Abstract
In the absence of available data, we evaluated the effects of delayed hospitalization (symptom-to-door time [SDT] ≥ 24 h) on major clinical outcomes after new-generation drug-eluting stent implantation in patients with non-ST-segment elevation myocardial infarction (NSTEMI) and complex lesions. In total, 4373 patients with NSTEMI were divided into complex (n = 2106) and non-complex (n = 2267) groups. The primary outcome was the 3-year rate of major adverse cardiac events (MACE), defined as all-cause death, recurrent MI, and any repeat revascularization. Secondary outcomes included the individual MACE components. In the complex group, all-cause death (adjusted hazard ratio [aHR], 1.752; p = 0.004) and cardiac death (aHR, 1.966; p = 0.010) rates were significantly higher for patients with SDT ≥ 24 h than for those with SDT < 24 h. In the non-complex group, all patients showed similar clinical outcomes. Patients with SDT < 24 h (aHR, 1.323; p = 0.031) and those with SDT ≥ 24 h (aHR, 1.606; p = 0.027) showed significantly higher rates of any repeat revascularization and all-cause death, respectively, in the complex group than in the non-complex group. Thus, in the complex group, delayed hospitalization was associated with higher 3-year mortalities.
Similar content being viewed by others
For patients with ST-segment elevation myocardial infarction (STEMI), rapid restoration of blood flow in the infarct-related artery (IRA) is critical to salvage the ischemic myocardium and improve long-term mortality1,2. Therefore, primary percutaneous coronary intervention (PPCI) is recommended for all STEMI patients presenting within 12 h of symptom onset1,2. However, published data concerning the effects of PCI on long-term clinical outcomes in STEMI patients who present > 12 h after symptom onset (latecomers) is inconsistent3,4,5. Previous reports have emphasized the importance of shortening the door-to-balloon time (DBT, < 60 min) to improve survival in patients with STEMI6,7. A recent report8 showed that DBT did not affect mortality in 4839 PPCI‐treated patients. Because the DBT interval occupies a later period in the flat slope of the time-myonecrosis curve, reperfusion has a small impact on myocardial salvage during this period; the total ischemic time becomes more important8. Considering these observations8, the symptom-to-door time [SDT] can be more important than DBT9. With regard to non-STEMI (NSTEMI), a previous study9 including patients with NSTEMI found that patients with delayed hospitalization (SDT ≥ 24 h) exhibited a higher 3-year mortality rate than did those without delayed hospitalization (SDT < 24 h) (17.0% vs. 10.5%, p < 0.001). However, approximately 15% of the study population did not receive PCI or had underwent unsuccessful PCI, and patients who received bare-metal stents or first-generation drug-eluting stents (DES) were included9. Moreover, some important laboratory results of patients with acute myocardial infarction (AMI), such as cardiac biomarkers, the lipid profile, and serum creatinine levels, were not included in the baseline characteristics of the study population. Because of these limitations, this study9 could not accurately reflect current real-world practice. To the best of our knowledge, there are no large-scale studies comparing long-term clinical outcomes according to the presence or absence of delayed hospitalization in patients with NSTEMI and complex lesions. Compared to non-complex lesions, PCI for complex lesions frequently requires extended procedural durations and specialized interventional skills and techniques, and is often associated with the risk of hemodynamic instability10. Therefore, considering the association between increased mortality and delayed hospitalization in patients with NSTEMI9, we investigated the impact of delayed hospitalization on clinical outcomes in complex and non-complex groups, as well as the total study population in order to provide a more precise understanding of the significance of delayed hospitalization in patients with NSTEMI. We also attempted to identify independent predictors of poorer clinical outcomes in NSTEMI patients with complex lesions, with the aim of effectively addressing and managing these independent predictors to improve the clinical outcomes of these patients. To reflect current real-world practice, we limited the study population to patients with NSTEMI who received successful new-generation DES implantation. Finally, according to the presence or absence of complex lesions, we compared clinical outcomes between NSTEMI patients with SDT < 24 h and those with SDT ≥ 24 h who received successful new-generation DES implantation.
