Abstract
Radical cystectomy is a gold-standard treatment for muscle-invasive bladder cancer. We recently introduced robot-assisted radical cystectomy (RARC) with perioperative enhanced recovery after surgery (ERAS). The medical records of patients with bladder cancer who underwent open radical cystectomy (ORC) or RARC/ERAS at NTT Medical Center Tokyo were retrospectively reviewed to compare the surgical outcomes, hospital stay, and medical costs between groups. Multidisciplinary full ERAS items were provided for the RARC/ERAS group. The median estimated blood losses in the ORC and RARC/ERAS groups were 650 and 100 mL, and the median operative times were 312 and 445 min, respectively. In addition, the median times to liquid food intake in these groups were 6 and 0 days, the median times to first flatus and first defecation were 2 and 1 day, and 3 and 1.5 days, respectively. The rates of postoperative ileus in the ORC and RARC/ERAS groups were 27.5% and 4.5%, and the median postoperative hospital stays was 26.5 and 12 days, respectively. Medical costs excluding surgery were significantly lower in the RARC/ERAS group. In conclusion, RARC/ERAS represents a safe treatment option for muscle-invasive bladder cancer with decreased perioperative complications and lower medical costs.
Similar content being viewed by others
Introduction
Bladder cancer is the 10th most common cancer globally. In Japan, more than 9000 patients died of bladder cancer in 20221. Tobacco smoking, exposure to carcinogens including organic solvents, male sex, and advanced age are well-known risk factors for bladder cancer2,3.
Radical cystectomy with urinary diversion is the gold-standard surgical treatment for muscle-invasive bladder cancer and carcinoma in situ, which are refractory to bacillus Calmette-Guérin intravesical immunotherapy. Urinary diversions after radical cystectomy include ileal conduit, ileal neobladder, and ureterostomy. For urinary diversion using the small intestine in particular, the surgical procedure can be especially invasive.
Although robot-assisted radical cystectomy (RARC) has been replacing open radical cystectomy (ORC) or laparoscopic radical cystectomy in Japan since it gained insurance coverage in 2018, reports on RARC with enhanced recovery after surgery (ERAS) are rare. In this study, we report our early experience with RARC/ERAS, and surgical outcomes and medical costs were compared between RARC/ERAC and ORC. The objective of this retrospective observational study was to verify the advantages of RARC/ERAS concerning postoperative patient recovery and medical costs.
Results
In total, 40 patients who underwent ORC and 22 patients who underwent RARC/ERAS were enrolled in this retrospective observational study. Patient characteristics at baseline are presented in Table 1. The median patient ages in the ORC and RARC/ERAS groups were 74 and 75.5 years, respectively, the proportions of men were 80.0% and 90.9%, respectively, and the BMIs were 21.3 and 21.8 kg/m2, respectively. These variables did not differ between the groups. Neoadjuvant chemotherapy (gemcitabine plus cisplatin) was administered in 17 patients in the ORC group and 11 patients in the RARC/ERAS group. Preoperative hospital stay was significantly longer in the ORC group because of the need for preoperative mechanical bowel preparation (4.5 days vs 1 day, p < 0.001). As part of the ERAS protocol, patients in the RARC/ERAS group received preoperative stoma care training by a certified nurse.
The surgical results are presented in Table 2. The median estimated blood loss was significantly smaller in the RARC/ERAS group, whereas the operative time was longer in this group. In the ORC group, 17.5% of patients received blood transfusions. The median numbers of retrieved lymph nodes were 10 and 22 in ORC and RARC/ERAS groups, respectively (P < 0.001). Because we performed ERAS simultaneously with RARC, ERAS was not adopted in the ORC group. Patients in the RARC/ERAS group started fluid intake, liquid food intake, and mobilization at 3 h after surgery. Notably, the median times to first flatus and first defecation were significantly shorter in the RARC/ERAS group. Concerning complications, postoperative paralytic ileus (POI) developed in 27.5% and 4.5% of patients in the ORC and RARC/ERAS groups, respectively. The length of hospital stay was significantly shorter in the RARC group than in the ORC group (12 days vs. 26.5 days).
