can be detected. The PCR is based on species-specific chromosomal locations of IS711, whose position differs among Brucella species29 and it was later enhanced for the additional differentiation of vaccine strains B. abortus S19 and RB1530. However, with this approach, not all Brucella species can be detected. Thus, a different assay was developed based on marker genes, with which all classical Brucella sp., B. neotomae, B. pinnipedialis, B. ceti and some vaccine strains could be identified, called Bruce-ladder PCR31,32. For further PCR-based discrimination of B. suis biovars and the closely related B. canis, a Suis-ladder PCR was developed33. In this multiplex PCR using four primer pairs, the B. suis biovars can be identified based on varying product lengths in some of the investigated loci.
For epidemiological studies aiming at deciphering the relationship between strains, genome sequencing and bioinformatic analysis should be employed. Already before the advent of sequencing techniques, the high genomic similarity of Brucella sp. has been described34. Thus, the common thresholds for species delineation in the analysis of the average nucleotide identity (ANI) analysis, does not apply35. For example, the ANI of B. suis strains is > 99.85%, i.e. individual strains may differ in as little as 0.15% of their genome from each other. Therefore, single nucleotide substitutions have to be employed for the reconstruction of strain similarities, that help identifying the infection source36,37. This analysis heavily depends on the availability of genome sequence data, with which an isolate’s sequence can be compared. In particular for B. melitensis, single nucleotide polymorphism (SNP) typing helped identifying the potential geographic origin of the infection of travel-associated human brucellosis cases in Germany38.
Here, we report on the genotypic and phenotypic peculiarities of an isolate from a rare case of human brucellosis, for which B. suis bv. 5 was identified as causing agent. The unambiguous identification of the pathogen was hampered by the fact that bacteriological diagnostics based on standard differential tests indicated that this isolate was a strain of B. suis bv. 5, but one band in the Suis-ladder PCR did not yield the expected size for this biovar. Thus, genome sequencing-based analysis, which is now routinely used for diagnostic purposes, had to be used for identification and genotyping of the human isolate, revealing its affiliation to biovar 5.
Methods
Isolate origin and case description
In 2008, a suspected Brucella sp. isolate was sent to the National Reference Laboratory (NRL) for Bovine, Porcine, Ovine and Caprine Brucellosis at Friedrich-Loeffler-Institut for confirmation and further typing. The following information on the sample was provided by the sender: The isolate was obtained in Germany from a blood culture of a 71-year old male patient with a septic clinical picture with fever episodes up to 41 °C and nearly fever-free intervals. The isolate was given the FLI number 08RB3647.
Phenotypic methods
The isolate was cultivated on nutrient agar (Merck, Germany) and bacteriological tests for Brucella differentiation were conducted as described elsewhere39, i.e. testing for catalase, oxidase and urease activity, CO2 requirement, H2S production, agglutination assays, phage lysis and tolerance to the dyes fuchsin and thionin. Further, VITEK GN ID card (bioMérieux, Marcy-l′Etoile, France) was used for genus confirmation.
DNA extraction and PCR
DNA was isolated for molecular investigations using the High Pure PCR Template Preparation Kit (Roche Molecular Systems, Pleasanton, CA, USA). For identifying the species, AMOS and Bruce-ladder PCR were conducted as described before29,32,40. Suis-ladder PCR, hereafter referred to as B. suis ladder PCR, according to López-Goni et al.33, was used for strain differentiation on the biovar level. For the latter, DNA from reference strains B. suis bv. 1 strain 1330, B. suis bv. 2 strain Thomsen, B. suis bv. 3 strain 686, B. suis bv. 4 strain 40 and B. suis bv. 5 strain 513 were used as references. Cultivation and DNA extraction was conducted as described for strain 08RB3647.
Genome sequencing and assembly
For Illumina short-read sequencing, a DNA library was prepared using the Nextera XT library preparation kit (Illumina Inc., San Diego, CA, USA), and sequenced on a MiSeq device in paired-end mode using v3 chemistry. Additionally, long-read sequencing was performed by Eurofins Genomics Germany GmbH (Ebersberg, Germany) on a PacBio RSII instrument. The raw data from both technologies were used for de novo genome assembly in a hybrid approach using Unicycler v.0.4.841. Starting positions of the chromosomes were adjusted by circlator v1.5.542 and the assembly aligned to B. suis bv. 5 CVI_73 (GCF_014884485.1) with Mauve 43 for checking for assembly errors. QUAST v5.0.244 was used for further assessing assembly statistics and genome annotation was performed by Prokka v.1.14.545. Raw sequencing data and the assembled genome were deposited under the BioProject number PRJEB62596.
In silico genome characterization
Using the in_silico_pcr script by Egon A. Ozer (v0.5.1) (https://github.com/egonozer/in_silico_pcr) with allowing one mismatch in the primer binding site (option “-m”) and primers by López-Goni et al.33, an in silico B. suis ladder PCR was conducted for confirmation of the in vitro result. The products were aligned using MAFFT v746 and visualized by pyBoxShade (https://github.com/mdbaron42/pyBoxshade). The average nucleotide identity of the de novo genome to the genomes of the strains B. suis bv. 1 1330 (GCF_000223195.1), B. suis bv. 2 Thomsen (GCA_000018905.1), B. suis bv. 3 686 (GCF_000740255.1), B. suis bv. 4 40 (GCF_000160275.1), B. suis bv. 5 513 (GCF_000157755.1) and B. suis bv. 5 CVI_73 (GCF_014884485.1) was determined by fastANI v1.147.