Results
Baseline characteristics
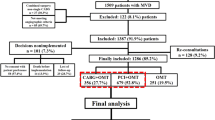
Figure 1 shows the study flowchart. Table 1 shows the baseline characteristics of the SDT < 24 h and SDT ≥ 24 h groups according to the presence or absence of complex lesions. In both the NSTEMI and complex group (complex group) and NSTEMI and non-complex group (non-complex group), the number of male patients, current smokers, and patients who used emergency medical services (EMS) to arrive at the hospital; the mean systolic blood pressure and diastolic blood pressure values; and peak creatine kinase myocardial band (CK-MB), troponin-I, and blood glucose levels were higher for patients with SDT < 24 h than for patients with SDT ≥ 24 h. In contrast, the mean age; the mean Global Registry of Acute Coronary Events (GRACE) risk score; the number of patients with atypical chest pain and dyspnea, Killip class II/III, hypertension, and diabetes mellitus; and number of people who visited hospitals incapable of performing PCI were higher in the SDT ≥ 24 h group than in the SDT < 24 h group. Table S1 in the Supplementary Appendix shows the baseline characteristics in the complex and non-complex groups according to the presence or absence of delayed hospitalization. For both patients with SDT < 24 h and those with SDT ≥ 24 h, the mean age; the number of patients with Killip class II/III, hypertension, diabetes mellitus, and the American College of Cardiology/American Heart Association (ACC/AHA) type B2/C lesions; and mean blood glucose levels were higher in the complex group than in the non-complex group. However, the mean left ventricular ejection fraction (LVEF) was higher in the non-complex group than in the complex group. Table S2 in the Supplementary Appendix compares the baseline characteristics between the SDT < 24 h and SDT ≥ 24 h groups in the total study population and propensity score (PS)-matched population.
Flowchart. AMI acute myocardial infarction, KAMIR-NIH Korea Acute Myocardial Infarction Registry-National Institute of Health, PCI percutaneous coronary intervention, POBA plain old balloon angioplasty, CABG coronary artery bypass graft, BMS bare-metal stent, DES drug-eluting stent, STEMI ST-segment-elevation myocardial infarction, NSTEMI non-STEMI, CPR cardiopulmonary resuscitation, SDT symptom-to-door time. Complex lesions were defined as PCI for unprotected left main coronary disease, multivessel PCI, multiple stents implantation (≥ 3 stents per patient), or those with the total length of deployed stent being over 38 mm.
Clinical outcomes
The 3-year major clinical outcomes are summarized in Tables 2, 3, and Fig. 2. In the complex group, after multivariable-adjusted analyses, the major adverse cardiac events (MACE) rate (adjusted hazard ratio [aHR], 1.217; 95% confidence interval [CI], 0.923–1.640; p = 0.164; Fig. 2A) was similar in the SDT < 24 h and SDT ≥ 24 h groups. However, all-cause death (aHR, 1.752; 95% CI, 1.194–2.569; p = 0.004; Fig. 2B) and cardiac death (CD) (aHR, 1.966; 95% CI, 1.179–3.280; p = 0.010; Fig. 2C) rates were significantly higher for patients with SDT ≥ 24 h than for those with SDT < 24 h. The non-CD (NCD, Fig. 2D), recurrent MI (Fig. 2E), and repeat revascularization (Fig. 2F) rates were not significantly different patients with SDT < 24 h and those with SDT ≥ 24 h (Table 2). In the non-complex group, the primary and secondary outcomes were not significantly different patients with SDT < 24 h and those with SDT ≥ 24 h. In the total study population, the all-cause death (aHR, 1.512; 95% CI 1.125–2.033; p = 0.006) and CD (aHR, 1.614; 95% CI 1.100–2.448; p = 0.015) rates were significantly higher for patients with SDT ≥ 24 h than for those with SDT < 24 h (Table 2). These results were confirmed by PS-adjusted analyses (Table 2). For patients with SDT < 24 h group, multivariable-adjusted analyses showed that MACE (aHR, 1.235; p = 0.034) and repeat revascularization (aHR, 1.323; p = 0.031) rates were significantly higher in the complex group than in the non-complex group (Table 3). For patients with SDT ≥ 24 h, the MACE (aHR, 1.381; p = 0.039) and all-cause death (aHR, 1.606; p = 0.027) rates were significantly higher in the complex group than in the non-complex group (Table 3). When the total study population was considered, MACE (aHR, 1.283; p = 0.003), all-cause death (aHR, 1.303; p = 0.033), and repeat revascularization (aHR, 1.281; p = 0.028) rates were significantly higher in the complex group than in the non-complex group. Figure 3A and B show the results of subgroup analysis of all-cause death. Among patients without dyspnea, those with hypertension, and those with a low GRACE risk score (< 140) in the complex group (Fig. 3A), SDT < 24 h was associated with a lower all-cause death rate than was SDT ≥ 24 h. In the non-complex group (Fig. 3B), all subgroups, except for those showing significant p-for-interaction, demonstrated comparable all-cause death rates between the SDT < 24 h and SDT ≥ 24 h groups. Table 4 shows the independent predictors of all-cause death. In both the complex and non-complex groups with NSTEMI, old age (≥ 65 years), a reduced left ventricular ejection fraction (< 50%), atypical chest pain, and a high GRACE risk score were common independent predictors of all-cause death.