Medical costs were compared between the groups (Table 3). Drug fees including oral medication and injections were decreased by nearly fivefold in the RARC/ERAS group (14.2 thousand yen vs. 78.7 thousand yen). Examination fees including test and diagnostic imaging costs also were lower in the RARC/ERAS group (58.9 thousand yen vs. 122.9 thousand yen). The operation/anesthesia fees were 1513.9 and 1658.9 thousand yen in the ORC and RARC/ERAS groups, respectively, reflecting the higher insurance fee point for RARC. Medical fees excluding operation/anesthesia were 964.7 and 655.7 thousand yen in the ORC and RARC/ERAS groups, respectively. In total, the medical costs in these groups were 2478.6 and 2314.6 thousand yen, respectively.
Discussion
The prognosis of muscle-invasive bladder cancer is poor. Even with improvements in multimodal treatments including radical cystectomy and chemotherapy, the 12-month disease-free survival remains as low as 62.8%4. In multimodal treatment for bladder cancer, it is important to reduce the invasiveness of surgery. Despite the progress in surgical techniques, radical cystectomy remains associated with a considerably high risk of complications5.
POI is one of the major postoperative complications after radical cystectomy, occurring at the incidence of 1.58–23.5%6,7,8. Older age and higher BMI are associated with the development of POI8. POI has mainly been studied in patients undergoing gastrointestinal surgeries7,9,10,11,12. Gum chewing and early oral fluid intake alone have not prevented POI12,13. In the ERAS protocol, several items for the prevention of POI including carb loading, the prevention of postoperative nausea and vomiting (PONV), opioid-sparing analgesia, and early mobilization are applied. The synergistic effect of these strategies might greatly reduce the risk of POI. In this study, the incidence of POI was significantly lower in the RARC/ERAS group than in the ORC group. Notably, the patient with POI in the RARC/ERAS group had comorbid hypothyroidism and required 100 IU of levothyroxine sodium hydrate. Delayed replacement of levothyroxine sodium hydrate during fasting might have led to impaired intestinal function.
ERAS was first reported as a multidisciplinary approach to facilitate postoperative recovery in gastrointestinal surgeries14. A meta-analysis of colorectal surgeries revealed significant advantage of ERAS in reducing the complication rate (relative risk = 0.53, 95% confidence interval = 0.44–0.64) and shortening the length of hospital stay (− 2.55 days)15. Preferable effects of ERAS protocol during open radical cystectomies have been reported by several groups16,17,18. Notably, a randomized controlled trial clarified lower rates of postoperative complications and lower demand for analgesics in the ERAS group compared to the conservative regimen group17. In this setting, however, there were no significant differences between the groups in terms of gastrointestinal events17.
Few reports investigate the effect of ERAS protocol during RARC. A comparative study reported that a multifactorial fast-track regimen decreased time to mobilization, time to regular diet, and the use of postoperative morphine equivalents in the RARC setting19. Another retrospective study reported a shorter length of hospital stay in the enhanced recovery program group during RARC20. Although the evidence levels were low, the ERAS Society also published guidelines for perioperative care after radical cystectomy, in which early removal of a nasogastric tube, controlled fluid administration, and multimodal prevention of ileus, including gum chewing, prevention of PONV, and minimally invasive surgery, were recommended21.
Compared to the findings for ORC, RARC is associated with shorter hospital stays and lower medical costs22,23,24,25. However, no active attempts have been made to shorten hospital stays in Japan, partly because of the Japanese medical expense payment system (diagnosis procedure combination/per-diem payment system)26. In this study, the hospital stay was significantly shorter in the RARC/ERAS group. Preoperatively, we could safely omit fasting and mechanical and medical bowel preparation, resulting in shortened preoperative hospital stays. Postoperatively, the decreased incidence of complications including POI also led to shorter hospitalization. The time to the acquisition of stoma care skills determined the length of postoperative hospital stay in most patients.
Along with hospital stay, medical costs were lower in the RARC/ERAS group than in the ORC group. Importantly, the medical cost excluding the operation cost decreased from 964.7 thousand yen for ORC to 655.7 thousand yen for RARC/ERAS, reflecting the shorter hospital stay and lower complication rate during treatment. A meta-analysis comparing ORC, RARC/ICUD, and RARC/extracorporeal urinary diversion in Israel and the United States identified ORC with ERAS and RARC/ICUD with ERAS as the two most cost-effective strategies. Importantly, the ERAS protocol improved cost-effectiveness compared to their parallel non-ERAS counterpart22. Further large-scale prospective studies are needed to verify the impact of ERAS on medical costs in Japan.
The limitations of this study included the relatively small number of patients and the retrospective nature. Because this was a comparative study between ORC and RARC/ERAS, the pure effect of ERAS could not be addressed. Prospective randomized studies are necessary to further verify the impact of RARC/ERAS on the management of muscle-invasive bladder cancer in Japan.
