Abstract
Nonalcoholic fatty liver disease (NAFLD) can lead to a prothrombotic state, which significantly burdens public healthcare systems. This study investigated the relationship between NAFLD and the incidence of venous thromboembolism (VTE) in Korea using National Health Insurance Service-National Sample Cohort 2.0 data. A population-based retrospective cohort analysis was conducted on 472,212 healthy individuals who underwent national health check-ups in Korea from 2009 to 2014. NAFLD was defined using the fatty liver index (FLI). Multivariate Cox proportional hazards regression models were used to analyze the association between FLI and VTE. Individuals were categorized into four quartiles according to FLI values (first quartile [Q1], 0–5.7; second quartile [Q2], 5.8–15.3; third quartile [Q3], 15.4–37.2; and fourth quartile [Q4], > 37.2). The incidence of VTE tended to increase with increasing FLI values (Q1, 598 [0.5%]; Q2, 1,033 [0.9%]; Q3, 1,443 [1.2%]; and Q4, 1,425 [1.2%]). In the age- and sex-adjusted multivariate model, the hazard ratio (HR) (95% confidence interval [CI]) was 1.47 (1.33‒1.62) for Q4 compared with Q1. After adjusting for clinical variables with P < 0.1 in the univariate analyses, the HR (95% CI) was 1.45 (1.30‒1.62) for Q4 compared with Q1. FLI was related to VTE risk, as confirmed after adjusting for other risk factors.
Similar content being viewed by others
Introduction
Nonalcoholic fatty liver disease (NAFLD) refers to a broad spectrum of liver diseases ranging from steatosis to nonalcoholic steatohepatitis (NASH) and cirrhosis. It has become increasingly prevalent worldwide, placing a significant burden on public healthcare systems1. The fatty accumulation in NAFLD is not only confined to the liver. It is a multisystem disease with possible extrahepatic manifestations, including colorectal cancer, cardiovascular disease (CVD), type 2 diabetes, metabolic syndrome, chronic kidney disease, polycystic ovary syndrome, and obstructive sleep apnea2.
Aside from NAFLD, venous thromboembolism (VTE) is also an emerging health problem and a leading cause of death worldwide3, 4. It is caused by various risk factors, including immobility, trauma, cancer, age, genetic or acquired thrombophilia, oral contraceptives, and obesity5. The development of VTE is related to venous stasis, hypercoagulability, and endothelial cell damage, which are known as Virchow’s triad.
Studies found that NAFLD is a “thrombophilic state”6,7,8 and CVD, to some extent attributable to arterial thrombosis, are the leading causes of death in patients with NAFLD1, 9. Several studies have investigated the relationship between advanced liver disease and increased risk of VTE10,11,12. However, only few small sample-sized studies revealed the association between fatty liver and VTE risk and their underlying mechanisms13,14,15, while only one observational study had a sufficient sample size11. Therefore, the present study aimed to assess the relationship between NAFLD and the incidence of VTE among healthy Korean adults.
Results
Baseline characteristics of participants
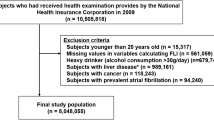
A total of 644,940 participants underwent national health check-ups at least once from January 2009 to December 2014. Based on the prespecified exclusion criteria, the data of 472,212 participants were analyzed. Figure 1 shows a list of participants who were excluded. The study population was divided into four groups based on fatty liver index (FLI) quartile values (first quartile [Q1], 0–5.7; second quartile [Q2], 5.8–15.3; third quartile [Q3], 15.4–37.2; and fourth quartile [Q4], > 37.2). Table 1 summarizes the baseline characteristics of the study population according to FLI quartile values.
An increase in the percentage of men, body mass index (BMI), proportion of current smokers, and amount of alcohol consumption was observed among participants from Q1 to Q4. Participants with higher FLI values had higher blood pressures, fasting glucose levels, and gamma-glutamyltransferase (GGT) levels and more comorbidities than those with lower FLI values. The lipid profiles became unfavorable with increasing FLI values.
The development of VTE was related to older age; more comorbidities; and higher BMI, glucose, cholesterol, aspartate aminotransferase (AST), and AST/alanine transaminase (ALT) ratio (Table 2). Alcohol consumption, ALT, and activity were not related to the development of VTE.