The genotype of the investigated strain was determined by in silico multi-locus sequence typing (MLST) and multiple locus variable number of tandem repeats analysis (MLVA) as allele-based methods. The tools mlst v2.19.0 (https://github.com/tseemann/mlst) with the MLST-9 scheme by from PubMLST48, and MISTReSS (https://github.com/Papos92/MISTReSS) employing the MLVA-16 scheme by Le Flèche et al.49 and Al Dahouk et al.50 were used for these purposes, respectively. The MLVA profile was used as query in a search for identical or similar profiles in the MLVAbank database (https://microbesgenotyping.i2bc.paris-saclay.fr/)51 (accessed on 5th December 2022). In addition, single nucleotide polymorphism (SNP) analysis was carried out using Snippy v.4.6.0 (https://github.com/tseemann/snippy), with B. suis bv. 5 CVI_73 as reference genome. Data of B. suis reference strains and other closely related species (Supplementary Table S1) from the NCBI Sequence Read Archive were also included in this analysis. The resulting alignment of core genome SNPs was used as input for maximum likelihood analysis by RAxML v8.2.1252 employing the GTRGAMMA model of rate heterogeneity and optimization of substitution rates and the final tree was visualized by FigTree v1.4.3 (http://tree.bio.ed.ac.uk/soft-ware/figtree/).
The novel genome was screened for potential antimicrobial resistance genes by comparing the sequences to entries in three databases (Resfinder53, CARD 54, AMRFinder55) by ABRicate v0.8.10 (https://github.com/tseemann/abricate). Additionally, the VFanalyzer pipeline of the VFDB56 was employed for detecting genes related to virulence (accessed on 1st December 2022).
Antimicrobial susceptibility testing
Analysis of antimicrobial resistance was conducted in user-defined commercial microdilution plates (Sensititre; Thermo Scientific, Waltham, MA, USA) containing antibiotics in the following final concentration ranges: chloramphenicol (0.5–16 µg/ml), ciprofloxacin (0.002–4 µg/ml), doxycycline (0.004–8 µg/ml), gentamicin (0.004–8 µg/ml), levofloxacin (0.004–4 µg/ml), rifampicin (0.125–8 µg/ml), streptomycin (0.008–16 µg/ml), tetracycline (0.004–8 µg/ml), trimethoprim/sulfamethoxazole (0.002/0.04–4/76 µg/ml) and ceftriaxone (0.004–0.12 µg/ml). For inoculation, the strain was cultivated on Columbia blood agar (Thermo Scientific, Waltham, MA, USA) for 48 h at 37 °C under aerobic conditions. Subsequently, a 1:10 diluted 0.5 McFarland suspension was prepared in 0.9% NaCl solution, of which 200 µl were added to 11 ml cation-adjusted Mueller Hinton broth (CAMHB) (BD Diagnostics, Franklin Lakes, NJ, USA). To each well of the microdilution plate, 100 µl were added and the plate was closed and incubated at 37 °C for 48 h under aerobic conditions. The minimum inhibitory concentration (MIC) endpoints were evaluated visually using an inverted mirror. For susceptibility evaluation the epidemiological cut-off values (ECOFFs) of the European Committee on Antimicrobial Susceptibility Testing (EUCAST) for B. melitensis were used (https://mic.eucast.org/; accessed on 06.09.2023), as no official values exist for B. suis.
Results
Differential testing and PCR
Based on differential testing at the NRL, strain 08RB3647 can be described as Gram-negative, non-motile coccoid rods. The strain did not require CO2 and was negative for haemolysis and H2S production but positive for the production of catalase, oxidase and urease (Table 1). Biochemical identification by VITEK GN ID card indicated Brucella melitensis. In the serum agglutination the strain showed agglutination with anti-M monospecific serum only, which is characteristic for B. suis bv. 5. Further, tests for lysis by phages gave overall negative results for all of the tested phages, although small, single plaques could be observed within the tested zones. Only at an increased concentration lysis was observed for phage Tbilisi (Tb).
The Bruce-ladder PCR confirmed that the isolate 08RB3647 was indeed a B. suis strain, as it gave the expected band pattern that corresponds to this species. Subsequently, the B. suis biovar should also be determined by PCR. Strain 08RB3641 was negative in the AMOS PCR, which ruled out its identity as B. suis bv. 1. However, the result of the B. suis ladder PCR was unexpected, as a band of appr. 500 bp length could be observed (Fig. 1), which was not characteristic for any of the known B. suis biovars.
