Abstract
Sperm quality can be easily influenced by living environmental and occupational factors. This study aimed to discover potential semen quality related living environmental and occupational factors, expand knowledge of risk factors for semen quality, strengthen men's awareness of protecting their own fertility and assist the clinicians to judge the patient’s fertility. 465 men without obese or underweight (18.5 < BMI < 28.5 kg/m2), long-term medical history and history of drug use, were recruited between June 2020 to July 2021, they are in reproductive age (25 < age < 45 years). We have collected their semen analysis results and clinical information. Logistic regression was applied to evaluate the association of semen quality with different factors. We found that living environment close to high voltage line (283.4 × 106/ml vs 219.8 × 106/ml, Cohen d = 0.116, P = 0.030) and substation (309.1 × 106/ml vs 222.4 × 106/ml, Cohen d = 0.085, P = 0.015) will influence sperm count. Experienced decoration in the past 6 months was a significant factor to sperm count (194.2 × 106/ml vs 261.0 × 106/ml, Cohen d = 0.120, P = 0.025). Living close to chemical plant will affect semen PH (7.5 vs 7.2, Cohen d = 0.181, P = 0.001). Domicile close to a power distribution room will affect progressive sperm motility (37.0% vs 34.0%, F = 4.773, Cohen d = 0.033, P = 0.030). Using computers will affect both progressive motility sperm (36.0% vs 28.1%, t = 2.762, Cohen d = 0.033, P = 0.006) and sperm total motility (57.0% vs 41.0%, Cohen d = 0.178, P = 0.009). After adjust for potential confounding factors (age and BMI), our regression model reveals that living close to high voltage line is a risk factor for sperm concentration (Adjusted OR 4.03, 95% CI 1.15–14.18, R2 = 0.048, P = 0.030), living close to Chemical plants is a protective factor for sperm concentration (Adjusted OR 0.15, 95% CI 0.05–0.46, R2 = 0.048, P = 0.001) and total sperm count (Adjusted OR 0.36, 95% CI 0.13–0.99, R2 = 0.026, P = 0.049). Time spends on computer will affect sperm total motility (Adjusted OR 2.29, 95% CI 1.11–4.73, R2 = 0.041, P = 0.025). Sum up, our results suggested that computer using, living and working surroundings (voltage line, substation and chemical plants, transformer room), and housing decoration may association with low semen quality. Suggesting that some easily ignored factors may affect male reproductive ability. Couples trying to become pregnant should try to avoid exposure to associated risk factors. The specific mechanism of risk factors affecting male reproductive ability remains to be elucidated.
Similar content being viewed by others
Introduction
As the problem of astogeny and birth rates falling became more popular worldwide, infertility has significantly negative affecting on overall fertility and family harmony1. Infertility is a disease that defined as fail to conceive after 12 months of regular and unprotected sexual intercourse. In recent decades, affect by multiple negative factors, the infertility rate increased significantly worldwide, which is about 12–20%2,3. The infertility rate in China is about 12.5%, and is also rising. In up to 40% of the infertility couples, men must be responsible for the inability to conceive4.
Male infertility is related with a few varieties of causation. Except for the irreversible reasons (such as genetic), and the organic diseases like varicocele, we should also pay attention to demographic factors. For example, occupations and living environment, which may not be so influential as organic disorder and genopathy to male fertility, yet these factors are easy to be ignored. But for most of people, they tend to maintain only one or several similar occupations and seldom change their living environment, this may lead to the potential infertility related factors of environment and occupations influence people’s fertility for their entire life. Furthermore, manifold factors can affect together as an additive effect, may result in an infertility phenotype even more serious than organic disorder. Thus, in addition to clinical diagnosis or medical research on male infertility, attention also should be paid on the influence from occupational and environmental factors on male fertility.
A mass of researches have been conducted about effect of occupational and environmental factors on male fecundity, studies about occupations and semen quality indicated that sperm of the people engaged in the transportation business have the lowest motility5,6. Another research had pointed out that occupations like farmer, workers in printing factories and oil workers who are close to toxic chemicals are related to poor male fertility7,8. Although many researches are supporting the view that occupations are relevant to semen quality, some papers have different standpoint, they drew a conclusion that occupation had no significant association to semen quality9. This kind of discrepancy may due to variety of occupations and population differences and more explorations are needed.
