Abstract
The aim of the study was to assess the influence of different regimes of patient’s preparation before trabeculectomy on the markers of healing process in Tenon’s fibroblast cultures.The studied group consisted of 66 patients with open angle glaucoma undergoing primary trabeculectomy. The patients were divided into 5 groups with different regimes of preparation before the surgery based on application or withdrawal of topical antiglaucoma medications and steroids (G1—patients using antiglaucoma drops until the day of the surgery; G2—patients using antiglaucoma drops until the day of the surgery and additionally dexamethasone for 4 weeks before surgery; G3—patients who stopped using antiglaucoma drops 4 weeks before the surgery and introduced dexamethasone for 4 weeks before surgery; G4—patients who stopped using antiglaucoma drops 4 weeks before the surgery; G5—control group, patients with newly diagnosed glaucoma in whom trabeculectomy was the first treatment option without medical treatment). During trabeculectomy the samples of Tenon’s capsule were obtained. Tenon fibroblasts were isolated directly from the explants to test their proliferation ability and the level of released healing markers. Following factors typical of healing process were evaluated using commercially available ELISA kits: IL 1-β, IL-6, IL-8, VEGF-A, TGF-β1 and MMP-9. Concentrations of IL-1β, IL-6 and TGF-β1 were significantly higher in the group obtaining antiglaucoma drops. Additionally, in this group the fibroblasts revealed the highest proliferation potential, indicating the active healing process. The levels of IL-8, VEGF-A and MMP-9 were similar between the groups. Our study shows that for the best conjunctival anti-inflammatory control, the most influential factor is the withdrawal of antiglaucoma medications.
Similar content being viewed by others
Introduction
Glaucoma is a group of multifactorial eye diseases that result in progressive irreversible damage of the optic nerve and cause vision loss and is considered the second leading cause of blindness in the world. The main element in the pathophysiology of glaucoma is the loss of retinal ganglion cells and their axons, which leads to changes in the morphology of the optic disc and consequently to visual field defects. The main risk factor for glaucoma development and progression is elevated intraocular pressure (IOP). All effective strategies in the treatment of glaucoma are based on the IOP decrease which could be obtained by medical or surgical management.
Trabeculectomy is a surgical procedure in glaucoma which evolved since its introduction in 19681,2,3 and became the golden standard surgical option for glaucoma, as evidence from clinical trials such as the Collaborative Initial Glaucoma Treatment Study and the Advanced Glaucoma Intervention Study showed that trabeculectomy could sufficiently minimise progression of glaucomatous neuropathy. During the surgery the fistula between anterior chamber and subconjunctival space is created to promote a new pathway for aqueous humour outflow3. The meticulous postoperative period is fundamental to its success and can be more challenging than the procedure itself since it is associated with many complications. The most frequent cause of late failure of trabeculectomy is malfunction of the filtering bleb associated with IOP increase and caused by excessive subconjunctival scarring4.
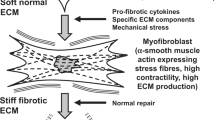
The surgical injury caused by trabeculectomy induces a cascade of pathophysiological reactions causing tissue fibrosis in the bleb region and therefore minimising the aqueous humour outflow. The exposure of fibroblasts to proinflammatory factors promotes phenotypic changes leading to increases in proliferation and migration, and tissue remodelling. Inflammation occurs in an early phase of wound healing and is attributable to immune cell activation of neutrophils and macrophages which infiltrate into a wound and produce proinflammatory cytokines and chemokine. Various proinflammatory cytokines released by infiltrating inflammatory cells induce mesenchymal cell and fibroblast activation, migration and finally transformation into myofibroblasts. Myofibroblasts, transformed and activated by proinflammatory cytokines, produce contractile proteins which cause extracellular matrix (ECM) reorganisation and loss of tissue functionality5.
The controlling of the healing processes after trabeculectomy is the key factor to keep persistence of outflow and bleb function. This goal is realised at the different stages of the surgery. First, preoperatively, the minimising of the conjunctival inflammation connected with the prolonged medical treatment is introduced. During the surgery antiproliferative agents (5-fluorouracil or mitomycin C) are applied in different concentrations and time, aimed at controlling postoperative healing. Although they are potent healing inhibitors, their usage is limited by the risk of complications, some severe leading to blindness, such as persistent leakage of the filtering bleb, clinical hypotony and bleb-related endophthalmitis. After the surgery prolonged topical steroid application and intensive care of the bleb with massage and removal of releasable sutures4,6.
There is no clear scheme of preparation of the patients before trabeculectomy. Usually, in the preoperative period, according to the clinical presentation of patients, medical therapy is remodulated with the attempt to simplify the therapy regimen.
