Abstract
With ageing populations, new elderly end-stage kidney disease (ESKD) cases rise. Unlike younger patients, elderly ESKD patients are less likely to undergo kidney transplant, and therefore the decision of receiving peritoneal dialysis (PD) and hemodialysis (HD) is more crucial. A total of 36,852 patients, aged more than 65, who were newly diagnosed with ESKD and initiated renal replacement therapy between 2013 and 2019 were identified. These patients were categorized into two groups: the PD group and the HD group according to their long-term renal replacement treatment. After propensity score matching, the PD group (n = 1628) displayed a lower incidence of major adverse cardiac and cerebrovascular events (MACCE) (10.09% vs. 13.03%, hazard ratio (HR): 0.74, 95% confidence interval (CI): 0.66–0.83), malignancy (1.23% vs. 2.14%, HR: 0.55, 95% CI: 0.40–0.76), and MACCE-associated mortality (1.35% vs. 2.25%, HR: 0.62, 95% CI: 0.46–0.84) compared to the HD group (n = 6512). However, the PD group demonstrated a higher rate of infection (34.09% vs. 24.14%, HR: 1.28, 95% CI: 1.20–1.37). The risks of all-cause mortality and infection-associated mortality were not different. This study may provide valuable clinical information to assist elderly ESKD patients to choose HD or PD as their renal replacement therapy.
Similar content being viewed by others
For patients who are newly diagnosed with end-stage kidney disease (ESKD) and require renal replacement therapy, kidney transplantation has been proven to be the most effective treatment, regardless of whether it is from a living donor or a cadaveric donor1,2,3. However, suitable donors are not always available, and most ESKD patients still need a waiting time before successful transplantation. According to a report from Taiwan in 2019, the average waiting time for a kidney transplant was 4.7 years4. Thus, to decide to receive hemodialysis or peritoneal dialysis (PD), which are the two major renal replacement therapy, is inevitable for most patients with new-onset ESKD. Hemodialysis involves the use of an artificial semi-permeable membrane, known as a dialyzer, to remove uremic toxins from the patient's blood. This process typically lasts for around 4 h and requires complex equipment such as a dialysis machine to pump blood into the dialyzer and a water filter system to prevent bacteria or toxins from entering the patient’s bloodstream. Skilled professionals are also needed to perform tasks like arteriovenous fistula (AVF) puncture5. Except for certain limited areas, most hemodialysis patients are required to receive treatment at specific facilities, such as dialysis centers or hospitals6. On the other hand, PD, which removed uremia toxin through patients’ own peritoneum via infusion of dialysate into abdominal cavity and release it after several hours of dwelling time. The requirement of technic and equipment of PD is relatively simple compared to hemodialysis and thus could be performed by patient self or families. Since PD is a home-based treatment, compared to Hemodialysis, it may have less impact on patients' original lifestyle and may improve health-related quality of life7,8.
Aging is a crucial and continuous global healthcare issue in these decades, for example, in Taiwan, people aged more than 65 will account for more than 20% of the total population by 20259,10. Similarly, the number of elderly patients with newly diagnosed end-stage kidney disease (ESKD) has been rapidly increasing, and this trend shows no sign of slowing down in the coming years4. The percentage of ESKD patients aged more than 65 has exceeded 50% of whole ESKD population in Taiwan by 20174. Due to the risks associated with surgery and anesthesia, as well as factors like performance and cognitive status, polypharmacy (including drug-drug interactions with immunosuppressants), and shorter life expectancy, elderly ESKD patients have a lower rate of receiving kidney transplants11,12. As a result, the decision to receive either hemodialysis or PD, both of which may be lifelong treatments, becomes even more crucial for elderly ESKD patients compared to younger patients. Along with patients aging, the progressively difficult mobility13, cognitive decline, frailty, and susceptible to infectious disease make PD, a home-based treatment, which may help the elderly ESKD patients to remain in their community and maintain their original daily life, an attractive option. However, to make an informed decision, elderly ESKD patients need more objective information about crucial outcomes, such as mortality rates, risks of cardiovascular events, infection diseases, and malignancy, which are of utmost importance for this age group. Currently, there is only limited research available that evaluates these essential outcomes between hemodialysis and PD among elderly ESKD patients, and the results are inconsistent. Therefore, a large-scale comprehensive study is warranted for better understanding the following outcomes after receiving maintenance hemodialysis or PD among elderly patients.