Living environmental factors are also related to male fertility and plenty of relevant researches had been conducted. A meta-analysis conducted by J. A. Adams had shown that cellular telephones using may negatively correlate with sperm motility but have no relationship with sperm concentration10. Abdollahi held a single fertility center cohort study which indicated that environmental noise will result in the low motility and abnormality of sperm11,12. Houses decoration also potentially affect male fertility. During the decoration, there are mainly three toxic substances correlated with semen quality: benzene, formaldehyde and ammonia. And these kinds of toxins remain high levels of concentration in the house after the decoration. Researches had shown that these substances are highly relevant to male infertility13,14.
To learn as much as we can about the environmental and occupational factors our patients have experienced. We had designed three questionnaires about demographic characteristics and living environmental and occupational factors as exposures. We constructed these questionnaires base on the living habits of most Chinese people.
Herein, based on our fertility cohort, more than 465 couples were enrolled to this research during June 2020 to July 2021. We had collected couples’ essential information as well as occupation and environment expose questionnaires. In addition, we had finished these couples’ pregnancy follow-up visits. This study intends to explore which occupational and environmental factors related to low semen quality and influence the likelihood of a successful pregnancy.
Materials and methods
Study population
We enrolled couples from Guangzhou Women and Children's Medical Center in China, Guangzhou for free pre-pregnancy medical examinations. As a national welfare of China, this program, provided as part of China's national welfare system, allows couples to undergo comprehensive physical check-ups before marriage and planning pregnancy to ensure the health of both parents and the baby. They were invited to take part in a prospective cohort which were focused on the issue if occupational and environmental factors influence fertility. Herein, after excluded male partners with a medical history of systemic diseases, infertility related disease (including varicocele, cryptorchidism, and azoospermia, etc.), obese or underweight (18.5 < BMI < 28.5 kg/m2), and long-term medication history, totally 465 male partners of couple age 31 to 43 years were included in this study between June 2020 to July 2021. All of them have completed three questionnaires which were about living environment, occupation, and basis information of demographic, respectively. The study population consisted of individuals of East Asian descent.
After excluding male partners with a medical history of systemic diseases, infertility-related diseases (including varicocele, cryptorchidism, and azoospermia, etc.), and long-term medication history, a total of 465 couples were included in this study between June 2020 to July 2021.
Physical examination and semen analysis
Physical examinations and semen analyses were conducted on the same day. Participants' body mass index (BMI: weight divided by height squared (kg/m2)) was recorded, and the testicles and scrotums were examined to exclude individuals with varicocele or other abnormalities of the reproductive organs.
Participants were instructed to abstain from sexual activity for three to seven days before the semen analysis and physical examination. Semen samples were collected in a sterile semen container by masturbation and placed in a 37 °C incubator for 30 min to liquefy. After the liquefaction, semen analysis was performed by computer aid sperm analysis (CASA, SuiJia Software, Beijing, China) to evaluate semen PH, Semen volume, sperm concentration, sperm count, sperm progressive motility, total motility. All our operations and reference values of semen parameters followed the newest guidelines of the World Health Organization (WHO)15.
Our laboratory conducted quality control regularly to guarantee the high quality of the semen analysis results.
Environment and occupation questionnaires
According to the living and working habits of people in China, we design two separate questionnaires to access participants’ environmental and occupational exposures. The questionnaires included items related to previously reported factors associated with low semen quality, such as painters7,16, drivers17, and office staff18,19. We had also designed a few extra questions for the basis demographic characteristics. Our questionnaires would be performed as multiple-choice questions.
Designed by experts from the Department of pre-marriage and pre-pregnancy health care of Guangzhou Women and Children Medical Center, the first pilot test was carried out in Wanqingsha Hospital, Nansha District, Guangdong Province. Finally, part of the questionnaires was modified according to the pilot testing results, and then conduct this study.
Ethics statement
The present study protocol was reviewed and approved by the Ethics Review Committee of the Guangzhou Women and Children's Medical Center (2016102416). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Statistical analysis
Shapiro–Wilk test and histograms was applied to assessed the normality of the data. All the seminal parameters did not conform to the normality except progressive motility (%). All data was presented as median (25th, 75th percentiles). The association between semen quality parameters and environmental and occupational factors were evaluated, Mann–Whitney U-test and Kruskal–Wallis H test for the data with a non-normal distribution (pH value, semen volume, sperm concentration, sperm count, total motility) and ANOVA for the normally distributed data (progressive motility). In order to explain the practical value of the results and judge the impact of the sample size on the results of this study, we introduced Cohen's d value to represent the effect size20.