However, there is only scant of evidence for such regimen. An “inflammatory activated conjunctiva” may reduce the likelihood of trabeculectomy success as the prolonged application of antiglaucoma medical treatment causes and promotes conjunctival fibrosis7,8,9. Local steroid application before trabeculectomy would diminish the fibroblastic activity with inhibition of wound healing. There is some evidence to show that a 1-month course of fluorometholone10 will improve the state of the conjunctiva preoperatively. It is generally assumed that such preoperative preparation should improve the likelihood of trabeculectomy success, though the evidence base regarding time and manner of preoperative medical treatment before trabeculectomy is still weak.
The aim of the study was to assess the influence of different regimes of patient’s preparation before trabeculectomy on the markers of the healing process.
Materials and methods
Studied groups
The studied group consisted of 66 patients undergoing trabeculectomy at the Department of Diagnostics and Microsurgery of Glaucoma, Medical University of Lublin, Poland between 2018 and 2020. All participants wrote informed consent before enrolment. The study adhered to the tenets of the Declaration of Helsinki, and the study design was approved by the Bioethics Committee of the Medical University of Lublin (0254/138/2016).
At the inclusion the following parameters were assessed: BCVA, using Snellen charts with decimal scale; slit lamp biomicroscopy with the evaluation of the anterior segment of the eye; gonioscopy, using Zeiss four-mirror gonioscope; as well as the stereoscopic fundus examination of the eye with a detailed assessment of the optic disc morphology. IOP was measured by Goldman applanation tonometry. Additionally visual field evaluation was performed with Humphrey Field Analyzer 745i (Carl Zeiss). The detailed general and ophthalmic histories were obtained. Only the patients fulfilling all inclusion criteria but none of exclusion criteria were included.
Inclusion criteria were as follows:
-
1.
Primary open angle glaucoma or pseudoexfoliative glaucoma
The open angle glaucoma was defined according to the presence of glaucomatous neuroretinal rim loss, glaucomatous VF damage in at least three valuable perimetric tests and an open angle in gonioscopy. The diagnosis of pseudoexfoliation syndrome was based on the presence of dandruff-like exfoliative material on the anterior lens capsule in the central disc and peripheral band (double concentric ring) pattern and/or in the anterior segment of the eye. The criteria of glaucoma diagnosis in PEX syndrome were the same as mentioned above.
-
2.
Application of the same scheme of antiglaucoma drops (latanoprost + dorzolamide + timolol) for at least 6 months before enrolment. The same scheme antiglaucoma therapy was applied to avoid bias in conjunctival status caused by drops with different mechanisms of action.
-
3.
Planned trabeculectomy. Trabeculectomy was performed in all patients if the target pressure was not obtained by maximal medical therapy. Group 5 include untreated patients with newly diagnosed advanced glaucoma with high IOP in whom according to the results of the AGIS11, primary trabeculectomy would better stabilise the disease.
Exclusion criteria were as follows: angle closure glaucoma, neovascular glaucoma, uveitic glaucoma, silicone oil glaucoma, previous antiglaucoma surgery or any surgery involving conjunctiva or sclera, previous argon laser trabeculoplasty, coexisting connective tissue diseases, haematologic or immunologic disorders, diabetes mellitus, general or local immunomodulating treatment.
Patients included to the study were randomly assigned to one of the groups and asked to use the specified preparation scheme before the planned trabeculectomy. The exception was group 5 which involved patients previously untreated. Patients were asked to apply different scheme of preparation 4 weeks before planned trabeculectomy:
-
Group 1—patients using antiglaucoma drops until the day of the surgery.
-
Group 2—patients using antiglaucoma drops until the day of the surgery and additionally dexamethasone (Dexamethasone phosphate 1 mg/1 ml, without preservatives) 4 times a day for 4 weeks before surgery.
-
Group 3—patients who stopped using antiglaucoma drops 4 weeks before the surgery and introduced dexamethasone (Dexamethasone phosphate 1 mg/1 ml, without preservatives) 4 times a day for 4 weeks before surgery. Patients obtained oral acetazolamide 2 × 250 mg to control IOP.
-
Group 4—patients who stopped using antiglaucoma drops 4 weeks before the surgery. Patients obtained oral acetazolamide 2 × 250 mg to control IOP.
-
Group 5—control group, patients with newly diagnosed glaucoma in whom trabeculectomy was the first treatment option without medical treatment.
Initially, 66 patients with POAG or PEXG were enrolled to the study and after preparation according to the scheme have performed trabeculectomy. During the surgery the samples of the Tenon's layer were obtained as described later. In 13 patients (19.69%) enough of the cells during tissue culture was not obtained, 5 patients (7.58%) were excluded because of the new circumstances fulfilling exclusion criteria. In 11 cases (16.67%) cultured cells died during defrosting. Final analysis was performed in 37 patients (56.06%).
Demographic characteristics of studied groups are put in Table 1.
