Abstract
The architectural design of hospitals worldwide is centred around individual departments, which require the movement of patients between wards. However, patients do not always take the simplest route from admission to discharge, but can experience convoluted movement patterns, particularly when bed availability is low. Few studies have explored the impact of these rarer, atypical trajectories. Using a mixed-method explanatory sequential study design, we firstly used three continuous years of electronic health record data prior to the Covid-19 pandemic, from 55,152 patients admitted to a London hospital network to define the ward specialities by patient type using the Herfindahl–Hirschman index. We explored the impact of ‘regular transfers’ between pairs of wards with shared specialities, ‘atypical transfers’ between pairs of wards with no shared specialities and ‘site transfers’ between pairs of wards in different hospital site locations, on length of stay, 30-day readmission and mortality. Secondly, to understand the possible reasons behind atypical transfers we conducted three focus groups and three in-depth interviews with site nurse practitioners and bed managers within the same hospital network. We found that at least one atypical transfer was experienced by 12.9% of patients. Each atypical transfer is associated with a larger increase in length of stay, 2.84 days (95% CI 2.56–3.12), compared to regular transfers, 1.92 days (95% CI 1.82–2.03). No association was found between odds of mortality, or 30-day readmission and atypical transfers after adjusting for confounders. Atypical transfers appear to be driven by complex patient conditions, a lack of hospital capacity, the need to reach specific services and facilities, and more exceptionally, rare events such as major incidents. Our work provides an important first step in identifying unusual patient movement and its impacts on key patient outcomes using a system-wide, data-driven approach. The broader impact of moving patients between hospital wards, and possible downstream effects should be considered in hospital policy and service planning.
Similar content being viewed by others
Introduction
The management of patients from hospital entry to exit is a major challenge in healthcare, amid bed reductions and an ageing population1. Secondary health systems are often structured as wards within departmental disciplines, departments within hospitals, and hospitals within multi-site organisational networks (or hospital ‘trusts’ in the UK). Patients must move through various locations as their needs evolve, making intrahospital transfers a daily practice in health systems worldwide. Many initiatives have attempted to optimise this process, otherwise known as ‘patient flow’2,3, typically by predicting demand on the most commonly used patient pathways, and managing the points of ‘constraint’ (i.e. where demand overwhelms the capacity) such as the emergency department (ED)4,5,6,7. Often trade-offs exist between admitting patients to the most appropriate ward and accommodating all patients during peaks in bed demands. Patients can therefore undertake convoluted movement patterns, particularly when bed availability is low. The impact of these rarer, atypical trajectories is unclear. Despite the activity around expediting patient flow, few studies have analysed hospital-wide patient movement with an etiological approach which questions whether potential associations exist between specific transfer patterns and clinical outcomes2,8.
Several studies have examined the link between the number of intrahospital transfers undergone by patients and adverse outcomes9. Taking a whole-system view of the patient journey, they show that patients with more intrahospital movements have worse outcomes with respect to length of stay (LOS), falls, infection risk and carers’ perceptions of patient discharge readiness10,11,12,13,14,15,16. However, intrahospital transfers occur for a variety of reasons, (e.g. isolation due to infection, transfer to higher level-of-care, procedures, bed pressures and patient preference) and this approach may overlook their unequal impacts on outcomes. From a more targeted perspective, the outcomes of ‘outlying’, ‘bed-spaced’ or ‘boarding’ individuals, which have been placed on clinically inappropriate wards have been assessed17. The practice of outlying individuals into a ward outside of their home speciality, resulting in transfers between inlier and outlier wards, can be a strategic decision to reduce ED congestion, and is reported across health systems18,19,20. By definition such patients deviate from the regular trajectory for their speciality. Some evidence suggests this increases LOS, subsequent readmissions, and mortality17. However, outliers are usually defined in a binary sense by whether the individual has been placed on an inappropriate ward, without consideration to their movements up to and beyond the outlying ward. This may be a significant source of unobserved confounding between outlying status and LOS, with intrahospital transfers shown to double LOS in some populations11. A second limitation is a lack of specificity in the definition of an outlying patient, which can be unclear, or simplified to medical patients on a surgical ward17. Relying on predefined speciality definitions may overlook occurrences where patients are on a suboptimal ward within their overarching division21, or misclassify patients admitted to wards with multi-speciality staff. These factors may lead to inaccurate effect estimates.