To further explore the association between semen quality and environmental and occupational factors. Binomial logistic regression was applied to detect the independent predictors which were significantly affect semen quality, confounders were adjusted for the analysis: education21, BMI22, smoking23, alcohol consuming24 and age25. We calculated the effect size of each factor using the Cohen d statistic for the two groups comparison, and eta-squared for the observations more than two sets20,26. All P-value of less than 0.05 was taken to indicate statistical significance. Statistical analyses were performed by using SPSS version 26.0 (SPSS Inc., Chicago, IL, USA).
Preprint
A previous version of this manuscript was published as a preprint27.
Results
Characteristics of study population
As shown in Table 1, there were totally 465 males of reproductive age enrolled in this study, the mean age was 37.5 years (± 5.7 years) and the mean BMI was 23.85 kg/m2 (± 4.42 kg/m2). All participants had a permanent job and was willing to accept our follow-up service. Approximately 20.9% and 8.8% of our population are current alcohol consumers and smokers, respectively. Our study had included people of every degree of education.
Semen quality
According to our current study, the median (25th, 75th percentiles) values for semen PH was 7.4 (7.2–7.6), semen volume was 4.2 (2.6–5.2) ml, sperm concentration was 80.5 (37.0–103.6) × 106/ml, sperm count was 341.6 (121.6–429.4) × 106/ml, total motility was 54.3 (39.0–69.5) %, and the sperm progressive motility was 36.0 (22.0–48.0) (Table 2).
Correlation between environment and occupation factors and semen quality
All semen parameters did not follow the normal distribution except progressive motility (%). Mann–Whitney U-test and Kruskal–Wallis H test were applied for analysis to semen measurements with non-normal distribution. ANOVA was applied for analysis to semen measurements with normal distribution. Our results suggested that male who lived within two kilometers of a high voltage line which is defined as distribution line AC voltage in more than 1000 voltage or DC voltage in more than 1500 V electrical connection line (283.4 × 106 vs. 219.8 × 106; P = 0.030; Cohen d = 0.116) or a substation (309.1 × 106 vs. 222.4 × 106; P = 0.015; Cohen d = 0.085) would increase the sperm count (106/ml). However, when there were power distribution room located within two kilometers from our participants’ residences, their sperm progressive motility (%) decreased significantly (37.0% vs. 34.0%; F = 4.773, P = 0.030; Cohen d = 0.033). Living close to a chemical factory was another factor affecting semen quality, but based on our data from this research, although the semen PH was increased significantly (7.5 vs. 7.2; t = 2.762; P = 0.001; Cohen d = 0.181), but according to WHO’s guideline, the reference range for PH value is between 7.2 and 7.8. Therefore, whether living close to a chemical factory is a negative factor to human semen quality, more researches are needed. Decoration materials’ reproduction toxicity has got a lot of attentions. Our research found out that if anyone lives in a house undergone decoration within a half year, his sperm count would decrease (194.2 × 106 vs. 261.0 × 106; P = 0.025; Cohen d = 0.120). Another factor which has drawn much attention in recent years is computers using. We observed a decline of sperm progressive motility (within eight hours: 36.0%vs. more than 8 h: 28.1%; P = 0.006; Cohen d = 0.033) and sperm total motility (within 8 h: 57.0% vs. more than 8 h: 41.0%; P = 0.009; Cohen d = 0.178) in our participants who attach to computers every day (Table 3).