Until 2019, according to data from National Healthcare Insurance Research database (NHIRD), approximately 86,840 patients underwent dialysis in Taiwan, of which about 6,901 patients received peritoneal dialysis4. Moreover, NHIRD can provide comprehensive and detailed clinical information about these patients. By utilizing these abundant data, this study is aimed to evaluate all-cause mortality, CV outcomes, malignancy risks, and frequency of hospitalizations between PD and HD among ESKD patients aged more than 65.
Materials and methods
Data source
The patient data of this study were obtained from NHIRD. Taiwan’s National Health Insurance (NHI) program, which is a single-payer, mandatory enrollment system, have launched since March 1, 1995. In this system, all medical costs are covered by a single public entity, and all medical institutions in Taiwan are required to join in14 As a result, this program covers nearly 100% of Taiwan's population. Furthermore, the NHIRD provides academic units and scholars with access for research in medical and public health-related fields. After application, the NHIRD provides detailed information for researchers, including outpatient visits, hospitalizations, disease diagnoses, surgeries, and the drug use. Regarding diagnoses, the International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) was used before 2016 and ICD-10 has been adopted thereafter. Moreover, in Taiwan, the patients with new-onset ESKD would obtain certifications as having catastrophic illness and then the copayment of dialysis would be covered by NHI. All applications for this catastrophic illness certification are comprehensively reviewed by experts, thereby ensuring a high degree of diagnostic accuracy. As a result, the data from the catastrophic illness file has been extensively utilized for case verification in various related studies. The NHIRD has replaced the names or identifications of patients, healthcare providers, and medical institutions with anonymous numbers to protect patient privacy15. Thus, because this was a database study by using the NHIRD, the requirement for written informed consent was waived. This study has been performed in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of the Chang Gung Medical Foundation (IRB number: 201900840B0).
Study design
In our study, we utilized data from the NHIRD to evaluate the risks of major adverse cardiac and cerebrovascular events (MACCE), infection, malignancy, or infection and MACCE induced mortality between patients under PD and HD. As shown in Fig. 1, patients aged 65 years or older were included if they obtained ESKD catastrophic illness certification, which indicated new-onset ESKD initiating long-term dialysis, from January 1, 2013, to December 31, 2019. The index date was defined as the date of the next dialysis session after obtaining the catastrophic disease certificate. Exclusion criteria were: 1. Patients without diagnosis of previous chronic kidney disease before index date 2. Patients without records of dialysis 3. Incomplete demographic data 4. Presence of malignancy before the index date 5. History of kidney transplantation before the index date 6. Change from PD to HD or HD to PD within the first 90 days after the index date because numerous prior papers used the 90 days as the dividing point16,17,18. Finally, if a patient undergoes PD on the index date, they would be assigned to the PD group, and vice versa. If patients remained on PD or HD for more than 90 days after the index date and were initially categorized into the PD or HD group, they would continue to be classified in the same group, even if they later switched to the other type of dialysis or underwent kidney transplantation after this 90-day period. However, it's important to note that the observational period for the outcomes we calculated only extends up to the day before they switched to the other type of dialysis or underwent kidney transplantation.
Covariates and outcomes
In this study, the covariates included age, gender, level of residential urbanization, primary renal diseases, comorbidities, Charlson Comorbidity Index (CCI)19, index date, hospitalization history, abdominal surgery history and medication usage. The primary renal diseases in question were hypertensive nephropathy, DM nephropathy, chronic glomerulonephritis (eg, lupus nephritis, IGA nephropathy, and focal segmental glomerulosclerosis), and other forms of renal disease (eg, obstructive nephropathy and interstitial nephritis). Comorbidities were identified if they were reported for more than two outpatient visits or one inpatient stay within the year prior to the index date, which was adopted by numerous previous database studies to define the comorbidities20,21. Medications were identified according to the prescriptions within 3 months preceding the index date.
We focused on outcomes such as MACCE (a composite of myocardial infarction, cardiogenic shock, newly diagnosed heart failure, coronary revascularization, malignant arrhythmia, stroke, and cerebrovascular events), infection, malignancy, MACCE-related mortality, infection-related mortality, and overall mortality. MACCE and infection events were identified according to the principal diagnosis during inpatient, outpatient, or emergency room visits. The diagnosis of malignancy occurrence is based on obtaining catastrophic illness certification of malignancy, as the application for this certification requires both evidence from histopathological biopsy and image examinations. All-cause mortality was defined as the patient's name appearing in the Taiwan Death Registry. Due to the potential decline in peritoneal function with prolonged PD duration, a significant number of patients who initially start with PD may switch to HD after approximately 10 years. This disparity in treatment duration between PD and HD could introduce an observational interval imbalance. To mitigate this bias, we have limited our analysis to outcomes within the first 5 years of treatment.