Kaplan–Meier curved analysis for MACE (A), all-cause death (B), cardiac death (C), non-cardiac death (D), recurrent MI (E), and any repeat revascularization (F). MACE major adverse cardiac events, SDT symptom-to-door time, aHR adjusted hazard ratio, PCI percutaneous coronary intervention, MI myocardial infarction.
Discussion
The main findings of this nonrandomized, multicenter, prospective cohort study were as follows. First, in the complex group and the total study population, all-cause death and CD rates were significantly higher for patients with SDT ≥ 24 h than for those with SDT < 24 h after adjustment. Second, in the non-complex group, all clinical outcomes showed no significant different between patients with SDT < 24 h and those with SDT ≥ 24 h after adjustment. Third, MACE and repeat revascularizations for patients with SDT < 24 h and MACE and all-cause death for patients with SDT ≥ 24 h were significantly higher in the complex group than in the non-complex group. Fourth, in both complex and non-complex groups, old age, a reduced left ventricular ejection fraction, atypical chest pain, and a high GRACE risk score were common independent predictors of all-cause death.
Although prehospital delay is considered an important factor in long-term mortality in patients with STEMI8, the importance of prehospital delay for patients with NSTEMI remains unclear. Till date, few studies have shown the effects of delayed hospitalization on the clinical outcomes of patients with NSTEMI9,10. As mentioned earlier, Cha et al.9 reported that the 3-year all-cause mortality was significantly higher for patients with SDT ≥ 24 h than for those with SDT < 24 h (aHR, 1.35; 95% CI, 1.17–1.56; p < 0.001). A Turkish study reported11 that patients with NSTEMI who were transferred from a non-PCI center to a PCI center showed a 60% delay in the total prehospital delay (p < 0.001).
In the present study, patients with SDT ≥ 24 h group were more likely to be older and tended to have a high cardiovascular risk profile (such as a high mean GRACE risk score and higher rates of Killip class II/III and diabetes mellitus) than did patients with < 24 h in both the complex and non-complex groups (Table 1). Interestingly, these characteristics of NSTEMI patients in our study population were similar to those of patients who presented later (between 12 and 24 h after symptom onset) in other studies3,5,12. In general, older patients may have difficulty in moving and may need help with transportation, which may contribute to delayed hospitalization13. In addition, older patients may have other comorbidities, which may lead to delayed recognition13. Delayed hospitalization in diabetes mellitus may arise from inadequate sensory feeling caused by diabetic neuropathy and a higher rate of silent myocardial infarction in this population13. In patients with acute coronary syndrome, atypical ischemic symptoms are frequent and lead to delayed hospitalization14,15. In our study, old age (≥ 65 years, p < 0.001), diabetes mellitus (p < 0.001), a high GRACE risk score (p < 0.001), and atypical chest pain (p < 0.001) were independent predictors of all-cause death in the complex group (Table 4).