Genome sequencing and characterisation
Sequencing yielded short reads of 247 bp for 287-fold coverage in case of Illumina technology and 80,359 reads with a mean length of 9678 bp giving an average coverage of 211-fold for PacBio technology. By combining reads from both techniques in a de novo hybrid assembly approach, two chromosomes with sizes of 2,131,613 bp and 1,187,908 bp could be assembled (Table 2). The average genomic GC content was 57.25% and 3091 coding regions were predicted. These values were in accordance with those of the genome assembly of B. suis bv. 5 CVI_73, which was the only complete B. suis bv. 5 genome available at NCBI at the time of writing.
To confirm species identification and to clarify the identification on biovar level, the average nucleotide identity (ANI) of the de novo assembly to B. suis reference strains and the field isolate CVI_73 was determined (Table 3). Strain 08RB3647 exhibited high ANI values to all B. suis biovars (ANI > 99.7%), but the highest identity was observed to B. suis bv. 5 strains, particularly strain CVI_73, which differed by only 0.009%, confirming the affiliation of strain 08RB3647 to biovar 5.
The high genomic concordance to B. suis bv. 5 strains raised the question why the B. suis ladder PCR did not yield the expected band of 614 bp length, but a shorter band. Therefore, this PCR was repeated in silico. The strains B. suis bv. 5 513 and CVI_73 yielded the expected patterns with products of 774 bp, 614 bp, 278 bp and 197 bp in length, whereas in strain 08RB3647 the product of primers BMEI0205f/r was truncated exhibiting a size of 488 bp, due to a 126 bp deletion in a locus homologous to BMEI0205 (Fig. 2). Apart from this deletion, the products of strain CVI_73 and strain 08RB3647 were identical for this locus, whereas nucleotide substitutions were observed in the product of B. suis bv. 4 strain 40, which yielded a band of identical size.
Regarding potential antimicrobial resistance and virulence genes, no particularities could be observed. Genes encoding a multidrug efflux RND transporter (bepD-G) and the integral membrane protein MprF were identified in strain 08RB3647 as well as in the other B. suis bv. 5 strains. Likewise, the results for potential virulence-associated genes was identical in the tested strains.
Genotyping
In silico typing showed that strain 08RB3647 belonged to MLST-9 sequence type 19, like B. suis bv. 5 strain 513. Regarding the MLVA-16 profile, both strains differed in eight loci (Table 4), whereas B. suis bv. 5 strain CVI_73 was almost identical to the reference strain 513, differing only in one locus. When searching the MLVAbank for strains with a similar profile to strain 08RB3647, no strains with identical MLVA profiles were found. The most similar strains were REF 513 and BCCN#R29, both of which belong to B. suis bv. 5, probably derivatives of the reference strain 513, and differ from strain 08RB3647 in eight and six loci, respectively.
For a more detailed genomic comparison, core genome SNP analysis was conducted, including reference strains of B. suis and other Brucella spp. (Fig. 3). The human isolate 08RB3647 clustered with other B. suis bv. 5 strains, which originate from animals. However, 35 and 63 SNPs differed between strain 08RB3647 and the reference strains 513/ 513UK and the field strain CVI_73 from Slovakia, respectively. The latter differed in 28 SNPs from the references, which were both identical in cgSNP analysis. Over 4000 SNPs differentiated this B. suis bv. 5 cluster from the other B. suis biovars, while the difference to the B. pinnipedialis and B. microti reference strains merely amounted to 2607 and 2720 SNPs, respectively.
Antimicrobial susceptibility testing
Strain 08RB3647 was tested for susceptibility to antibiotics of different classes: aminoglycosides (gentamicin, streptomycin), cephalosporins (ceftriaxone), fluoroquinolones (ciprofloxacin, levofloxacin), sulphonamides (sulfamethoxazole) and tetracyclines (doxycycline, tetracycline), as well as the antimicrobial compounds chloramphenicol and rifampicin. The MIC values for all substances were in the lower range of the tested concentrations, not exceeding 1 µg/ml, which was the highest tolerated concentration observed for chloramphenicol and rifampicin. When compared to the epidemiological cut-off values given by EUCAST, the strain could be classified as susceptible to all tested compounds (Table 5).
Discussion
Human brucellosis cases are rare in the European Union, and in particular in Germany, where the mean annual notification rate was as low as 0.38/1,000,000 population between 2006 and 20185. Also, it can be expected that B. melitensis is the most common agent of human brucellosis in Germany and Middle Europe, as this was the most frequently identified species in investigative studies38,57. However, in the majority of brucellosis cases, the species was not determined5,15, thus, the true prevalence of Brucella species remains elusive. For epidemiological investigations it would be desirable to not only identify the causative agent on the genus level, but also to mandatorily identify the species and possibly the biovar. However, this would require close collaboration between clinics, contract laboratories, authorities and the reference laboratories, as not every laboratory has the capacity for in-depth investigation of isolates.
For the human brucellosis case presented in this study B. suis was identified as infecting agent. This species comprises five biovars, that differ in host specificities and prevalence in human brucellosis cases. In the period between 2015 and 2019 only a single human case of B. suis infection has been reported to the authorities15. The latter was a patient from Germany who was infected by B. suis bv. 17. This biovar is more common in Latin America58. In Europe, several human infections with B. suis bv. 2 have been reported. This biovar is endemic in wild boars, pigs and hares18,19,20,59, why hunters and farmers are predominantly affected6,60. B. suis bv. 3 infections are reported from patients in China4. Most human B. suis bv. 4 infections were found in northern Canada22. Whatmore et al.61 also list a human isolate from 1979 originating from Finland.