Patient movement connects many areas of the hospital and may lead to unintended consequences, aligning with common characterisations of a complex system22. However, while complexity can increase with the quantity and uniqueness of relationships between components23, the literature taking a whole-system view of patient transfers has not distinguished between transfer type, while the targeted outlier literature does not usually consider the whole patient trajectory. A combination of these two approaches is needed, which demarcates these more complex patient transfers from regular transfers, while maintaining a view of the whole patient hospital journey. Guided by a data-driven definition of ward specialities using electronic health record (EHR) data, this two-strand study firstly defines atypical transfers as movements between wards with no overlapping specialities and explores their association with key patient outcomes. Secondly, to understand the nature of this novel exposure more fully, we explore the causes of atypical transfers using in-depth qualitative interviews and focus groups with site nurse practitioners and bed managers.
Objectives
The overarching aim of this study is to understand the impact of atypical transfers on patient outcomes, and why these transfers occur. Fulfilling this aim therefore requires both quantitative and qualitative data sources and is well suited to a mixed-methods approach24. The specific objectives from the quantitative and qualitative strands of the study are:
Quantitative objectives:
-
To provide a systematic, data-driven definition of atypical transfers
-
To explore the differential effects of atypical movement patterns on the patient outcomes of: LOS, 30-day readmission and mortality
Qualitative objectives
-
To identify the possible causes of atypical transfers based on site nurse practitioners’ and bed managers’ perceptions
Methods
An explanatory sequential mixed-methods study design, with a quantitative focus, was conducted using routinely collected quantitative EHR record hospital data and qualitative semi-structured focus groups and interviews. The quantitative data were collected and analysed under a retrospective cohort study design, while exploratory thematic content analysis was used to describe the factors underlying the quantitative results. Quantitative and qualitative findings were therefore integrated to generate an in-depth understanding of the atypical transfers exposure. An overview of the study design is given in Fig. 1.
Retrospective cohort study
Study setting and participants
De-identified EHRs of patients admitted over a 3-years period (falling between 2015 and 2018) were extracted to three main hospital sites, all part of a single hospital ‘trust’. Hospital trusts are an organisational unit in the NHS, consisting of hospitals serving a geographical region. They provide acute and emergency care under one or more hospital sites, which can include general hospitals as well as national specialist care centres25,26,27. The data included patient and spell unique identifiers, while dates of admission were fully anonymised. The data structure and setting are described in detail elsewhere14. A retrospective cohort study design was used to examine the association between atypical ward transfers and the outcomes of LOS, 30-day readmission, and in-hospital mortality. Aiming to compare the relative effects of different types of patient movements, we excluded patients who had been treated on one ward for their entire spell, meaning the minimum exposure was therefore one intrahospital transfer. Our quantitative analysis therefore asks the question: among patients who move, does moving atypically increase LOS, odds of readmission, or mortality? Maternity and paediatric patients were excluded (see Supplementary Note 1a). Likewise, elective patients were excluded as planned admissions exhibit a different acuity profile to emergency patients. The full inclusion criteria are shown in Supplementary Fig. 1 and pre-analysis data processing is outlined in Supplementary Fig. 2.
Exposure variables
Patient ward changes were defined as any change of location in the patients EHR, including temporary movements to procedure wards but excluding informal movements and those from the emergency department. The phrases patient transfer and movement are used interchangeably. Three types of patient transfers were considered: atypical, regular and site transfers (see Fig. 2 for descriptions).
Ward specialities
We defined ward specialities based on the true hospital usage of the whole patient population, including elective and day-only patients. A concise description of the patient’s condition was first obtained using treatment function codes (TFCs), which refer to the clinical division of the dominant healthcare professional responsible for the patient during an episode of care28. TFCs are time-dependent, with broader admitting specialities (e.g., general medicine) typically evolving into more specific descriptions (e.g., cardiology) as diagnoses and treatments are decided. The last recorded tfc was assumed to be the most accurate summary of the patient’s condition and selected for analysis. The patient’s final TFC was recorded against each unique ward entered during the spell, such that the patient ‘deposited’ their specialty at each stage of their journey through the hospital. Frequencies of tfcs were generated per ward, and a commonly used measure of market competitiveness, the herfindahl–hirschman index (HHI)29, was used to create a speciality diversity index, defined as:\(HHI = \mathop \sum \limits_{i = 1}^{N} S_{i}^{2}\)where \(S_{i}\) is the ‘share’ or proportion of patients admitted to a given ward from speciality i, and N is the total number of main specialities observed on the ward. The inverse of the HHI index is a measure of the ‘effective number of’ groupings, or the equivalent market size (EMS) corresponding to patient specialties ranked in descending order30. Each ward was assigned a number of representative specialties corresponding to their EMS rounded to the nearest integer. A high EMS indicates a multifunctional ward, while a low EMS indicates a highly specialist ward. Wards assigned the same specialties are not necessarily equivalent in function but could indicate a regular patient movement trajectory across two wards which deliver different services.
