Abstract
Chronic smoking causes dysfunction of vascular endothelial cells, evident as a reduction of flow-mediated dilation in smokers, but the role of nicotine is still controversial. Given the increasing use of e-cigarettes and other nicotine products, it appears essential to clarify this issue. We studied extracts from cigarette smoke (CSE) and vapor from e-cigarettes (EVE) and heated tobacco (HTE) for their effects on vascular relaxation, endothelial nitric oxide signaling, and the activity of soluble guanylyl cyclase. The average nicotine concentrations of CSE, EVE, and HTE were 164, 800, and 85 µM, respectively. At a dilution of 1:3, CSE almost entirely inhibited the relaxation of rat aortas and porcine coronary arteries to acetylcholine and bradykinin, respectively, while undiluted EVE, with a 15-fold higher nicotine concentration, had no significant effect. With about 50% inhibition at 1:2 dilution, the effect of HTE was between CSE and EVE. Neither extract affected endothelium-independent relaxation to an NO donor. At the dilutions tested, CSE was not toxic to cultured endothelial cells but, in contrast to EVE, impaired NO signaling and inhibited NO stimulation of soluble guanylyl cyclase. Our results demonstrate that nicotine does not mediate the impaired endothelium-dependent vascular relaxation caused by smoking.
Similar content being viewed by others
Introduction
Cigarette smoking is an established risk factor for developing severe cardiovascular diseases, including atherosclerosis, coronary artery disease, and stroke1,2. The impaired function of vascular endothelial cells exposed to toxic compounds in tobacco smoke contributes significantly to the cardiovascular harm of smoking3. Vascular endothelial cells exert various protective effects, and dysfunction of these cells results in inflammation, activation of blood platelets, and vasoconstriction. Endogenous receptor agonists, such as acetylcholine, histamine or bradykinin, as well as increased blood flow trigger endothelium-dependent relaxation of blood vessels through stimulation of endothelial nitric oxide (NO) synthase (eNOS), resulting in NO-mediated activation of soluble guanylyl cyclase (sGC) and accumulation of 3′,5′-cyclic GMP (cGMP) in adjacent vascular smooth muscle cells4. Endothelium-dependent vasodilation of the brachial artery in response to increased blood flow, provoked by a short period of ischemia, can be measured noninvasively by ultrasound in laboratory animals and humans5. Using this flow-mediated dilation (FMD) approach and other techniques, numerous clinical studies provided evidence for pronounced endothelial dysfunction of chronic smokers3. It is conceivable that oxidative stress caused by smoking reduces the bioavailability of endothelium-derived NO through increased generation of superoxide and peroxynitrite formation6 or oxidation of the eNOS cofactor tetrahydrobiopterin7,8.
In the past decade, new nicotine products have become available, which allow users nicotine consumption without inhaling the smoke of burned tobacco. Electronic cigarettes (e-cigarettes) vaporize nicotine-containing liquids to generate aerosols with liquid droplets (“vapor”) that are inhaled by users9. While e-cigarettes do not contain tobacco, tobacco heating systems (THS) generate aerosols by heating tobacco sticks to a maximum 300 °C, a temperature below the threshold for combustion10. Since these alternative products do not generate toxic combustion products, users are exposed to lower levels of potentially hazardous substances than smokers11,12. Given the large body of evidence demonstrating reduced risks, these alternative nicotine products are recommended by health organizations as alternatives to smokers who are unable or unwilling to quit13.
Despite unequivocal evidence for their potential to reduce the harm of smoking, these new products are not entirely risk-free, and there is an ongoing debate about the regulatory measures required to protect adolescents and non-smokers from risks posed by e-cigarettes and THS. Moreover, besides referring to the potentially harmful effects of flavoring compounds, oxidation products of solvents formed in liquid vaporization, or toxicants extracted from heated tobacco, it has been emphasized that most smokers switching to these products will still consume comparable amounts of nicotine as they did before. Thus, sustained nicotine addiction and cardiovascular harm could still be an issue. In addition, although clinical studies showed that nicotine administered via patches or other medicinal products does not significantly increase the risk for severe cardiovascular disease14,15, a residual risk of nicotine inhalation with e-cigarettes or THS cannot be excluded16.
Considering the consistent results showing endothelial dysfunction of chronic smokers (for review, see Golbidi et al.3), clarifying whether nicotine contributes to this harmful effect of tobacco smoke appears essential. Several recent studies have addressed this issue using different experimental approaches, including FMD measurements of humans. Unfortunately, these studies did not provide consistent results. While some studies reported reduced FMD17,18,19,20 or impaired microvascular funtion21 by acute inhalation of nicotine-containing e-cigarette vapor, others observed no acute effects of nicotine inhalation22,23. Several studies have recently addressed the mid-term and long-term changes of FMD in smokers who replaced tobacco cigarettes with e-cigarettes with and without nicotine. George et al.24 showed that the endothelial function of smokers was significantly improved one month after replacing tobacco cigarettes by e-cigarettes with or without nicotine. Similar results were reported by Klonizakis et al.25, showing that the reduction of FMD persisted for at least six months in smokers who had either received nicotine replacement therapy or switched to e-cigarettes with or without nicotine. These observations were recently confirmed by the VAPing Observational Research Study-Endothelial Function (VAPORS-E) study data. Individuals who had exclusively used e-cigarettes for at least six months, the majority with nicotine according to cotinine plasma levels, did not differ significantly from non-users in their mean FMD26. Taken together, these results suggest that the chronic endothelial dysfunction of smokers is not caused by nicotine but by toxic constituents in the smoke of burned tobacco. However, Mohammadi et al. reported that chronic e-cigarette users and smokers had lower FMD than non-users27, indicating that this issue has not yet been fully settled.
The results reported with laboratory animals, isolated blood vessels, and cultured endothelial cells exposed to smoke or vapor are also controversial. While tobacco smoke extracts were consistently reported to cause vascular and endothelial dysfunction, presumably via increased oxidative stress28,29,30, the role of nicotine is less clear. Some studies reported impaired endothelial function in mice and rats exposed to nicotine-containing e-cigarette vapor31,32,33. In contrast to these findings, activating nicotinic receptors appears to cause NO release in the brain34, in renal blood vessels35, and in several types of human vascular endothelial cells36,37. In line with these observations, Zou et al.38 found that activation of nicotinic receptors contributes to acetylcholine-induced relaxation of rat aorta, and Mizrak et al.39 reported that the vasorelaxation to acetylcholine was significantly enhanced in rats fed for 12 months with nicotine in drinking water.
In the present study, we compared the effects of aqueous smoke extracts from Marlboro cigarettes (cigarette smoke extracts, CSE) with extracts of vapor generated by a popular e-cigarette device filled with a nicotine-containing liquid (20 mg/ml) (e-cigarette vapor extracts, EVE) or the aerosol emitted by a THS (heated tobacco extracts, HTE) on endothelium-dependent and -independent relaxation of rat aorta ex vivo. In addition, we studied NO/cGMP signaling and cytotoxicity in cultured endothelial cells and measured the NO-dependent and -independent activities of purified sGC in the presence of aerosol extracts. The potential scavenging of NO by the extracts was studied with a NO-sensitive electrode. We observed pronounced differences between CSE and EVE or HTE that did not correlate with measured nicotine concentrations, suggesting that nicotine does not significantly impair endothelial function ex vivo and in vitro.
