Abstract
Resting full-cycle ratio (RFR), an alternative to fractional flow reserve (FFR) for evaluating intermediate coronary artery stenosis, helps reduce patients’ time, cost, and discomfort. However, the validation data for RFR and FFR are lacking. We aimed to assess the diagnostic accuracy of RFR and FFR and evaluate effective decision-making for revascularization using their values. Patients subjected to an invasive physiological study for intermediate coronary artery stenosis in Yongin Severance hospital between October 2020 and April 2022 were prospectively and consecutively recruited. We evaluated the correlation between RFR and FFR measurements and the diagnostic performance of RFR (≤ 0.89) versus FFR (≤ 0.80). In all, 474 intermediate coronary stenosis lesions from 400 patients were evaluated using RFR and FFR values. There was a strong linear relationship between RFR and FFR (r = 0.75, 95% CI 0.70–0.78, p < 0.01). Comparing diagnostic performance between RFR and FFR, RFR demonstrated diagnostic accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of 85.0%, 80.0%, 86.7%, 67.1%, and 92.7%, respectively. We analyzed the RFR value in the hyperemia zone (0.86–0.93) according to positive (RFR: 0.86–0.89) and negative (RFR: 0.90–0.93) areas. PPV in positive area is 47.8% (95% Confidence Interval [CI]: 33.8% to 62.0%) and NPV in negative area is 87.7% (95% CI: 80.3% to 93.1%). Excellent correlation exists between RFR and FFR and the diagnostic value of RFR without hyperemia compared with FFR in establishing the accurate functional significance of coronary artery stenosis was shown. RFR alone could evaluate the functional significance of coronary artery stenosis without unnecessary hyperemia, except in the positive area.
Trial registration: URL: http://trialsearch.who.int; Unique identifier: KCT0005255.
Similar content being viewed by others
Introduction
Fractional flow reserve (FFR) is a reliable index of the functional severity of coronary artery stenosis, which is determined using coronary pressure measurement during cardiac catheterization. Notably, several studies have shown that invasive coronary physiology assessment could improve clinical outcomes by appropriately selecting patients who may benefit from percutaneous coronary interventions (PCI) with stent implantation1,2,3. Therefore, current guidelines recommend evaluating coronary pressure-derived FFR to evaluate the hemodynamic significance of intermediate coronary lesions in patients with symptomatic angina and undocumented ischemia4,5. However, FFR has several disadvantages, including the need to induce maximal hyperemia, which requires additional time and cost and to minimize the effect of coronary microcirculation by administering pharmacological agents such as intravenous or intracoronary adenosine, which causes discomfort for patients6. Therefore, the hurdle of hyperemia in clinical practice could reduce FFR use. Recent studies have reported that the rate of FFR-guided PCI for intermediate lesions was only 6.1% in the United States, 8.2% in Japan, and 5.1% in South Korea7,8,9.
Instantaneous wave-free ratio (iFR) has been developed to overcome the limitation of FFR requiring maximal hyperemia. With accumulating evidence, iFR, which is similar to FFR, is also recommended for evaluating the hemodynamic significance of intermediate coronary stenosis in the current guidelines10,11,12,13. Notably, several non-hyperemic pressure ratios (NHPR) have been developed, including the entire cardiac cycle, and one of them is the resting full-cycle ratio (RFR). RFR evaluates the hemodynamic significance of coronary stenosis by identifying the lowest distal arterial pressure (Pd)/arterial pressure (Pa) ratio within the entire cardiac cycle. The validation of a novel non-hyperemic index of coronary artery stenosis severity i.e., the RFR (VALIDATE RFR) study reported that RFR is diagnostically equivalent to iFR14. However, data regarding the comparison between RFR and FFR in patients with intermediate coronary artery disease are limited15,16,17. Therefore, the present study aimed to assess the diagnostic value of RFR and FFR in real-world practice.