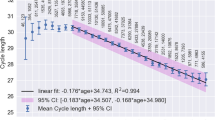
Independent predictors of low semen quality in Binomial logistic regression analysis
Table 4 and Fig. 1 shows the binomial logistic analysis results. Abnormal semen quality parameters were defined according to the guidelines of the World Health Organization15. After adjusting for potential confounders(age and BMI), our results show that to shorten the time length using the computer within a day is a protective factor to total sperm motility (Adjusted OR 2.29; 95% CI 1.11–4.73;P = 0.025; R2 = 0.041) And living close to high voltage line is a positive factor for higher sperm concentration (Adjusted OR 4.03; 95% CI 1.15–14.18; P = 0.030; R2 = 0.048). But living close to a chemical plant is a significant protective factor for higher semen concentration (Adjusted OR 0.15; 95% CI 0.05–0.46; P = 0.001; R2 = 0.048) and a higher total sperm count (Adjusted OR 0.36; 95% CI 0.13–0.99; P = 0.049; R2 = 0.026). In addition, after adjusting for confounding factors, the effect of computer use time on sperm progressive motility (%) becomes not significant. (Adjusted OR 1.07; 95% CI 0.57–1.10; P = 0.835; R2 = 0.038), it seems that this factor is more influenced by BMI or age.
Discussion
Research status
Twenty-first century to present, experts in the related field had noticed the decreasing trend in human semen quality28. There are many different possible causation for the change. It can be due to the unhealthy diet habits, such as alcohol or cigarettes intake29,30. But such negative factors can be avoided by accepting doctors’ advice. While organizing a plan for pregnancy, couples need to quit smoking or drinking alcohol as well as carry on healthy diet habits, such as refrain from taking high fat food. By following doctors’ guidance to quit smoking and drinking at least six months before trying to get pregnant, male-partners of couples would always have a better physical condition and semen quality23,31, and the chances of successful pregnancy are usually increased32. These kind of changes avoid additional expenditure while it usually will lead to a relative remarkable effect. But when it comes to environmental and occupational factors, on account of these factors are always connected to people’s working and living surroundings which are usually much steadier than diet habits, the cost of change is usually much higher. Based on our clinic experience, when we pointed out that one should avoid contacting reproduction toxic substance that existed in their working place33,34, they tended to refuse the advice. We didn't regard that they refuse to follow the intervention in an irrational way since it is impossible for an organic chemical worker to completely isolate from chemicals, and the uncertain consequence of quitting their jobs is usually unacceptable. Similarly, to avoid some of the negative factors like noise12, and electromagnetic radiation10,35,36 around their domicile, they may have to move. In the view of almost all residents, to quit a job or move to a new house just because of giving birth sounds unnecessary, even more so for couples have already raised a child. Under these circumstances, this problem had stuck into a dead loop. The negative factors keep affecting people’s fertility as long as they still exist, but changing their jobs and domicile are remaining unable to afford to most of people.
Principal findings and comparison with other studies
In this research, we analyzed several factors that may affect semen quality. We have got some results which indicated environmental and occupational factors may affect male’s fertility. Firstly, our result show that living close to power lines and substations are the positive factors for the higher level of sperm count. Besides, living close to a power distribution room may associated to a higher sperm progressive motility. Our data may indicate that electric field energy has a certain effect on semen quality, but the actual effect remains to be further studied and confirmed. Research on effect of electric field to semen quality is relative rare. However, there are also studies that indicate that the electric field effect is related to the decline of semen quality37,38, but controversy is existed in academia39. These three independent but relevant reports all indicated that electric field may be a beneficial to better sperm quality. But due to most of the power distributions or substations are away from the urban. The population live outside the cities are mainly persons of good economic conditions. which is a well-known fertility related factors which is40. Therefore, more experiments should be conducted to verify its effect. Another result shown that living close to a chemical factory may be a negative factor to semen concentration. This result is in accord with other researches, which show that amounts of industrial chemicals will do harm to reproductive system and reduce semen quality16,41,42,43. There are few works had analyzed the association between computer using and semen quality, but related factors (sitting for a long time44, electromagnetic wave45 and radiation46, etc.) had also been reported to be correlated to lower semen quality. It’s still unclear that if using computer or brain work has effect on semen quality, further experiment and researches should be conducted. To figure out the mechanisms of such multi-angle associations are quite challenging but critical issues in the field of public health, especially in the current condition when computers are widely used.
According to our results, we can draw a preliminary conclusion that some of the occupations, and environment factors will affect males’ semen quality. These kinds of factors usually damage human fertility gradually in a cumulative way, because the influence of these factors does not appear as acute diseases. In such condition, people won’t treat the negative factors seriously until they suffer from infertility problems. Fortunately, the negative impact of most factors in our everyday life are reversible. The easiest way is to intervene these factors so that they can avoid their continually damage to our reproduction system. But pregnancy consultation clinics should pay more attention to collect patients’ background information in order to provide personalized a treatment strategy.
