Abstract
The relationship between Helicobacter pylori infection and rheumatoid arthritis has been investigated, but the results remain controversial. This study aims to determine the association between the two diseases via a 17-year retrospective cohort study. Using the National Health Insurance Research Database, a nationwide population based in Taiwan, we identified 97,533 individuals with H. pylori infection and matched controls between 2000 and 2017 using propensity score matching at a 1:1 ratio. The adjusted hazard ratio of rheumatoid arthritis was determined by multiple Cox regression. The incidence rate of rheumatoid arthritis was 1.28 per 10,000 person-months in the H. pylori cohort, with a higher risk compared to the control group. In the < 30 years old subgroup, the risk was highest, especially in women < 30 years old with H. pylori infection. Patients with < 1 year follow-up showed 1.58 times higher susceptibility to rheumatoid arthritis. Individuals with follow-ups of 1–5 years and over 5 years demonstrated 1.43 and 1.44 times higher risks of rheumatoid arthritis, respectively. Our study showed H. pylori infection was associated with the development of rheumatoid arthritis. Clinicians should note higher risk, especially < 30 years old. More research needed to understand underlying mechanism.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune systemic inflammatory disorder that involves synovial joints primarily. The main clinical features of RA include the articular manifestations of swelling, pain, and stiffness in joints1,2. Failure to treat patients and late-stage disease states can destroy joints due to uncontrolled inflammation damage to cartilage and bone, eventually leading to joint deformities and disability; furthermore, various systemic and extraarticular complications could be significant and prominent3,4,5. However, the definitive cause of RA remains unknown. RA is theorized to develop when a genetically susceptible individual experiences an environmental stimulus such as exposure to infections that trigger an autoimmune reaction6,7,8.
Helicobacter pylori (H. pylori) is a gram-negative, spiral-shaped, flagellated, microaerophilic, extracellular bacterium, and is one of the most common chronic bacterial infections in humans9,10. Immune activation occurs after persistent H. pylori infection and is manifested by continuous cytokine signaling from epithelial cells and infiltration of gastric mucosa by neutrophils, macrophages, lymphocytes, and the generation of antibodies and effector T cells with both Th1 and Th2 components11. Chronic H. pylori infection was found to be a source of persistent antigenic stimulation and experiments have shown that H. pylori infection is related to several autoimmune diseases involving alterations of gastric autoimmunity. These findings imply that RA may also have a similar pathogenesis12,13,14,15,16.
Although a few studies have been published reviewing the relationship between H. pylori infection and RA, some found a positive correlation, but others showed the opposite results13,14,17. Given the conflicting results regarding RA risk among H. pylori infection patients, and due to the challenge of various disabilities and systemic complications resulting from RA, as well as the need for early identification of RA, we were interested in determining the relationship between RA and H. pylori and any related factors. In this study, we investigated the relationship between H. pylori infection and RA by analyzing a nationwide, longitudinal population-based retrospective cohort in Taiwan.
Methods
Data source
The retrospective cohort study aims to investigate the relationship between H. pylori infection and RA. The flow diagram is displayed in Fig. 1. The Longitudinal Health Insurance Research Database (LHID) contains 2,000,000 individuals that are sampled randomly from the National Health Insurance Research Database (NHIRD), which is a national population-based insurance system enrolling over ninety-nine percent population in Taiwan and comprises medical data that date back to 199718,19. In addition, the LHID is a large and reliable database that has been extensively used in numerous studies published worldwide. Patients' diagnoses are documented following the International Classification of diseases, both the 9th (ICD-9-CM) and 10th Revision, Clinical Modification (ICD-10-CM). The LHID also involves demographic data, claims for hospital and hospital expenditures, and other patients’ clinical information. Propensity score matching was done for chosen variables to control the deviations to avoid confounding biases.
A large number of studies have been published using this database. All methodologies were executed in strict adherence to pertinent guidelines and regulations. This research was conducted in alignment with the principles outlined in the Declaration of Helsinki. The personal data of all participants underwent thorough de-identification throughout the study. Furthermore, the study was approved by the Chung Shan Medical University Hospital Institution Review Committee (IRB number CS1-20201) and informed consent is waved by the committee since retrospective nature of study.
Study population
We identified individuals who received a diagnosis of H. pylori infection spanning the years 2000 to 2017, employing the following criteria: H. pylori infection (ICD-9-CM: 041.86, ICD-10-CM: B96.81), gastrointestinal tract hemorrhage (ICD-9-CM: 578.9, ICD-10-CM: K92.0-92.2), or peptic ulcer (ICD-9-CM: 531–534; ICD-10-CM: K25-28), and had subsequently undergone H. pylori eradication therapy. Verification of H. pylori treatment was achieved through upper endoscopic and biopsy-based assessment, in adherence to the National Health Insurance system guidelines. This verification process encompassed histological evaluation, rapid urease testing, or biopsy culture. The administration of anti-H. pylori treatment encompassed both the standard triple therapy (consisting of H2 receptor antagonists or proton pump inhibitors, tetracycline or amoxicillin, and clarithromycin or metronidazole) and the bismuth-containing quadruple therapy. The application of the drug combination followed a consistent protocol lasting 1–2 weeks for H. pylori eradication10.