Material
On the day of the surgery the patient obtained 1 drop of 2% of Pilocarpine and Fluorochinolone (Levomer, AdamedPharma). Peribulbar anaesthesia was performed with injection of 5 ml of standard prepared anaesthetic mixture of lignocaine, bupivacaine, adrenaline and hyaluronidase. Before the surgery the drop of 5% povidone-iodine solution was installed. At the beginning of the surgery, transcorneal fixating suture was placed to visualise the upper quadrant of the bulb. The small conjunctival incision was performed near the limbus and conjunctiva and Tenon’s layer were bluntly dissected posteriorly. At this stage, the Tenon’s layer was visualised, and the small fragment (approx.1 × 2 mm) was cut with care not to take conjunctiva. The obtained material was placed in a 1.5 ml sterile Eppendorf tube fulfilled with the solution of 0.5 ml phosphate buffered saline (PBS, Sigma-Aldrich Chemicals) with 300 U/ml penicillin, 300 μg/ml streptomycin and 0,75 μg/ml amphotericin B (Sigma-Aldrich Chemicals). The surgery was further performed typically as limbus-based procedure with mitomycin C application and removable sutures. The obtained material was immediately delivered to the clean room for isolation of the cells.
Methods
Isolation and culture of Tenon fibroblasts
Isolation and culture of Tenon fibroblasts was performed according to the previously developed and described procedure1. Briefly, at the beginning explant of Tenon capsule was twice washed with PBS solution and divided with the sterile blade into 2 or more pieces. The explant samples were then transferred to the wells of 12-multiwell plate and cultured in EMEM medium supplemented with: 5% fetal bovine serum (FBS, EU Professional grade, Pan-Biotech), 5 μg/ml recombinant human (rh) insulin, 5 ng/ml rh basic fibroblast growth factor (rh FGF b), 50 μg/ml ascorbic acid (components of Fibroblast Growth Kit, ATCC—LGC Standards), 7 mM L-glutamine (Sigma-Aldrich Chemicals), 100 U/ml penicilin, 100 μg/ml streptomycin, and 0.25 μg/ml amphotericin B. The culture conditions were as follows: 37 °C in a humidified atmosphere of 5% CO2 and 95% air. Half of the culture medium was changed every 3 days to enhance the cell growth. After formation of monolayer, the fibroblasts were detached by trypsinization and transferred to a 25 cm2 T-flask. The successful isolation of Tenon fibroblasts was confirmed by immunofluorescence staining of vimentin filaments as described earlier12. The cells were cryopreservated at third passage and stored in a liquid nitrogen until use. Before the planned tests the cells isolated from tissue explants of all patients were thawed in a water bath at 37 °C, and their viability was checked with trypan blue. Cells isolated from 11 tissue samples (16, 67%) did not retain sufficient viability to use them in the experiments. After thawing, the cells were cultured in a basal EMEM medium with 10% FBS and antibiotics (100 U/ml penicillin 100 μg/ml streptomycin) without other supplements used for isolation. The isolated fibroblasts were subjected to proliferation assay. Moreover, the level of healing markers and pro-inflammatory cytokines was assessed in the cell culture supernatants.
Cell proliferation assay
To evaluate the fibroblasts’ ability to proliferate, the cells after thawing were seeded at low density of 6 × 104 cells/well into 12-multiwell plate. The cells were incubated for 2 days in 10% EMEM. The exact number of cells was calculated on seeding day and after 2-day culture by means of commercially available proliferation test—WST-8 (Cell Counting Kit-8, Sigma-Aldrich Chemicals), which was performed according to the manufacturer's instruction. Doubling Time (time in hours required to double cell population) of the Tenon fibroblasts was calculated using Doubling Time Computing software.
Evaluation of healing markers and pro-inflammatory cytokines
After thawing the part of fibroblasts suspension was seeded at density of 6 × 104 cells/well into 12-multiwell plates and incubated in 10% EMEM in 37 °C for 24 h, then the supernatants were collected. The level of healing markers and pro-inflammatory cytokines was measured in the cell culture supernatants using commercially available ELISA kits. The following factors were evaluated: interleukin-1β (Interleukin-1 beta Human ELISA, BioVendor), interleukin-6 (Interleukin-6 beta Human ELISA, BioVendor), interleukin-8 (Interleukin-8 Human ELISA, BioVendor), Human vascular endothelial growth factor-A (Human VEGF-A ELISA Kit, Diaclone), Human transforming growth factor-β1 (Human TGF-beta1 ELISA Kit, Diaclone), and matrix metalloproteinase-9 (Human MMP-9 ELISA, BioVendor). All tests were performed according to the manufacturer's instructions. In order to obtain reliable data and exclude the effect of different cell density on the level of healing markers and pro-inflammatory cytokines, the ELISA results were normalized per 1 mg of cellular proteins. Total cellular proteins were assessed in cell lysates by Bradford colorimetric method using commercially available kit (Pierce™ BCA Protein Assay Kit, ThermoFisher Scientific). The test was performed according to manufacturer’s instructions. To obtain cell lysates, culture medium was discarded and replaced with PBS containing protease inhibitors (Sigma Aldrich-Chemicals). Cell lysis was performed by 3 freeze–thaw cycles and sonification with ultrasounds.