Karwowski et al.16 reported that although there is a lack of data in patients with NSTEMI, rapid restoration of flow could result in a smaller infarct size and better prognosis. Therefore, patients with SDT ≥ 24 h had a larger infarct size and poorer prognosis than did those with SDT < 24 h. Compared to PCI for non-complex lesions, PCI for complex lesions typically requires a longer procedural duration and demands a relatively advanced level of procedural skills. Consequently, there is a relatively higher risk of hemodynamic instability10. Therefore, in the complex group, considering the similar DBT (p = 0.162) for patients with SDT < 24 h and those with SDT ≥ 24 h (Table 1), the former showed lower all-cause death (aHR, 1.752; p = 0.004) and CD (aHR, 1.966; p = 0.010) rates than did the latter (Table 2). Moreover, the symptom-to-balloon time was significantly lower in the SDT < 24 h group than in the SDT ≥ 24 h group (p < 0.001) (Table 1). However, in the non-complex group, the 3-year mortality rate was not significantly different between the two groups (Table 2). Because of limited data9,11 regarding long-term outcomes after new-generation DES implantation in patients with NSTEMI with SDT < 24 h and those with SDT ≥ 24, we could not compare our results with those of other studies; moreover, we could not precisely define the causal relationship in the non-complex group in our study. As reported earlier10, we speculate that because PCI for non-complex lesions is a simple technique requiring relatively short procedural times and carrying a low risk of hemodynamic deterioration, the effect of delayed hospitalization on 3-year mortality may be insignificant compared with that in the complex group. However, further studies are required to confirm our results.
A recent study17 found that patients requiring complex PCI were older and more frequently showed ACC/AHA type B2/C lesions than did patients not requiring complex PCI. As shown in Table S1 in the Supplementary Appendix, for both patients with SDT < 24 h and SDT ≥ 24 h, the mean age and number of patients with ACC/AHA type B2/C lesions were significantly higher in the complex group than that in the non-complex lesion group. Furthermore, during a 3-year follow-up period, patients who required complex PCI showed a higher rate of target lesion failure (aHR, 1.89; 95% CI, 1.31–2.73; p = 0.001) than did those not requiring complex PCI17. Riku et al.18 showed that the repeat revascularization rate was significantly higher in the complex group than in the non-complex group (log-rank p = 0.001) during a 10-year follow-up period after sirolimus-eluting stent implantation. Another study19 suggested that PCI for complex lesions was independently associated with a higher 2-year MACE rate (aHR, 1.56; p < 0.00001). In the present study, for patients with SDT < 24 h and the total study population, the repeat revascularization rates (aHR, 1.323; p = 0.031 and aHR, 1.281; p = 0.028, respectively) were significantly higher in the complex group than in the non-complex group (Table 3); this was related to a higher MACE rate for both patients with SDT < 24 h and the total study population (aHR, 1.235; p = 0.034 and aHR, 1.283; p = 0.03, respectively). Patients who underwent PCI for unprotected left main coronary disease (LM) showed a higher rate of 1-year all-cause death (5.6% vs. 2.3%; p < 0.001) than did patients who underwent PCI for non-LM20. During a 10-year follow-up period, the all-cause death rate was 2.9 times higher in patients with multivessel disease than for those with one-vessel disease21. A previous study22 showed that a stepwise increase in MACE (composite of death, MI, and target lesion revascularization (TLR)) with an increasing stent length (8.0%, 10.1%, 11.8%, and 14.8%, p < 0.001). In our study, all-cause death rates were significantly higher in the complex group than that in the non-complex group for both patients with SDT ≥ 24 h and total study population (aHR, 1.606; p = 0.027 and aHR, 1.303; p = 0.033, respectively) (Table 3).
Although we tend to assume that the long-term clinical outcomes could be poorer for patients with the complex lesions than for patents with non-complex group after PCI10, there are no data showing the different effects of delayed hospitalization on long-term clinical outcomes in these patients. From the Korea Acute Myocardial Infarction Registry-National Institute of Health (KAMIR-NIH), a conclusion could not be reached because of an insufficient sample size. However, 20 tertiary high-volume university hospitals participated in this study, and we believe that our results could provide useful information for interventional cardiologists with regard to the importance of shortening SDT, especially for patients with NSTEMI and complex lesions. Furthermore, based on the findings from Table 4, which indicate that complex lesions and delayed hospitalization are associated with a higher mortality rate in NSTEMI patients with old age, diabetes mellitus, a high GRACE risk score, and atypical chest pain, it is evident that increased attention, more proactive follow-up, and guideline-directed intensive treatment are warranted23. Therefore, we believe that our findings can contribute to a decrease in the mortality rate for patients who present with NSTEMI and complex lesions, particularly those with delayed hospitalization.