The index date, for the purpose of this study, was established as the earliest date of H. pylori infection diagnosis, gastrointestinal tract hemorrhage diagnosis, or peptic ulcer diagnosis. Exclusions from the study comprised patients with pre-existing medical histories of RA, cancer, or documented deaths prior to the index date, along with cases diagnosed before the year 2000, individuals who had previously received H. pylori eradication therapy prior to the index date, and instances where a suitable control, matched by propensity score, could not be identified.
The control cohort was comprised of individuals registered within the LHID who had not undergone anti-H. pylori treatment. To counterbalance the potential influence of confounding bias arising from comorbidities on the incidence of RA, control participants were subjected to a 1:1 propensity score-based matching process with H. pylori-infected patients, employing an 8-to-1 digit greedy matching algorithm. For the control group, the index date was harmonized with the corresponding matched cases. In this intricate process, a logistic regression model was deployed to predict the probability, incorporating variables such as age, sex, urbanization level, insurance type, and comorbidities within the year preceding the index date. Following the propensity score matching, the standardized differences in covariates between the two groups were revealed to be below 0.1, thus affirming a satisfactory balance between the cohorts. Ultimately, the analysis encompassed a total of 97,533 patients who underwent H. pylori eradication therapy, matched one-to-one with control individuals based on propensity scores, resulting in an equivalent number of participants in each group, namely 97,533.
Outcome and comorbidities
We identified RA patients by searching the ICD-9-CM code 714.0, and ICD-10-CM codes M05 and M06, and the RA diagnostic accuracy was determined by incorporating patients with a previous diagnosis code, which included at least one hospitalization or three outpatient visits. Comorbidities related to RA were listed. We selected the following comorbidities: hypertension, diabetes mellitus, hyperlipidemia, asthma, cerebrovascular disease, chronic pulmonary diseases, chronic kidney disease, chronic liver disease, pneumonia, osteoporosis, Sjogren’s syndrome, systemic lupus erythematosus (SLE), and ankylosing spondylitis. All comorbidities were defined by having at least hospitalization for one time or outpatient visits two times for a particular ICD code in 2 years prior to the index date. The comorbidities were applied as covariates in the multivariate analysis.
Statistical analysis
Descriptive statistics were harnessed to scrutinize the distribution of foundational characteristics. In order to mitigate the potential bias arising from measured factors, a meticulous 1:1 propensity score matching (PSM) was meticulously carried out, employing a method of greedy nearest-neighbor, non-replacement matching, with a precisely defined caliper width of 0.01. The assessment of disparities in covariates between the two cohorts was facilitated by the application of the absolute standardized difference (ASD). A value of ASD lower than 0.10 serves as an indicator of equilibrium in the characteristics of the studied groups20.
The incidence rate of study events, along with their corresponding 95% confidence intervals (CIs), was computed utilizing the normal approximation to the Poisson distribution. The cumulative probability of RA was evaluated through the utilization of Kaplan–Meier analysis21. The discernment of variations in Kaplan–Meier curves between the study groups was accomplished via a log-rank test. Employing Cox proportional hazard analysis, the estimation of the hazard ratio (HR) for RA was undertaken. This endeavor encompassed multifaceted Cox proportional hazard regression models, encompassing parameters such as age, sex, urbanization level, insurance type, and comorbidities.
Sensitivity analysis was conducted to explore the association between H. pylori infection and RA risk, stratified by follow-up time (within 0–12 months, 12–60 months, and beyond 60 months from the index date), as well as by sex and age. All statistical analyses were executed utilizing SAS software version 9.4. A significance level denoted by p < 0.05 was held as the threshold for statistical significance.
Ethics approval and consent to participate
The study was approved by the Chung Shan Medical University Hospital Institution Review Committee (IRB number CS1-20201). Since the large database contains over 2 million individuals, and all data derived from the LHID were de-identification, the consent to participants is not applicable.
Results
After employing propensity score matching, the distribution of selected parameters including index year, age, sex, urbanization, social status, insurance coverage, and comorbidities showed close balance between the two cohorts (Table 1). The average follow-up duration was approximately 126 months for individuals in the H. pylori group and 122 months for those in the control group. To assess the monthly incidence rates of RA, diagnoses were categorized by the month they were identified. The results demonstrated a significant difference in the incidence rate of RA between the two groups, with the H. pylori group experiencing a higher rate compared to the control group (1.28 vs. 0.89 per 10,000 person-months respectively, adjusted hazard ratio (aHR): 1.45, 95% confidence interval (CI) 1.34–1.56, Table 2).