Methods
Study population
The Invasive physiologic assessment of coronary artery stenosis by RFR and FFR (ICE-FLOWER) study was a prospective, single-center observational study conducted at Yongin Severance Hospital in South Korea. Patients aged > 19 years with suspected ischemic heart disease (IHD) between October 2020 and April 2022 were enrolled in this study if diagnosed with de novo stenosis. We excluded patients with single lesion in acute coronary syndromes, left main coronary artery disease, stenosis in a coronary artery bypass graft, and a life expectancy of < 1 year. For non-culprit lesions in patients with acute coronary syndrome, we performed RFR/FFR immediately if the patient was stable, and staged RFR/FFR measurement was done within 7 days if the patient was unstable. This study protocol was approved by the Institutional Review Board of Yongin Severance Hospital (approval number: 9–2020-0072), and all participants provided written informed consent before participating in the study. The study protocol was registered in the International Clinical Trial Registry Platform (KCT0005255) on July 24th, 2020 (https://trialsearch.who.int/Trial2.aspx?TrialID=KCT0005255) and adhered to the ethical guidelines of the Declaration of Helsinki. The funding sources did not participate in the design or conduct of the study, analysis or interpretation of the data, or the decision to submit the manuscript for publication.
Cardiac catheterization and quantitative coronary angiography
Coronary angiography (CAG) was performed by five interventional cardiologists with extensive experience in CAG and PCI according to current guidelines and standard technique using a femoral, proximal, or distal radial approach4,12. Diameter stenosis percentage, minimal and reference lumen diameter, and lesion length were assessed with quantitative coronary angiography (QCA) using CASS workstation 7.4 (Pie Medical Imaging, Maastricht, Netherlands). All QCA images were retrospectively re-analyzed by two independent observers with > 5 years of experience in cardiac catheterization. All diameters were determined as the average of the diameter values obtained independently. The reference diameter was determined using the proximal and distal reference diameters.
Coronary physiologic measurements and assessment
Physiological assessments of the intermediate coronary lesions (50%–90% diameter stenosis using QCA analysis) were performed as follows. All coronary physiologic measurements were performed using a 0.014″ intracoronary wireless pressure wire (PressureWire™ X Guidewire [Abbott Vascular Inc., Santa Clara, CA, USA]) and automatically calculated using the QUANTIEN™ system (Abbott Vascular Inc.) and OPTIS™ Mobile System (Abbott Vascular Inc.). The pressure wire was equalized to the aortic pressure, and equalization was then performed after placing the pressure wire on the tip of the guiding catheter and removing contrast media using saline flushing. First, the pressure wire was advanced distally to a target vessel to evaluate the RFR value. The instantaneous Pd/Pa was continuously measured throughout five cardiac cycles to calculate RFR, defined as the point where the Pd/Pa ratio was the lowest during the entire cardiac cycle. After the RFR measurement, the pressure wire was pulled back into the tip of the guiding catheter to check the presence of pressure drift. A final Pd/Pa between 0.97 and 1.03 is considered acceptable18,19. After confirming that there was no pressure drift, the pressure wire was re-advanced to the distal portion of the target vessel to evaluate the FFR value. In all lesions, FFR values were measured with hyperemia, achieved using an intracoronary (IC) bolus injection of 2 mg nicorandil (Sigmart®; Chugai Pharmaceutical Co., Ltd., Tokyo, Japan). Based on previous studies regarding IC bolus injection of nicorandil for hyperemia, FFR measurement was obtained during maximal hyperemia, defined as a period between 20 and 50 s after IC bolus injection of nicorandil6,20. The pressure drift was checked after FFR measurement. In patients with multivessel disease, there were sufficient time intervals between measurements of each vessel21.
Definitions
We evaluated the correlation between RFR and FFR measurements and the diagnostic performance of RFR to identify FFR-positive coronary stenosis. Hemodynamically significant stenosis was defined as FFR ≤ 0.80 and RFR ≤ 0.89. Based on the actual RFR cut-off of 0.89, the gray zone with an RFR value between 0.86 and 0.93, called the “hyperemia zone,” is further subdivided into the positive (RFR 0.86–0.89) and negative (RFR 0.90–0.93) areas22. The diagnostic accuracy, positive predictive value (PPV), and negative predictive value (NPV) of RFR in the hyperemia zone were re-evaluated. We also evaluated the relationship between RFR and Pd/Pa.