Statistical analysis
The biochemical markers for each patient were evaluated by ELISA in 2 repetitions. The mean value was calculated and used for further analysis.
The results were statistically analysed with computer programs IBM SPSS Statistics v. 26 and STATISTICA 13 (StatSoft Polska) with ANOVA test for comparisons between the groups and Spearman correlation tests to look for the correlations. The statistically significant results were when p level was lower than 0.05.
Results
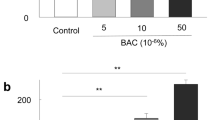
Proliferation potential
Fibroblast doubling time
The most actively dividing fibroblasts were observed in group 1, the statistical difference was observed in comparison to groups 2, 4 and 5 (test U Mann–Whitney. In group 2 fibroblast DT was the longest and the significant comparison was observed to all groups. In group 3 fibroblast DT was statistically shorter compared to groups 2, 4 and 5. The results did not differ between groups 4 and 5. The detailed results are put in Table 2 and Fig. 1.
Markers of inflammation
Interleukin-1 beta
Concentration of IL-1β was significantly higher in group 1 and compared to groups 3, 4, 5. The results did not differ between groups 1 and 2, and groups 3, 4, 5. The detailed results are put in Table 2 and Fig. 2.
Interleukin-6
The Il-6 concentration was statistically higher in group 1 compared to all remaining groups. In group 2 Il-6 concentrations were significantly compared to group 3 and 5. Groups 3, 4, 5 did not statistically differ regarding Il-6 concentration. The detailed results are put in Table 2 and Fig. 3.
Markers of angiogenesis
Interleukin-8
The highest Il-8 concentration was observed in group 1, however, the difference was not significant compared to all groups. The detailed results are put in Table 2 and Fig. 4.
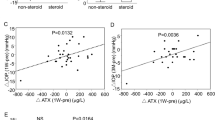
VEGF-A
Mean VEGF-A concentrations were similar between the groups. The detailed results are put in Table 2 and Fig. 5. Positive correlation (rho = 0.5140) was observed between concentrations of Il-8 and VEGF.
Markers of maturation and remodelling
Transforming Growth Factor-beta 1
Concentration of TGF-β1 was significantly higher in group 1 and compared to groups 3, 4, 5. The concentrations did not significantly differ between groups 1 and 2; and between groups 3, 4 and 5. The detailed results are put in Table 2 and Fig. 6.
Matrix metalloproteinase-9
In all studied groups the detectable MMP-9 values were obtained from 8 patients (3 from group 1, 1 from group 2, 2 in group 3, none in group 4 and in group 5-2 patients). The data were not sufficient for the statistical analysis. The results are put in Table 2
Discussion
The final long-term success of trabeculectomy is related to sufficient management of healing processes. The rate of clinical failures is higher in patients chronically treated with antiglaucoma drops13, because of induced prolonged conjunctival inflammation as the response for toxic and allergic actions of both active substances and preservatives14,15,16. In patients before trabeculectomy to diminish chronic inflammation of the ocular surface preoperatively, most of the surgeons withdraw antiglaucoma drops and introduce local steroid application. However, the detailed scheme of preparation schedule is rather intuitive, there are no clear indications. In this study we aimed to check the influence of steroids and antiglaucoma medications on inflammatory parameters which may be related to the subsequent wound healing. Two main factors were changed in our preoperative schemes: antiglaucoma drops which were long term used as maximal medical therapy and withdrawn in some groups 4 weeks before planned surgery, and local dexamethasone application introduced in some groups of patients. The time of the preoperative therapy was related to the fact that for most antiglaucoma drops wash-out time lasts a month17. This time seems to be sufficient, the studied parameters were statistically similar between the group with stopped drops and the untreated control group. To facilitate the patients fulfilling the preoperative schedule, the steroids were introduced in a similar manner. The previous studies showed that steroid installation for 3–4 weeks before trabeculectomy decreases the failure rate in long term observation8,18. However, prolonged steroid treatment in some glaucoma patients may cause IOP increase. In this study, we used dexamethasone as a potent steroid which is used in our typical practice in trabeculectomy patients and which at the time of study design was the only preservative-free steroid medicament in drops commercially available in Poland. Although, some previous research15,16 used fluorometholone as the one with the smaller potential to cause IOP spikes.