Our findings, derived from the propensity score matched data, indicated that the risk of RA was notably elevated in the H. pylori infection group, extending to specific subgroups such as individuals with low socioeconomic status, women, the elderly, and patients with comorbidities like chronic kidney disease, chronic liver disease, osteoporosis, and other autoimmune disorders such as Sjogren’s syndrome, SLE, and ankylosing spondylitis (Table 3). Even after applying multivariate adjustment, the group with H. pylori infection still exhibited an increased risk of RA (aHR: 1.45, 95% CI 1.34–1.56, as shown in Table 3).
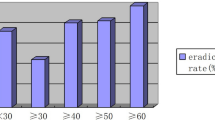
Further elaboration from sensitivity analysis indicated that patients below the age of 30, with H. pylori infection, exhibited a notably higher inclination towards RA (aHR: 2.19, 95% CI 1.41–3.38). Sequentially, the risk tendencies were observed in the 45–64 years age group (1.5 times higher risk), followed by the 30–44 years age group (1.4 times higher risk), and finally the ≥ 65 years age group (1.25 times higher risk). Additionally, it was noted that the highest RA risk occurred within the first year following H. pylori diagnosis (aHR: 1.58, 95% CI 1.26–1.99), with a subsequent risk of 1.43 within 1–5 years and 1.44 after 5 years, all of which displayed statistical significance (Table 4).
Upon delving into age-sex subgroup analysis (Table 5), the highest adjusted hazard ratio was evident among female patients under 30 years of age (2.22, 95% CI 1.26–3.91), followed by male patients of the same age category (2.12, 95% CI 1.07–4.20). To visually represent the cumulative probability of RA, Fig. 2 displayed the Kaplan–Meier curves.
Discussion
According to our study findings, the development of RA was statistically associated with H. pylori infection. The incidence rate of RA was significantly higher in the H. pylori-infected group than in the non-infected group during the follow-up interval, which ranged from the first year to more than 5 years. Intriguingly, the incidence rate of RA increased more significantly in patients with H. pylori infection under the age of 30, in both males and females. To date, this is the first and the largest cohort of a national, longitudinal, population-based dataset to reveal a higher risk of RA among H. pylori-infected patients. The epidemiological interpretation of this association might provide insight into the pathogenesis of RA. In addition, physicians should remain vigilant about the risk of RA in patients with H. pylori infection.
Genetic and environmental influences such as infections are believed to interact and trigger adaptive responses associated with autoimmunity and have been implicated in the development of RA22. H. pylori has been intensely studied over the past three decades to determine the characteristics involved in instigating host immunity that results in some autoimmune diseases. Various mechanisms have been proposed, including chronic inflammatory progress, polyclonal lymphocyte activation, molecular mimicry, superantigens, epitope spreading, bystander activation, endothelial cell damage, and highly immune-dominant virulence23,24.
The virulent factors of H. pylori in the development of autoimmune diseases have attracted widespread attention over the last two decades. According to the literature, H. pylori possesses several virulence factors. Two crucial markers of virulence have been widely researched in H. pylori, including vacuolating cytotoxin A (VacA), which leads to epithelial cell damage, and cytotoxin-associated gene A (CagA), which is translocated into the gastric epithelium, endowing it with an increased intensity of gastric inflammation by increasing the secretion of pro-inflammatory cytokines25,26,27,28. Several scholars have suggested that the relationships between the infectious agent and the autoimmunity response may differ depending on the virulence of the infecting strain. Infection with H. pylori CagA-positive strains was associated with more serious inflammatory reactions and an increase in the risk of adverse clinical consequences. H. pylori virulence factors had antigenic similarity with host proteins antigens and were involved in the development of autoimmune diseases through alternative intracellular signaling pathways, which modulated and dysregulated the host immune response13.
Hamed et al. investigated the effects of H. pylori’s existence and activity on RA disease activity. According to their results, patients with active RA (DAS-28 > 3.2) showed a higher positive rate of H. pylori stool antigen than patients in remission29. Ebrahimia et al. showed that RA patients who were H. pylori CagA-positive tended to have severe clinical manifestations with higher DAS-28 scores and higher mean VAS scores than CagA-negative patients. Furthermore, in their study, the laboratory indices of activity including rheumatoid factor (RF), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), anti-cyclic citrullinated peptide (Anti.CCP), and anti-mutated citrullinated vimentin (Anti-MCV) were significantly higher in patients with H. pylori-positive than in the negative patients30. A report by Zentilin et al. found similar findings that H. pylori-eradicated RA patients demonstrated obvious improvement over time in clinical parameters such as joint symptoms, functional ability, and progressive decreases in laboratory indices, such as ESR, CRP, and antinuclear antibody compared with H. pylori-negative RA patients31. That is, H. pylori infection might be one of the pathogenesis of RA. Whereas other studies demonstrated different trends. Nakamura et al. have shown that RA patients with H. pylori infection have lower values of rheumatoid factor compared with H. pylori-negative in RA patients32. Ishikawa et al. showed H. pylori infection was not associated with increased disease activity in patients with RA treated with NSAIDs33. Further prospective research with more participants is required to reach a definitive conclusion.