Little information is available on isolates of B. suis bv. 5. Since the 1960s, atypical Brucella strains have been isolated from mouse-like rodents (Murinae) in the northern foothills of the Greater Caucasus, which, at that time, could not be unambiguously positioned within the known Brucella taxonomy23,62. These isolates differed from other B. suis biovars regarding their growth characteristics, as they are fast-growing like the "non-classical" Brucella microti, whose primary hosts are also rodents63, and reactions in biochemical tests64, but their pathogenicity and differential characteristics are matching those of B. suis isolates23,62,65. Therefore, the Subcommittee on Taxonomy of Brucella of the International Committee on Systematic Bacteriology postulated a new B. suis biotype for these strains, biovar 5, in 198266. A couple of years later, the reference strain B. suis bv. 5 513, which was isolated from a house mouse (Mus musculus)24, was deposited under the number NCTC 11996 in the National Collection of Type Cultures, Colindale, London67, despite the fact that Vershilova et al.62 proposed a different strain, 514, as type strain. The reference strain 513 is one of two strains which is commonly used in the literature when in need of a B. suis bv. 5 strain. The other being ELT80 (sometimes also called BCCN#R29 or BCCN 82.75). The origin of this strain cannot be determined for certain, as some studies state that the strain was isolated from a patient in England34,68, while others place the geographic origin in the USA31,32,33 or state that it is unknown49. Due to this small number of available bv. 5 isolates, one of these two strains, 513 or ELT80, is usually used for the development of Brucella sp. detection assays, e.g. Bruce-ladder PCR or Suis-ladder31,33, or genotyping approaches, e.g. MLVA49. There are no comprehensive studies applying these assays on several isolates of this biovar. Isolate 08RB3647 showed a deletion in one of the loci that is targeted in the Suis-ladder PCR. This prevented the unambiguous identification of the strain by PCR. Since no other B. suis bv. 5 field strains were available, it cannot be assessed whether this deletion is common among the strains of this biovar. However, deletion or modifications in genomic loci which are targeted by diagnostic PCRs are known from other pathogens, e.g. Burkholderia mallei69, and investigators should be aware of the possibility of false conclusions based on these assays.
Therefore, in the present study, the identity of the human isolate 08RB3647 as B. suis bv. 5 strain could only be unambiguously determined by genome sequencing and subsequent genotyping. Although the isolate was also correctly identified using classical phenotyping, this method is reserved for specialized laboratories due to the limited availability of the required monospecific sera.
The species B. suis belongs to core clade of Brucella phylogeny70 and in contrast to other Brucella species, e.g. B. melitensis37,71, strains of the same biovars form distinct clusters in the polytomy. From the beginnings of Brucella genotyping, allele-based typing methods already indicated that B. suis bv. 5 is quite distinct from the other B. suis biovars49,72. This was confirmed by whole genome comparison, in which B. suis bv. 5 displayed higher concordances with B. microti CCM4915 and B. pinnipedialis strains, while other B. suis biovars formed one cluster at a different branch of the phylogenetic tree70. This higher genomic similarity to B. microti might have led some authors to deeming B. suis bv. 5 as “misidentified” species73. However, this similarity was also found in the present study for strain 08RB3647 and other B. suis bv. 5 strains based on SNP typing. Due to the lack of sequencing data of field isolates, only the reference strains 513 and 513 UK and one other B. suis bv. 5 isolate, CVI_73, could be used for comparison. There is little information on the origin of the latter strain. Duvnjak et al.20 state that this strain was collected in 2004 in Slovenia from an animal. Regarding the 28 SNP difference between this strain and the reference strains, it can be assumed that CVI_73 is not the strain 513, which was passaged through an animal. Interestingly, the human isolate 08RB3647 showed a higher average nucleotide identity to the Slovenian isolate, while in SNP typing the similarity was higher to the reference strains. This might result from misassemblies in the genome. Nevertheless, the differences in SNP typing exceed by far the threshold of 5 to 7 SNPs, which is often applied for the definition of closely related strains74,75. It can be concluded, that strain 08RB3647 is most likely a field isolate and not the reference strain B. suis bv. 5 513.
There is a lack of knowledge on the pathogenicity of B. suis bv. 5 to humans. To our knowledge, the only report on a human brucellosis outbreak caused by B. suis bv. 5 was published by Repina et al.76 in 1993. The authors report that a family and two neighbours were diagnosed with brucellosis after contact with the domestic cat owned by the family. Brucella isolates were obtained from one patient and the cat and differential characterization identified B. suis bv. 5. The authors hypothesized that the urine of the cat promoted the spread of Brucella. The exact location was not mentioned in the report, but with regard to the involved institutions from e.g. Novosibirsk, it can be expected to be in South West Siberia.
To the authors’ knowledge, this is the first study reporting MICs of B. suis bv. 5 for antimicrobial substances determined by microdilution method. The susceptibility profile observed for strain 08RB3647 was comparable to the MICs found for B. melitensis strains as given by EUCAST. However, comprehensive data on antimicrobial susceptibility of B. suis is lacking and should be addressed in future studies.