Methods
Animals and tissue preparation
All animal experiments were performed in compliance with the Austrian law on experimentation with laboratory animals (last amendment 2013) based on the European Union guidelines for the Care and the Use of Laboratory Animals (European Union Directive 2010/63/EU) and are reported in accordance with the ARRIVE guidelines for reporting experiments involving animals40. The killing of animals solely for the use of their organs or tissues is explicitly excluded in Article 3 (page L276/39) of EU Directive 2010/63/EU on the protection of animals used for scientific purposes.
Sprague–Dawley rats (total number 15) of either sex were obtained from Charles River Laboratories (Sulzfeld, Germany) and housed at the local animal facility until they were used for the study at 16–20 weeks of age (body weight: 250–300 g). Rats were kept in approved conventional polycarbonate cages (Ehret, Emmerdingen, Germany), two to three animals per cage with dust-free laboratory bedding and enrichment (nesting material and rodent tunnels; from Abedd GmbH, Vienna, Austria). Animals were maintained at 23 ± 1 °C, with a relative humidity of 50–70% and kept on a regular 12-h dark/light cycle. Housing and care of the animals was according to the guidelines of the Austrian Federal Ministry of Science and Research and is periodically controlled by the authority. Rats were fed standard chow (Altromin 3023; obtained from Königshofer Futtermittel (Ebergassing, Austria)) and received water ad libitum. The animals were euthanized in a box gradually filled with CO2 until no more vital signs (cessation of respiration and circulation) were noticed. Subsequently, the thorax of the animals was opened, the thoracic aorta removed, cleaned from connective tissue, and used for assessment of vessel function. Aortas were randomly assigned to the different treatment protocols, with none excluded.
Porcine hearts were obtained from a local abattoir and immediately transported to the laboratory. The right coronary artery was carefully explanted, cleaned from connective tissue, and used to assess vessel function.
Preparation of aqueous extracts from tobacco cigarettes, THS and e-cigarettes
According to a published protocol41, aqueous extracts were obtained by passing cigarette smoke, e-cigarette vapor, or THS aerosol through 30 ml Dulbecco's Modified Eagle’s Medium (DMEM) supplemented with amphotericin B (1.25 µg/ml), penicillin (100 U/ml) and streptomycin (0.1 µg/ml) using a glass impinger. A rodent ventilator (Ugo Basile, Italy) connected to the glass impinger acted as a puffing machine to ensure a constant puffing regime (55 ml puff taken over 3 s in 30-s intervals, square wave puffing profile). For adequate comparison of the effects of the extracts, stroke rates, volume, and the length of tubing was kept consistent for all experimental protocols.
Based on recent sales data, showing that Marlboro is still the most popular cigarette brand42, commercially available Marlboro red cigarettes (0.8 mg nicotine, 10 mg tar, Philip Morris) were used to prepare CSE. Aqueous extracts were generated by passing 800 ml cigarette smoke through 30 ml DMEM.
The same setup was used to prepare aqueous EVE using an Eleaf iStick 50 W battery with Aspire Nautilus X 2 ml tanks and Nautilus X atomizer heads (1.8 Ohm; InnoCigs GmbH & Co KG, Germany) operated at 15.0 W. The battery was fully charged before use, and the tank was filled with pure unflavored e-liquid (i-steam; ROPA, Vienna, Austria) containing nicotine (20 mg/ml) in 50/50 (vol/vol.) glycerol/propylene glycol. E-cigarettes were activated by manually holding a button for 5 s in 5-s intervals. In order to achieve the same conditions as for preparing cigarette extracts, 800 ml of EVE was passed through 30 ml DMEM.
HTE was prepared with an IQOS 3 DUO (Philip Morris), equipped with commercially available tobacco sticks ("Heets", Siena Selection, red label, 0.5 mg nicotine; Philip Morris). To achieve the same vaping time and aerosol volume (800 ml) as for cigarettes and e-cigarettes, two Heets were used to prepare one extract. Passing cigarette smoke, e-cigarette vapor or THS aerosol through DMEM did not significantly affect pH values (pH 7.4 ± 0.2).
For HPLC analysis, sGC activity assays, and electrochemical NO measurements, the extracts were prepared in 50 mM triethanolamine buffer (TEA/HCl, pH 7.4), as DMEM interfered with these methods. For cell culture experiments, extracts were passed through sterile syringe filters (pore diameter 0.2 µm).
Determination of nicotine
The nicotine concentration of the extracts was determined using a 1260 Infinity HPLC System from Agilent equipped with a diode-array detector using a reversed-phase poroshell 120 EC-C18 column (4.6 × 50 mm, 2.7 µm). Elution was carried out isocratically using 70% of 20 mM phosphate buffer (pH 7.4), and 30% of methanol.
The extracts were passed through a syringe filter with 0.2 µm pore size, 10 µl aliquots were injected onto the column and separated at a flow rate of 1.0 ml/min at a column temperature of 25 °C. For quantification, calibration curves with a linear range from 0.003 to 0.3 mg/ml were established with analytical grade nicotine (Sigma, N5511) and analyzed based on the area of the peak detected at 260 nm (retention time 4.0 min).
Electrochemical determination of NO
Potential NO scavenging by aqueous extracts was tested with a nitric oxide sensor (ISO-NOP, World Precision Instruments, Berlin, Germany) connected to a TBR 4100 Free Radical Analyzer (World Precision Instruments). The sensor was calibrated daily with acidified nitrite as described previously43. Free NO radical was generated by incubation of 2-(N,N-diethylamino)-diazenolate-2-oxide diethylammonium salt (DEA/NO) at the indicated concentrations in 1 ml of 50 mM TEA/HCl buffer (pH 7.4), or the respective extract at 37 °C and monitored using LabChart 6 Software (ADInstruments, Version 6.1.3).
Isometric tension vasomotor studies
Rings with intact endothelium obtained from one vessel were preincubated in DMEM alone or different CSE, EVE, or HTE dilutions for 24 h at 37 °C and 5% CO2. Rings were randomly assigned to the different incubation protocols to avoid any systematic effects due to the repeated use of similar vessel segments. Rings were then suspended in 5-ml organ baths containing oxygenated Krebs–Henseleit buffer (concentrations in mM: NaCl 118.4, NaHCO3 25, KCl 4.7, KH2PO4 1.2, CaCl2 2.5, MgCl2 1.2, D-Glucose 11; pH 7.4), as previously described in detail44. After equilibration for 60 min at the optimal resting tension of 20 mN, maximal contractility was determined with a depolarizing solution containing 60 mM KCl. Rings that did not elicit adequate and stable contraction to high K+ were considered damaged and omitted from the study. Cumulative concentration–response curves to acetylcholine (1 nM–10 µM) or DEA/NO (1 nM–10 µM) were performed with rings that had been pre-contracted with 9,11-dideoxy-9α,11α-epoxy-methanoprostaglandin F2α (U-46619; ~ 90% of maximal contraction). To examine endothelial-dependent relaxation of porcine coronary arteries, concentration–response curves to bradykinin (0.1 nM–1 µM) in high K+ precontracted rings were carried out. Relaxation responses are expressed as percent reversal of U-46619 or K+-induced precontraction. Concentration–response curves of different ring segments from a single animal were averaged and counted as an individual experiment.