The correlation and mechanisms of H. pylori infection in the pathogenesis of RA are still controversial. Yamanishi et al. found that purified urease by H. pylori chronically stimulates splenic B cells in vitro, causing the production of antigen-specific conventional antibodies such as IgM-type rheumatoid factor34. Moreover, some research has reported that H. pylori induces antigen-stimulated T-cell activation and interferes with the maturation of dendritic cells, resulting in a tolerogenic phenotype. The initial steps of the autoimmune response in RA are likely to involve environmental triggers on mucosal surfaces, such as exposure to cigarette smoke in the airway, oral bacteria, specifically Porphyromonas gingivalis, resulting in periodontitis35,36, and even the gut microbiota37. Furthermore, a variety of investigations have attempted to elucidate the association between the gut microbiome and the development of RA38. Studies of stool samples and culture-independent microbiota have demonstrated significant enrichment of the Prevotellaceae bacterial family, especially Prevotella spp. in patients in pre-clinical stages of RA compared with controls, which demonstrates that the gastrointestinal microbiome may act as an environmental modulator that could dysregulate the autoimmune response, eventually leading to RA39.
The interaction of H. pylori with the gastrointestinal microbiome and its role in dysbiosis leading to the development of autoimmune arthritis have recently attracted much attention. It has been shown that H. pylori commonly colonizes and changes the microbiota in the upper gastrointestinal tract31,40,41,42. H. pylori may cause large intestinal microbiota changes through stomach immunopathogenesis, including hypochlorhydria and hypergastrinemia43. Moreover, a study on the microbial 16S ribosomal RNA gene of gastric biopsies and stool samples by Gu et al. found that H. pylori infection is a pivotal factor in gastric and gut dysbiosis, which changes the microbial diversity and community structure, and is possibly involved in gastric carcinogenesis44. Block et al. reported the mechanisms whereby the gut microbiota regulates arthritis development by modulating follicular helper T (Tfh) cell differentiation45. In addition, in an animal study using SKG mice harboring a microbiota dominated by Prevotella copri from RA patients, interleukin-17 (IL-17) was increased with a higher number of intestinal Th17 cells, which response to the arthritis-related autoantigen 60S ribosomal protein L23a (RPL23A) in the lymphocytes of regional lymph nodes and the colon, leading to the development of arthritis. According to their results, dysbiosis increases arthritis sensitivity by activating autoreactive T cells in the intestine46. Both T follicular helper cells and IL-17 are produced by Th17 or mast cells appearing in the RA synovium and are crucial mediators of inflammation in RA pathogenesis47,48,49,50,51.
Thus, the gastrointestinal microbiota is hypothesized to play a contributory role in the pathogenesis of RA via the gut-joint axis. Concerning the mechanisms underlying our study results, we speculate that the increased incidence of RA in H. pylori-infected patients may be caused by a chronic inflammatory response, immune dysregulation, and autoimmune reaction through H. pylori infection, and may also even involve dysbiosis of the gastrointestinal microbiome, which could serve as a trigger of environmental factors in the development of RA. Further studies of the precise mechanism by which H. pylori affect the gastrointestinal microbiome and the dysregulation of immunological response in the development of RA are warranted.
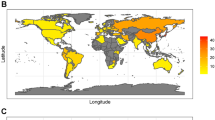
In previous epidemiological and clinical studies, data on the prevalence of H. pylori infection between patients with RA and the general population are inconclusive. Ebrahimia et al. found that 57.9% of RA patients had H. pylori antigens30. A cohort study by Tanaka et al., which enrolled 1815 RA patients, showed that there was a lower prevalence of H. pylori infection with a total of 871 (49.3%) positive H. pylori serum antibodies in RA patients compared with healthy Japanese individuals52. For each group of age, the rate of H. pylori seropositivity increased with age, ranging from 24.5% in RA patients under 30 years old to 56.5% in patients over 60 years. These results are consistent with recent research on the epidemiology of H. pylori, which reported that the prevalence of H. pylori infection in the general population increases with age53,54. Nevertheless, the prevalence of H. pylori infection varies among children and adults and in different regions and continents worldwide55. Early exposure to H. pylori in childhood has been observed because intrafamilial transmission is common, especially in children under the age of 1556. H. pylori infection probably develops in children and chronic infection continues into adulthood until it is tested and the bacterium is eradicated10. In our study, patients under 30 years of age at the index date had a remarkably higher risk of RA. Therefore, we should be aware of possible related joint symptoms in patients diagnosed with H. pylori at a younger age, because early diagnosis is key to optimal therapeutic success.