IL1-β is produced by macrophages, fibroblasts, and vascular endothelial cells at the early stage of injury19 which enhances the inflammatory reaction. Increased IL-1β level was observed in tear film, conjunctiva, and aqueous humour of glaucoma patients but also in patients with dry eye syndrome and Meibomian gland dysfunction, frequent in patients on antiglaucoma medical treatment20,21. In our study, increased IL-1β level in Tenon’s fibroblasts culture was observed in patients constantly installing antiglaucoma drops. The withdrawal of antiglaucoma drops was the most important factor in decreasing IL-1β level; a 1-month antiglaucoma medication free declined the IL-1β level to the level observed in the naive patients. The introduction of corticosteroids was not a significant factor.
IL-1β-activated lymphocytes, macrophages, fibroblasts and vascular endothelial cells produce IL-6, whose concentration increases 12-16 h after the injury and further promotes inflammatory reactions22. Enhanced IL-6 expression was shown in conjunctiva of patients constantly using timolol23,24 and latanoprost25, which seemed preservatives independent23. Our results confirm these results, IL-6 level was the highest in the group of patients permanently applying antiglaucoma drops, application of steroids significantly augmented IL-6 level decrease. This drug combination likens IL-6 level to the one observed in untreated control. Dexamethasone directly reduces IL-6 expression but also inhibits its IL-1β induced production26,27.
In the wound healing after trabeculectomy, the early inflammatory phase initiates proliferation resulting in formation of loose granulation tissue consisting of fibroblasts, newly formed vessels, macrophage, and collagen fibres. Tenon’s capsule fibroblasts are the main cells involved in the tissue repair after surgery, their ability to migrate and proliferate reflects the healing potential. Sherwani et al.28 showed that prolonged medical antiglaucoma treatment increases the number of fibroblasts. In this study evaluating proliferative potential of fibroblasts, the fibroblasts obtained from the patients constantly using antiglaucoma drops were significantly more active. The most beneficial effect was observed in case of combined antiglaucoma and steroid therapy. It may reflect cumulative proapoptotic effects of preservatives from antiglaucoma drops and steroids, prevailing the beneficial effect of hypotensive medication withdrawal. The studies showed that for different antiglaucoma medications, the same apoptotic index was observed in case of the same number of BAK, no matter the active antiglaucoma compound29,30. Surprisingly, in a group of patients washed-out from glaucoma medications and using steroids, the proliferative potential of fibroblasts was similar to the group obtaining constant antiglaucoma drops, which was significantly higher to all remaining groups. The expected results in the steroid group would be a significant decrease in fibroblast proliferation due to diminishing influence on the proinflammatory cytokine production and cell cycle. However, the increased proliferative activation after dexamethasone treatment was observed also for other tissues31,32, the mechanisms remain elusive.
The other process crucial during the proliferative stage of healing is angiogenesis concurrent to dynamic fibroblast ingrowth. From the 4th day of injury, the most important proangiogenic factor in the granulation tissue is VEGF produced by fibroblasts and macrophages. It increases vascular permeability and has a promitotic influence on vascular endothelial cells. Patients applying antiglaucoma drops for prolonged periods of time show conjunctival redness resulting from chronic inflammation. However, there is only a scant amount of the research evaluating impact on antiglaucoma medications on VEGF status, the different classes of the drugs seem to have different influences33, similarly to the relation between dexamethasone and VEGF34,35,36. Our study also reflects these tendencies: the Tenon’s fibroblasts cultures showed high fluctuations not correlated to any applied schemes in preparation for trabeculectomy. On the other hand, it is probable that the main factor triggering angiogenesis is the surgical wound and no antiglaucoma drops nor steroid application in preoperative period influence proangiogenic factors.
IL-8 also promotes angiogenesis stimulating mitosis and vascular endothelial cells migration creating scaffolding for newly formed vessels37. High IL-8 level was described in patients with dry eye syndrome, allergic conjunctivitis and Moeibomian gland dysfunction. In glaucoma patients increased IL-8 concentrations were shown in aqueous humour, tears and conjunctiva19,38. Additionally, antiglaucoma medical therapy increases IL-8 expression14,23. In this study, IL-8 level was not significantly higher in patients using persistent antiglaucoma medications, which was slightly suppressed by dexamethasone addition. The suppressing action of dexamethasone on IL-8 synthesis was previously described39,40 on fibroblasts obtained from inflammatory orbit.