Statistical analysis
We employed the one-to-four propensity score matching (PSM), in which each patient in the PD group was matched with four counterparts in the HD group. The propensity score was the predicted probability in the PD group derived from logistic regression with all variables listed in Table 1, except for the CCI, which is inherently a composite of other covariates. Then, we can directly compare the outcomes between the two types of dialysis by using the propensity score-matched sample22,23,24. The balance of potential confounders between the groups at the index date was evaluated using the absolute standardized mean difference (ASMD) rather than statistical tests. This is because balance refers to an attribute of the sample and not of the underlying population. An ASMD value of ≤ 0.1 suggested a negligible difference in potential confounders between the groups, whereas an ASMD value between 0.1 and 0.2 indicated a small difference between the groups.
The incidence was calculated by dividing the total number of study results during the follow-up period by the person-years at risk. The all-cause mortality between the groups were compared with the Cox proportional hazards model. Other time-to-event outcomes, such as infection-related death and malignancy, were evaluated using a subdistribution hazard model that treated death during the follow-up period as a competing risk. We plotted the Kaplan–Meier curve for all-cause mortality and subdistribution cumulative incidence function for other time-to-event outcomes. In subgroup analysis, we re-estimated PSM to maintain the balance of covariates in each subgroup. A p-value less than 0.05 indicated statistical significance. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Patient characteristics
A total of 36,852 patients, aged more than 65, who were newly diagnosed with ESKD and initiated renal replacement therapy between 2013 and 2019 were identified from NHIRD (Fig. 1). Of these patients, 35,175 received hemodialysis and 1,677 received peritoneal dialysis. Table 1 presents the baseline characteristics of the two groups before long-term dialysis. Before propensity score matching, the HD group had a greater proportion of older patients, a lower rate of dependence, a higher Charlson comorbidity index score, a higher likelihood of hospitalization, a higher prevalence of DM and DM nephropathy and more frequent use of certain medications (i.e., aspirin/clopidogrel, non-steroidal anti-inflammatory drugs, insulin, and oral hypoglycemic agents) compared to the PD group. After propensity score matching, most ASMD values were less than 0.1 and all ASMD values were less than 0.2, indicating that the clinical characteristics between the groups were well balanced. It's worth noting that, whether before or after PSM, the comorbidity of dementia and the history of abdominal surgery between the PD and HD groups showed no significant difference.
Outcomes
Our objective was to evaluate the five-year outcomes between PD and HD regarding MACCE, infection, malignancy, MACCE-related mortality, infection-related mortality and all-cause mortality in new-onset ESKD patients aged 65 and older. The detailed 5-year outcomes are listed in Table 2.
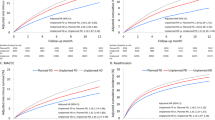
After PSM, compared to the HD group, the PD group exhibited lower rates (per person-years) of MACCE (10.09% vs. 13.03%, hazard ratio (HR): 0.74, 95% confidence interval (CI): 0.66–0.83), malignancy (1.23% vs. 2.14%, HR: 0.55, 95% CI: 0.40–0.76), and MACCE-associated mortality (1.35% vs. 2.25%, HR: 0.62, 95% CI: 0.46–0.84). On the contrary, the risks of infection were higher in the PD group (34.09% vs. 24.14%, HR: 1.28, 95% CI: 1.20–1.37). However, we found that PD-associated peritonitis or catheter infections represented a large part of infection events in PD group. After excluding PD-associated infections, the risks of other infections were lower in the PD group compared to the HD group. The risks of all-cause mortality (14.32% vs. 14.77%, HR: 0.98, 95% CI: 0.89–1.07) and infection-associated mortality (5.78% vs. 6.10%, HR: 0.93, 95% CI: 0.81–1.08) did not significantly differ between the two groups. Figure 2 presents the cumulative incidence of MACCE, infections, malignancy, and MACCE-associated mortality.