Studies on the relationship between H. pylori and RA have yielded contradictory findings in recent decades. In contrast to our results, Smyk et al. noted that the evidence supporting H. pylori infection as a cause of RA is less convincing14. A systematic review and meta-analysis study by Youssefi et al. showed no significant correlation between H. pylori infection and RA13. A similar finding was also reported in a cross-sectional and historical cohort study by L. E. Bartels et al. who evaluated a large population-based database of individuals in Denmark with 56,000 patients diagnosed as H. pylori-positive or -negative by urea breath test to explore a possible causative link between H. pylori and the development of RA, with a median follow-up of 8.2 years. Their results reported 390 patients were diagnosed with RA via the urea breath test and there was no significant association between the prevalence of RA and H. pylori infection, with an RA prevalence of 0.66% among H. pylori-positive patients compared to an RA prevalence of 0.71% among H. pylori-negative patients. During follow-up after the urea breath test, 299 patients developed RA. The study also demonstrated a comparable incidence of new RA cases between H. pylori-positive and -negative individuals (0.54% vs. 0.69%), which fit in with an adjusted HR of 0.80 (95% CI 0.56–1.13). That is, these findings did not support any connection between H. pylori infection and RA17. Our findings were the opposite of those reported in the population-based study in Denmark, which may be due to differences in immunological responses to H. pylori antigen among different ethnic populations, genetic differences, including human leukocyte antigen, the prevalence of H. pylori in different areas, and H. pylori strain heterogeneity in different geographic regions. Moreover, the criteria for diagnosis, follow-up interval, and sensitivity of the registry system in different studies may not have been the same. In line with our study, Etchegaray-Morales suggested there may have been links between H. pylori infection, with H. pylori playing a pivotal role as an environmental trigger, and the development of RA14.
Our study has several methodological strengths. First, the study cohort was obtained from the NHIRD, and so the sample size was large, with approximately 195,000 patients enrolled in this study, and the data were nationally representative, with a minimal likelihood of loss to follow-up or recall and selection bias. Second, we used propensity score matching to control and minimize potential confounders.
However, our study has several limitations. First, detailed information about family history, marriage, body weight index, physical activities, inflammatory biomarkers, such as rheumatoid factor or anti-citrullinated peptide antibody, and personal habits, such as dietary habits, cigarette use, and alcohol use are not collected in the NHIRD. It has been assumed that the composition of the gut microbiota, which is closely linked to lifestyle habits, may act as an environmental trigger in the development of RA. Our results might have been biased by these unmeasured confounding factors. In light of this, we focused on factors present in the database, including index year, age, sex, urbanization, social status, insurance properties, and comorbidities. These factors were used for propensity score matching to establish balanced cohorts for our analysis. Nevertheless, these lacking parameters could serve as avenues for more in-depth future research. Secondly, using the NHIRD database, we analyzed patients with H. pylori-related diagnoses and patients receiving anti-H. pylori treatment, but the severity and duration of H. pylori infection could not be measured in this study. The NHIRD does not contain data on H. pylori virulence factors. Therefore, the Cag A-positive H. pylori strain could not be identified, which could have revealed a potential association with an increased risk of developing RA and adverse clinical outcomes. The awareness of symptoms of H. pylori infection and RA among the public and general practitioners varies considerably, which could have affected patients presenting for care as well as the diagnosis by clinicians. Hence, the prevalence of H. pylori infection could have been underestimated, which would have influenced the incidence rate of RA. Furthermore, it was not possible to establish whether anti-H. pylori therapy could reduce RA risks, and it could not be determined whether H. pylori eradication may be capable of inducing improvement in RA disease activity in infected patients. Moreover, due to limitations within the NHIRD, we were unable to images, obtain histopathological reports, or laboratory serum test results for certain conditions such as autoimmune atrophy gastritis (requiring histopathological finding, macrocytic anemia and serum cobalamin level) and autoimmune pancreatitis (requiring image, histopathological finding, and IgG4 confirmation). As a result, these specific diagnoses were not included in our analysis. Hence, our research focused on major systemic autoimmune diseases. Other potentially related autoimmune diseases are areas of future exploration. Finally, the question of whether our study’s results are generally applicable to other ethnic groups remains unclear, as most patients were Taiwanese. Future research is needed to gain a deeper understanding of the possible mechanisms of these associations.
Conclusions
H. pylori infections were associated with the development of rheumatoid arthritis. Clinicians should be aware of the increased risk of developing rheumatoid arthritis among patients with H. pylori infection, particularly in patients under 30 years of age. Further investigation is needed to clarify the basic mechanism of the association.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to privacy purposes but are available from the corresponding author upon reasonable request.