This study has some limitations. First, the KAMIR-NIH data concerning transfers, distance to the nearest hospital, and the presence or absence of large differences between hospitals in the percentage of patients with delayed hospitalization were not mandatory variables; therefore we could not include them in our analysis. We believe that this is a major limitation. Second, although bifurcation lesions and chronic total occlusion lesions could be included in the complex lesion group24,25, information regarding these variables was not available in KAMIR-NIH. Third, regarding the characteristics of the registry data, there may have been some underreported and/or missing data. Fourth, although we performed multivariable-adjusted and PS-adjusted analyses to strengthen our results, variables not included in the KAMIR-NIH study may have affected study outcomes. Fifth, because the primary and secondary outcomes were compared based on the 24 h cutoff point, the results could be altered according to different cutoff points of delayed hospitalization. Sixth, some subgroups had relatively small sample sizes; hence, their analyses may have been underpowered for the detection of clinically meaningful differences. Seventh, although the total procedure time21, total amount of radiation26, and total doses of contrast media27 during the procedure were important in the complex groups, we could not include these variables in this analysis owing to the limitations of the KAMIR-NIH data. Eighth, although previous reports28,29 showed a relationship between procedural characteristics and operator volume during PCI, the operator volume according to individual participating centers was not included in this analysis; this variable may have acted as an important source of bias in this study. Finally, the 3-year follow-up period in this study was relatively short for estimating long-term clinical outcomes.
In conclusion, this multicenter, prospective cohort study showed that among NSTEMI patients with complex lesions, delayed hospitalization was associated with a higher 3-year mortality rate. Thus, our results emphasize the importance of SDT, especially for patients with complex lesions. In addition, old age, diabetes mellitus, a high GRACE risk score, and atypical chest pain were independent predictors of all-cause death in the complex group. Therefore, patients with these factors require increased attention, proactive follow-up, and guideline-directed intensive treatment. Further large-scale and long-term follow-up studies are needed to confirm our results.
Methods
Study population
In total, 13,104 patients with AMI were recruited from KAMIR-NIH30 between November 2011 and December 2015. Twenty high-volume PCI centers in the Republic of Korea participated in the KAMIR-NIH study. At the time of initial enrollment, only patients aged ≥ 18 years were included. We excluded patients who did not undergo PCI (n = 1369, 10.4%), those who underwent balloon angioplasty (n = 739, 5.6%), unsuccessful PCI (n = 152, 1.2%), coronary artery bypass graft (CABG, n = 44, 0.4%), bare-metal stents, or first-generation (1G)-DES implantation (n = 708, 5.4%); those with STEMI (n = 5365, 40.9%); those who were lost to follow-up (n = 134, 1.0%); and those with cardiogenic shock, cardiopulmonary resuscitation on admission; and in-hospital death (n = 220) (Fig. 1). Overall, 43,733 patients with NSTEMI who underwent successful PCI using new-generation DES were enrolled and divided into complex (n = 2106, 48.2%) and non-complex (n = 2267, 51.8%). In both groups, patients were subdivided according to SDT < 24 h (group A [n = 1464] and group C [n = 1685]) and SDT ≥ 24 h (group B [n = 642] and group D [n = 582]) (Fig. 1). The types of new-generation DES used during PCI are shown in the footnotes of Table 1. According to the ethical guidelines of the 2004 Declaration of Helsinki, this study was approved by the Ethics Committee of each participating center and the Chonnam National University Hospital Institutional Review Board Ethics Committee (CNUH-2011–172). A total of 4573 patients who were included in the study provided written informed consent prior to enrollment. They completed a 3-year clinical follow-up through face-to-face interviews, phone calls, and chart reviews. Enrolled data were collected from all participating PCI centers using a web-based system. Event adjudication processes have been described in a previous publication by KAMIR investigators30. This study was performed using a web-based report from the Internet-based Clinical Research and Trial management system, supported by a grant from the Korean Centers for Disease Control and Prevention since November 2011.
PCI procedure and medical treatment
The operators performed CAG and PCI via a transfemoral or transradial approach in accordance with general guidelines31. The patients were prescribed 200–300 mg aspirin, 300–600 mg clopidogrel, 180 mg ticagrelor, and 60 mg prasugrel as loading doses before PCI. After PCI, 100 mg aspirin was recommended for all patients, combined with 75 mg clopidogrel once daily, 90 mg ticagrelor twice daily, or 5–10 mg prasugrel once daily for a minimum of one year. Individual operators were able to choose the access site, revascularization strategy, and DES without any restrictions.