Association between FLI and VTE incidence
The median follow-up duration was 7.2 years (interquartile range, 4.6‒8.3), and new-onset VTE occurred in 4,499 individuals (1.0%). Figure 2 illustrates the cumulative incidence of new-onset VTE according to the FLI quartile groups. Supplementary Figs. 1 and 2 show the cumulative incidence of pulmonary thromboembolism (PTE) and deep vein thrombosis (DVT), respectively. The incidence of VTE tended to increase with increasing FLI values (Q1, 598 [0.5%]; Q2, 1033 [0.9%]; Q3, 1443 [1.2%]; and Q4, 1425 [1.2%]). Table 3 shows the univariate analysis results of new-onset VTE. In the age- and sex-adjusted multivariate model (model 1), the hazard ratio (HR) (95% confidence interval [CI]) was 1.47 (1.33‒1.62) for Q4 compared with Q1. When the model was further adjusted for clinical variables with P < 0.1 in the univariate analyses (model 2), the HR (95% CI) was 1.45 (1.30‒1.62) for Q4 compared with Q1 (Table 4).
The same trend was observed when PTE and DVT were analyzed separately (Supplementary Tables 1 and 2).
Additionally, the analysis was performed using various FLI cutoff criteria as suggested in previous studies. The group with the highest FLI values had the highest risk for new-onset VTE regardless of the cutoff criteria (Supplementary Table 3).
Subgroup analysis of clinical variables affecting VTE incidence
Figure 3 shows the adjusted HRs according to subgroups. In all subgroups, the VTE incidence tended to increase with higher FLI values (Fig. 3).
Discussion
This study investigated the relationship between NAFLD and VTE incidence in the Korean general population using national health check-up data. The results showed that FLI, a surrogate marker for fatty liver, was related to VTE risk, which was confirmed after adjusting for other clinical risk factors for VTE. This finding implies that individuals with higher FLI values and without overt liver disease have increased risk of VTE than those with lower FLI values. To the best of our knowledge, no previous study has investigated the relationship between FLI and VTE.
Despite the increasing prevalence of NAFLD, few studies have investigated the relationship between NAFLD and VTE incidence. In a case–control study of 138 consecutive patients with idiopathic VTE, Di Minno et al. found that the prevalence of NAFLD was 2.7-fold higher than that in the control group13. Furthermore, Stine et al. found that NASH etiology increased VTE risk by approximately 2.5-fold among hospitalized cirrhotic patients compared with other etiologies, implicating thrombosis mechanisms14. They also showed that liver transplant recipients with NASH were more likely to have portal vein thrombosis and VTE than those without15.
The development of VTE is related to venous stasis, endothelial dysfunction, and hypercoagulability. Among them, hypercoagulability and endothelial dysfunction could be implicated as the potential pathophysiologic mechanisms linking NAFLD to VTE16. Since the liver produces most factors associated with coagulation and fibrinolysis pathways, advanced liver disease of any etiology commonly exhibits disruptions in the coagulation pathway. NAFLD is associated with a relatively hypercoagulable state. Although the precise underlying mechanisms remain unknown, chronic liver inflammation is likely to be the most important trigger for disrupting the balance of the coagulation system16,17,18,19. Several studies found increased levels of individual procoagulant factors in patients with NAFLD. Kotronen et al. demonstrated increased activity of coagulation factors VIII, IX, XI, and XII in patients with NAFLD, independent of age, sex, and BMI20. In a study of histologically proven NAFLD, Verrijken et al. showed that NAFLD severity was independently associated with plasminogen activator inhibitor-1 levels among obese or overweight patients21. Tripodi et al. demonstrated a procoagulant imbalance in NAFLD using a new parameter called “thrombin generation,” a global coagulation procedure22. They found that thrombin generation increased sequentially from controls to steatosis or NASH and metabolic cirrhosis and that metabolic cirrhosis, the most advanced form, showed the highest factor VIII levels and lowest protein C levels.