Abbreviations
- H. pylori :
-
Helicobacter pylori
- RA:
-
Rheumatoid arthritis
- LHID:
-
Longitudinal health insurance research database
- NHIRD:
-
National health insurance research database
- ICD:
-
International classification of diseases
References
Klareskog, L., Catrina, A. I. & Paget, S. Rheumatoid arthritis. Lancet 373, 659–672. https://doi.org/10.1016/s0140-6736(09)60008-8 (2009).
McInnes, I. B. & Schett, G. The pathogenesis of rheumatoid arthritis. N. Engl. J. Med. 365, 2205–2219. https://doi.org/10.1056/NEJMra1004965 (2011).
Lee, D. M. & Weinblatt, M. E. Rheumatoid arthritis. Lancet 358, 903–911. https://doi.org/10.1016/s0140-6736(01)06075-5 (2001).
Smolen, J. S., Aletaha, D. & McInnes, I. B. Rheumatoid arthritis. Lancet 388, 2023–2038. https://doi.org/10.1016/s0140-6736(16)30173-8 (2016).
Lee, Y. K. et al. Excess mortality persists in patients with rheumatoid arthritis. Int. J. Rheum. Dis. 24, 364–372. https://doi.org/10.1111/1756-185x.14058 (2021).
Croia, C. et al. One year in review 2019: Pathogenesis of rheumatoid arthritis. Clin. Exp. Rheumatol. 37, 347–357 (2019).
Gibofsky, A. Epidemiology, pathophysiology, and diagnosis of rheumatoid arthritis: A synopsis. Am. J. Manag. Care 20, S128-135 (2014).
Scott, D. L., Wolfe, F. & Huizinga, T. W. Rheumatoid arthritis. Lancet 376, 1094–1108. https://doi.org/10.1016/s0140-6736(10)60826-4 (2010).
Goodwin, C. S. & Worsley, B. W. Microbiology of Helicobacter pylori. Gastroenterol. Clin. N. Am. 22, 5–19 (1993).
Kamboj, A. K., Cotter, T. G. & Oxentenko, A. S. Helicobacter pylori: The past, present, and future in management. Mayo Clin. Proc. 92, 599–604. https://doi.org/10.1016/j.mayocp.2016.11.017 (2017).
Blaser, M. J. & Atherton, J. C. Helicobacter pylori persistence: Biology and disease. J. Clin. Invest. 113, 321–333. https://doi.org/10.1172/jci20925 (2004).
Wang, L. et al. Helicobacter pylori and autoimmune diseases: Involving multiple systems. Front. Immunol. 13, 833424. https://doi.org/10.3389/fimmu.2022.833424 (2022).
Youssefi, M., Tafaghodi, M., Farsiani, H., Ghazvini, K. & Keikha, M. Helicobacter pylori infection and autoimmune diseases; Is there an association with systemic lupus erythematosus, rheumatoid arthritis, autoimmune atrophy gastritis and autoimmune pancreatitis? A systematic review and meta-analysis study. J. Microbiol. Immunol. Infect. 54, 359–369. https://doi.org/10.1016/j.jmii.2020.08.011 (2021).
Etchegaray-Morales, I. et al. Helicobacter pylori and its association with autoimmune diseases: Systemic lupus erythematosus, rheumatoid arthritis and Sjögren syndrome. J. Transl. Autoimmun. 4, 100135. https://doi.org/10.1016/j.jtauto.2021.100135 (2021).
Smyk, D. S. et al. Helicobacter pylori and autoimmune disease: Cause or bystander. World J. Gastroenterol. 20, 613–629. https://doi.org/10.3748/wjg.v20.i3.613 (2014).
Hasni, S., Ippolito, A. & Illei, G. G. Helicobacter pylori and autoimmune diseases. Oral. Dis. 17, 621–627. https://doi.org/10.1111/j.1601-0825.2011.01796.x (2011).
Bartels, L. E. et al. Helicobacter pylori infection is not associated with rheumatoid arthritis. Scand. J. Rheumatol. 48, 24–31. https://doi.org/10.1080/03009742.2018.1464205 (2019).
Hsing, A. W. & Ioannidis, J. P. A. Nationwide population science: Lessons from the Taiwan National Health Insurance Research Database. JAMA Intern. Med. 175, 1527–1529. https://doi.org/10.1001/jamainternmed.2015.3540 (2015).
Hsieh, C. Y. et al. Taiwan’s national health insurance research database: Past and future. Clin. Epidemiol. 11, 349–358. https://doi.org/10.2147/clep.S196293 (2019).
Austin, P. C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 28, 3083–3107. https://doi.org/10.1002/sim.3697 (2009).