Statistical analysis
All data were expressed as mean ± standard deviation (SD) or numbers (%) of patients. The 95% confidence intervals (CIs) of the means of continuous variables and percentages of categorical variables were calculated with t-tests and Clopper–Pearson (exact) approaches, respectively. Pearson’s correlation coefficient (r) between RFR and FFR was computed with 95% CIs. The receiver operating characteristic (ROC) curve was used to represent the overall prediction performance of the RFR for FFR ≤ 0.80 and Pd/Pa ≤ 0.92 with the area under the ROC curve (AUC). Youden’s index was used to determine the optimal RFR cut-off against FFR ≤ 0.80 and the prediction of Pd/Pa ≤ 0.92. Prediction performance measures, such as sensitivity, specificity, PPV, NPV, and accuracy were calculated. The cut-off value of RFR calculated using Youden’s index was determined to be 0.89, consistent with the value in previous studies10,14. Statistical significance was set at P < 0.05 (two-sided). All statistical analyses were performed with SPSS statistical software (SPSS version 25.0 for Windows; IBM Corp., Armonk, NY, USA) and R software (version 4.3.0; R Foundation for Statistical Computing, Vienna, Austria).
Results
Study population
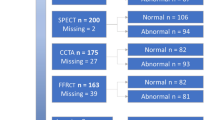
A total of 474 stenoses from 400 patients were investigated and included in this study. A STAndards for the Reporting of Diagnostic Accuracy Studies (STARD)-type flow chart depicts this process as shown in Fig. 1.23 Participants’ baseline clinical and angiographic characteristics are shown in Tables 1 and 2. The overall mean age was 66.2 ± 10.9 years, and 68.6% of patients were male. The common clinical presentation was stable angina (73.9%), followed by unstable angina (16.5%), and the lesions were located most often in the left anterior descending artery (63.5%). The distribution of the RFR and FFR values is shown in Supplementary Fig. S1 online. The study population comprised patients with angiographically intermediate stenosis (diameter stenosis [%]: 59.6 ± 6.1 using QCA). The mean ± SD and median values with interquartile range (IQR) of RFR were 0.91 ± 0.08 and 0.92 (IQR: 0.88–0.96), respectively. Notably, 120 (30.2%) vessels had RFR ≤ 0.89 (see Supplementary Fig. S2).
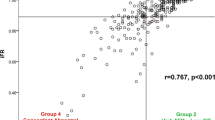
Relationship between RFR and FFR or Pd/Pa
Figure 2A shows the scatterplot of the relationship between RFR and FFR. A strong correlation was noted between both indices (r = 0.75, 95% CI 0.70–0.78, p < 0.01). Figure 2B also shows a strong correlation between RFR and Pd/Pa (r = 0.92, 95% CI 0.90–0.93, p < 0.01).
Concordance and discordance among resting full-cycle ratio (RFR) and fractional flow reserve (FFR) or distal coronary pressure (Pd)/ aortic pressure (Pa). (A) FFR and RFR showed a significant correlation (r = 0.747; p < 0.001), and (B) The correlation between RFR and Pd/Pa was also significant, with a similar correlation coefficient (r = 0.915; p < 0.001). FFR, fractional flow reserve; RFR, resting full-cycle ratio; Pd, distal coronary pressure; Pa, aortic pressure.
Compared with FFR, RFR demonstrated a diagnostic accuracy of 85.0%. RFR ≤ 0.89 demonstrated a sensitivity, specificity, PPV, and NPV of 80.0%, 86.7%, 67.1%, and 92.7%, respectively in predicting significant FFR ≤ 0.80. ROC analyses for the prediction of FFR ≤ 0.80 showed an AUC (C statistic) of 0.90 (95% CI 0.86–0.93, p < 0.01) (Fig. 3A). The optimal cut-off point of RFR was 0.89, with a Youden index of 0.67.
Receiver operating characteristic (ROC) curves. (A) ROC curves for RFR versus FFR ≤ 0.80 showed an area under the ROC curve (AUC) of 0.897 (0.862–0.933) and the following values: diagnostic accuracy, 0.85; sensitivity, 0.80; specificity, 0.87; positive predictive value, 0.67; negative predictive value, 0.93. (B) ROC curves for RFR versus Pd/Pa ≤ 0.92 showed an AUC of 0.960 (0.940–0.980) and the following values: diagnostic accuracy, 0.91; sensitivity, 0.87; specificity, 0.93; positive predictive value, 0.83; negative predictive value, 0.95. ROC, receiver operating characteristic curve; RFR, resting full-cycle ratio; FFR, fractional flow reserve; Pd, distal coronary pressure; Pa, aortic pressure.