The normal quality of semen determines the level of male fertility47. Our current results suggest that some environmental and occupational factors may be associated with changes in semen quality. This suggests that changes in environmental and occupational factors may affect male fertility by altering semen quality48. By following up the current cohort, we will in the future explore the effects of environmental and occupational factors on prolonged TTP (Time to pregnancy, TTP) due to decreased semen quality49.
Limitation and future researches direction
There were several limitations to our current findings. Firstly, due to semen quality may also be affected differently when exposed to the same occupational or environmental factors50. The population of our study is limited to Southern Chinese population, and none of our patients was from other ethnic groups. Secondly, our research only stays at epidemiology level. Thirdly, the existent of confounding factors (such as sleep duration within a day, dietary structure and economic condition, etc.) has interfered part of our results, so in the following research, we will improve our questionnaires to avoid such confounding factors. Fourthly, due to the large number of occupational and environmental factors, we did not include all relevant influencing factors in our analysis, so our current results may not account for the influence of other occupational and environmental factors on semen quality. Fifthly, the effect of dose effects of different factor was not considered in our records yet (such as the length of duration a men lived beside a high voltage line)51. In our following research, a modified quantifying will be conducted. Lastly, we only investigated epidemiological risk factors, but what are the specific substances that play a role in each risk factor. Further work should be done to isolate the specific high-risk substances from risk factors, such as specific compounds that may be present around chemical plants that can affect semen quality. In addition, the mechanisms of how high-risk substances affect human sperm quality are still waiting to be explored.
Conclusion
In summary, our research shown that computer using, living and working surroundings (voltage line, substation and chemical plants, transformer room) and housing decoration are influenced potentially semen quality. However, it is important to note that these findings are based on a limited sample size, and further research with a larger and more diverse population is required to confirm our results. Depending on the characteristics of our population, more different occupational and environmental factors should also be analyzed in our research. Additionally, due to the large number of environmental and occupational factors, we did not include all suspected factors in this study, other factors should be analyzed in future studies. Furthermore, the specific mechanisms through which these risk factors affect semen quality remain unknown, necessitating further investigation.
Overall, our findings highlight the importance of considering the impact of various environmental and occupational factors on semen quality. Continued research in this field will contribute to a better understanding of the potential risks and mechanisms involved, enabling the development of targeted interventions and strategies to support male reproductive health.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Assaysh-Oberg, S., Borneskog, C. & Ternstrom, E. Women’s experience of infertility & treatment: A silent grief and failed care and support. Sex Reprod. Healthc. 37, 100879 (2023).
Wang, L. et al. Feasibility analysis of incorporating infertility into medical insurance in China. Front. Endocrinol. 13, 967739 (2022).
Vander Borght, M. & Wyns, C. Fertility and infertility: Definition and epidemiology. Clin. Biochem. 62, 2–10 (2018).
Corsini, C. et al. Is there a relevant clinical impact in differentiating idiopathic versus unexplained male infertility?. World J. Men Health 41, 354 (2022).
Zarei, S. et al. Assessment of semen quality of taxi drivers exposed to whole body vibration. J. Occup. Med. Toxicol. 17(1), 16 (2022).
Vaziri, M. H. et al. The relationship between occupation and semen quality. Int. J. Fertil. Steril. 5(2), 66–71 (2011).
Irnandi, D. F., Hinting, A. & Yudiwati, R. DNA fragmentation of sperm in automobile painters. Toxicol. Ind. Health 37(4), 182–188 (2021).
Wijesekara, G. U. et al. Environmental and occupational exposures as a cause of male infertility. Ceylon Med. J. 60(2), 52–56 (2015).
Gracia, C. R. et al. Occupational exposures and male infertility. Am. J. Epidemiol. 162(8), 729–733 (2005).
Adams, J. A. et al. Effect of mobile telephones on sperm quality: A systematic review and meta-analysis. Environ. Int. 70, 106–112 (2014).
Abdollahi, M. B. et al. Comparison of mice’ sperm parameters exposed to some hazardous physical agents. Environ. Anal. Health Toxicol. 36(3), e2021013-2021010 (2021).