This study had some limitations. First, FLI is a “surrogate marker” for fatty liver, not a diagnostic test. Although liver biopsy is considered the gold standard for diagnosing NAFLD, it is invasive, expensive, and has a possibility of sampling error. On the other hand, other imaging tests including abdominal ultrasound, computed tomography scan, and magnetic resonance imaging also have their limitations when used uniformly in a large number of patients. Many epidemiologic studies have used the FLI scoring system, which has shown relatively good diagnostic accuracy23,24,25. Second, NAFLD is defined as fat accumulation in the liver “without excessive alcohol intake” (< 140 g per week in women and 210 g per week in men). Thus, some individuals with alcoholic fatty liver might have been included in our cohort considering the amount of alcohol consumption. However, subgroup analysis showed equally significant results for nonalcoholics. Third, since this is an observational study, the causal relationship between NAFLD and increased risk of VTE could not be proven. Therefore, additional studies are needed to prove the causality.
In conclusion, FLI, a surrogate marker for NAFLD, was found to be associated with VTE incidence among the general adult population in Korea.
Methods
Ethical approval
This study was approved by the Institutional Review Board of Chungnam National University Hospital (No. 2023-04-001) and conducted in accordance with the Declaration of Helsinki (1989) by the World Medical Association. Informed consent was waived by the Institutional Review Board of Chungnam National University Hospital because anonymous clinical data were used in the analysis.
Data source
This study analyzed data from the National Health Insurance Service-National Sample Cohort 2.0 (NHIS-NSC 2.0), a population-based sample cohort. The NHIS is a mandatory universal health insurance program that provides comprehensive medical care coverage to all residents in Korea, covering 97% of the total population. Approximately 2% of the total population in Korea was randomly sampled in 2006 with retrospective and prospective follow-up data from 2002 to 2015. The insured population (n = 48,222,537) was stratified into 2142 classes based on sex, age, region, eligibility status, and socioeconomic status. Subsequently, 2.1% of samples for each class were randomly selected (n = 1,021,208). Therefore, the NHIS-NCS 2.0 cohort can represent the whole Korean population26.
This cohort includes four databases: (1) beneficiary’s social demographic dataset; (2) dataset of medical claims with diagnoses based on the 10th revision of the International Classification of Disease (ICD-10) codes, hospitalization, and treatment; (3) national health check-up dataset of cohort members; and (4) dataset of medical institutions.
Adults aged 18 years or older in Korea are recommended to undergo a national health screening every other year, consisting of a laboratory test, chest radiography, physical examination, and questionnaire regarding medical history and health-related behaviors (including alcohol consumption and smoking status). In the 2013 NHIS data, 72.1% of beneficiaries reported receiving a national health check-up (26). Mortality data, including the date and cause of death from the national statistical office’s death registration database, were also included.
The NHIS-NSC 2.0 data are available to any investigator with protocols approved by the NHIS review board. This study was approved by the Institutional Review Board of Chungnam National University Hospital, Daejeon, Korea.
Study population
Adults over 18 years who had undergone national health check-ups more than once from 2009 to 2014 were enrolled in this study. The first national health check-up was defined as the index check-up, and the year of the index check-up was defined as the index year. The exclusion criteria were as follows: (a) individuals with liver disease; (b) those with prescribed medications, including lipid-lowering agents, within 2 years before the index check-up; and (c) those with missing data in the index check-up. The existence of each criterion was identified using two-year claims data before the index year.
Definition of data
BMI was calculated by dividing body weight (kg) by height squared (m2). Smoking status was classified into non-smoker, ex-smoker, and current smoker. Alcohol consumption was estimated using standardized self-report questionnaires, including questions about how much alcohol was consumed at a time and how many days of the week alcohol was consumed. Subsequently, the amount of alcohol consumption was calculated by multiplying the answers from both questions. Physical activity was estimated using the following questions: how many days in a week do you perform 30 min of light exercise, 30 min of moderate exercise, and 20 min of vigorous exercise. Light exercise, moderate exercise, and vigorous exercise were defined as two metabolic equivalent of tasks (METs), three METs, and six METs, respectively. They were multiplied by 30, 30, and 20 min, respectively, and the respective number of days in a week and then summed.
The incidence of VTE was defined as the first occurrence of DVT or PTE, or death with a diagnosis of DVT or PTE. DVT and PTE were diagnosed based on ICD-10 codes (I80.1, I80.2, and I80.3 for DVT and I26 for PTE). Data were censored at the time of VTE occurrence, loss of NHIS eligibility because of death or immigration, or completion of study (December 31, 2015).