Study definitions and clinical outcomes
We defined NSTEMI based on the fourth universal definition of MI32. Successful PCI was defined as residual stenosis of < 30% and thrombolysis in MI (TIMI) flow grade 3 in the IRA. We calculated the GRACE risk score33 for all enrolled patients. Complex lesions during PCI were defined per the following criteria: PCI for LM, multivessel PCI (≥ 2 major epicardial coronary vessels treated in one PCI session), multiple stent implantation (≥ 3 stents per patient), or a total deployed stent length greater than 38 mm24,25. The primary outcome was the rate of MACE defined as all-cause death, recurrent MI, and any repeat revascularization, at 3 years, while the secondary outcomes were individual MACE components. Any repeat coronary revascularization included target-lesion revascularization, target-vessel revascularization (TVR), and non-TVR. All-cause death was considered cardiac death (CD) unless an undisputed noncardiac cause was present34. Previously, we reported definitions of re-MI, TLR, TVR, and non-TVR35.
Statistical analysis
For continuous variables, between-group differences were evaluated using unpaired t-tests. Data are expressed as mean ± standard deviation or median (interquartile range). For discrete variables, between-group differences were expressed as counts and percentages and were analyzed using the chi-square or Fisher’s exact test. We performed univariate analyses for all variables in the groups with or without delayed hospitalization and the groups with or without complex lesions; a p-value of < 0.005 was considered statistical significance. Subsequently, a multicollinearity test36 was performed for the included variables to confirm the noncollinearity among them (Table S3 in the Supplementary Appendix). We measured the variance inflation factor values to determine the degree of multicollinearity among the variables. A measured variance inflation factor > 5 was considered as high correlation37. Multicollinearity was presumed when the tolerance value was < 0.138 or the condition index was > 1037. Finally, the following variables were included in the multivariate Cox regression analysis: male sex, age, LVEF, systolic blood pressure, diastolic blood pressure, DBT, atypical chest pain, dyspnea, Q-wave on electrocardiogram, ST-segment depression, T-wave inversion, Killip class II/III, EMS, non-PCI center, hypertension, diabetes mellitus, previous stroke, current smoker, peak CK-MB, peak troponin-I, and blood glucose. Moreover, to correct for confounding variables, a PS-adjusted analysis was performed using a logistic regression model. All the baseline characteristics shown in Table 1 were included in the PS-adjusted analysis. The c-statistic for the PS-matched (PSM) analysis in this study was 0.703. Using the nearest available pair-matching method in a 1:1 fashion, patients in the SDT ≥ 24 h group were matched to those in the SDT < 24 h group. The caliper width was 0.01. Table S3 shows the results of the collinearity test for MACE between the SDT < 24 h and SDT ≥ 24 h groups. Various clinical outcomes were estimated using Kaplan–Meier curve analysis, and group differences were compared using the log-rank test. A p-value of < 0.05 was considered statistically significant. Table S4 in the Supplementary Appendix shows the results of the collinearity test for MACE between the complex and non-complex groups. SPSS software version 20 (IBM, Armonk, NY, USA) was used to perform the statistical analyses.
Data availability
Data is contained with the article or supplementary material.
References
Ibanez, B. et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 39, 119–177 (2018).
Lawton, J. S. et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 79, e21–e129 (2022).
Bouisset, F. et al. Percutaneous myocardial revascularization in late-presenting patients with STEMI. J. Am. Coll. Cardiol. 78, 1291–1305 (2021).
Ndrepepa, G., Kastrati, A., Mehilli, J., Antoniucci, D. & Schömig, A. Mechanical reperfusion and long-term mortality in patients with acute myocardial infarction presenting 12 to 48 hours from onset of symptoms. JAMA 301, 487–488 (2009).
Cho, K. H. et al. Long-term outcomes of patients with late presentation of ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 77, 1859–1870 (2021).
Cannon, C. P. et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 283, 2941–2947 (2000).
Yudi, M. B. et al. Impact of door-to-balloon time on long-term mortality in high- and low-risk patients with ST-elevation myocardial infarction. Int. J. Cardiol. 224, 72–78 (2016).
Meisel, S. R. et al. Direct admission of patients with ST-segment-elevation myocardial infarction to the catheterization laboratory shortens pain-to-balloon and door-to-balloon time intervals but only the pain-to-balloon interval impacts short- and long-term mortality. J Am Heart Assoc. 10, e018343 (2021).