In conclusion, RARC/ERAS proved safe for treatment of muscle-invasive bladder cancer. Along with shortened hospital stays and decreased perioperative complications, RARC/ERAS consequently reduced the medical costs.
Methods
Patients
The medical records of patients with bladder cancer who underwent ORC (between September 2015 and June 2021) or RARC/ERAS (between July 2021 and March 2023) at NTT Medical Center Tokyo (Tokyo, Japan) were retrospectively reviewed. Patient characteristics, surgical results, hospital stay, and medical costs were analyzed.
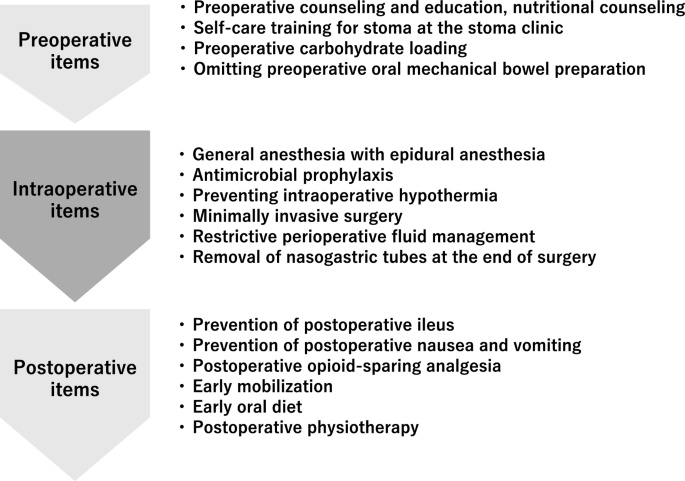
ERAS program
Multidisciplinary ERAS team
Our ERAS items were provided by a multidisciplinary team composed of urologists, anesthesiologists, physical therapists, registered dietitians, nurses, pharmacists, diabetologists, and clinical care pathway committee members as described elsewhere27. The timeline of our ERAS protocol is shown in Fig. 1.
ERAS items
Preoperative items
Preoperative counselling and education and nutritional counseling
Preoperative counseling in the outpatient setting was provided by nationally certified nutritionists, urologists, and anesthesiologists. Patients were advised to maintain a normal diet until the night before surgery unless they had malnutrition according to the European Society for Clinical Nutrition and Metabolism guidelines28. Patients were given a document on their expected recovery after surgery. Preoperative morbidities were optimized as possible.
Patients were taught self-care for stoma at the stoma clinic before the operation.
Preoperative carbohydrate loading
Patients were administered 250 mL of carbohydrate fluid (Arginaid Water®, Nestle healthscience, Tokyo, Japan:100 kcal, 22.5 g carbohydrate with 2.5 g arginine per 125 mL) at 12 and 2 h before surgery.
Preoperative oral mechanical bowel preparation
Oral mechanical bowel preparation was omitted. Sennoside (24 mg) was administered before bedtime on the night before surgery.
Intraoperative items
Anesthesia
General anesthesia was induced using propofol, fentanyl, remifentanil, and rocuronium and maintained using air/oxygen/desflurane, remifentanil, fentanyl, and rocuronium bromide. Epidural anesthesia with 7.5 mg/mL ropivacaine hydrochloride hydrate was provided. The total amount of fentanyl was restricted to 5 μg/kg. Intravenous acetaminophen was administered before the end of surgery.
Preventing intraoperative hypothermia
Warming blankets (Full Body Bair Hugger™, 3 M) were used to prevent hypothermia during surgery.
Minimally invasive surgery
RARC was performed by experienced urologists certified by the Japanese Urological Association using the Da Vinci Xi® system (Intuitive Surgical Ltd., Sunnyvale, CA, USA). Urinary diversion was performed intracorporeally (intracorporeal urinary diversion [ICUD]). The small intestine was cut and anastomosed using the SureForm® stapling system (Intuitive Surgical Ltd., Sunnyvale, CA, USA).
Resection site drainage
A drainage tube (8 mm) was placed at the bottom of the pelvic cavity until postoperative day (POD) 1.
Restrictive perioperative fluid management
Intraoperative intravenous fluid administration was limited to 3 mL/kg/h, and it included Ringer’s bicarbonate solution, antibiotics, and acetaminophen.
Nasogastric intubation
Nasogastric tubes were removed at the end of surgery.