Choe, S. A. et al. Nighttime environmental noise and semen quality: A single fertility center cohort study. PLoS ONE 15(11), e0240689 (2020).
Lv, M. Q. et al. Semen quality following long-term occupational exposure to formaldehyde in China. JAMA Netw. Open 5(9), e2230359 (2022).
Rubes, J. et al. Semen quality and sperm DNA integrity in city policemen exposed to polluted air in an urban industrial agglomeration. Int J. Hyg. Environ. Health 237, 113835 (2021).
World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen (World Health Organization, 2010).
Naha, N. & Chowdhury, A. R. Inorganic lead exposure in battery and paint factory: Effect on human sperm structure and functional activity. J UOEH. 28(2), 157–171 (2006).
Jung, A. & Schuppe, H. C. Influence of genital heat stress on semen quality in humans. Andrologia 39(6), 203–215 (2007).
Gill, K. et al. The impact of sedentary work on sperm nuclear DNA integrity. Folia Histochem. Cytobiol. 57(1), 15–22 (2019).
Jurewicz, J. et al. Effects of occupational exposure: Is there a link between exposure based on an occupational questionnaire and semen quality?. Syst. Biol. Reprod. Med. 60(4), 227–233 (2014).
Brunoni, A. R. et al. The sertraline vs. electrical current therapy for treating depression clinical study: Results from a factorial, randomized, controlled trial. JAMA Psychiatry 70(4), 383–391 (2013).
Glazer, C. H. et al. Racial and sociodemographic differences of semen parameters among US men undergoing a semen analysis. Urology 123, 126–132 (2019).
Bibi, R. et al. The influence of paternal overweight on sperm chromatin integrity, fertilization rate and pregnancy outcome among males attending fertility clinic for IVF/ICSI treatment. BMC Pregnancy Childbirth 22(1), 620 (2022).
Kulaksiz, D. et al. Sperm concentration and semen volume increase after smoking cessation in infertile men. Int. J. Impot. Res. 34, 614–619 (2022).
Amor, H. et al. Impact of heavy alcohol consumption and cigarette smoking on sperm DNA integrity. Andrologia 54(7), e14434 (2022).
Petrella, F. et al. Impact of age and fertility status on the consistency of repeat measurements of sperm dna damage: A single-center, prospective, dual visit study. Urology 169, 96–101 (2022).
Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 4, 863 (2013).
Mai, M. et al. Association of Environment and Occupations Factors With Semen Quality in Male Partners of Couples Trying to Conceive, 02 March 2022, PREPRINT (Version 1) available at Research Square [https://doi.org/10.21203/rs.3.rs-1391533/v1]
Virtanen, H. E., Jorgensen, N. & Toppari, J. Semen quality in the 21(st) century. Nat. Rev. Urol. 14(2), 120–130 (2017).
Tang, Q. et al. Semen quality and cigarette smoking in a cohort of healthy fertile men. Environ. Epidemiol. 3(4), e055 (2019).
Suliga, E. & Gluszek, S. The relationship between diet, energy balance and fertility in men. Int. J. Vitam. Nutr. Res. 90(5–6), 514–526 (2020).
Finelli, R., Mottola, F. & Agarwal, A. Impact of alcohol consumption on male fertility potential: A narrative review. Int. J. Environ. Res. Public Health 19(1), 328 (2021).
Tempest, N. et al. Habitual physical activity levels in women attending the one stop infertility clinic: A prospective cross-sectional observational study. Reprod. Fertil. 3, 231–236 (2022).
Ribeiro, I. M. et al. Could metal exposure affect sperm parameters of domestic ruminants? A meta-analysis. Anim. Reprod Sci. 244, 107050 (2022).
Louis, G. M. et al. Perfluorochemicals and human semen quality: The LIFE study. Environ. Health Perspect. 123(1), 57–63 (2015).
Sterling, L., Harris, L. R. & Carroll, K. The effects of wireless devices on male reproductive health: A literature overview. Rev. Int. Androl. 20(3), 196–206 (2022).
Hagras, A. M., Toraih, E. A. & Fawzy, M. S. Mobile phones electromagnetic radiation and NAD(+)-dependent isocitrate dehydrogenase as a mitochondrial marker in asthenozoospermia. Biochim. Open 3, 19–25 (2016).