Cha, J. J. et al. Clinical outcomes in patients with delayed hospitalization for non-ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 79, 311–323 (2022).
Brener, S. J. et al. A novel risk score to predict one-year mortality in patients undergoing complex high-risk indicated percutaneous coronary intervention (CHIP-PCI). J. Invasive Cardiol. 33, E253-e258 (2021).
Erol, M. K. et al. Time delays in each step from symptom onset to treatment in acute myocardial infarction: Results from a nation-wide TURKMI registry. Anatol. J. Cardiol. 25, 294–303 (2021).
Griffin, A. C. G. et al. Frequency and outcomes of STEMI patients presenting between 12 and 24 h after symptom onset: Late-presenting STEMI. Catheter. Cardiovasc. Interv. 101, 1–10 (2023).
Kyzer, M. et al. Factors associated with prehospital delay in patients with ST-segment elevation myocardial infarction. Coron. Artery Dis. 33, 329–330 (2022).
McKee, G. et al. Multivariate analysis of predictors of pre-hospital delay in acute coronary syndrome. Int. J. Cardiol. 168, 2706–2713 (2013).
Ting, H. H. et al. Factors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarction. Arch. Intern. Med. 168, 959–968 (2008).
Karwowski, J. et al. Total coronary occlusion of infarct-related arteries in patients with non-ST-elevation myocardial infarction undergoing percutaneous coronary revascularisation. Kardiol. Pol. 75, 108–116 (2017).
Hemetsberger, R. et al. Complex vs. non-complex percutaneous coronary intervention with newer-generation drug-eluting stents: An analysis from the randomized BIOFLOW trials. Clin. Res. Cardiol. 111, 795–805 (2022).
Riku, S. et al. Very long-term clinical outcomes after percutaneous coronary intervention for complex vs non-complex lesions: 10-year outcomes following sirolimus-eluting stent implantation. Nagoya J. Med. Sci. 84, 352–365 (2022).
Généreux, P. et al. Impact of percutaneous coronary intervention extent, complexity and platelet reactivity on outcomes after drug-eluting stent implantation. Int. J. Cardiol. 268, 61–67 (2018).
Akin, I. et al. Outcome of percutaneous coronary intervention with drug-eluting stents in unprotected left main versus non-left main native coronary artery disease: Results from the prospective multicenter German DES.DE registry. Clin. Res. Cardiol. 102, 679–686 (2013).
Wang, R. et al. Impact of established cardiovascular disease on 10-year death after coronary revascularization for complex coronary artery disease. Clin. Res. Cardiol. 110, 1680–1691 (2021).
Caputo, R. P. et al. Impact of drug eluting stent length on outcomes of percutaneous coronary intervention (from the EVENT registry). Am. J. Cardiol. 110, 350–355 (2012).
Collet, J. P. et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 42, 1289–1367 (2021).
Choi, K. H. et al. Impact of intravascular ultrasound-guided percutaneous coronary intervention on long-term clinical outcomes in patients undergoing complex procedures. JACC Cardiovasc. Interv. 12, 607–620 (2019).
Valgimigli, M. et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 39, 213–260 (2018).
Sanchez, R. M., Siiskonen, T. & Vano, E. Current status of diagnostic reference levels in interventional cardiology. J. Radiol. Prot. https://doi.org/10.1088/1361-6498/aca2b3 (2022).
Maksimczuk, J., Galas, A. & Krzesiński, P. What promotes acute kidney injury in patients with myocardial infarction and multivessel coronary artery disease-contrast media, hydration status or something else?. Nutrients 15, 21 (2022).
Fanaroff, A. C. et al. Outcomes of PCI in relation to procedural characteristics and operator volumes in the United States. J. Am. Coll. Cardiol. 69, 2913–2924 (2017).
Fanaroff, A. C. et al. Relationship between operator volume and long-term outcomes after percutaneous coronary intervention. Circulation 139, 458–472 (2019).
Kim, J. H. et al. Multicenter cohort study of acute myocardial infarction in Korea—Interim analysis of the Korea acute myocardial infarction registry-national institutes of health registry. Circ. J. 80, 1427–1436 (2016).
Grech, E. D. ABC of interventional cardiology: Percutaneous coronary intervention. II: The procedure. BMJ 326, 1137–1140 (2003).