Lee, S. W. Kaplan–Meier and Cox proportional hazards regression in survival analysis: Statistical standard and guideline of Life Cycle Committee. Life Cycle 3, e8. https://doi.org/10.54724/lc.2023.e8 (2023).
Karami, J., Aslani, S., Jamshidi, A., Garshasbi, M. & Mahmoudi, M. Genetic implications in the pathogenesis of rheumatoid arthritis; an updated review. Gene 702, 8–16. https://doi.org/10.1016/j.gene.2019.03.033 (2019).
Radić, M. Role of Helicobacter pylori infection in autoimmune systemic rheumatic diseases. World J. Gastroenterol. 20, 12839–12846. https://doi.org/10.3748/wjg.v20.i36.12839 (2014).
Chmiela, M. & Gonciarz, W. Molecular mimicry in Helicobacter pylori infections. World J. Gastroenterol. 23, 3964–3977. https://doi.org/10.3748/wjg.v23.i22.3964 (2017).
Perez-Perez, G. I., Peek, R. M., Legath, A. J., Heine, P. R. & Graff, L. B. The role of CagA status in gastric and extragastric complications of Helicobacter pylori. J. Physiol. Pharmacol. 50, 833–845 (1999).
Ansari, S. & Yamaoka, Y. Helicobacter pylori virulence factor cytotoxin-associated gene A (CagA)-mediated gastric pathogenicity. Int. J. Mol. Sci. 21, 1. https://doi.org/10.3390/ijms21197430 (2020).
Camilo, V., Sugiyama, T. & Touati, E. Pathogenesis of Helicobacter pylori infection. Helicobacter 22(Suppl 1), 1. https://doi.org/10.1111/hel.12405 (2017).
Costa, A. C., Figueiredo, C. & Touati, E. Pathogenesis of Helicobacter pylori infection. Helicobacter 14(Suppl 1), 15–20. https://doi.org/10.1111/j.1523-5378.2009.00702.x (2009).
Hamed, A. E. et al. The effect of Helicobacter pylori seropositivity and activity on disease outcome in patients with rheumatoid arthritis, systemic lupus erythematosus and ankylosing spondylitis. Egypt J. Immunol. 28, 206–214 (2021).
Ebrahimi, A. et al. Relationship between Helicobacter pylori cytotoxin-associated gene A protein with clinical outcomes in patients with rheumatoid arthritis. Immunol. Lett. 211, 49–52. https://doi.org/10.1016/j.imlet.2019.05.014 (2019).
Zentilin, P. et al. Eradication of Helicobacter pylori may reduce disease severity in rheumatoid arthritis. Aliment Pharmacol. Ther. 16, 1291–1299. https://doi.org/10.1046/j.1365-2036.2002.01284.x (2002).
Nakamura, H. et al. Gastrointestinal disorder and Helicobacter pylori infection in patients with rheumatoid arthritis. Mod. Rheumatol. 11, 23–27. https://doi.org/10.3109/s101650170039 (2001).
Ishikawa, N. et al. Helicobacter pylori infection in rheumatoid arthritis: Effect of drugs on prevalence and correlation with gastroduodenal lesions. Rheumatology (Oxford) 41, 72–77. https://doi.org/10.1093/rheumatology/41.1.72 (2002).
Yamanishi, S. et al. Implications for induction of autoimmunity via activation of B-1 cells by Helicobacter pylori urease. Infect. Immun. 74, 248–256. https://doi.org/10.1128/iai.74.1.248-256.2006 (2006).
Moen, K. et al. Synovial inflammation in active rheumatoid arthritis and psoriatic arthritis facilitates trapping of a variety of oral bacterial DNAs. Clin. Exp. Rheumatol. 24, 656–663 (2006).
Reichert, S. et al. Detection of oral bacterial DNA in synovial fluid. J. Clin. Periodontol. 40, 591–598. https://doi.org/10.1111/jcpe.12102 (2013).
Miyauchi, E., Shimokawa, C., Steimle, A., Desai, M. S. & Ohno, H. The impact of the gut microbiome on extra-intestinal autoimmune diseases. Nat. Rev. Immunol. https://doi.org/10.1038/s41577-022-00727-y (2022).
Bedaiwi, M. K. & Inman, R. D. Microbiome and probiotics: Link to arthritis. Curr. Opin. Rheumatol. 26, 410–415. https://doi.org/10.1097/bor.0000000000000075 (2014).
Alpizar-Rodriguez, D. et al. Prevotella copri in individuals at risk for rheumatoid arthritis. Ann. Rheum. Dis. 78, 590–593. https://doi.org/10.1136/annrheumdis-2018-214514 (2019).
He, C., Yang, Z. & Lu, N. Imbalance of gastrointestinal microbiota in the pathogenesis of Helicobacter pylori-associated diseases. Helicobacter 21, 337–348. https://doi.org/10.1111/hel.12297 (2016).