ROC analyses for the prediction of Pd/Pa ≤ 0.92 showed an AUC (C statistic) of 0.96 (95% CI 0.94–0.98, p < 0.01). Using Pd/Pa ≤ 0.92 as a reference, the sensitivity, specificity, PPV, NPV, and overall diagnostic accuracy of RFR were determined as 86.8%, 92.6%, 82.5%, 94.6%, and 90.9%, respectively. (Fig. 3b).
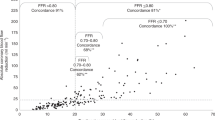
Accuracy of RFR with FFR in the RFR hyperemia zone (RFR: 0.86–0.93)
In the RFR hyperemia zone (RFR: 0.86–0.93), the value was divided into positive (RFR: 0.86 to 0.89) and negative (RFR: 0.90 to 0.93) areas to evaluate the accuracy of RFR with FFR, which was 47.8% (95% CI 33.8%–62.0%) in the positive area and 87.7% (95% CI 80.3%–93.1%) in the negative area. Outside the hyperemia zone, the accuracy of RFR < 0.86 with FFR ≤0.80, and RFR >0.93 with FFR >0.80 were 84.2% (64/76, 95% CI 72.5%–92.4%) and 96.8% (179/185, 95% CI 92.4–99.0%), respectively (Fig. 4). Therefore, the accuracy of RFR with FFR in the entire outer part of the hyperemia zone was 93.1% (95% CI 88.7–96.2) (Fig. 5).
FFR versus RFR in the hyperemia and hyperemia-free zones. Red and blue dots represent the disagreement and agreement, respectively, between the two strategies (RFR vs. FFR) in the hyperemia-free zone (RFR value < 0.86 and > 0.93). Light red and blue dots represent the hyperemia zone (RFR: 0.86–0.93), reclassified into positive (RFR: 0.86–0.89) and negative (RFR: 0.90–0.93) areas.
Comparison of patient numbers according to RFR and FFR values in the hyperemia and hyperemia-free zones. Red and blue spots represent the disagreement and agreement, respectively, between the two strategies in the hyperemia-free zone. In the hyperemia-free zone, the accuracy rate is 93.1% (243/261).
Clinical predictors of discordance between FFR and RFR
In univariable analysis for discordance predictors, diabetes mellitus and left anterior descending artery lesion were the factors with p value less than 0.1. However, diabetes mellitus [odds ratio (OR); 1.80, 95% confidence interval (CI); 1.07–3.07; p = 0.026] was the only significant factor for predicting discordance between FFR and RFR in multivariate analysis. (Supplementary Table 1).
Discussion
This prospective observational study (ICE-FLOWER) analyzed the validation of a novel non-hyperemic resting physiologic index using RFR for coronary artery intermediate stenosis in patients with IHD. Herein, we reported several clinically important findings to support the effective application of RFR with FFR in daily clinical practice. First, RFR value showed a good correlation with FFR value in the present study as compared to that in the previous study that used iFR, which is the gold standard of NHPR. Second, compared with the FFR (≤ 0.80) value, RFR (≤ 0.89) value in the present study showed a favorable accuracy rate of 85.0%, which was comparable to that of iFR or FFR in other studies. Third, RFR value demonstrated low accuracy (47.8%) in the positive area of the hyperemia zone (0.86–0.89); therefore, additional FFR would be required to evaluate functional coronary stenosis accurately in the positive area.