The source of the human infection reported in the present study remains elusive. It can be assumed that the infection was contracted by close contact to an infected animal. A more thorough determination of the geographic origin of strain 08RB3647 is hampered by the lack of available sequence data of this biovar. Also, to our knowledge, there are no studies on the geographic distribution of B. suis bv. 5. However, as in case of the species, the biovars of isolates are not always determined and the prevalence of biovars might be underestimated. Due to this gap, we cannot state whether the deletion observed in one of the Suis-ladder target loci is of general importance for the PCR-based identification of this biovar. Nevertheless, microbiologists should be aware of the problems caused by mutations in the pathogen’s genome that could prohibit correct diagnosis by PCR.
Data availability
The datasets generated and analysed during the current study are available in the European Nucleotide Archive repository, under the BioProject number PRJEB62596.
References
Moreno, E., Blasco, J.-M. & Moriyón, I. Facing the human and animal brucellosis conundrums: The forgotten lessons. Microorganisms 10(5), 942. https://doi.org/10.3390/microorganisms10050942 (2022).
Bruce, D. Note on the discovery of a microorganism in malta fever. Practitioner 40, 161–170 (1887).
Pappas, G., Papadimitriou, P., Akritidis, N., Christou, L. & Tsianos, E. V. The new global map of human brucellosis. Lancet Infect. Dis. 6(2), 91–99. https://doi.org/10.1016/S1473-3099(06)70382-6 (2006).
Jiang, H. et al. Genetic comparison of Brucella suis biovar 3 in clinical cases in China. Vet. Microbiol. 160(3), 546–548. https://doi.org/10.1016/j.vetmic.2012.06.030 (2012).
Enkelmann, J., Stark, K. & Faber, M. Epidemiological trends of notified human brucellosis in Germany, 2006–2018. Int. J. Infect. Dis. 93, 353–358. https://doi.org/10.1016/j.ijid.2020.02.019 (2020).
Mailles, A. et al. Brucella suis biovar 2 infection in humans in France: Emerging infection or better recognition?. Epidemiol. Infect. 145(13), 2711–2716. https://doi.org/10.1017/S0950268817001704 (2017).
Zange, S. et al. A headache with surprising outcome: First case of brucellosis caused by Brucella suis biovar 1 in Germany. Infection 47(5), 863–868. https://doi.org/10.1007/s15010-019-01312-7 (2019).
Naha, K., Dasari, S., Pandit, V. & Seshadri, S. A rare case of seronegative culture-proven infection with Brucella suis. Australas Med. J. 5(7), 340–343. https://doi.org/10.4066/AMJ.2012.1177 (2012).
Paton, N. I., Tee, N. W. S., Vu, C. K. F. & Teo, T.-P. Visceral abscesses due to Brucella suis infection in a retired pig farmer. Clin. Infect. Dis. 32(8), e129–e130. https://doi.org/10.1086/319748 (2001).
Jiang, W. et al. Epidemiological characteristics, clinical manifestations and laboratory findings in 850 patients with brucellosis in Heilongjiang Province, China. BMC Infect. Dis. 19(1), 439. https://doi.org/10.1186/s12879-019-4081-5 (2019).
Alavi, S. M., Alavi, S. M. R. & Alavi, L. Relapsed human brucellosis and related risk factors. Pak. J. Med. Sci. 25(1), 46–50 (2009).
Dougas, G. et al. Brucellosis underreporting in Greece: Assessment based on aggregated laboratory data of culture-confirmed cases from public hospitals. Hippokratia 23(3), 106–110 (2019).
Laine, C., Johnson, V., Scott, H. M. & Arenas-Gamboa, A. Global estimate of human brucellosis incidence. Emerg. Infect. Dis. J. 29(9), 1789. https://doi.org/10.3201/eid2909.230052 (2023).
EFSA, ECDC. The European union one health 2021 zoonoses report. EFSA J. 20(12):7666 (2022) DOI: https://doi.org/10.2903/j.efsa.2022.7666.
EFSA, ECDC. The European union one health 2019 zoonoses report. EFSA J. 19(2):e06406 (2021) DOI: https://doi.org/10.2903/j.efsa.2021.6406
Garofolo, G. et al. Cases of human brucellosis in Sweden linked to Middle East and Africa. BMC Res. Notes. 9(1), 277. https://doi.org/10.1186/s13104-016-2074-7 (2016).
De Massis, F. et al. Distribution of Brucella field strains isolated from livestock, wildlife populations, and humans in Italy from 2007 to 2015. PLOS ONE 14(3), e0213689. https://doi.org/10.1371/journal.pone.0213689 (2019).
Melzer, F., Lohse, R., Nieper, H., Liebert, M. & Sachse, K. A serological study on brucellosis in wild boars in Germany. Eur. J. Wildl. Res. 53(2), 153–157. https://doi.org/10.1007/s10344-006-0072-0 (2007).
Kreizinger, Z. et al. Genetic relatedness of Brucella suis biovar 2 isolates from hares, wild boars and domestic pigs. Vet. Microbiol. 172(3), 492–498. https://doi.org/10.1016/j.vetmic.2014.05.031 (2014).