Atypical transfers
Atypical transfers were defined as a transfer between pairs of wards with no overlapping specialities identified from their EMS (see Fig. 3). We therefore use the term atypical neutrally, reflecting the fact that such movements were uncommon given the speciality profiles of the two wards, rather than an appraisal on the appropriateness of the transfer at the individual patient level. To avoid inflating atypical transfer count by reciprocal trips to and from one ward, wards which only admitted patients for an average of 6 h or less were verified and removed from the atypical transfer list if functioning as a temporary minor procedure ward, such as endoscopy. All other transfers were regarded as regular (non-atypical) transfers, with the exception site transfers (see Fig. 2).
A depiction of a regular and atypical transfer movement. Ward pairs (i,k), and (i,p) belong to the same overarching speciality, making all transfers between them ‘regular’. Similarly, ward pairs (a,b) belong to an alternative overarching speciality and transfers between this pair are ‘regular’. Meanwhile, transfers between crossing specialities (such as (a,k), and (i,b)) are classed as ‘atypical’.
Box 1 is an illustrative fictitious example of an atypical patient’s hospital journey, based on true trajectories, demonstrating how variables in the EHR dataset were used to reconstruct patient journeys through the hospital.
Outcome variables
Three outcomes were investigated: LOS, 30-day readmission and in-hospital mortality. A continuous variable for LOS was derived for each spell using the difference between admission and discharge timestamps (recorded up to 15 min resolution) converted to days and fraction of days. Unplanned readmissions were defined as emergency readmissions for any reason (except for pregnancy) within 30 days of an index hospitalisation. Index admissions were defined iteratively, such that each spell could become an index admission if followed by a subsequent admission. The unit of analysis in this regression was the index admission, and all covariates are taken from this spell. As all hospital sites pertained to the same hospital network, readmissions to different sites were included in the analysis (and distinguished from site transfers which were categorised under the same spell ID)31. If the index hospitalisation ended in death, it was excluded from the analysis of readmission. Finally, in-hospital mortality was recorded as a binary variable if the spell ended in the patient’s death. The unit of analysis for all outcomes were hospital spells, therefore patients could contribute more than one hospitalisation to the main model if it fulfilled the selection criteria.
Confounding variables
We aimed to control for available covariates which confounded the exposure-outcome relationship32. Separate models were fitted for each outcome, and directed acyclic graphs, were used to guide variable selection (Supplementary Fig. 3). As acutely unwell patients have been shown to have a higher number of transfers, and non-standard needs may be more prone to taking uncommon routes through the hospital33, patient acuity and complexity were considered confounders. We controlled for patient demographics and the following variables in the modelling: Elixhauser comorbidity index, admission to an ICU/critical care, weekend admissions and out of hours admissions (7 pm–7am), the number of primary ICD-10 codes (as an estimate of multi-morbidity34), the major diagnostic category of the first primary ICD-10 code recorded, discharge destination and severity of surgical procedures (diagnostic, minor, intermediate, and major procedures using existing code lists created by Abbott et al. (see supplementary Note 1b) in addition to diagnostic imaging35).
Statistical Analysis
Atypical transfers were explored using network analysis and depicted using a chord diagram. Univariable regressions (see Supplementary Table 1a, c) and multivariable regression models were fitted separately. The association between atypical transfers and LOS was modelled by a generalized linear model (GLM) using a gamma distribution and a log-link. Average marginal effects (AMEs) were computed with respect to the variables of interest, holding all other variables constant36. It can be interpreted as the impact of a change in a focal independent variable on predicted value of the outcome, holding other variables constant37. AMEs were computed in R using the ‘margins’ command, specifying ‘type = response’38. An interaction term between atypical transfers and age was explored and found to be statistically insignificant. Logistic regressions were used to examine associations for the outcomes of mortality and 30-day readmission. Clustered standard errors by individual patient were implemented in all regression models using the Sandwich package. No major collinearity existed between variables. Large LOS ‘outliers’ were not removed, on the basis that these are true values in the data39,40. Spells containing incomplete information were removed as missingness was minimal. The DHARMa package in R (Hartig 2018) was used to evaluate all models’ fit.