Cell culture
Porcine aortic endothelial cells (PAECs) were isolated as described45 and cultured at 37 °C, 5% CO2, and 80% humidity in DMEM containing 10% heat-inactivated fetal calf serum (FCS), penicillin (100 U/ml), streptomycin (0.1 mg/ml), and amphotericin (1.25 μg/ml). Cells were subcultured on 24-well plates to determine cGMP formation or on 6-well plates to analyze endothelial L-citrulline formation.
Determination of endothelial NOS activity and cGMP accumulation
NO synthase (NOS) activity was determined in PAECs by monitoring the conversion of L-[3H]arginine to L-[3H]citrulline as described46. Cells were preincubated with the extracts diluted in DMEM for 24 h at 37 °C and then assayed in 50 mM Tris buffer (pH 7.4) containing 100 mM NaCl, 5 mM KCl, 1 mM MgCl2, and 2.5 mM CaCl2. Preincubations were performed in the absence and presence of the non-selective NO synthase inhibitor NG-nitro-L-arginine (L-NNA; 1 mM). Reactions were started by the addition of L-[2,3,4,5-3H]arginine (~ 106 dpm) and the Ca2+-ionophore A23187 (1 μM) and terminated after 4 min by washing the cells with chilled incubation buffer. After lysis of the cells with 10 mM HCl (1 ml) for 1 h at ambient temperature, an aliquot (0.1 ml) was removed to determine incorporated radioactivity. The remaining sample was mixed with 200 mM sodium acetate buffer (pH 13.0) containing 10 mM L-citrulline (final pH ~ 5.0), and L-[3H]citrulline was separated from L-[3H]arginine by cation exchange chromatography, followed by determination of radioactivity by liquid scintillation counting.
Accumulation of intracellular cGMP was determined as described44. Cells were preincubated for 24 h at 37 °C with the extracts diluted in medium and then assayed in 50 mM Tris buffer (pH 7.4), containing 100 mM NaCl, 5 mM KCl, 1 mM MgCl2, 2.5 mM CaCl2, 1 mM 3-isobutyl-1-methylxanthine, and 1 μM indomethacin. Reactions were started by addition of A23187 or the NO donor DEA/NO (1 μM, each) in the absence and presence of 1 mM L-NNA and terminated after 4 min by removal of incubation medium, followed by cell lysis with 10 mM HCl for 1 h at ambient temperature and determination of released cGMP by radioimmunoassay.
Acute effects of CSE and EVE on eNOS activity were studied by incubating the cells for 15 min in the presence of the extracts under identical conditions with and without 1 mM L-NNA, followed by determination of L-[3H]arginine to L-[3H]citrulline conversion.
Determination of endothelial cell viability
Cell viability was assessed using the XTT Cell Proliferation Assay Kit (#10,010,200) from Cayman Chemical, purchased through Sanova Pharma GesmbH (Vienna, Austria). PAECs were seeded on 96-well plates and incubated for 24 h with the extracts diluted in DMEM, as indicated in the text and figure. Colorimetric reactions, based on the reduction of 2,3-bis-(2-methoxy-4-nitro-5-sulfophenyl)-2H-tetrazolium-5-carboxanilide (XTT) to a water-soluble formazan derivative by respiring cells, were carried out according to the manufacturer’s instructions. Absorbance was measured at 450 nm using a SPECTROstar® Nano microplate reader (BMG LABTECH GmbH, Ortenberg, Germany).
Determination of cGMP formation by purified sGC
Bovine lung sGC was purified as described47. The enzyme was incubated at 37 °C for 10 min in a final volume of 0.1 ml in the absence or presence of the extracts diluted as indicated in the figures. The final assay mixtures contained the extracts at 88% (vol/vol). The resulting final nicotine concentrations in undiluted EVE and CSE were 23.8 and 114.4 µg/ml, respectively. Assay mixtures contained 50 mM TEA/HCl buffer (pH 7.4), 0.5 mM [α-32P]GTP (∼200,000 cpm), 3 mM MgCl2, and 1 mM cGMP. Reactions were started by adding DEA/NO or cinaciguat at the indicated concentrations and terminated by adding 0.45 ml zinc acetate (120 mM) and 0.45 ml sodium bicarbonate (120 mM). After centrifugation (20,000×g at 4 °C for 10 min), supernatants were applied onto Al2O3 columns (acidified with 0.1 M HClO4). After washing the columns with distilled water, [32P]cGMP was eluted with sodium acetate (50 mM) and quantified by liquid scintillation counting. Blank values were measured in the absence of sGC.
Basal enzyme activity was determined without any stimulating agent (i.e., DEA/NO or cinaciguat). The activity of the oxidized enzyme was determined in the presence of 10 µM of the heme-oxidizing agent 1H-[1,2,4]oxadiazolo-[4,3-a]quinoxalin-1-one (ODQ)48. Heme-depleted sGC was generated by adding 0.5% (vol./vol.) Tween 20 during incubation49. The experiments with the activator cinaciguat were performed in the presence of 0.5% Tween 20.
To test for reversibility of effects caused by the extracts, sGC (50 ng) was preincubated in the absence or presence of the extracts for 5 min at 37 °C and then diluted 35-fold in the assay mixture. Reactions were started by addition of DEA/NO, and cGMP formation was determined as described above.
Randomization and blinding
Laboratory animals were randomly assigned to experiments. Porcine hearts were collected by slaughters of the abattoir, and the researcher had no influence on the selection of hearts. Experiments were not blinded in this study, as investigators were responsible for conducting and analyzing experiments. Blinding is not a usual procedure for this form of study and cannot be applied retrospectively. To reduce experimental bias, data analysis was not performed until the complete data set had been collected, and no complete recording was excluded.
Statistical analysis
Results are presented as mean values ± SEM of n experiments. Maximal effects (Emax and vmax) and half-maximal effective concentrations (EC50 values) were obtained by fitting concentration–response curves to a Hill-type model using Kaleidagraph (Synergy Software, version 4.5). EC50 values are reported as geometric means with 95% confidence limits. Paired Student’s t-test or analysis of variance (ANOVA) with Dunnett's post hoc test was used to compare groups using Kaleidagraph software. Significance was assumed at p < 0.05.
Results
Nicotine concentration of the aerosol extracts
The nicotine concentrations measured in the aqueous extracts prepared with the aerosols generated by tobacco cigarettes, e-cigarettes, and THS were 26.7 ± 0.9 µg/ml (164 ± 5.4 µM), 129.7 ± 26 µg/ml (800 ± 16 µM), and 13.8 ± 0.4 µg/ml (85 ± 2.3 µM), respectively (Table 1). These values agree well with previously published data obtained with the same protocol41. The vaporized volume of e-cigarette liquid (containing 20 mg of nicotine per ml) was 257 ± 0.18 µl (n = 3), corresponding to a theoretical nicotine concentration of 171 µg/ml in EVE (30 ml). Thus, about 25% of nicotine in the e-cigarette liquid was lost during the procedure, possibly due to partial decomposition or escape from the collecting fluid. Note that the nicotine concentrations of the undiluted extracts used in this study are about 1800- (CSE), 900- (HTE), and 4300-fold (EVE) higher than the average plasma concentration of chronic smokers, which is around 30 ng/ml50.