Postoperative items
Urethral drainage
A double-lumen urethral catheter (20 Fr) was placed in the neobladder until its removal on POD 14 in patients who underwent ileum neobladder urinary diversion.
Prevention of postoperative ileus
To prevent postoperative ileus, patients were encouraged to chew gum every 3 h starting 3 h after surgery. Magnesium oxide (300 mg) was administered three times daily until POD 7.
Prevention of postoperative nausea and vomiting
To prevent postoperative nausea and vomiting, 6.6 mg of dexamethasone were intravenously administered at the induction of anesthesia.
Postoperative opioid-sparing analgesia
For postoperative analgesia, patients were intravenously administered 1000 mg of acetaminophen every 6 h for 24 h and oral celecoxib (200 mg) every 12 h.
Early mobilization
The patients were instructed to stand 3 h after surgery. The physical therapist assessed the patients’ condition and assisted with early mobilization from POD 1. On POD 1, patients were encouraged to walk 100 m and attempt to be out of bed for 6 h. They were also encouraged to be out of bed for more than 2 h. On POD 2, patients walked more than 300 m with assistance by physical therapists. They were encouraged to be out of bed for more than 6 h.
Early oral diet
Patients were allowed to drink clear fluid 3 h after surgery. A liquid diet was also provided 3 h after surgery.
Statistical analysis
Fisher’s chi-squared test was used to analyze categorical variables. Mann-Whitney U test was performed to analyze numerical variables. Statistical significance was indicated by P < 0.05. All statistical analyses were performed using SPSS version 24.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki (revised in 2013).
This study is approved by the ethics committee of NTT Medical Center Tokyo. Informed consent was obtained in the form of opt-out on the web-site. Those who rejected were excluded.
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Japan NCC. Projected Cancer Death in Japan. Accessed February 17th, 2023. https://ganjoho.jp/reg_stat/statistics/stat/short_pred_en.html#anchor2
Lenis, A. T., Lec, P. M., Chamie, K. & Mshs, M. D. Bladder cancer: A review. Jama 324(19), 1980–1991. https://doi.org/10.1001/jama.2020.17598 (2020).
Lobo, N. et al. Epidemiology, screening, and prevention of bladder cancer. Eur. Urol. Oncol. 5(6), 628–639. https://doi.org/10.1016/j.euo.2022.10.003 (2022).
Bajorin, D. F. et al. Adjuvant nivolumab versus placebo in muscle-invasive urothelial carcinoma. N. Engl. J. Med. 384(22), 2102–2114. https://doi.org/10.1056/NEJMoa2034442 (2021).
Yamada, S. et al. Comparative study of postoperative complications after radical cystectomy during the past two decades in Japan: Radical cystectomy remains associated with significant postoperative morbidities. Urol. Oncol. 40(1), 11.e17-11.e25. https://doi.org/10.1016/j.urolonc.2021.09.005 (2022).
Hirobe, M. et al. Complications within 90 days after radical cystectomy for bladder cancer: Results of a multicenter prospective study in Japan. Int. J. Clin Oncol. 23(4), 734–741. https://doi.org/10.1007/s10147-018-1245-z (2018).
Ramirez, J. A. et al. Definition, incidence, risk factors, and prevention of paralytic ileus following radical cystectomy: A systematic review. Eur. Urol. 64(4), 588–597. https://doi.org/10.1016/j.eururo.2012.11.051 (2013).
Svatek, R. S. et al. Age and body mass index are independent risk factors for the development of postoperative paralytic ileus after radical cystectomy. Urology 76(6), 1419–1424. https://doi.org/10.1016/j.urology.2010.02.053 (2010).
Nazzani, S. et al. Postoperative paralytic ileus after major oncological procedures in the enhanced recovery after surgery era: A population based analysis. Surg. Oncol. 28, 201–207. https://doi.org/10.1016/j.suronc.2019.01.011 (2019).
Schuster, T. G. & Montie, J. E. Postoperative ileus after abdominal surgery. Urology 59(4), 465–471. https://doi.org/10.1016/s0090-4295(01)01561-8 (2002).
Namba, Y. et al. Clinical indicators for the incidence of postoperative ileus after elective surgery for colorectal cancer. BMC Surg. 21(1), 80. https://doi.org/10.1186/s12893-021-01093-7 (2021).
Short, V. et al. Chewing gum for postoperative recovery of gastrointestinal function. Cochrane Database Syst Rev. 2015(2), CD006506. https://doi.org/10.1002/14651858.CD006506.pub3 (2015).