Sensitivity analyses
We performed 6 sensitivity analyses to examine the robustness of the results by altering parameters related to the patient population, covariates, exposure and model diagnostics (Table 1).
Analyses were conducted using R version 4.2.1.
Qualitative focus groups and interviews
Study population
A purposeful sampling strategy was adopted whereby the clinical study lead sent an invitation email to site nurse practitioners (clinical staff, denoted by prefix ‘S’ in participant quotations) and bed managers (non-clinical staff, denoted by prefix ‘B’ in participant quotations) of varying seniority at the study setting. Participants were prioritised by years of experience, due to the quantitative data being historic (collected between 2015 and 2019) and by familiarity with all three hospital sites. Three focus groups (consisting of 4 to 5 participants) and three one-to-one interviews were conducted (totalling 16 participants). On average, participants had 13 years of experience at the hospital trust. The number of focus groups chosen was a pragmatic decision based on the availability of participants in this role during the study period.
Data collection
All focus groups and interviews were conducted remotely via Microsoft Teams between 9 July 2022 and 29 October 2022. The focus groups duration was around 1 h and interviews 40 min. The decision to use online data collection methods was due to the risk posed by the potential of Covid-19 transmission between participants, and the fact it allowed participants to join from different sites while minimising disruption to their working hours. A focus group topic guide which comprised visualisations of atypical transfer pathways was pilot tested and revised.
Data analysis
Interviews and focus groups were visually recorded, transcribed and checked for accuracy by EM. The thematic framework method was used to analyse the qualitative data content surrounding atypical transfers. Codes were inductively generated from the data, with the resulting codes used as the basis of a thematic framework. Subsequently, the framework was used to index, chart, map and interpret the data within and between cases42. A descriptive approach was taken, with themes remaining close to the participant’s accounts, and attention was paid to deviant cases which were included in the findings43. Annotation and coding of transcripts were conducted using NVivo (Version 12, QSR International, Burlington, Massachusetts, USA).
Ethical approval
This study was defined as a service evaluation by the Health Service Research Authority and therefore NHS Research Ethics Committee approval was not needed. The study was approved as a service evaluation through Imperial College Healthcare NHS Trust (Ref:347/Ref:719). Ethical research practice standards were followed throughout, including obtaining informed consent and right to withdraw from the study at any point. All methods were conducted in accordance with the relevant guidelines and regulations in place.
Results
Patient characteristics
A total of 55,152 non-elective spells taking place during the 3-years study period met the entry criteria, of which 7088 (12.9%) experienced at least one atypical transfer between pairs of wards with no common main specialities (Fig. 4). Of these, 5844 (82.4%) undertook one atypical transfer, while 1244 (17.6%) undertook two or more atypical transfers. Meanwhile, 8.5% of all patients experienced at least one site transfer. Over half of the population (54.2%) were transferred only once during their spell (n = 29,868). A breakdown of transfer type for patients with multiple transfers is given in Supplementary Fig. 4. Most of the study population was male (52.9%), over 65-years old (55.2%), and 69.8% exhibited at least one Elixhauser comorbidity. Out-of-hours admissions were common, with 48.0% of admissions occurring between 7 pm and 7am, while 23.8% of admissions occurred at weekends. The median LOS was 7.2 days, and 3022 (5.5%) of spells resulted in in-hospital death.
Chord diagrams depicting atypical transfers over the three hospital sites (1-3). Each sector in the outer track represents a ward, while each link between wards represents an atypical transfer. The thickness of the link is proportional to the volume of patients exchanged, between approximately 10 and 360 patients. The label of the track reflects the top specialities of the patients residing on that ward based on the whole patient population, with a maximum of 3 specialities.
Patients undertaking atypical transfers did not differ from those with no atypical transfers with respect to age, site transfers, Elixhauser comorbidities, or in-hospital death, with no statistically significant differences between non-atypical and atypical transfer patients (Table 2). However, atypical transfer patients were more likely to be admitted at weekends and out-of-hours (25.3% vs 23.5% p < 0.001, and 52.0% vs 47.4% p < 0.001, respectively). Such patients also underwent more procedures of all categories (excluding major procedures), but had fewer admissions to the intensive care unit (ICU) (5.8% vs 6.9%, p < 0.001) (Table 2). A full descriptive characteristics table is given in Supplementary Table 2.