Effects of aerosol extracts on vascular relaxation
Rings with intact endothelium of rat aorta or porcine coronary arteries were preincubated for 24 h with aqueous extracts diluted as indicated in the figures, followed by recording concentration–response curves to the endothelium-dependent vasodilator acetylcholine or bradykinin, respectively. Endothelium-independent relaxation was induced with the NO donor DEA/NO.
Figure 1a shows that CSE impaired acetylcholine-induced relaxation of rat aorta by about 50% at 1:20 dilution and almost entirely inhibited vasodilation if the vessels had been preincubated with a 1:3 diluted extract. In contrast, even undiluted EVE had only very minor effects on relaxation to acetylcholine (Fig. 1b). HTE inhibited acetylcholine-induced relaxation but to a significantly lesser extent than CSE (Fig. 1c). The vasodilation caused by the NO donor DEA/NO was not affected by any of the extracts (Fig. 1d–f), suggesting that CSE and HTE specifically impair endothelium-dependent relaxation. The effects of the extracts on Emax and EC50 on relaxation of rat aortas in response to acetylcholine and DEA/NO are summarized in Table 2. While CSE in 1:20 dilution containing 1.35 µg/ml nicotine reduced Emax in response to acetylcholine to 58% of controls, undiluted EVE with a 100-fold higher nicotine concentration (130 µg/ml) had no significant effect. The effect of HTE was in between those of CSE and EVE. At 1:20 dilution, corresponding to 0.70 µg/ml nicotine, the extract had no effect but reduced Emax by about 50% at lower dilutions. Endothelium-independent vasodilation induced with the NO donor DEA/NO was not affected under any experimental condition. The lack of significant effects on acetylcholine potency (EC50 values) suggests non-competitive inhibition of endothelium-dependent relaxation by CSE and—to a lesser extent—by HTE.
Effects of aerosol extracts on relaxation of rat aortic rings to acetylcholine or DEA/NO. CSE (a) and HTE (c), but not EVE (b) impaired endothelial dependent relaxation. In contrast, endothelium-independent relaxation induced with the NO donor DEA/NO was not affected by CSE (d), EVE (e) or HTE (f). Two rings from a single animal were averaged and counted as an individual experiment. Data are expressed as mean values ± SEM derived from 5 animals. For Statistics see Table 2.
Similar results were obtained with porcine coronary arteries. CSE inhibited relaxation induced by bradykinin, whereas EVE had no significant effect (Fig. 2 and Table 3). The relationship between maximal acetylcholine-induced relaxation and nicotine concentrations of the extracts shown in Fig. 3 demonstrates that the impaired vasodilation observed with CSE and HTE is not caused by nicotine but by other constituents in the aerosols of burned or heated tobacco.
Effects of aerosol extracts on relaxation of porcine coronary arteries to bradykinin. CSE (a) impaired endothelial dependent relaxation, whereas EVE (b) had no effect. Two rings from a single animal were averaged and counted as an individual experiment. Data are expressed as mean values ± SEM derived from 3 separate hearts. For statistics see Table 3.
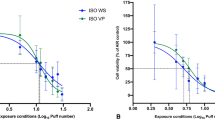
Endothelial cell viability
Potential cytotoxic effects of the extracts on endothelial cells were assessed with an established cell proliferation assay. Figure 4 shows the viability of PAECs which had been exposed for 24 h at 37 °C to aerosol extracts diluted as indicated in the figure. While EVE had no effect even if applied undiluted, CSE and HTE caused concentration-dependent cytotoxicity. Toxicity of undiluted CSE was close to the maximal cytotoxicity observed in the presence of Triton X-100. Since EVE had no effect despite at least tenfold higher nicotine concentration, the results demonstrate that the cytotoxic effects of extracts from burned or heated tobacco are not caused by nicotine.
Cytotoxic effects of aerosol extracts on cultured porcine aortic endothelial cells measured by XTT test. While EVE did not affect metabolic activity, even if applied undiluted, CSE and HTE reduced metabolic activity in a concentration-dependent manner. Triton X-100 (1%; TX) served as positive control. Data are expressed as percent of untreated controls and represent mean values ± SEM of 3–8 independent experiments performed in triplicate. *Indicates p < 0.05 (ANOVA with Dunnett’s post hoc test).
Endothelial NO/cGMP signaling
To mimic the experimental conditions of the isometric tension studies with isolated aortas, cultured endothelial cells were incubated for 24 h with the extracts, followed by determination of L-arginine-to-L-citrulline conversion and accumulation of cGMP in response to activation of endothelial NO synthase by the Ca2+ ionophore A23187. The non-selective NOS inhibitor L-NNA was used to control for basal L-citrulline and cGMP formation independent of eNOS activation by A23187. As shown in Fig. 5, EVE had no effect, whereas CSE and HTE caused various degrees of inhibition of NO/cGMP signaling. CSE and HTE inhibited eNOS activity measured as the formation of L-citrulline by about 30 and 50%, respectively (Fig. 5a). To test for direct effects on eNOS activity we measured L-citrulline formation by the cells incubated for 15 min with EVE or CSE. As shown in Fig. 5b, undiluted EVE significantly increased eNOS activity, while CSE caused a slight, non-significant inhibition of L-citrulline formation. Pure nicotine had no effect (0.2–1.6 mM; n = 3; data not shown), pointing to a non-specific effect of EVE, which was not further studied. The reduction in cGMP formation shown in Fig. 5c was much more pronounced, suggesting additional effects of the tobacco extracts downstream of NO synthesis. This assumption was tested by directly activating endothelial sGC with the NO donor DEA/NO. Figure 5d shows that 1:2 diluted CSE markedly inhibited cGMP formation in the presence of up to 0.3 µM DEA/NO, while inhibition was much less pronounced at higher concentrations of the NO donor. CSE increased the EC50 value of DEA/NO from 52 ± 15 to 447 ± 37 nM (calculated by forcing the curve through the maximum of the control). The observation that the degree of inhibition decreased with increasing NO concentrations most likely reflects the limited NO scavenging capacity of the extract (see Fig. 7a below). The results may partially explain the pronounced inhibition of A23187-induced cGMP accumulation shown in Fig. 5c.
Effects of aerosol extracts on NO/cGMP signaling in PAECs. (a) A23187-stimulated eNOS activity (measured as % conversion of L-arginine-to-L-citrulline) was significantly impaired by CSE and HTE after 24 h of preincubation, whereas EVE had no effect. L-NNA (1 mM) was used to control for eNOS-independent L-citrulline formation. Data represent mean values ± SEM of 6 independent experiments performed in triplicate. (b) Direct effects on A23187-induced eNOS activity were studied by preincubation of the cells for 15 min in the absence and presence of CSE or EVE. Undiluted EVE significantly increased eNOS activity, while CSE had no effect. Data represent mean values ± SEM of three independent experiments performed in triplicate. (c) A23187-stimulated cGMP formation measured by radioimmunoassay was significantly impaired in the presence of HTE and nearly abolished by CSE. Data represent mean values ± SEM of 3–7 independent experiments performed in triplicate. (d) Presence of CSE (1:2) caused a pronounced rightward shift of the DEA/NO concentration–response curve. Data represent mean values ± SEM of three independent experiments performed in triplicate. *Indicates p < 0.05 (ANOVA with Dunnett’s post hoc test).