Houston, B. J. et al. The effects of radiofrequency electromagnetic radiation on sperm function. Reproduction 152(6), R263–R276 (2016).
International Commission on Non-Ionizing Radiation P. Guidelines for limiting exposure to electromagnetic fields (100 kHz to 300 GHz). Health Phys. 118(5), 483–524 (2020).
Lewis, R. C. et al. Exposure to power-frequency magnetic fields and the risk of infertility and adverse pregnancy outcomes: Update on the human evidence and recommendations for future study designs. J. Toxicol. Environ. Health B 19(1), 29–45 (2016).
Muhamad, S. et al. Sociodemographic factors associated with semen quality among Malaysian men attending fertility clinic. Andrologia 51(10), e13383 (2019).
Bernard, A. Dermal exposure to hazardous chemicals in baby diapers: A re-evaluation of the quantitative health risk assessment conducted by the French agency for food, environmental and occupational health and Safety (ANSES). Int. J. Environ. Res. Public Health 19(7), 4159 (2022).
Calvert, L. et al. Assessment of the emerging threat posed by perfluoroalkyl and polyfluoroalkyl substances to male reproduction in humans. Front. Endocrinol. 12, 799043 (2021).
Tian, T. et al. Association of bisphenol A exposure with LINE-1 hydroxymethylation in human semen. Int. J. Environ. Res. Public Health 15, 1770 (2018).
Koskelo, R., Zaproudina, N. & Vuorikari, K. High scrotal temperatures and chairs in the pathophysiology of poor semen quality. Pathophysiology 11(4), 221–224 (2005).
Kamali, K. et al. Effects of electromagnetic waves emitted from 3G+wi-fi modems on human semen analysis. Urologia 84(4), 209–214 (2017).
Wdowiak, A. et al. Background ionizing radiation and semen parameters of men with reproductive problems. Ann. Agric. Environ. Med. 27(1), 43–48 (2020).
Buck Louis, G. M. et al. Semen quality and time to pregnancy: The Longitudinal Investigation of Fertility and the Environment Study. Fertil. Steril. 101(2), 453–462 (2014).
Wu, W. et al. Association between ambient particulate matter exposure and semen quality in fertile men. Environ. Health 21(1), 16 (2022).
Snijder, C. A. et al. Occupational exposure to chemical substances and time to pregnancy: A systematic review. Hum. Reprod. Update 18(3), 284–300 (2012).
Khandwala, Y. S. et al. Racial variation in semen quality at fertility evaluation. Urology 106, 96–102 (2017).
Ramos-Flores, A. et al. Temephos decreases sperm quality and fertilization rate and is metabolized in rat reproductive tissues at low-dose exposure. Toxicol. Sci. 184(1), 57–66 (2021).
Acknowledgements
We would like to thank the Clinical Biological Resource Bank of Guangzhou Women and Children’s Medical Center for curating clinical data.
Funding
This study was funded by the Guangdong Provincial Science and Technology Plan (China, 2017A030223003), Guangzhou Medical and Health Technology Projects (China, 20191A011021 and 20191A011033), the Guangdong Natural Science Foundation (China, 2019A1515012061), Guangzhou Science and Technology Program Key Projects (China, 201904010486), Guangzhou Health Commission (China, 2021A011034), Guangdong Basic and Applied Basic Research Foundation (China, 2022A1515011237), and the Guangzhou Science and technology project(China, 202201020632, 202201020638 and 202206010100).
Author information
Authors and Affiliations
Contributions
H.M., J.K. and M.L. contributed equally to this study. Conceptualization: L.Z, H.M. Data curation: Y.X., L.F., L.P., H.Z. Formal analysis: J.K., M.L. Funding acquisition: L.Z., J.Z., D.C., X.G. Investigation: L.Z., H.M. Methodology: M.H. Project administration: L.Z., H.M. Resources: Y.X., L.F., L.P., H.Z., H.Y. Software: J.K., M.L. Supervision: L.Z., J.Z. Validation: H.M. Visualization: S.C. Writing—original draft: H.M. Writing—review and editing: Y.Q., F.J., J.Z. All authors reviewed the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mai, H., Ke, J., Li, M. et al. Association of living environmental and occupational factors with semen quality in chinese men: a cross-sectional study. Sci Rep 13, 15671 (2023). https://doi.org/10.1038/s41598-023-42927-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42927-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.