Diagnosis of hepatic steatosis
FLI is widely known as a well-verified surrogate marker for identifying individuals with steatosis. It was calculated using four variables (triglycerides [TG], BMI, GGT, and waist circumference [WC]):\({\text{FLI }} = \, {{\left( {{\text{e}}^{{0.{953 } \times {\text{loge}}\left( {{\text{TG}}} \right) \, + \, 0.{139} \times {\text{BMI }} + \, 0.{718} \times {\text{loge}}\left( {{\text{GGT}}} \right) \, + \, 0.0{53} \times {\text{WC }} - { 15}.{745}}} } \right)} \mathord{\left/ {\vphantom {{\left( {{\text{e}}^{{0.{953 } \times {\text{loge}}\left( {{\text{TG}}} \right) \, + \, 0.{139} \times {\text{BMI }} + \, 0.{718} \times {\text{loge}}\left( {{\text{GGT}}} \right) \, + \, 0.0{53} \times {\text{WC }} - { 15}.{745}}} } \right)} {\left( {{1 } + {\text{ e}}^{{0.{953} \times {\text{loge}}\left( {{\text{TG}}} \right) \, + \, 0.{139} \times {\text{BMI }} + \, 0.{718} \times {\text{loge}}\left( {{\text{GGT}}} \right) \, + \, 0.0{53} \times {\text{WC }} - { 15}.{745}}} } \right)}}} \right. \kern-0pt} {\left( {{1 } + {\text{ e}}^{{0.{953} \times {\text{loge}}\left( {{\text{TG}}} \right) \, + \, 0.{139} \times {\text{BMI }} + \, 0.{718} \times {\text{loge}}\left( {{\text{GGT}}} \right) \, + \, 0.0{53} \times {\text{WC }} - { 15}.{745}}} } \right)}} \times {1}00\).
Initially, an FLI value ≥ 60 was suggested as the criterion for diagnosing hepatic steatosis with a positive likelihood ratio of 4.3 in the general population27. Although the FLI is easy to obtain and calculated to screen fatty liver disease, there is insufficient evidence to support the diagnosis of fatty liver disease in Asians using FLI because they have lower BMI and WC compared with other ethnic populations28. Consequently, the study population was classified into quartiles according to their FLI value and then analyzed.
Statistical analysis
Data are expressed as mean ± standard deviation for continuous variables and percentages for categorical variables. One-way analysis of variance and Pearson’s chi-square test were used to compare the difference between FLI quartiles. Kaplan‒Meier estimates and log-rank test were used to calculate and compare cumulative event rates between FLI quartile-based groups. Cox proportional hazards regression models were used to provide adjusted HRs with 95% CI for VTE incidence. Data were adjusted for age and sex (model 1). Moreover, clinical variables showing borderline association with new-onset VTE (P < 0.10) in univariate analyses were incorporated into model 2.
For subgroup analyses, FLI values were integrated into the statistical model as a continuous variable after log transformation. Statistical significance was considered at P < 0.05. R software (version 3.4.4) was used for statistical analyses (R Foundation for Statistical Computing, Vienna, Austria; www.r-project.org).
Data availability
The NHIS-NSC 2.0 is available to investigator with a protocol approved by the NHIS review board. The datasets is opened to investigator for a limited period of time. The analysis results of the current study are available from the corresponding author on reasonable request.
References
Murag, S., Ahmed, A. & Kim, D. Recent epidemiology of nonalcoholic fatty liver disease. Gut Liver 15(2), 206–216 (2021).
Byrne, C. D. & Targher, G. NAFLD: A multisystem disease. J. Hepatol. 62(1), S47–S64 (2015).
Raskob, G. E. et al. Thrombosis: A major contributor to the global disease burden. J. Thromb. Haemost. 12(10), 1580–1590 (2014).
Beckman, M. G., Hooper, W. C., Critchley, S. E. & Ortel, T. L. Venous thromboembolism. Am. J. Prev. Med. 38(4), S495–S501 (2010).
Anderson, F. A. & Spencer, F. A. Risk factors for venous thromboembolism. Circulation 107(23), 748 (2003).
Virovic-Jukic, L., Stojsavljevic-Shapeski, S., Forgac, J., Kukla, M. & Mikolasevic, I. Non-alcoholic fatty liver disease—a procoagulant condition?. Croat. Med. J. 62(1), 25–33 (2021).