Yap, T. W. et al. Helicobacter pylori eradication causes perturbation of the human gut microbiome in young adults. PLoS ONE 11, e0151893. https://doi.org/10.1371/journal.pone.0151893 (2016).
Chen, L. et al. The impact of Helicobacter pylori infection, eradication therapy and probiotic supplementation on gut microenvironment homeostasis: An open-label, randomized clinical trial. EBioMedicine 35, 87–96. https://doi.org/10.1016/j.ebiom.2018.08.028 (2018).
Heimesaat, M. M. et al. Helicobacter pylori induced gastric immunopathology is associated with distinct microbiota changes in the large intestines of long-term infected Mongolian gerbils. PLoS ONE 9, e100362. https://doi.org/10.1371/journal.pone.0100362 (2014).
Guo, Y. et al. Effect of Helicobacter pylori on gastrointestinal microbiota: A population-based study in Linqu, a high-risk area of gastric cancer. Gut 69, 1598–1607. https://doi.org/10.1136/gutjnl-2019-319696 (2020).
Block, K. E., Zheng, Z., Dent, A. L., Kee, B. L. & Huang, H. Gut microbiota regulates K/BxN autoimmune arthritis through follicular helper T but not Th17 cells. J. Immunol. 196, 1550–1557. https://doi.org/10.4049/jimmunol.1501904 (2016).
Maeda, Y. et al. Dysbiosis contributes to arthritis development via activation of autoreactive T cells in the intestine. Arthritis Rheumatol. 68, 2646–2661. https://doi.org/10.1002/art.39783 (2016).
Hueber, A. J. et al. Mast cells express IL-17A in rheumatoid arthritis synovium. J. Immunol. 184, 3336–3340. https://doi.org/10.4049/jimmunol.0903566 (2010).
Rao, D. A. et al. Pathologically expanded peripheral T helper cell subset drives B cells in rheumatoid arthritis. Nature 542, 110–114. https://doi.org/10.1038/nature20810 (2017).
Sharif, K., Sharif, A., Jumah, F., Oskouian, R. & Tubbs, R. S. Rheumatoid arthritis in review: Clinical, anatomical, cellular and molecular points of view. Clin. Anat. 31, 216–223. https://doi.org/10.1002/ca.22980 (2018).
Himer, L. et al. Role of Th17 cells in rheumatoid arthritis. Orv. Hetil. 151, 1003–1010. https://doi.org/10.1556/oh.2010.28880 (2010).
Chu, C.-Q. The bacterial link with rheumatoid arthritis. Int. J. Rheum. Dis. 26, 603–604. https://doi.org/10.1111/1756-185X.14598 (2023).
Tanaka, E. et al. Prevalence of Helicobacter pylori infection and risk of upper gastrointestinal ulcer in patients with rheumatoid arthritis in Japan. Mod. Rheumatol. 15, 340–345. https://doi.org/10.1007/s10165-005-0419-5 (2005).
Eusebi, L. H., Zagari, R. M. & Bazzoli, F. Epidemiology of Helicobacter pylori infection. Helicobacter 19(Suppl 1), 1–5. https://doi.org/10.1111/hel.12165 (2014).
Leja, M., Grinberga-Derica, I., Bilgilier, C. & Steininger, C. Review: Epidemiology of Helicobacter pylori infection. Helicobacter 24(Suppl 1), e12635. https://doi.org/10.1111/hel.12635 (2019).
Hooi, J. K. Y. et al. Global prevalence of Helicobacter pylori infection: Systematic review and meta-analysis. Gastroenterology 153, 420–429. https://doi.org/10.1053/j.gastro.2017.04.022 (2017).
Burucoa, C. & Axon, A. Epidemiology of Helicobacter pylori infection. Helicobacter 22(Suppl 1), 1. https://doi.org/10.1111/hel.12403 (2017).
Acknowledgements
The authors gratefully acknowledge the use of the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by National Health Research Institutes. We would also like to show our gratitude for the support from the medical research department of Taichung Veteran General Hospital. This work was supported by a grant from Taichung Veterans General Hospital Research Foundation TCVGH-1116502C and 1118701B.
Author information
Authors and Affiliations
Contributions
M.W. and T.L. contributed to the conception and design of the study. P.L. organized the database and performed the statistical analysis. T.L. wrote the first draft of the manuscript. M.W., M.L., C.L., and J.W. revised the manuscript. All authors contributed to the manuscript revision, and read, and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, TH., Wu, MC., Lee, MH. et al. Influence of Helicobacter pylori infection on risk of rheumatoid arthritis: a nationwide population-based study. Sci Rep 13, 15125 (2023). https://doi.org/10.1038/s41598-023-42207-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42207-w
This article is cited by
-
Re-evaluation of dietary interventions in rheumatoid arthritis: can we improve patient conversations around food choices?
Rheumatology International (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.