One of the crucial factors in every stage of wound healing is TGF-β1released in the early phase, which has a chemotactic influence on inflammatory cells, enhances fibroblast proliferation and boosts VEGF production. It is also engaged in late healing stages initiating remodelling and maturation of the scar by MMP synthesis and collagen production37. Its expression in the eye is enhanced in case of ocular surface inflammation observed in dry eye syndrome and Moeibomian gland dysfunction, frequently coexisting with prolonged medical treatment of glaucoma. Moreover, TGF-β1 induced fibroblast transformation into active myofibroblasts is the mechanism of trabecular meshwork, astrocytes, and lamina cribrosa transformation during glaucoma41. The small studies regarding the influence of antiglaucoma drops on TGF-β1 level showed its increased level after prostaglandin analogue installation especially when combined with preservatives42,43. Our study showed that in a group of patients applying antiglaucoma medications until the time of trabeculectomy TGF-β1 level was the highest, which was only slightly decreased by adding dexamethasone. However, suppressing action of steroids on TGF-β1 was described previously44,45,46,47. Our results regarding TGF-β1 strongly encourage antiglaucoma drops withdrawal before penetrating surgery.
Maturation stage during the wound healing is connected to active myofibroblast shrinkage and collagen production, which are mediated by TGF-β1, and extracellular matrix remodelling moderated by MMPs. MMP-9 cleavages collagen type III increases myofibroblast shrinkage48. Elevated MMP-9 level was shown in excessive scarring37. There are limited studies concerning the influence of antiglaucoma treatment on MMP-9 level, latanoprost was described to increase its concentration42,43,49. In this study, MMP-9 was rarely detected no matter the applied preparation regime.
To sum up, prolonged application of antiglaucoma drops before trabeculectomy in preoperative period results in high concentrations of the factors promoting healings in Tenon’s capsule, which may be related to late bleb failure and lack of postoperative success. The introduction of dexamethasone enabled for their decrease and in the studied groups the clinical success in 30% IOP decrease was highest in group 3 and the lowest in group 1. However, our patients using preoperative steroids tended to have more frequently early wound leakage and hypotony (unpublished data), which is concordant with other clinical studies showing that introduction of the steroids did not improve the results of trabeculectomy but increased the risk of complications50,51. On the other hand, our results did not focus on the influence of intraoperative applications of antimetabolites and postsurgical topical steroids as the branches for healing control.
Our study shows that for the best conjunctival anti-inflammatory control, the most influential factor is to withdraw the topical antiglaucoma medications, with IOP control with oral acetazolamide if needed.
Data availability
All the data are available on request from the corresponding author.
References
Cairns, J. E. Trabeculectomy. Preliminary report of a new method. Am. J. Ophthalmol. 66, 673–679 (1968).
Watson, P. G. Trabeculectomy. Dev. Ophthalmol. 1, 61–70 (1981).
Khaw, P. T. et al. Enhanced trabeculectomy: The moorfields safer surgery system. Dev. Ophthalmol. 59, 15–35 (2017).
de Oliveira, C. M. & Ferreira, J. L. M. Overview of cicatricial modulators in glaucoma fistulizing surgery. Int. Ophthalmol. 40, 2789–2796 (2020).
Yamanaka, O., Kitano-Izutani, A., Tomoyose, K. & Reinach, P. S. Pathobiology of wound healing after glaucoma filtration surgery. BMC Ophthalmol. 15, 157 (2015).
Koike, K. J. & Chang, P. T. Trabeculectomy: A brief history and review of current trends. Int. Ophthalmol. Clin. 58, 117–133 (2018).
Eke, T. Preoperative preparation and anesthesia for trabeculectomy. J. Curr. Glaucoma Pract. 10, 21–35 (2016).
Broadway, D. C., Grierson, I., Stürmer, J. & Hitchings, R. A. Reversal of topical antiglaucoma medication effects on the conjunctiva. Arch. Ophthalmol. 114, 262–267 (1996).
Agnifili, L. et al. Preparing the ocular surface for glaucoma filtration surgery: An unmet clinical need. Acta Ophthalmol. 100, 740–751 (2022).
Baudouin, C. et al. Efficacy of indomethacin 01% and fluorometholone 01% on conjunctival inflammation following chronic application of antiglaucomatous drugs. Graefes Arch. Clin. Exp. Ophthalmol. 240, 929–935 (2002).
Agis Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS Investigators. Am. J. Ophthalmol. 130(4), 429–440 (2000).
Przekora, A., Zarnowski, T. & Ginalska, G. A simple and effective protocol for fast isolation of human Tenon’s fibroblasts from a single trabeculectomy biopsy—a comparison of cell behaviour in different culture media. Cell. Mol. Biol. Lett. 22, 5 (2017).
Lavin, M. J., Wormald, R. P., Migdal, C. S. & Hitchings, R. A. The influence of prior therapy on the success of trabeculectomy. Arch. Ophthalmol. Chic. Ill 1960(108), 1543–1548 (1990).
Mastropasqua, L., Agnifili, L., Mastropasqua, R. & Fasanella, V. Conjunctival modifications induced by medical and surgical therapies in patients with glaucoma. Curr. Opin. Pharmacol. 13, 56–64 (2013).