MacVicar, E. et al. A systematic review of the impact of post-operative oral fluid intake on ileus following elective colorectal surgery. Int. J. Surg. 103, 106651. https://doi.org/10.1016/j.ijsu.2022.106651 (2022).
Kehlet, H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br. J. Anaesth. 78(5), 606–617. https://doi.org/10.1093/bja/78.5.606 (1997).
Varadhan, K. K. et al. The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: A meta-analysis of randomized controlled trials. Clin. Nutr. 29(4), 434–440. https://doi.org/10.1016/j.clnu.2010.01.004 (2010).
Daneshmand, S. et al. Enhanced recovery protocol after radical cystectomy for bladder cancer. J. Urol. 192(1), 50–55. https://doi.org/10.1016/j.juro.2014.01.097 (2014).
Karl, A. et al. A new concept for early recovery after surgery for patients undergoing radical cystectomy for bladder cancer: Results of a prospective randomized study. J. Urol. 191(2), 335–340. https://doi.org/10.1016/j.juro.2013.08.019 (2014).
Arumainayagam, N., McGrath, J., Jefferson, K. P. & Gillatt, D. A. Introduction of an enhanced recovery protocol for radical cystectomy. BJU Int. 101(6), 698–701. https://doi.org/10.1111/j.1464-410X.2007.07319.x (2008).
Saar, M. et al. Fast-track rehabilitation after robot-assisted laparoscopic cystectomy accelerates postoperative recovery. BJU Int. 112(2), E99-106. https://doi.org/10.1111/j.1464-410X.2012.11473.x (2013).
Collins, J. W. et al. Introducing an enhanced recovery programme to an established totally intracorporeal robot-assisted radical cystectomy service. Scand. J. Urol. 50(1), 39–46. https://doi.org/10.3109/21681805.2015.1076514 (2016).
Cerantola, Y. et al. Guidelines for perioperative care after radical cystectomy for bladder cancer: Enhanced Recovery After Surgery (ERAS(®)) society recommendations. Clin. Nutr. 32(6), 879–887. https://doi.org/10.1016/j.clnu.2013.09.014 (2013).
Kord, E., Leshno, M. & Haifler, M. The effects of surgical approaches and enhanced recovery protocols on the cost effectiveness of radical cystectomy. J. Pers. Med. 12(9), 1433. https://doi.org/10.3390/jpm12091433 (2022).
Tan, W. S. et al. Intracorporeal robot-assisted radical cystectomy, together with an enhanced recovery programme, improves postoperative outcomes by aggregating marginal gains. BJU Int. 121(4), 632–639. https://doi.org/10.1111/bju.14073 (2018).
Schiavina, R. et al. The robotic approach improves the outcomes of ERAS protocol after radical cystectomy: A prospective case-control analysis. Urol. Oncol. 39(12), 833.e1-833.e8. https://doi.org/10.1016/j.urolonc.2021.04.015 (2021).
Chen, J. et al. Surgical approach as a determinant factor of clinical outcome following radical cystectomy: Does Enhanced Recovery After Surgery (ERAS) level the playing field?. Urol. Oncol. 37(10), 765–773. https://doi.org/10.1016/j.urolonc.2019.06.001 (2019).
Hayashida, K., Murakami, G., Matsuda, S. & Fushimi, K. History and profile of diagnosis procedure combination (DPC): Development of a real data collection system for acute inpatient care in Japan. J. Epidemiol. 31(1), 1–11. https://doi.org/10.2188/jea.JE20200288 (2021).
Nakamura, M. et al. Early experience with implementing enhanced recovery after surgery protocol during robot-assisted radical prostatectomy. AME Surg. J. 3, 33. https://doi.org/10.21037/asj-23-4 (2023).
Lassen, K. et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin. Nutr. 31(6), 817–830. https://doi.org/10.1016/j.clnu.2012.08.011 (2012).
Author information
Authors and Affiliations
Contributions
Data collection: M.N., I.T., T.I, A.O.; Writing - original draft preparation: M.N. Writing—review and editing: All authors; Supervision: S.K., H.K., Y.S.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakamura, M., Tsuru, I., Izumi, T. et al. Advantages of enhanced recovery after surgery program in robot-assisted radical cystectomy. Sci Rep 13, 16237 (2023). https://doi.org/10.1038/s41598-023-43489-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43489-w
This article is cited by
-
Effect of RARC-ERAS nursing program on clinical outcomes in patients undergoing RARC surgery: a retrospective, propensity matching study
Journal of Robotic Surgery (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.