Effects of CSE and EVE on the activity of purified sGC
The effects of CSE and EVE on sGC activity were studied with the purified enzyme. Figure 6a shows that undiluted EVE slightly reduced enzymatic cGMP formation in the presence of increasing concentrations of DEA/NO, but neither the reduction of vmax (from 11.1 ± 1.1 to 8.5 ± 1.0 µmol × min−1 × mg−1) nor the increase of the EC50 value (from 63.1 ± 2.5 to 107.3 ± 16 nM) were statistically significant (ANOVA with Dunnett’s post hoc test). In contrast, undiluted CSE almost completely inhibited sGC stimulation by DEA/NO, resulting in a reduction of vmax 1.4 ± 0.9 µmol × min−1 × mg−1 (~ 12% of control) and an increase of EC50 to 145.5 ± 30.4 nM (2.3-fold vs. control). The effect of CSE was concentration-dependent (Fig. 6b), fully reversible (Fig. 6c), and almost completely prevented in the presence of 0.5 mg/ml BSA (Fig. 6d).
Effects of aerosol extracts on purified sGC. The formation of cGMP was measured in the absence or presence of the extracts. (a) CSE caused almost complete inhibition of DEA/NO-stimulated enzyme activity, whereas the effect of EVE was much less pronounced. (b) The inhibition caused by CSE shown in panel (a) was concentration-dependent. (c) Preincubation experiments revealed that inhibition of sGC by the extracts was fully reversed by dilution of the CSE-exposed enzyme. (d) The presence of BSA (0.5 mg/ml) prevented the inhibition caused by CSE. (e) Basal enzyme activity (measured in the absence of DEA/NO) was not affected by the extracts (control). In addition, the extracts had no significant effects on the activity of the enzyme oxidized with ODQ or heme-depleted with Tween 20. (f) The extracts did not affect cGMP formation by Tween 20-treated sGC in the presence of the NO-independent heme-site activator cinaciguat. Data are expressed as mean values ± SEM derived from 3 independent experiments. *Indicates p < 0.05 in paired Student’s t-test (d), or ANOVA with Dunnett’s post hoc test vs. control (b) or vs. buffer/buffer control (c), respectively.
Basal sGC activity measured in the absence of DEA/NO was not affected by any of the three extracts. Similarly, the extracts had no effects on the activity of heme-free or oxidized sGC, measured in the presence of Tween 20 and ODQ, respectively (Fig. 6e), or the cinaciguat-activated enzyme (Fig. 6f). Taken together, these data suggest that CSE interferes with the NO stimulation of sGC.
Correlation of sGC activity with NO release from DEA/NO
Figure 7a shows the peak concentrations of NO released from 1, 3, and 10 µM DEA/NO in the absence and presence of EVE and CSE. The extracts had no detectable effects at high DEA/NO concentrations (3 and 10 µM), but NO released from 1 µM DEA/NO was significantly scavenged by CSE (from 1.36 ± 0.1 to 0.49 ± 0.08 µM, corresponding to 36% of control). Scavenging was reduced but not prevented in the presence of 0.5 mg/ml BSA (63% of control). Limited electrode sensitivity precluded reliable NO release measurements from lower DEA/NO concentrations. The correlation of sGC activity with NO release measured under identical conditions (Fig. 7b) illustrates the pronounced inhibition of NO-stimulated sGC by CSE.
Effects of aerosol extracts on NO release from DEA/NO. Peak concentrations of released NO were measured with a Clark-type electrode in the absence or presence of EVE and CSE. (a) CSE significantly reduced maximal NO concentration released from 1 µM DEA/NO, whereas EVE had no effect. Neither of the extracts affected NO release from 3 and 10 µM DEA/NO. (b) The correlation of sGC activity with measured NO peak concentrations under identical conditions shows that CSE caused pronounced inhibition of NO-stimulated sGC beyond NO scavenging. Data are expressed as mean values ± SEM from three independent experiments. *Indicates p < 0.05 in ANOVA with Dunnett’s post hoc test.
Discussion
The present study unequivocally demonstrates that the inhibition of agonist-induced endothelium-dependent relaxation, which has been consistently observed with inhaled tobacco smoke3, is not mediated by nicotine. CSE significantly inhibited the relaxation of aortas and coronary arteries to acetylcholine and bradykinin, respectively, whereas EVE had no effect despite much higher nicotine concentrations. The finding that CSE did not affect relaxation induced by DEA/NO indicates that tobacco smoke constituents specifically impair endothelium-dependent vasodilation. Furthermore, pronounced inhibition was observed with CSE diluted to a concentration tenfold lower than the threshold of cytotoxicity (1:20 vs. 1:2), suggesting interference with agonist-induced NO/cGMP signaling in endothelial cells rather than a non-specific toxic effect.
The observation that CSE impaired agonist-induced relaxation without affecting the response to DEA/NO is in apparent conflict with the results obtained with cultured endothelial cells and purified sGC. The activity of eNOS, measured as L-arginine-to-L-citrulline conversion in response to stimulation of the cells with A23187, was inhibited by about 50% in the presence of CSE diluted 1:2, while the extract caused virtually complete inhibition of vascular relaxation at 1:3 dilution (cf. Figures 1a and 5a). When we tested the acute effects of the extract on endothelial cells, we observed a similar tendency of inhibition of L-citrulline formation, but the effects were not statistically significant (see Fig. 5b).
Endothelial cGMP accumulation in response to A23187 or low concentrations of DEA/NO (up to 30 nM) was abolished by CSE at 1:2 dilution (see Fig. 5, panels c and d). Similarly, the activity of DEA/NO-stimulated sGC was inhibited in a concentration-dependent manner by CSE (see Fig. 6b). In comparison, the extract had no significant effect on DEA/NO-induced vasodilation (Fig. 1b). Since basal sGC activity (measured in the absence of added DEA/NO) was not inhibited by CSE and the extract had no effect on the cinaciguat-stimulated or heme-free enzyme (see Fig. 6, panels e and f), the extract apparently interferes with the stimulation of sGC by NO. The protective effect of BSA (see Fig. 6d) suggests that CSE causes reversible oxidative modification of the enzyme, but NO scavenging (Fig. 7) may additionally contribute to the observed effect. Taken together, these data suggest that inhibition of sGC by constituents of tobacco smoke results in impaired NO stimulation in endothelial cells, while the enzyme is protected from this modification in smooth muscle cells by a protein acting like BSA, which was used as an experimental model protein to protect sGC.
The most relevant information on the effects of e-cigarette vapor on endothelium-dependent vasodilation is provided by in vivo measurements of FMD upon acute inhalation or chronic use of aerosols generated by tobacco cigarettes, e-cigarettes, or THS. There is conclusive evidence that FMD is significantly reduced in chronic smokers7,51,52. Improvement of FMD by supplementation with antioxidants7,53 indicates that the endothelial dysfunction of smokers may be caused by vascular oxidative stress, resulting in reduced bioavailability of endothelium-derived NO. The widespread use of e-cigarettes as alternative nicotine sources has raised the question of whether nicotine contributes to this effect. The rapid reversal of impaired FMD in smokers switching to nicotine-containing e-cigarettes24,25 and identical FMD of e-cigarette users and non-users26 appears to exclude nicotine causing chronic damage to the endothelium, but several studies reported an acute reduction of FMD after short-term e-cigarette use17,18,19,20. The issue is further complicated by some reports showing that inhaled e-cigarette vapor caused an acute reduction of FMD even in the absence of nicotine20,54,55. These findings may reflect vascular oxidative stress caused by aerosol inhalation. However, while it is conceivable that inhaled propylene glycol, glycerol, or flavorings affect the function of lung epithelial cells, effects on blood vessels are not particularly plausible. Recently, it was reported that the inhalation of inert carbon nanoparticles impaired FMD to a similar degree as aerosols from cigarettes, e-cigarettes, or HTS56. As bilateral cervical vagotomy blocked this effect in rats, airway irritation appears to trigger vagus nerve signaling, resulting in endothelial dysfunction. The authors conclude that there is no single constituent or class of constituents responsible for acute impairment of endothelial function caused by aerosol inhalation56. These findings may at least partially explain the divergent results on acute vs. long-term effects of aerosol inhalation and agree well with our conclusion that the impaired vasodilation caused by tobacco smoke is not mediated by nicotine.