FFR-guided PCI has shown superior clinical outcomes in randomized trials, and it is recommended as class 1A in current guidelines for intermediate coronary artery stenosis4,5,24. However, the rate of FFR-guided PCI for intermediate coronary lesions in real-world practice is very low because of time, cost, and risk of adenosine- or nicorandil-induced maximal hyperemia7,8,9. NHPRs have emerged recently, and among them, iFR demonstrated non-inferiority compared with FFR in two randomized control trials; further it is recommended in the guidelines for class 1A10,11. RFR is one of the NHPR indices, and it has been introduced for obtaining the absolute Pd/Pa value of the entire cardiac cycle14. The present study demonstrated a good correlation between RFR and FFR and excellent diagnostic accuracy of RFR (> 85%) as compared to FFR in real-world practice. A few recent studies showed that RFR was diagnostically equivalent to iFR and had a comparable value with FFR16,17,25. In two recently published studies comparing RFR and FFR, the accuracy rate was 78% in a study from Germany that analyzed 712 lesions and 79% in a study from Spain that analyzed 380 lesions16,17. These accuracy rates were similar to those in previous studies comparing iFR and FFR26,27. Regarding the validation of RFR, the present study showed a higher accuracy rate than previous studies.
Discordant findings of NHPRs and FFR have shown worse prognosis compared to concordant negative indices in previous trials. In our study, only diabetes mellitus known as microvascular dysfunction, a discordant factor also identified in previous studies28, was found to be a significantly influencing factor. Further, there is an ongoing debate with growing interest whether discordant lesions should be revascularized29. To overcome such disadvantages and limitations, few studies have suggested a hybrid approach using FFR and NHPR simultaneously during decision-making for revascularization22. However, the accuracy of iFR or RFR in the hyperemia-free zone is reported to be > 90% in some studies, except for the gray zone with a value of 0.86–0.9316,30. When the hyperemia zone was excluded, the accuracy of the correlation of RFR with FFR increased in the present study (93.1%) compared to that in other studies. In addition, we further analyzed the hyperemia zone by dividing it into positive (RFR: 0.86–0.89) and negative (RFR: 0.90–0.93) areas. Notably, the accuracy rate in the negative area was 87.7%, similar to that in the hyperemia-free zone, whereas the accuracy rate in the positive area was only 47.8%. Previous iFR studies suggested the need for a hybrid approach in the entire hyperemia zone because of the low accuracy rate11,13,22, and a recent RFR-FFR study also reported a low accuracy rate of 68% in the hyperemia zone (RFR: 0.86–0.93)16. However, because the present study showed that the accuracy rate in the negative area was similar to that in the hyperemia-free zone, we cautiously suggest that RFR alone could predict the functional significance of the intermediate lesion, except in the positive area of the hyperemia zone (13.8% of participants in the present study). The strategy of additionally implementing FFR in the positive area of the hyperemia zone might improve the diagnostic accuracy of RFR and can avoid unnecessary adenosine- or nicorandil-induced hyperemia to ensure patients’ comfort and time and cost savings. In the future, a large-scale randomized trial should be conducted using FFR and NHPR, including iFR with RFR, which can overcome the limitations of iFR and RFR to evaluate intermediate coronary artery stenosis accurately.
Study limitations
This study has several limitations. First, it was a prospective observational study conducted in a single center. Second, among NHPR, iFR, which is the gold standard, could not be compared directly with RFR in this study. However, since RFR showed a strong correlation with Pd/Pa, it might be replaced by the iFR value. Third, the percentage of stenosis > 70% (26/474, 5.5%) was limited, which reduced the validity in reference to angiographically significant lesions (see Supplementary Fig. S2). To address these limitations, a large-scale multicenter trial using RFR with FFR is required.
Conclusions
RFR and FFR values showed a good correlation with a high accuracy rate (RFR ≤ 0.89, FFR ≤ 0.8) in real-world clinical practice for intermediate coronary lesions. In addition, for further analysis of the hyperemia zone, RFR alone could evaluate the functional significance of coronary artery stenosis without unnecessary hyperemia, except in the positive area (RFR: 0.86–0.89) of the hyperemia zone.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Pijls, N. H. et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J. Am. Coll. Cardiol. 49(21), 2105. https://doi.org/10.1016/j.jacc.2007.01.087 (2007).
Tonino, P. A. et al. FAME study investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N. Engl. J. Med. 360(3), 213. https://doi.org/10.1056/NEJMoa0807611 (2009).