Duvnjak, S. et al. Characterisation of Brucella suis isolates from Southeast Europe by multi-locus variable-number tandem repeat analysis. Vet. Microbiol. 180(1), 146–150. https://doi.org/10.1016/j.vetmic.2015.08.013 (2015).
García-Yoldi, D. et al. Comparison of multiple-locus variable-number tandem-repeat analysis with other PCR-based methods for typing Brucella suis isolates. J. Clin. Microbiol. 45(12), 4070–4072. https://doi.org/10.1128/JCM.01096-07 (2007).
Forbes, L. B. Isolates of Brucella suis biovar 4 from animals and humans in Canada, 1982–1990. Can. Vet. J. 32(11), 686–688 (1991).
Liamkin, G. I., Taran, I. F., Safronova, V. M., Tikhenko, N. I. & Shiranovich, M. P. Taxonomic position and ecology of the causative agent of brucellosis isolated from murine rodents in regions of the northern foothills of the greater Caucasus. II. The ecological and pathogenetic characteristics of Brucella strains isolated from murine rodents. Zh. Mikrobiol. Epidemiol. Immunobiol. 7, 31–35 (1983).
Dranovskaia, E. A., Malikov, V. E. & Grekova, N. A. Biological and physicochemical properties of Brucella isolated from murine rodents. Zh. Mikrobiol. Epidemiol. Immunobiol. 1, 47–53 (1983).
Kautzsch, S., Seyfarth, D., Schöne, R. & Stehmann, R. An outbreak of brucellosis in pigs and conclusions for characteristics of this epidemic disease. Berl. Münch. Tierärztl. Wochenschr. 108(6), 201–205 (1995).
van Tulden, P. et al. Monitoring results of wild boar (Sus scrofa) in The Netherlands: analyses of serological results and the first identification of Brucella suis biovar 2. Infect. Ecol. Epidemiol. 10(1), 1794668. https://doi.org/10.1080/20008686.2020.1794668 (2020).
Macías Luaces, L. et al. Seroprevalence of Brucella infection in wild boars (Sus scrofa) of Bavaria, Germany, 2019 to 2021 and associated genome analysis of Five B. suis Biovar 2 isolates. Microorganisms 11(2), 204478. https://doi.org/10.3390/microorganisms11020478 (2023).
Abril, C. et al. A novel isolation method of Brucella species and molecular tracking of Brucella suis biovar 2 in domestic and wild animals. Vet. Microbiol. 150(3–4), 405–410. https://doi.org/10.1016/j.vetmic.2011.02.056 (2011).
Bricker, B. J. & Halling, S. M. Differentiation of Brucella abortus bv. 1, 2, and 4, Brucella melitensis, Brucella ovis, and Brucella suis bv. 1 by PCR. J. Clin. Microbiol. 32(11), 2660–2666. https://doi.org/10.1128/jcm.32.11.2660-2666.1994 (1994).
Bricker, B. J. & Halling, S. M. Enhancement of the Brucella AMOS PCR assay for differentiation of Brucella abortus vaccine strains S19 and RB51. J. Clin. Microbiol. 33(6), 1640–1642. https://doi.org/10.1128/jcm.33.6.1640-1642.1995 (1995).
García-Yoldi, D. et al. Multiplex PCR assay for the identification and differentiation of all Brucella Species and the vaccine strains Brucella abortus S19 and RB51 and Brucella melitensis Rev1. Clin. Chem. 52(4), 779–781 (2006).
López-Goñi, I. et al. Evaluation of a multiplex PCR assay (Bruce-ladder) for molecular typing of all Brucella species, including the vaccine strains. J. Clin. Microbiol. 46(10), 3484–3487. https://doi.org/10.1128/jcm.00837-08 (2008).
López-Goñi, I. et al. New Bruce-ladder multiplex PCR assay for the biovar typing of Brucella suis and the discrimination of Brucella suis and Brucella canis. Vet. Microbiol. 154(1), 152–155. https://doi.org/10.1016/j.vetmic.2011.06.035 (2011).
Verger, J.-M., Grimont, F., Grimont, P. A. D. & Grayon, M. Brucella, a monospecific genus as shown by deoxyribonucleic acid hybridization. Int. J. Syst. Evol. Microbiol. 35(3), 292–295. https://doi.org/10.1099/00207713-35-3-292 (1985).
Ciufo, S. et al. Using average nucleotide identity to improve taxonomic assignments in prokaryotic genomes at the NCBI. Int. J. Syst. Evol. Microbiol. 68(7), 2386–2392. https://doi.org/10.1099/ijsem.0.002809 (2018).
Bardenstein, S., Gibbs, R. E., Yagel, Y., Motro, Y. & Moran-Gilad, J. Brucellosis outbreak traced to commercially sold camel milk through whole-genome sequencing. Israel. Emerg. Infect. Dis. 27(6), 1728–1731. https://doi.org/10.3201/eid2706.204902 (2021).