The effects of HTE were between those of EVE and CSE concerning impaired agonist-induced vasodilation, inhibition of eNOS activity, endothelial cGMP accumulation, and cytotoxicity. Our results agree well with studies comparing the emissions and health risks of e-cigarettes and THS (for a comprehensive review, see Murkett et al.57), suggesting that heating tobacco results in partial extraction of toxic compounds, which mediate the observed effects on endothelial NO/cGMP signaling. Some studies reported that aerosols from heated tobacco cause endothelial dysfunction, measured as FMD, to a similar degree as tobacco smoke in acutely exposed rats58 and chronic smokers59,60. We observed a significant inhibition of acetylcholine-induced relaxation of rat aortic rings. However, the effect was less pronounced than that of CSE despite much higher nicotine concentrations (see Table 2). Figure 3 illustrates that the nicotine concentration of the extracts does not correlate with maximal inhibition of vasorelaxation, further confirming that the effect is not caused by nicotine.
Limitations of the study
We tested extracts prepared from the different aerosols, but the properties of extracts do not necessarily reflect the properties of the aerosols that users inhale. In addition, it should be considered that we used only one type of vaporizer under defined conditions. Extracts from aerosols generated with other devices operating at different power levels could exert distinct biological effects.
Another limitation is the focus on endothelium-dependent relaxation and NO/cGMP signaling. Since impaired vasodilation is only one of several hallmarks of endothelial dysfunction, our results do not exclude other detrimental effects of inhaled nicotine on endothelial cell function. Besides its role in vasodilation, the endothelium inhibits platelet adhesion and aggregation, regulates inflammatory processes, is essential for capillary integrity, and promotes angiogenesis through cell migration. There is general agreement that the inhalation of tobacco smoke negatively affects these biological processes3, but the role of nicotine is controversial concerning angiogenesis/cell migration61,62,63, endothelial barrier function64,65, and platelet activation66,67,68. There is conclusive evidence that inhalation of e-cigarette vapor increases markers of oxidative stress and inflammation19,20, but e-cigarettes induce substantially less pronounced biological responses than tobacco smoke69, and a recent cross-sectional study found no differences in the levels of inflammatory markers between e-cigarette users and non-users26. Nevertheless, we wish to emphasize that e-cigarette vapor contains potentially toxic compounds besides nicotine, which may affect the function of vascular endothelial cells if efficiently resorbed into the systemic circulation. Further work is warranted to clarify this issue.
Data availability
The original data generated in this study will be made freely available in the Zenodo repository (https://zenodo.org/deposit/7963137).
References
Burns, D. M. Epidemiology of smoking-induced cardiovascular disease. Prog. Cardiovasc. Dis. 46, 11–29. https://doi.org/10.1016/S0033-0620(03)00079-3 (2003).
Benowitz, N. L. & Liakoni, E. Tobacco use disorder and cardiovascular health. Addiction https://doi.org/10.1111/add.15703 (2021).
Golbidi, S., Edvinsson, L. & Laher, I. Smoking and endothelial dysfunction. Curr. Vas. Pharmacol. 18, 1–11. https://doi.org/10.2174/1573403X14666180913120015 (2020).
Mayer, B. & Hemmens, B. Biosynthesis and action of nitric oxide in mammalian cells. Trends. Biochem. Sci. 22, 477–481 (1997).
Harris, R. A., Nishiyama, S. K., Wray, D. W. & Richardson, R. S. Ultrasound assessment of flow-mediated dilation. Hypertension 55, 1075–1085. https://doi.org/10.1161/HYPERTENSIONAHA.110.150821 (2010).
Landmesser, U., Harrison, D. G. & Drexler, H. Oxidant stress—a major cause of reduced endothelial nitric oxide availability in cardiovascular disease. Eur. J. Clin. Pharmacol. 62, 13–19. https://doi.org/10.1007/s00228-005-0012-z (2006).
Heitzer, T. et al. Tetrahydrobiopterin improves endothelium-dependent vasodilation in chronic smokers—evidence for a dysfunctional nitric oxide synthase. Circ. Res. 86, E36–E41. https://doi.org/10.1161/01.res.86.2.e36 (2000).
Taylor, B. A., Zaleski, A. L., Dornelas, E. A. & Thompson, P. D. The impact of tetrahydrobiopterin administration on endothelial function before and after smoking cessation in chronic smokers. Hypertens. Res. 39, 144–150. https://doi.org/10.1038/hr.2015.130 (2016).
Breland, A. et al. Electronic cigarettes: what are they and what do they do?. Ann. NY Acad. Sci. 1394, 5–30. https://doi.org/10.1111/nyas.12977 (2017).
Baker, R. R. Smoke generation inside a burning cigarette: modifying combustion to develop cigarettes that may be less hazardous to health. Prog. Energy Combust. Sci. 32, 373–385. https://doi.org/10.1016/j.pecs.2006.01.001 (2006).
Haziza, C. et al. Reduction in exposure to selected harmful and potentially harmful constituents approaching those observed upon smoking abstinence in smokers switching to the Menthol Tobacco heating system 2.2 for 3 months (Part 1). Nicotine Tob. Res. 22, 539–548. https://doi.org/10.1093/ntr/ntz013 (2020).
Haziza, C. et al. Favorable changes in biomarkers of potential harm to reduce the adverse health effects of smoking in smokers switching to the Menthol Tobacco Heating System 2.2 for 3 months (Part 2). Nicotine Tob. Res. 22, 549–559. https://doi.org/10.1093/ntr/ntz084 (2020).
Britton, J., Arnott, D., McNeill, A. & Hopkinson, N. Nicotine without smoke—putting electronic cigarettes in context. BMJ 353, i1745. https://doi.org/10.1136/bmj.i1745 (2016).
Benowitz, N. L. et al. Cardiovascular safety of varenicline, bupropion, and nicotine patch in smokers: a randomized clinical trial. JAMA Intern. Med. 178, 622–631. https://doi.org/10.1001/jamainternmed.2018.0397 (2018).
La Rosa, G., Vernooij, R., Qureshi, M., Polosa, R. & O’Leary, R. Clinical testing of the cardiovascular effects of e-cigarette substitution for smoking: a living systematic review. Intern. Emerg. Med. https://doi.org/10.1007/s11739-022-03161-z (2023).
Price, L. R. & Martinez, J. Cardiovascular, carcinogenic and reproductive effects of nicotine exposure: a narrative review of the scientific literature. F1000Res 8, 1586. https://doi.org/10.12688/f1000research.20062.2 (2020).