De Bruyne, B. et al. FAME 2 trial investigators fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N. Engl. J. Med. 367(11), 991–1001. https://doi.org/10.1056/NEJMoa1205361 (2012).
Neumann, F. J. et al. ESC scientific document group 2018 ESC/EACTS guidelines on myocardial revascularization. Eur. Heart J. 40(2), 87–165. https://doi.org/10.1093/eurheartj/ehy394 (2019).
Lawton, J. S. et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation 145(3), e18–e114. https://doi.org/10.1161/CIR.0000000000001038 (2022).
Jang, H. J. et al. Safety and efficacy of a novel hyperaemic agent, intracoronary nicorandil, for invasive physiological assessments in the cardiac catheterization laboratory. Eur. Heart J. 34(27), 2055–2062. https://doi.org/10.1093/eurheartj/eht040 (2013).
Dattilo, P. B., Prasad, A., Honeycutt, E., Wang, T. Y. & Messenger, J. C. Contemporary patterns of fractional flow reserve and intravascular ultrasound use among patients undergoing percutaneous coronary intervention in the United States: Insights from the national cardiovascular data registry. J. Am. Coll. Cardiol. 60(22), 2337–2339. https://doi.org/10.1016/j.jacc.2012.08.990 (2012).
Kim, J. H. et al. The current status of intervention for intermediate coronary stenosis in the Korean percutaneous coronary intervention (K-PCI) registry. Korean Circ. J. 49(11), 1022–1032. https://doi.org/10.4070/kcj.2019.0074 (2019).
Tanaka, N. et al. Treatment strategy modification and its implication on the medical cost of fractional flow reserve-guided percutaneous coronary intervention in Japan. J Cardiol. 73(1), 38–44. https://doi.org/10.1016/j.jjcc.2018.05.018 (2019).
Davies, J. E. et al. Use of the instantaneous wave-free ratio or fractional flow reserve in PCI. N. Engl. J. Med. 376(19), 1824–1834. https://doi.org/10.1056/NEJMoa1700445 (2017).
Götberg, M. et al. iFR-SWEDEHEART Investigators. Instantaneous wave-free ratio versus fractional flow reserve to guide PCI. N. Engl. J. Med. 376(19), 1813–1823. https://doi.org/10.1056/NEJMoa1616540 (2017).
Lawton, J. S. et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. J. Am. Coll. Cardiol. 79(2), e21–e129. https://doi.org/10.1016/j.jacc.2021.09.006 (2022).
Cook, C. M. et al. Fractional flow reserve/ instantaneous wave-free ratio discordance in Angiographically intermediate coronary Stenoses: An analysis using doppler-derived coronary flow measurements. JACC Cardiovasc Interv. 10(24), 2514–2524. https://doi.org/10.1016/j.jcin.2017.09.021 (2017).
Svanerud, J. et al. Validation of a novel non-hyperaemic index of coronary artery stenosis severity: The Resting Full-cycle Ratio (VALIDATE RFR) study. EuroIntervention. 14(7), 806–814. https://doi.org/10.4244/EIJ-D-18-00342 (2018).
Muroya, T. et al. Relationship between resting full-cycle ratio and fractional flow reserve in assessments of coronary stenosis severity. Catheter Cardiovasc Interv. 96(4), E432–E438. https://doi.org/10.1002/ccd.28835 (2020).
Wienemann, H. et al. Comparison of resting full-cycle ratio and fractional flow reserve in a german real-world cohort. Front Cardiovasc Med. 24(8), 744181. https://doi.org/10.3389/fcvm.2021.744181 (2021).
Casanova-Sandoval, J. et al. Usefulness of the Hybrid RFR-FFR Approach: Results of a prospective and multicenter analysis of diagnostic agreement between RFR and FFR-The RECOPA (REsting full-cycle ratio comparation versus fractional flow reserve (a prospective validation)) study. J. Interv. Cardiol. 31(2021), 5522707. https://doi.org/10.1155/2021/5522707 (2021).
Fearon, W. F. et al. ACIST-FFR study investigators ACIST-FFR Study (assessment of catheter-based interrogation and standard techniques for fractional flow reserve measurement). Circ Cardiovasc Interv. 10(12), e005905. https://doi.org/10.1161/CIRCINTERVENTIONS.117.005905 (2017).