Subgroup analysis
To ascertain if the benefits of PD or HD are only observed under specific clinical conditions, we further conducted subgroup analyses for MACCE, infection, and malignancy (Fig. 3). Concerning MACCE, PD demonstrated superior performance over HD in most subgroups. About infection, on the contrary, HD outperformed PD in most subgroups, especially in female and a CCI of 3 or higher. In the context of malignancy, PD demonstrated superior performance over HD in most subgroups.
Mean times of hospitalizations between PD and HD
In this study, we observed that patients in the PD group had a lower hospitalization rate during the first year of treatment. However, in the subsequent 2–5 years, they experienced a higher hospitalization rate (Table 3). Despite a statistically significant difference between the two groups, the hospitalization rates were relatively close (Fig. 4).
Discussion
Because population ageing and the progress of medicine, new-onset ESKD patients aged more than 65 years old increased rapidly in recent decades. Since large portion of elderly ESKD patients would not receive kidney transplantation due to the shorter life expectancy, the decision of receiving PD or HD for this population may be more crucial than younger ESKD patients. By using a large-scale database, this study is aimed to evaluate the risks of all-cause mortality, CV events, infection, and malignancy, which are the most critical health issues in elderly patients, between PD and HD.
Regarding the CV risks, elderly patients under PD seems to be superior to patients under HD. We speculated that the reasons might be multifactorial, including the higher prevalence of myocardial stunning, intradialytic hypotension, cardiac arrhythmias, and transient hypoperfusion of brain during the process of HD25,26. In patients under HD, the accumulated uremia toxin and fluid are required to be removed in a short interval and therefore the cardiac hypoperfusion is common. This phenomenon, known as myocardial stunning, can lead to increased CV mortality in ESKD patients. 27,28,29,30 A prior study from Taiwan have indicated that HD is more likely to result in new onset of coronary artery disease than PD31. In addition, the occurrence of arrhythmias in hemodialysis patients is also higher than in peritoneal dialysis patients. A 2019 report on newly diagnosed dialysis in older people found that the chance of new-onset atrial fibrillation was higher in the HD group than the PD group32. In addition, intradialytic hypotension is more common in HD patients, which leads to a higher chance of intradialytic arrhythmia in HD patients33. Intradialytic hypotension is a cause of morbidity and mortality in elderly patient. 34 A 2018 study on hemodialysis in older people pointed out that the process of hemodialysis will lead to a decline in cerebral blood flow. If intradialytic cerebral blood flow declines continue to occur, it may lead to ischemic stroke35.
In this study, we observed that HD was superior to PD in infection rates. Infection is the second most common reason for hospitalization among dialysis patients4. PD- associated peritonitis represents a significant hurdle for patients considering PD as a dialysis modality. Indeed, in this study, we found PD-associated peritonitis or catheter infection represented a large part of infection events in PD group. A previous study has demonstrated that PD-associated peritonitis is the most prevalent cause for patients transitioning to HD and carries a mortality rate of 2–6%36. However, along with the improvement of design of PD dialysis devices and the use of effective intra-peritoneal antibiotics, PD-associated peritonitis has resulted in less mortality and technical failure in recent years7,37,38. Thus, although the risks of infection among patients under PD is higher in our study and may consequently result in a slightly higher hospitalization rate, especially since the second year of dialysis, we found no significant difference in all-cause mortality or infection-related mortality between PD and HD. We believed this information is crucial for new-onset ESKD patients to choose dialysis modalities.
The risks of malignancy are another critical issue for elderly patients. Interestingly, this study found that the risks of new-onset malignancy are higher in patients undergone HD compared to PD. The incidence of cancer is higher in patients with ESKD compared to the general population39,40,41. However, there are very few studies investigating which renal replacement modality is associated with the higher incidence of cancer. One prior study indicated that the incidence of cancer was lowest in kidney transplant patients, followed by peritoneal dialysis patients, with the highest incidence observed in hemodialysis patients42. For the elderly ESKD patients, our study reached a similar conclusion. A 2017 study in Taiwan informed us that among new dialysis patients, liver cancer is most prevalent, especially in male patients43. Other two studies also indicated that age greater than 65 and chronic liver disease are risk factors for cancer in dialysis patients44,45. Patients under HD have a higher chance to contact Hepatitis B virus and Hepatitis C virus compared to the patients under PD, thereby may increase their likelihood of developing liver cancer in the future46,47. However, to in-depth analyze why the PD patients are associated with lower risks of malignancy and the differences are mainly in which kinds of cancers is beyond the scope of this study. Our research team intends to design further studies to answer these questions comprehensively.