Sherwood, M. B., Grierson, I., Millar, L. & Hitchings, R. A. Long-term morphologic effects of antiglaucoma drugs on the conjunctiva and Tenon’s capsule in glaucomatous patients. Ophthalmology 96, 327–335 (1989).
Mastropasqua, L. et al. Topical steroids and glaucoma filtration surgery outcomes: An in vivo confocal study of the conjunctiva. J Clin Med. 11(14), 3959 (2022).
Diaconita, V. et al. Washout duration of prostaglandin analogues: A systematic review and meta-analysis. J. Ophthalmol. 2018, 3190684 (2018).
Breusegem, C. et al. Preoperative nonsteroidal anti-inflammatory drug or steroid and outcomes after trabeculectomy: A randomized controlled trial. Ophthalmology 117, 1324–1330 (2010).
Shida, Y., Kondo, T., Kimura, A., Matsushima, K. & Mukaida, N. Absence of IL-1 receptor antagonist impaired wound healing along with aberrant NF-κB activation and a reciprocal suppression of TGF-β signal pathway. J. Immunol. 176, 5598–5606 (2006).
Mikalauskiene, L., Grzybowski, A. & Zemaitiene, R. Ocular surface changes associated with ophthalmic surgery. J. Clin. Med. 10(8), 1642 (2021).
Csősz, É. et al. Comparative analysis of cytokine profiles of glaucomatous tears and aqueous humour reveals potential biomarkers for trabeculectomy complications. FEBS Open Bio 9, 1020–1028 (2019).
Gallucci, R. M. et al. Impaired cutaneous wound healing in interleukin–6-deficient and immunosuppressed mice. Faseb J. 14(15), 2525–2531. https://doi.org/10.1096/fj.00-0073com (2000).
Baudouin, C. et al. Conjunctival epithelial cell expression of interleukins and inflammatory markers in glaucoma patients treated over the long term. Ophthalmology 111, 2186–2192 (2004).
Er, H. et al. Effects of L-NAME and timolol on aqueous IL-1beta, IL-6, IL-8, TNF-alpha and NO levels after Nd:YAG laser iridotomy in rabbits. Eur. J. Ophthalmol. 12, 281–286 (2002).
Tong, L., Matsuura, E., Takahashi, M., Nagano, T. & Kawazu, K. Effects of anti-glaucoma prostaglandin ophthalmic solutions on cultured human corneal epithelial cells. Curr. Eye Res. 44, 856–862 (2019).
Amano, Y., Lee, S. W. & Allison, A. C. Inhibition by glucocorticoids of the formation of interleukin-1 alpha, interleukin-1 beta, and interleukin-6: Mediation by decreased mRNA stability. Mol. Pharmacol. 43, 176–182 (1993).
Lee, H., Kim, M., Park, Y. H. & Park, J. B. Dexamethasone downregulates SIRT1 and IL6 and upregulates EDN1 genes in stem cells derived from gingivae via the AGE/RAGE pathway. Biotechnol. Lett. 40, 509–519 (2018).
Sherwani, R. K. et al. Conjunctival cytology in glaucomatous patients using long-term topical therapy. J. Cytol. 25, 50 (2008).
Doğan, A. S., Orhan, M., Söylemezoğlu, F., Irkeç, M. & Bozkurt, B. Effects of topical antiglaucoma drugs on apoptosis rates of conjunctival epithelial cells in glaucoma patients. Clin. Exp. Ophthalmol. 32, 62–66 (2004).
Hamard, P. et al. In vitro effects of preserved and unpreserved antiglaucoma drugs on apoptotic marker expression by human trabecular cells. Graefes Arch. Clin. Exp. Ophthalmol. 241, 1037–1043 (2003).
Duman, E. et al. The effects of steroidal and non-steroidal anti-inflammatory drugs on tracheal wound healing in an experimental rat model. Interact. Cardiovasc. Thorac. Surg. 30, 646–651 (2020).
Fouty, B., Moss, T., Solodushko, V. & Kraft, M. Dexamethasone can stimulate G1-S phase transition in human airway fibroblasts in asthma. Eur. Respir. J. 27, 1160–1167 (2006).
Cheng, T., Cao, W., Wen, R., Steinberg, R. H. & LaVail, M. M. Prostaglandin E2 induces vascular endothelial growth factor and basic fibroblast growth factor mRNA expression in cultured rat Müller cells. Invest. Ophthalmol. Vis. Sci. 39, 581–591 (1998).
Hegeman, M. A. et al. Dexamethasone Attenuates VEGF Expression and Inflammation but Not Barrier Dysfunction in a Murine Model of Ventilator-Induced Lung Injury. PLoS ONE 8, e57374 (2013).