Ogresta, D. et al. Coagulation and endothelial dysfunction associated with NAFLD: Current status and therapeutic implications. J. Clin. Transl. Hepatol. 10(2), 339–355 (2022).
Tripodi, A. et al. Hypercoagulability in patients with non-alcoholic fatty liver disease (NAFLD): Causes and consequences. Biomedicines 10, 2 (2022).
Byrne, C. D. & Targher, G. NAFLD: A multisystem disease. J. Hepatol. 62(1 Suppl), S47-64 (2015).
Wu, H. & Nguyen, G. C. Liver cirrhosis is associated with venous thromboembolism among hospitalized patients in a nationwide US study. Clin. Gastroenterol. Hepatol. 8(9), 800–805 (2010).
Søgaard, K. K. et al. Risk of venous thromboembolism in patients with liver disease: A nationwide population-based case-control study. Am. J. Gastroenterol. 104(1), 96–101 (2009).
Ambrosino, P. F. et al. The risk of venous thromboembolism in patients with cirrhosis. A systematic review and meta-analysis. Thrombos. Haemost. 26(1), 139–148 (2017).
Di-Minno, M. N. D. High prevalence of nonalcoholic fatty liver in patients with idiopathic venous thromboembolism. World J. Gastroenterol. 16, 48 (2010).
Stine, J. G. et al. Increased risk of venous thromboembolism in hospitalized patients with cirrhosis due to non-alcoholic steatohepatitis. Clin. Transl. Gastroenterol. 9, 3 (2018).
Stine, J. G. et al. Increased risk of portal vein thrombosis in patients with cirrhosis due to nonalcoholic steatohepatitis. Liver Transpl. 21(8), 1016–1021 (2015).
Ciavarella, A. et al. Translational insight into prothrombotic state and hypercoagulation in nonalcoholic fatty liver disease. Thromb. Res. 198, 139–150 (2021).
Chen, J. & Chung, D. W. Inflammation, von Willebrand factor, and ADAMTS13. Blood 132(2), 141–147 (2018).
Esmon, C. T. The interactions between inflammation and coagulation. Br. J. Haematol. 131(4), 417–430 (2005).
Targher, G. et al. Non-alcoholic hepatic steatosis and its relation to increased plasma biomarkers of inflammation and endothelial dysfunction in non-diabetic men. Role of visceral adipose tissue. Diabet. Med. 22(10), 1354–1358 (2005).
Kotronen, A. et al. Increased coagulation factor VIII, IX, XI and XII activities in non-alcoholic fatty liver disease. Liver Int. 31(2), 176–183 (2011).
Verrijken, A. et al. Prothrombotic factors in histologically proven nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology 59(1), 121–129 (2014).
Tripodi, A. et al. Procoagulant imbalance in patients with non-alcoholic fatty liver disease. J. Hepatol. 61(1), 148–154 (2014).
Cho, E.-J. et al. Fatty liver index for predicting nonalcoholic fatty liver disease in an asymptomatic Korean population. Diagnostics 11, 12 (2021).
Huang, X. et al. Validation of the fatty liver index for nonalcoholic fatty liver disease in middle-aged and elderly Chinese. Medicine 94(40), e1682 (2015).
Motamed, N. et al. Fatty liver index (FLI) and prediction of new cases of non-alcoholic fatty liver disease: A population-based study of northern Iran. Clin. Nutr. 39(2), 468–474 (2020).
Lee, J., Lee, J. S., Park, S.-H., Shin, S. A. & Kim, K. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. https://doi.org/10.1093/ije/dyv319 (2016).
Bedogni, G. et al. The Fatty Liver Index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 6(1), 78 (2006).
Grundy, S. M. et al. Diagnosis and management of the metabolic syndrome. Circulation 112(17), 2735–2752 (2005).
Funding
This work was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, the Ministry of Food and Drug Safety) (Project Number: RS-2020-KD000013).
Author information
Authors and Affiliations
Contributions
C.Y.K. wrote the main manuscript text. N.K. contributed to drafting of the tables. J.H.R. and N.K. contributed equally to this work as corresponding authors. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, CY., Kim, N. & Roh, JH. Association of nonalcoholic fatty liver disease and venous thromboembolic disease in healthy adults in Korea: a nationwide study. Sci Rep 13, 16069 (2023). https://doi.org/10.1038/s41598-023-42963-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42963-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.