This study has several limitations that should be acknowledged. Firstly, the data analyzed in this study was retrieved from the NHIRD, which lacks certain laboratory data, such as hemoglobin, creatinine, lipid profiles, albumin, and electrolyte levels. This limitation may have affected the comprehensiveness of our analysis. Secondly, being an observational cohort study, it may be susceptible to inherent biases. Nevertheless, conducting randomized clinical trials to evaluate the outcomes of different dialysis modalities would be impractical and ethically challenging. Third, despite the utilization of matching methods, the potential for residual confounding cannot be completely eliminated. For example, if relevant factors (such as dietary habits, smoking, radiation, alcohol, etc.) are not fully adjusted, residual confounding could impact the research findings. Besides, because patients did not randomly select.
PD or HD as long-term treatment, their self-care ability, personality, and familial support system are likely to have influenced their choices, potentially introducing selection bias. Fourth, our study lacked data on cancer-related risk factors, such as smoking and family history of cancer, and information on types of cancer, stages, and mortality rates were not available in our study. These limitations impeded our ability to explore the possible mechanisms behind the increased risk of malignancy occurrence in elderly HD patients compared to those on PD. Our research team plans to design a follow-up study to address this issue.
In conclusion, for the elderly patients with new-onset ESKD, this study found that peritoneal dialysis presents lower risks in MACCE, malignancy, and MACCE associated mortality but is associated with higher risks of infection and slightly higher frequency of hospitalization. The all-cause mortality or infection-related mortality did not differ between PD and HD. This information may help elderly ESKD patients to better choose HD or PD as long-term renal replacement therapy.
Data availability
The datasets generated and analysed during the current study are not publicly available because the NHIRD dataset can only be accessed after a qualified investigator submits an application.
References
Nesrallah, G. & Mendelssohn, D. C. Modality options for renal replacement therapy: The integrated care concept revisited. Hemodial. Int. 10, 143–151 (2006).
Tonelli, M. et al. Systematic review: Kidney transplantation compared with dialysis in clinically relevant outcomes. Am. J. Transplant. 11, 2093–2109. https://doi.org/10.1111/j.1600-6143.2011.03686.x (2011).
Poggio, E. D., Augustine, J. J., Arrigain, S., Brennan, D. C. & Schold, J. D. Long-term kidney transplant graft survival-Making progress when most needed. Am. J. Transplant. 21, 2824–2832. https://doi.org/10.1111/ajt.16463 (2021).
Nephrology, T. S. o. Annual report on kidney disease in Taiwan. Taiwan Society of Nephrology (2021).
Hakim, R. M. in National Kidney Foundation Primer on Kidney Diseases (Sixth Edition) (eds Scott J. Gilbert & Daniel E. Weiner) 508–519 (W.B. Saunders, 2014).
Sinnakirouchenan, R. & Holley, J. L. Peritoneal dialysis versus hemodialysis: Risks, benefits, and access issues. Adv. Chronic Kidney Dis. 18, 428–432 (2011).
Biebuyck, G. K. M., Neradova, A., de Fijter, C. W. H. & Jakulj, L. Impact of telehealth interventions added to peritoneal dialysis-care: A systematic review. BMC Nephrol. 23, 292. https://doi.org/10.1186/s12882-022-02869-6 (2022).
Zazzeroni, L., Pasquinelli, G., Nanni, E., Cremonini, V. & Rubbi, I. Comparison of quality of life in patients undergoing hemodialysis and peritoneal dialysis: A systematic review and meta-analysis. Kidney Blood Press. Res. 42, 717–727. https://doi.org/10.1159/000484115 (2017).
Nations, U. World population ageing, 1950–2050. (UN, 2002).
Lin, Y.-Y. & Huang, C.-S. Aging in Taiwan: Building a society for active aging and aging in place. Gerontologist 56, 176–183 (2016).
Huang, E., Segev, D. L. & Rabb, H. Kidney transplantation in the elderly. Semin. Nephrol. 29, 621–635. https://doi.org/10.1016/j.semnephrol.2009.07.011 (2009).
Yemini, R., Rahamimov, R., Ghinea, R. & Mor, E. Long-term results of kidney transplantation in the elderly: Comparison between different donor settings. J. Clin. Med. https://doi.org/10.3390/jcm10225308 (2021).