Carnevale, R. et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest 150, 606–612. https://doi.org/10.1016/j.chest.2016.04.012 (2016).
Chaumont, M. et al. Differential effects of e-cigarette on microvascular endothelial function, arterial stiffness and oxidative stress: a randomized crossover trial. Sci. Rep. https://doi.org/10.1038/s41598-018-28723-0 (2018).
Kuntic, M. et al. Short-term e-cigarette vapour exposure causes vascular oxidative stress and dysfunction: evidence for a close connection to brain damage and a key role of the phagocytic NADPH oxidase (NOX-2). Eur. Heart J. 41, 2472-2483A. https://doi.org/10.1093/eurheartj/ehz772 (2020).
Chatterjee, S. et al. Acute e-cig inhalation impacts vascular health: a study in smoking naïve subjects. Am. J. Physiol. 320, H144–H158. https://doi.org/10.1152/AJPHEART.00628.2020 (2021).
Ben Taleb, Z. et al. Pod-based e-cigarettes versus combustible cigarettes: the impact on peripheral and cerebral vascular function and subjective experiences. Tob Induc Dis 21, 71. https://doi.org/10.18332/tid/162366 (2023).
Cossio, R., Cerra, Z. A. & Tanaka, H. Vascular effects of a single bout of electronic cigarette use. Clin. Exp. Pharmacol. Physiol. 47, 3–6. https://doi.org/10.1111/1440-1681.13180 (2020).
Haptonstall, K. P. et al. Differential effects of tobacco cigarettes and electronic cigarettes on endothelial function in healthy young people. Am. J. Physiol. 319, H547–H556. https://doi.org/10.1152/ajpheart.00307.2020 (2020).
George, J. et al. Cardiovascular effects of switching from tobacco cigarettes to electronic cigarettes. J. Am. Coll. Cardiol. 74, 3112–3120. https://doi.org/10.1016/j.jacc.2019.09.067 (2019).
Klonizakis, M., Gumber, A., McIntosh, E. & Brose, L. S. Medium- and longer-term cardiovascular effects of e-cigarettes in adults making a stop-smoking attempt: a randomized controlled trial. BMC Med. 20, 276. https://doi.org/10.1186/s12916-022-02451-9 (2022).
Boakye, E. et al. Examining the association of habitual e-cigarette use with inflammation and endothelial dysfunction in young adults: the VAPORS-Endothelial function study. Tob. Induc. Dis. 21, 75. https://doi.org/10.18332/tid/162327 (2023).
Mohammadi, L. et al. Chronic E-cigarette use impairs endothelial function on the physiological and cellular levels. Arterioscler. Thromb. Vasc. Biol. 42, 1333–1350. https://doi.org/10.1161/Atvbaha.121.317749 (2022).
Shimosato, T., Geddawy, A., Tawa, M., Imamura, T. & Okamura, T. Chronic administration of nicotine-free cigarette smoke extract impaired endothelium-dependent vascular relaxation in rats via increased vascular oxidative stress. J. Pharmacol. Sci. 118, 206–214. https://doi.org/10.1254/jphs.11187fp (2012).
Teasdale, J. E., Newby, A. C., Timpson, N. J., Munafò, M. R. & White, S. J. Cigarette smoke but not electronic cigarette aerosol activates a stress response in human coronary artery endothelial cells in culture. Drug Alcohol Depend. 163, 256–260. https://doi.org/10.1016/j.drugalcdep.2016.04.020 (2016).
Horinouchi, T., Mazaki, Y., Terada, K. & Miwa, S. Cigarette smoke extract and its cytotoxic factor acrolein inhibit nitric oxide production in human vascular endothelial cells. Biol. Pharm. Bull. 43, 1804–1809. https://doi.org/10.1248/bpb.b20-00522 (2020).
Rao, P., Liu, J. & Springer, M. L. JUUL and combusted cigarettes comparably impair endothelial function. Tobacco Reg. Sci. 6, 30–37. https://doi.org/10.18001/TRS.6.1.4 (2020).
El-Mahdy, M. A. et al. Long-term electronic cigarette exposure induces cardiovascular dysfunction similar to tobacco cigarettes: role of nicotine and exposure duration. Am. J. Physiol. 320, H2112–H2129. https://doi.org/10.1152/ajpheart.00997.2020 (2021).
El-Mahdy, M. A. et al. Electronic cigarette exposure causes vascular endothelial dysfunction due to NADPH oxidase activation and eNOS uncoupling. Am. J. Physiol. 322, H549–H567. https://doi.org/10.1152/ajpheart.00460.2021 (2022).
Di Matteo, V. et al. Critical role of nitric oxide on nicotine-induced hyperactivation of dopaminergic nigrostriatal system: electrophysiological and neurochemical evidence in rats. CNS Neurosci. Ther. 16, 127–136. https://doi.org/10.1111/j.1755-5949.2010.00136.x (2010).
El-Mas, M. M., El-Gowilly, S. M., Gohar, E. Y. & Ghazal, A. R. M. Pharmacological characterization of cellular mechanisms of the renal vasodilatory effect of nicotine in rats. Eur. J. Pharmacol. 588, 294–300. https://doi.org/10.1016/j.ejphar.2008.04.048 (2008).
Wu, J. C. et al. Cholinergic modulation of angiogenesis: role of the α7 nicotinic acetylcholine receptor. J. Cell. Biochem. 108, 433–446. https://doi.org/10.1002/jcb.22270 (2009).
Park, H. S., Cho, K., Park, Y. J. & Lee, T. Chronic nicotine exposure attenuates proangiogenic activity on human umbilical vein endothelial cells. J. Cardiovasc. Pharmacol. 57, 287–293 (2011).
Zou, Q., Leung, S. W. S. & Vanhoutte, P. M. Activation of nicotinic receptors can contribute to endothelium-dependent relaxations to acetylcholine in the rat aorta. J. Pharmacol. Exp. Ther. 341, 756–763. https://doi.org/10.1124/jpet.112.192229 (2012).
Mizrak, S., Göksel Ülker, S., Ercan, G. & Sönmez, B. The effect of long term nicotine exposure on endothelial function in rats. Drug. Chem. Toxicol. https://doi.org/10.1080/01480545.2020.1845714 (2020).
Percie du Sert, N. et al. Reporting animal research: explanation and elaboration for the ARRIVE guidelines 2.0. PLoS Biol. 18, e3000411. https://doi.org/10.1371/journal.pbio.3000411 (2020).
Bozhilova, S. et al. Optimization of aqueous aerosol extract (AqE) generation from e-cigarettes and tobacco heating products for in vitro cytotoxicity testing. Toxicol. Lett. 335, 51–63. https://doi.org/10.1016/j.toxlet.2020.10.005 (2020).
Tobacco Brand Preferences, <https://www.cdc.gov/tobacco/data_statistics/fact_sheets/tobacco_industry/brand_preference/index.htm> (2017).
Mayer, B., Klatt, P., Werner, E. R. & Schmidt, K. Kinetics and mechanism of tetrahydrobiopterin-induced oxidation of nitric oxide. J. Biol. Chem. 270, 655–659 (1995).
Wölkart, G. et al. Effects of flavoring compounds used in electronic cigarette refill liquids on endothelial and vascular function. PLoS ONE 14, e0222152. https://doi.org/10.1371/journal.pone.0222152 (2019).