Dadar, M., Brangsch, H., Alamian, S., Neubauer, H. & Wareth, G. Whole-genome sequencing for genetic diversity analysis of Iranian Brucella spp. isolated from humans and livestock. One Health 16, 100483. https://doi.org/10.1016/j.onehlt.2023.100483 (2023).
Georgi, E. et al. Whole genome sequencing of Brucella melitensis isolated from 57 patients in Germany reveals high diversity in strains from Middle East. PLoS One 12(4), e0175425. https://doi.org/10.1371/journal.pone.0175425 (2017).
Alton, G. G., Jones, L. M., Angus, R. D. & Verger, J. M. Techniques for the Brucellosis Laboratory (INRA, 1988).
Mayer-Scholl, A., Draeger, A., Göllner, C., Scholz, H. C. & Nöckler, K. Advancement of a multiplex PCR for the differentiation of all currently described Brucella species. J. Microbiol. Methods. 80(1), 112–114. https://doi.org/10.1016/j.mimet.2009.10.015 (2010).
Wick, R. R., Judd, L. M., Gorrie, C. L. & Holt, K. E. Unicycler: Resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput. Biol. 13(6), e1005595. https://doi.org/10.1371/journal.pcbi.1005595 (2017).
Hunt, M. et al. Circlator: Automated circularization of genome assemblies using long sequencing reads. Genome Biol. 16(1), 294. https://doi.org/10.1186/s13059-015-0849-0 (2015).
Darling, A. C., Mau, B., Blattner, F. R. & Perna, N. T. Mauve: multiple alignment of conserved genomic sequence with rearrangements. Genome Res. 14(7), 1394–1403. https://doi.org/10.1101/gr.2289704 (2004).
Gurevich, A., Saveliev, N., Vyahhi, N. & Tesler, G. QUAST: Quality assessment tool for genome assemblies. Bioinformatics 29, 1072–1075. https://doi.org/10.1093/bioinformatics/btt086 (2013).
Seemann, T. Prokka: Rapid prokaryotic genome annotation. Bioinformatics 30(14), 2068–2069. https://doi.org/10.1093/bioinformatics/btu153 (2014).
Katoh, K., Rozewicki, J. & Yamada, K. D. MAFFT online service: Multiple sequence alignment, interactive sequence choice and visualization. Brief Bioinform. 20(4), 1160–1166. https://doi.org/10.1093/bib/bbx108 (2017).
Jain, C., Rodriguez, R. L., Phillippy, A. M., Konstantinidis, K. T. & Aluru, S. High throughput ANI analysis of 90K prokaryotic genomes reveals clear species boundaries. Nat. Commun. 9(1), 5114. https://doi.org/10.1038/s41467-018-07641-9 (2018).
Jolley, K., Bray, J. & Maiden, M. Open-access bacterial population genomics: BIGSdb software, the PubMLST.org website and their applications. Wellcome Open Res. 3(124), 14826. https://doi.org/10.12688/wellcomeopenres.14826.1 (2018).
Le Fleche, P. et al. Evaluation and selection of tandem repeat loci for a Brucella MLVA typing assay. BMC Microbiol. 6, 9. https://doi.org/10.1186/1471-2180-6-9 (2006).
Al Dahouk, S. et al. Evaluation of Brucella MLVA typing for human brucellosis. J. Microbiol. Methods 69(1), 137–145. https://doi.org/10.1016/j.mimet.2006.12.015 (2007).
Grissa, I., Bouchon, P., Pourcel, C. & Vergnaud, G. On-line resources for bacterial micro-evolution studies using MLVA or CRISPR typing. Biochimie 90(4), 660–668. https://doi.org/10.1016/j.biochi.2007.07.014 (2008).
Stamatakis, A. RAxML version 8: A tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics 30(9), 1312–1313. https://doi.org/10.1093/bioinformatics/btu033 (2014).
Zankari, E. et al. Identification of acquired antimicrobial resistance genes. J. Antimicrob. Chemother. 67(11), 2640–2644. https://doi.org/10.1093/jac/dks261 (2012).
Jia, B. et al. CARD 2017: Expansion and model-centric curation of the comprehensive antibiotic resistance database. Nucleic Acids Res. 45(D1), D566–D573. https://doi.org/10.1093/nar/gkw1004 (2016).
Feldgarden, M. et al. Validating the AMRFinder tool and resistance gene database by using antimicrobial resistance genotype-phenotype correlations in a collection of isolates. Antimicrob Agents Chemother. 63(11), e00483-e519. https://doi.org/10.1128/AAC.00483-19 (2019).
Liu, B., Zheng, D., Zhou, S., Chen, L. & Yang, J. VFDB 2022: A general classification scheme for bacterial virulence factors. Nucleic Acids Res. 50(D1), D912–D917. https://doi.org/10.1093/nar/gkab1107 (2022).
Schaeffer, J. et al. Tracking the origin of austrian human brucellosis cases using whole genome sequencing. Front. Med. Lausanne. 8, 635547. https://doi.org/10.3389/fmed.2021.635547 (2021).
Lucero, N. E., Ayala, S. M., Escobar, G. I. & Jacob, N. R. Brucella isolated in humans and animals in Latin America from 1968 to 2006. Epidemiol. Infect. 136(4), 496–503. https://doi.org/10.1017/s0950268807008795 (2008).