Daley, M. J. & Spinks, W. L. Exercise, mobility and aging. Sports Med. 29, 1–12. https://doi.org/10.2165/00007256-200029010-00001 (2000).
Administration, N. H. I. (2023).
Hsieh, C. Y. et al. Taiwan’s national health insurance research database: past and future. Clin. Epidemiol. https://doi.org/10.2147/CLEP.S196293 (2019).
Boissinot, L. et al. Is transition between peritoneal dialysis and hemodialysis really a gradual process?. Perit. Dial. Int. 33, 391–397. https://doi.org/10.3747/pdi.2011.00134 (2013).
Nessim, S. J. et al. The impact of transfer from hemodialysis on peritoneal dialysis technique survival. Perit. Dial. Int. 35, 297–305. https://doi.org/10.3747/pdi.2013.00147 (2015).
Nadeau-Fredette, A.-C. et al. Mortality trends after transfer from peritoneal dialysis to hemodialysis. Kidney Int. Rep. 7, 1062–1073. https://doi.org/10.1016/j.ekir.2022.02.016 (2022).
Hemmelgarn, B. R., Manns, B. J., Quan, H. & Ghali, W. A. Adapting the Charlson comorbidity index for use in patients with ESRD. Am. J. Kidney Dis. 42, 125–132 (2003).
Valderas, J. M., Starfield, B., Sibbald, B., Salisbury, C. & Roland, M. Defining comorbidity: Implications for understanding health and health services. Ann. Fam. Med. 7, 357–363. https://doi.org/10.1370/afm.983 (2009).
Cheng, Y.-L. et al. Does statin therapy reduce the risks of mortality and major adverse cardiac and cerebrovascular events in young adults with end-stage renal disease? Population-based cohort study. J. Clin. Med. 10, 2097 (2021).
Haukoos, J. S. & Lewis, R. J. The propensity score. JAMA 314, 1637–1638. https://doi.org/10.1001/jama.2015.13480 (2015).
Rassen, J. A. et al. One-to-many propensity score matching in cohort studies. Pharmacoepidemiol. Drug Saf. 21, 69–80 (2012).
Austin, P. C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 28, 3083–3107 (2009).
Albakr, R. B. & Bargman, J. M. A comparison of hemodialysis and peritoneal dialysis in patients with cardiovascular disease. Cardiol. Clin. 39, 447–453. https://doi.org/10.1016/j.ccl.2021.04.013 (2021).
Brown, E. A., Finkelstein, F. O., Iyasere, O. U. & Kliger, A. S. Peritoneal or hemodialysis for the frail elderly patient, the choice of 2 evils?. Kidney Int. 91, 294–303. https://doi.org/10.1016/j.kint.2016.08.026 (2017).
Burton, J. O., Jefferies, H. J., Selby, N. M. & McIntyre, C. W. Hemodialysis-induced repetitive myocardial injury results in global and segmental reduction in systolic cardiac function. Clin. J. Am. Soc. Nephrol. 4, 1925–1931. https://doi.org/10.2215/cjn.04470709 (2009).
McIntyre, C. W. Haemodialysis-induced myocardial stunning in chronic kidney disease—A new aspect of cardiovascular disease. Blood Purif. 29, 105–110. https://doi.org/10.1159/000245634 (2010).
Selby, N. M. & McIntyre, C. W. Peritoneal dialysis is not associated with myocardial stunning. Perit. Dial. Int. 31, 27–33. https://doi.org/10.3747/pdi.2010.00007 (2011).
Buchanan, C. et al. Intradialytic cardiac magnetic resonance imaging to assess cardiovascular responses in a short-term trial of hemodiafiltration and hemodialysis. J. Am. Soc. Nephrol. 28, 1269–1277. https://doi.org/10.1681/asn.2016060686 (2017).
Hung, Y. M. et al. Association between dialysis modalities and risk of coronary artery disease: A population-based cohort study in Taiwan. Ther. Apher. Dial. 22, 469–475. https://doi.org/10.1111/1744-9987.12676 (2018).
Niu, J. et al. Dialysis modality and incident atrial fibrillation in older patients with ESRD. Am. J. Kidney Dis. 73, 324–331. https://doi.org/10.1053/j.ajkd.2018.09.011 (2019).