Patil, S. D., Papadmitrakopoulos, F. & Burgess, D. J. Concurrent delivery of dexamethasone and VEGF for localized inflammation control and angiogenesis. J. Control. Release Off. J. Control. Release Soc. 117, 68–79 (2007).
Shim, S.-H., Hah, J. H., Hwang, S.-Y., Heo, D. S. & Sung, M.-W. Dexamethasone treatment inhibits VEGF production via suppression of STAT3 in a head and neck cancer cell line. Oncol. Rep. 23, 1139–1143 (2010).
Townsend, C. M. T. Jr., Beauchamp, R. D., Evers, B. M. & Mattox, K. L. Sabiston Textbook of Surgery: Expert Consult Premium Edition: Enhanced Online Features (Elsevier Health Sciences, London, 2007).
Tamhane, M., Cabrera-Ghayouri, S., Abelian, G. & Viswanath, V. Review of biomarkers in ocular matrices: Challenges and opportunities. Pharm. Res. 36, 40 (2019).
Baiula, M. et al. Eosinophil as a cellular target of the ocular anti-allergic action of mapracorat, a novel selective glucocorticoid receptor agonist. Mol. Vis. 17, 3208–3223 (2011).
Burnstine, M. A., Elner, S. G. & Elner, V. M. Orbital fibroblast chemokine modulation: Effects of dexamethasone and cyclosporin A. Br. J. Ophthalmol. 82, 318–322 (1998).
Shu, D. Y. & Lovicu, F. J. Myofibroblast transdifferentiation: The dark force in ocular wound healing and fibrosis. Prog. Retin. Eye Res. 60, 44–65 (2017).
Leng, F., Liu, P., Li, H. & Zhang, J. Long-term topical antiglaucoma medications cause enhanced Tenon’s capsule fibroblast proliferation and abnormal TGF-β and MMP expressions: Potential effects on glaucoma filtering surgery. Curr. Eye Res. 36, 301–309 (2011).
Jung, K. I., Woo, J. E. & Park, C. K. Effects of aqueous suppressants and prostaglandin analogues on early wound healing after glaucoma implant surgery. Sci. Rep. 9, 5251 (2019).
Potchinsky, M., Nugent, P., Lafferty, C. & Greene, R. M. Effects of dexamethasone on the expression of transforming growth factor-beta in mouse embryonic palatal mesenchymal cells. J. Cell. Physiol. 166, 380–386 (1996).
Meisler, N. et al. Dexamethasone abrogates the fibrogenic effect of transforming growth factor-beta in rat granuloma and granulation tissue fibroblasts. J. Invest. Dermatol. 108, 285–289 (1997).
Li, Y. et al. Transforming growth factor beta is regulated by a glucocorticoid-dependent mechanism in denervation mouse bone. Sci. Rep. 7, 9925 (2017).
Roy, S. K., Wang, J. & Yang, P. Dexamethasone inhibits transforming growth factor-β receptor (TβR) messenger RNA expression in hamster preantral follicles: Possible association with NF-YA1. Biol. Reprod. 68, 2180–2188 (2003).
Mahale, A. et al. Histopathologic and immunohistochemical features of capsular tissue around failed Ahmed glaucoma valves. PLoS ONE 12, e0187506 (2017).
Yang, Y. et al. 0.005% preservative-free latanoprost induces dry eye-like ocular surface damage via promotion of inflammation in mice. Invest. Ophthalmol. Vis. Sci. 59, 3375–3384 (2018).
Lorenz, K. et al. Efficacy and safety of preoperative IOP reduction using a preservative-free fixed combination of dorzolamide/timolol eye drops versus oral acetazolamide and dexamethasone eye drops and assessment of the clinical outcome of trabeculectomy in glaucoma. PLoS ONE 12, e0171636 (2017).
Senthil, S. et al. Long-term outcomes and risk factors for failure of glaucoma filtering surgery in eyes with vernal keratoconjunctivitis and steroid-induced glaucoma. Indian J. Ophthalmol. 70, 820–825 (2022).
Funding
Grant from Medical University of Lublin, Poland.
Author information
Authors and Affiliations
Contributions
E.K.J. and T.Z. conceived of the presented idea. J.P., D.W.D., E.K.J. and T.Z. applied appropriate preparation before the trabeculectomy surgery and collected tissue explants. A.P. and PK verified the analytical methods, performed cell isolation and cell culture tests. All authors carried out the experiment. E.K.J. wrote the manuscript with support from A.P. J.P. and D.W.D. T.Z. supervised the project. All authors provided critical feedback and helped shape the research, analysis, and manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Piłat, J., Przekora, A., Wróbel-Dudzińska, D. et al. Analysis of the impact of different schemes of preparation to trabeculectomy on the healing markers on the Tenon fibroblasts cultures. Sci Rep 13, 16353 (2023). https://doi.org/10.1038/s41598-023-43246-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43246-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.