Damoser, J. & Hofer, E. Brucella suis biovar 2-Infektionen beim feldhasen. Z. Jagdwiss. 41(2), 137–141. https://doi.org/10.1007/BF02241370 (1995).
Teyssou, R. et al. A propos d’un cas de brucellose humaine a Brucella suis biovar 2. Med. Mal. Infect. 19(3), 160–161. https://doi.org/10.1016/S0399-077X(89)80221-5 (1989).
Whatmore, A. M., Perrett, L. L. & MacMillan, A. P. Characterisation of the genetic diversity of Brucella by multilocus sequencing. BMC Microbiol. 7, 34. https://doi.org/10.1186/1471-2180-7-34 (2007).
Vershilova, P. A., Liamkin, G. I., Malikov, V. E., Dranovskaya, E. A. & Taran, I. F. Brucella strains from mouselike rodents in southwestern USSR. Int J. Syst. Evol. Microbiol. 33(2), 399–400. https://doi.org/10.1099/00207713-33-2-399 (1983).
Hubálek, Z. et al. Brucellosis of the common vole (Microtus arvalis). Vector Borne Zoonotic Dis. 7(4), 679–687. https://doi.org/10.1089/vbz.2007.0143 (2007).
Al Dahouk, S. et al. Differential phenotyping of Brucella species using a newly developed semi-automated metabolic system. BMC Microbiol. 10(1), 269. https://doi.org/10.1186/1471-2180-10-269 (2010).
Zúñiga-Ripa, A. et al. The fast-growing brucella suis biovar 5 depends on phosphoenolpyruvate carboxykinase and pyruvate phosphate dikinase but not on fbp and glpx fructose-1,6-bisphosphatases or isocitrate lyase for full virulence in laboratory models. Front. Microbiol. 9, 641. https://doi.org/10.3389/fmicb.2018.00641 (2018).
Corbel, M. J. International committee on systematic bacteriology subcommittee on taxonomy of Brucella. Int. J. Syst. Evol. Microbiol. 34(3), 366–367. https://doi.org/10.1099/00207713-34-3-366 (1984).
Corbel, M. J. International committee on systematic bacteriology subcommittee on the taxonomy of Brucella. Int. J. Syst. Evol. Microbiol. 38(4), 450–452. https://doi.org/10.1099/00207713-38-4-450 (1988).
Whatmore, A. M. et al. Extended multilocus sequence analysis to describe the global population structure of the genus brucella: Phylogeography and relationship to biovars. Front Microbiol. 7, 2049. https://doi.org/10.3389/fmicb.2016.02049 (2016).
Laroucau, K. et al. A genetic variant of Burkholderia mallei detected in Kuwait: Consequences for the PCR diagnosis of glanders. Transbound. Emerg. Dis. 68(2), 960–963. https://doi.org/10.1111/tbed.13777 (2021).
Occhialini, A., Hofreuter, D., Ufermann, C.-M., Al Dahouk, S. & Köhler, S. The retrospective on Atypical Brucella species leads to novel definitions. Microorganisms 10(4), 813. https://doi.org/10.3390/microorganisms10040813 (2022).
Tan, K. K. et al. Full genome SNP-based phylogenetic analysis reveals the origin and global spread of Brucella melitensis. BMC Genomics 16(1), 93. https://doi.org/10.1186/s12864-015-1294-x (2015).
Whatmore, A. M. et al. Identification and characterization of variable-number tandem-repeat markers for typing of Brucella spp. J. Clin. Microbiol. 44(6), 1982–1993. https://doi.org/10.1128/jcm.02039-05 (2006).
Godfroid, J., Garin-Bastuji, B., Saegerman, C. & Blasco, J. M. Brucellosis in terrestrial wildlife. Rev. Sci. Tech. 32(1), 27–42. https://doi.org/10.20506/rst.32.1.2180 (2013).
Janowicz, A. et al. Core genome multilocus sequence typing and single nucleotide polymorphism analysis in the epidemiology of brucella melitensis infections. J. Clin. Microbiol. 56(9), e00517. https://doi.org/10.1128/JCM.00517-18 (2018).
Khan, A. U. et al. Whole-genome sequencing for tracing the genetic diversity of Brucella abortus and Brucella melitensis isolated from livestock in Egypt. Pathogens 10(6), 759. https://doi.org/10.3390/pathogens10060759 (2021).
Repina, L. P., Nikulina, A. I. & Kosilov, I. A. A case of human infection with brucellosis from a cat. Zh. Mikrobiol. Epidemiol. Immunobiol. 4, 66–68 (1993).
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: F.M., H.B.; Methodology: H.B.; Formal analysis and investigation: H.B.; Interpretation: H.B., F.M., M.A.H.; Writing—original draft preparation: H.B.; Writing—review and editing: F.M., M.A.H.; Supervision: F.M. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brangsch, H., Horstkotte, M.A. & Melzer, F. Genotypic peculiarities of a human brucellosis case caused by Brucella suis biovar 5. Sci Rep 13, 16586 (2023). https://doi.org/10.1038/s41598-023-43570-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43570-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.