Thygesen, K. et al. Fourth universal definition of myocardial infarction (2018). J. Am. Coll. Cardiol. 72, 2231–2264 (2018).
Fox, K. A. et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: Prospective multinational observational study (GRACE). BMJ 333, 1091 (2006).
Lee, J. M. et al. Multivessel percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction with cardiogenic shock. J. Am. Coll. Cardiol. 71, 844–856 (2018).
Kim, Y. H. et al. Impact of renin-angiotensin system inhibitors on long-term clinical outcomes in patients with acute myocardial infarction treated with successful percutaneous coronary intervention with drug-eluting stents: Comparison between STEMI and NSTEMI. Atherosclerosis 280, 166–173 (2019).
Vatcheva, K. P., Lee, M., McCormick, J. B. & Rahbar, M. H. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiology (Sunnyvale) 6, 227 (2016).
Kim, J. H. Multicollinearity and misleading statistical results. Korean J. Anesthesiol. 72, 558–569 (2019).
Kalantari, S. et al. Predictors of early adulthood hypertension during adolescence: A population-based cohort study. BMC Public Health 17, 915 (2017).
Acknowledgements
Investigators of KAMIR‐NIH (Korea Acute Myocardial Infarction Registry‐National Institutes of Health). Myung Ho Jeong, Chonnam National University Hospital, Gwangju, Korea, Young Jo Kim, Yeungnam University Medical Center, Daegu, Korea, Chong Jin Kim, Kyunghee University Hospital at Gangdong, Seoul, Korea, Myeong Chan Cho, Chungbuk National University Hospital, Cheongju, Korea, Hyo‐Soo Kim, Seoul National University Hospital, Seoul, Korea, Hyeon‐Cheol Gwon, Samsung Medical Center, Seoul, Korea, Ki Bae Seung, Seoul St. Mary’s Hospital, Seoul, Korea, Dong Joo Oh, Korea University Guro Hospital, Seoul, Korea, Shung Chull Chae, Kyungpook National University Hospital, Daegu, Korea, Kwang Soo Cha, Pusan National University Hospital, Busan, Korea, Junghan Yoon, Wonju Severance Christian Hospital, Wonju, Korea, Jei‐Keon Chae, Chonbuk National University Hospital, Jeonju, Korea, Seung Jae Joo, Jeju National University Hospital, Jeju, Korea, Dong‐Ju Choi, Seoul National University Bundang Hospital, Bundang, Korea, Seung‐Ho Hur, Keimyung University Dongsan Medical Center, Daegu, Korea, In Whan Seong, Chungnam National University Hospital, Daejeon, Korea, Doo II Kim, Inje University Haeundae Paik Hospital, Busan, Korea, Seok Kyu Oh, Wonkwang University Hospital, Iksan, Korea, Tae Hoon Ahn, Gachon University Gil Medical Center, Incheon, Korea, Jin‐Yong Hwang, Gyeongsang National University Hospital, Jinju, Korea.
Funding
This research was supported by a fund (2016-ER6304-02) by Research of Korea Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
Y.H.K. and A.-Y.H. researched data and wrote the manuscript. Y.H.K., A.-Y.H., S.-W.R., C.U.C., B.G.C., J.B.K., J.Y.P., W.G.C., and S.-H.P. contributed to study design. S.-W.R., C.U.C., B.G.C., J.B.K., S.P., D.O.K., and M.H.J. contributed to the role of data collection. Y.H.K., A.-Y.H., S.-W.R., C.U.C., B.G.C., J.B.K., J.Y.P., W.G.C., S.-H.P., and M.H.J. contributed to intellectual inputs for the discussion. Y.H.K., A.-Y.H., B.G.C., S.P., D.O.K., J.Y.P., W.G.C., and S.-H.P. contributed to data analysis and edited the manuscript. Y.H.K., S.-W.R., and M.H.J contributed to providing supervisor roles during the process of manuscript submission and editing. All authors have read and approved the manuscript, and all authors take full responsibility for this work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, Y.H., Her, AY., Rha, SW. et al. Effect of delayed hospitalization on patients with non-ST-segment elevation myocardial infarction and complex lesions undergoing successful new-generation drug-eluting stents implantation. Sci Rep 13, 16067 (2023). https://doi.org/10.1038/s41598-023-43385-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43385-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.