Matsumura, M. et al. Accuracy of fractional flow reserve measurements in clinical practice: Observations from a core laboratory analysis. JACC Cardiovasc Interv. 10(14), 1392–1401. https://doi.org/10.1016/j.jcin.2017.03.031 (2017).
Koo, B. K. et al. FLAVOUR investigators fractional flow reserve or intravascular ultrasonography to guide PCI. N. Engl. J. Med. 387(9), 779–789. https://doi.org/10.1056/NEJMoa2201546 (2022).
Lee, H. S. et al. Consensus document for invasive coronary physiologic assessment in Asia-Pacific countries. Cardiol J. 26(3), 215–225. https://doi.org/10.5603/CJ.a2019.0054 (2019).
Petraco, R. et al. Hybrid iFR-FFR decision-making strategy: Implications for enhancing universal adoption of physiology-guided coronary revascularisation. EuroIntervention 8(10), 1157–1165. https://doi.org/10.4244/EIJV8I10A179 (2013).
Bossuyt, P. M. et al. Standards for reporting of diagnostic accuracy. The STARD statement for reporting studies of diagnostic accuracy: Explanation and elaboration. Ann. Intern. Med. 138(1), W1-12. https://doi.org/10.7326/0003-4819-138-1-200301070-00012-w1 (2003).
Xaplanteris, P. et al. FAME 2 Investigators. Five-year outcomes with PCI guided by fractional flow reserve. N. Engl. J. Med. 379(3), 250–259. https://doi.org/10.1056/NEJMoa1803538 (2018).
Lee, J. M. et al. Physiological and clinical assessment of resting physiological indexes. Circulation 139(7), 889–900. https://doi.org/10.1161/CIRCULATIONAHA.118.037021 (2019).
Park, J. J. et al. Clinical validation of the resting pressure parameters in the assessment of functionally significant coronary stenosis; results of an independent, blinded comparison with fractional flow reserve. Int. J. Cardiol. 168(4), 4070–4075. https://doi.org/10.1016/j.ijcard.2013.07.030 (2013).
Sen, S. et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: Results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J. Am. Coll. Cardiol. 59(15), 1392–1402. https://doi.org/10.1016/j.jacc.2011.11.003 (2012).
Camici, P. G. & Crea, F. Coronary microvascular dysfunction. N. Engl. J. Med. 356(8), 830–840. https://doi.org/10.1056/NEJMra061889 (2007).
Lee, J. M. et al. Long-term clinical outcomes of nonhyperemic pressure ratios: resting full-cycle ratio, diastolic pressure ratio, and instantaneous wave-free ratio. J. Am. Heart Assoc. 9(18), e016818. https://doi.org/10.1161/JAHA.120.016818 (2020).
Shuttleworth, K., Smith, K., Watt, J., Smith, J. A. L. & Leslie, S. J. Hybrid instantaneous wave-free ratio-fractional flow reserve versus fractional flow reserve in the real world. Front Cardiovasc Med. 30(4), 35. https://doi.org/10.3389/fcvm.2017.00035 (2017).
Acknowledgements
The authors thank all the staff working in the cardiac catheterization laboratory at Yongin Severance Hospital for their commitment to this study.
Funding
This study was supported by a grant from Abbott Vascular. Abbott Vascular was not involved in the study design and data analysis or interpretation of findings.
Author information
Authors and Affiliations
Contributions
O.-H.L. and Y.K.: study concept and design and drafting for the manuscript. O.-H.L., J.R., Y.K., E.I., and D.-K.C.: acquired the data. Y.K. and D.-K.C.: supervised the progress of the study. O.-H.L., J.R., Y.K., and S.H.: acquisition, analysis, and interpretation of data. O.-H.L., J.R., Y.K., S.H., E.I., D.-K.C., critical revision of the manuscript for important intellectual content. All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, OH., Roh, J.W., Kim, Y. et al. Invasive physiologic assessment of coronary artery stenosis by resting full-cycle ratio and fractional flow reserve: a prospective observational study. Sci Rep 13, 15783 (2023). https://doi.org/10.1038/s41598-023-43082-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43082-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.