Mc Causland, F. R. et al. Intradialytic hypotension and cardiac arrhythmias in patients undergoing maintenance hemodialysis results from the monitoring in dialysis study. Clin. J. Am. Soc. Nephrol. 15, 805–812. https://doi.org/10.2215/cjn.06810619 (2020).
Sands, J. J. et al. Intradialytic hypotension: Frequency, sources of variation and correlation with clinical outcome. Hemodial. Int. 18, 415–422. https://doi.org/10.1111/hdi.12138 (2014).
Polinder-Bos, H. A. et al. Hemodialysis induces an acute decline in cerebral blood flow in elderly patients. J. Am. Soc. Nephrol. 29, 1317–1325. https://doi.org/10.1681/asn.2017101088 (2018).
Cho, Y. & Johnson, D. W. Peritoneal dialysis–related peritonitis: Towards improving evidence, practices, and outcomes. Am. J. Kidney Dis. 64, 278–289 (2014).
Okpechi, I. G. et al. Prevalence of peritonitis and mortality in patients with ESKD treated with chronic peritoneal dialysis in Africa: a systematic review. BMJ open 10, e039970 (2020).
Xu, X. et al. Telemedicine and clinical outcomes in peritoneal dialysis: A propensity-matched study. Am. J. Nephrol. 53, 663–674. https://doi.org/10.1159/000525917 (2022).
Butler, A. M. et al. Cancer incidence among US Medicare ESRD patients receiving hemodialysis, 1996–2009. Am. J. Kidney Dis. 65, 763–772 (2015).
Liang, J. A. et al. The association between malignancy and end-stage renal disease in Taiwan. Jpn. J. Clin. Oncol. 41, 752–757. https://doi.org/10.1093/jjco/hyr051 (2011).
Lin, M. Y. et al. Association of dialysis with the risks of cancers. PLoS One 10, e0122856. https://doi.org/10.1371/journal.pone.0122856 (2015).
Lee, M. J., Lee, E., Park, B. & Park, I. Epidemiological characteristics of cancers in patients with end-stage kidney disease: A Korean nationwide study. Sci. Rep. 11, 3929. https://doi.org/10.1038/s41598-021-83164-6 (2021).
Chien, C. C. et al. Epidemiology of cancer in end-stage renal disease dialysis patients: A national cohort study in Taiwan. J. Cancer 8, 9–18. https://doi.org/10.7150/jca.16550 (2017).
Wong, G. et al. Association of CKD and cancer risk in older people. J. Am. Soc. Nephrol. 20, 1341–1350. https://doi.org/10.1681/asn.2008090998 (2009).
Lee, J. E. et al. Cancer in patients on chronic dialysis in Korea. J. Korean Med. Sci. 24(Suppl), S95-s101. https://doi.org/10.3346/jkms.2009.24.S1.S95 (2009).
Patel, P. R., Thompson, N. D., Kallen, A. J. & Arduino, M. J. Epidemiology, surveillance, and prevention of hepatitis C virus infections in hemodialysis patients. Am. J. Kidney Dis. 56, 371–378. https://doi.org/10.1053/j.ajkd.2010.01.025 (2010).
Edey, M., Barraclough, K. & Johnson, D. W. Review article: Hepatitis B and dialysis. Nephrology 15, 137–145. https://doi.org/10.1111/j.1440-1797.2009.01268.x (2010).
Acknowledgements
The authors thank the statistical assistance and wish to acknowledge the support of the Maintenance Project of the Center for Big Data Analytics and Statistics (Grant CLRPG3N0011) at Chang Gung Memorial Hospital for study design and monitor, data analysis and interpretation.
The authors thank Mr. Yu-Tung Huang, and Miss Hui-Tzu Tu, for their assistance in the statistical analysis.
Author information
Authors and Affiliations
Contributions
Y.K.P., T.S.T., and C.L.Y. developed the concept for this study. C.Y.W., C.Y.T., C.C.H. provided substantial assistance in data collection. C.C.L., J.J.C., and H.Y.Y performed statistical analyses. Y.C.C and H.Y.Y contributed to data interpretation. Y.K.P and C.L.Y wrote the initial draft of the manuscript. All authors reviewed the manuscript and approved its final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peng, YK., Tai, TS., Wu, CY. et al. Clinical outcomes between elderly ESKD patients under peritoneal dialysis and hemodialysis: a national cohort study. Sci Rep 13, 16199 (2023). https://doi.org/10.1038/s41598-023-43476-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43476-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.