Schmidt, K., Mayer, B. & Kukovetz, W. R. Effect of calcium on endothelium-derived relaxing factor formation and cGMP levels in endothelial cells. Eur. J. Pharmacol. 170, 157–166 (1989).
Schmidt, K., Werner-Felmayer, G., Mayer, B. & Werner, E. R. Preferential inhibition of inducible nitric oxide synthase in intact cells by the 4-amino analogue of tetrahydrobiopterin. Eur. J. Biochem. 259, 25–31 (1999).
Russwurm, M. & Koesling, D. Purification and characterization of NO-sensitive guanylyl cyclase. Methods Enzymol. 396, 492–501 (2005).
Schrammel, A., Behrends, S., Schmidt, K., Koesling, D. & Mayer, B. Characterization of 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one as a heme-site inhibitor of nitric oxide-sensitive guanylyl cyclase. Mol. Pharmacol. 50, 1–5 (1996).
Kollau, A. et al. Irreversible activation and stabilization of soluble guanylate cyclase by the protoporphyrin IX mimetic cinaciguat. Mol. Pharmacol. 93, 73–78. https://doi.org/10.1124/mol.117.109918 (2018).
Hukkanen, J., Jacob, P. III. & Benowitz, N. L. Metabolism and disposition kinetics of nicotine. Pharmacol. Rev. 57, 79–115. https://doi.org/10.1124/pr.57.1.3 (2005).
Zeiher, A. M., Schachinger, V. & Minners, J. Long-term cigarette smoking impairs endothelium-dependent coronary arterial vasodilator function. Circulation 92, 1094–1100. https://doi.org/10.1161/01.cir.92.5.1094 (1995).
Celermajer, D. S. et al. Cigarette smoking is associated with dose-related and potentially reversible impairment of endothelium-dependent dilation in healthy young adults. Circulation 88, 2149–2155. https://doi.org/10.1161/01.CIR.88.5.2149 (1993).
Heitzer, T., Just, H. & Münzel, T. Antioxidant vitamin C improves endothelial dysfunction in chronic smokers. Circulation 94, 6–9 (1996).
Caporale, A. et al. Acute effects of electronic cigarette aerosol inhalation on vascular function detected at quantitative MRI. Radiology 293, 97–106. https://doi.org/10.1148/radiol.2019190562 (2019).
Burrage, E. N. et al. Long-term cerebrovascular dysfunction in the offspring from maternal electronic cigarette use during pregnancy. Am. J. Physiol. Heart Circ. Physiol. 321, 339–352. https://doi.org/10.1152/ajpheart.00206.2021 (2021).
Nabavizadeh, P. et al. Impairment of endothelial function by cigarette smoke is not caused by a specific smoke constituent, but by vagal input from the airway. Arterioscler. Thromb. Vasc. Biol. 42, 1324–1332. https://doi.org/10.1161/ATVBAHA.122.318051 (2022).
Murkett, R., Rugh, M. & Ding, B. Nicotine products relative risk assessment: an updated systematic review and meta-analysis. F1000Res 9, 1225. https://doi.org/10.12688/f1000research.26762.2 (2022).
Nabavizadeh, P. et al. Vascular endothelial function is impaired by aerosol from a single IQOS HeatStick to the same extent as by cigarette smoke. Tob. Control 27, s13–s19. https://doi.org/10.1136/tobaccocontrol-2018-054325 (2018).
Loffredo, L. et al. Impact of chronic use of heat-not-burn cigarettes on oxidative stress, endothelial dysfunction and platelet activation: the SUR-VAPES chronic study. Thorax 76, 618–620. https://doi.org/10.1136/thoraxjnl-2020-215900 (2021).
Rao, P. et al. Comparable impairment of vascular endothelial function by a wide range of electronic nicotine delivery devices. Nicotine Tob. Res. 24, 1055–1062. https://doi.org/10.1093/ntr/ntac019 (2022).
Liu, Z. Y. et al. Flavored and nicotine-containing e-cigarettes induce impaired angiogenesis and diabetic wound healing via increased endothelial oxidative stress and reduced NO bioavailability. Antioxidants-Basel https://doi.org/10.3390/antiox11050904 (2022).
Taylor, M. et al. A comparative assessment of e-cigarette aerosols and cigarette smoke on in vitro endothelial cell migration. Toxicol. Lett. 277, 123–128. https://doi.org/10.1016/j.toxlet.2017.06.001 (2017).
Giebe, S. et al. Comparative study of the effects of cigarette smoke versus next generation tobacco and nicotine product extracts on endothelial function. Redox Biol. https://doi.org/10.1016/j.redox.2021.102150 (2021).
Naik, P. et al. Oxidative and pro-inflammatory impact of regular and denicotinized cigarettes on blood brain barrier endothelial cells: Is smoking reduced or nicotine-free products really safe?. BMC Neurosci. 15, 51. https://doi.org/10.1186/1471-2202-15-51 (2014).
Heldt, N. A., Reichenbach, N., McGary, H. M. & Persidsky, Y. Effects of electronic nicotine delivery systems and cigarettes on systemic circulation and blood-brain barrier. Implications for cognitive decline. Am. J. Pathol. 191, 243–255. https://doi.org/10.1016/j.ajpath.2020.11.007 (2021).
Ljungberg, L. U., Persson, K., Eriksson, A. C., Green, H. & Whiss, P. A. Effects of nicotine, its metabolites and tobacco extracts on human platelet function in vitro. Toxicol. in Vitro 27, 932–938. https://doi.org/10.1016/j.tiv.2013.01.004 (2013).
Hom, S. et al. Platelet activation, adhesion, inflammation, and aggregation potential are altered in the presence of electronic cigarette extracts of variable nicotine concentrations. Platelets 27, 694–702. https://doi.org/10.3109/09537104.2016.1158403 (2016).
Mobarrez, F., Antoniewicz, L., Hedman, L., Bosson, J. A. & Lundback, M. Electronic cigarettes containing nicotine increase endothelial and platelet derived extracellular vesicles in healthy volunteers. Atherosclerosis 301, 93–100. https://doi.org/10.1016/j.atherosclerosis.2020.02.010 (2020).
Szostak, J. et al. A 6-month systems toxicology inhalation study in ApoE(-/-) mice demonstrates reduced cardiovascular effects of E-vapor aerosols compared with cigarette smoke. Am. J. Physiol. 318, H604–H631. https://doi.org/10.1152/ajpheart.00613.2019 (2020).
Acknowledgements
The authors thank Heike Stessel and Evamaria Imp for helpful technical assistance and the Austrian Science Fund (FWF) for financial support (Grant P32922).
Author information
Authors and Affiliations
Contributions
A.K. performed experiments, analyzed data, and contributed to preparation of the manuscript; G.W. performed experiments, analyzed data, and contributed to preparation of the manuscript; M.R. provided essential materials and contributed to data analysis; D.K. provided essential materials and contributed to data analysis; A.S. supervised experiments, analyzed data, prepared figures, and contributed to preparation of the manuscript; B.M. supervised the study and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wölkart, G., Kollau, A., Russwurm, M. et al. Varied effects of tobacco smoke and e-cigarette vapor suggest that nicotine does not affect endothelium-dependent relaxation and nitric oxide signaling. Sci Rep 13, 15833 (2023). https://doi.org/10.1038/s41598-023-42750-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42750-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.