Atypical transfer characteristics
Across the three hospital sites, 805 unique atypical transfer ward pairs were identified. While a small number of ward combinations account for the majority of atypical transfers, many atypical transfer routes rarely used, with 78% of pairs being used 10 or less times across the study period, and 29% of pairs only occurring once. Across all hospital sites the most travelled atypical paths included short-term observation wards such as assessment and clinical decision units (CDUs). While no transfers from A&E were recorded in the data, CDUs which are short stay wards under the care of emergency medicine consultants44, were labelled under the speciality A&E. This reflects the fact that most patients on this ward were discharged before seeing another consultant. Only 1.6% of all atypical transfers involved the ICU or critical care ward, meaning that few atypical pathways are used to transport acutely deteriorating patients.
Multivariable regression results
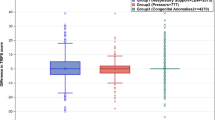
After adjusting for the listed confounders and averaging over all observations in the data sample, each additional atypical transfer results in an estimated increase in LOS of 2.84 days (95% CI 2.56–3.12). By comparison, regular ward transfers had an effect size of 1.92 days (95% CI 1.82–2.03) increase in LOS for each additional transfer. Meanwhile, site transfers showed the largest effect on LOS with an increase of 3.02 days in LOS (95% CI 2.70–3.35) for each additional site transfer. Figure 5a summarises the AMEs from the multivariable GLM used for the focal predictors LOS.
Multivariable regression results. Panel A shows the multivariable GLM regression with a gamma distribution and log-link predicting hospital LOS (n = 55,152). Results are presented as adjusted average marginal effects in days. In addition to atypical transfers, regular transfers, site transfers, the regression is controlled for age, gender, ethnicity, Elixhauser comorbidities, weekend admission, out-of-hours admission, discharge destination, admission to an ICU/critical care ward, number of primary diagnoses, imaging procedures, minor, intermediate and major surgical procedures, and major diagnostic category. Panel B shows a multivariable logistic regression predicting emergency readmission (n = 52,125), with results presented as adjusted odds ratios. All spells ending in in-hospital death were removed from this regression (n = 3022) and 5 remaining patients were removed from the major diagnostic category ‘External causes of morbidity' to avoid violating the positivity assumption39. In addition to atypical transfers, regular transfers, site transfers, the regression is controlled for age, gender, ethnicity, Elixhauser comorbidities, weekend admission, out-of-hours admission, discharge destination, admission to an ICU/critical care ward, number of primary diagnoses, imaging procedures, minor, intermediate and major surgical procedures, major diagnostic category and length of stay. Panel C shows a multivariable logistic regression predicting in-hospital mortality (n = 55,000), with results presented as adjusted odds ratios. Patients under the major diagnostic categories ‘external causes of morbidity’ and ‘factors influencing health status and contact with health services’ (n = 152) were similarly removed due to the positivity assumption. Covariates included in the model were: atypical transfers, regular transfers, site transfers, the regression is controlled for age, gender, ethnicity, Elixhauser comorbidities, weekend admission, out-of-hours admission, admission to an ICU/critical care ward, number of primary diagnoses, imaging procedures, minor, intermediate and major surgical procedures, and major diagnostic category. All 95% confidence intervals are based on standard errors clustered at the patient level.
Atypical transfers and site transfers did not have a significant association with readmission in the adjusted model (Fig. 5b). However, there was weak evidence that regular transfers are associated with a minor increase in odds of readmission (OR = 1.02, 95% CI 1.00–1.04).
Site transfers were associated with lower mortality (OR = 0.72, 95% CI 0.64–0.80), with a decrease of 28% in odds of death for each unit increase in site transitions (Fig. 5c). No relationship between atypical transfers or regular transfers and mortality was observed. Full multivariable regression models are given in Supplementary Tables 3–5.
Sensitivity analyses
The effect of atypical transfers was robust across the sensitivity analyses conducted, with results remaining consistent. Redefining atypical transfers by using the first TFC to determine patient specialities reduced the number of patients undertaking at least one atypical transfer by 22.8% (n = 5473). Nevertheless, effect sizes remained consistent, with the magnitude of the impact of atypical transfers on LOS only marginally decreasing (AME = 2.58; 95% CI 2.28–2.87, p < 0.001). Meanwhile, using an alternative categorisation of surgical procedures (See Supplementary Note 1c) increased the effect size to 3.03 days (95% CI 2.75–3.32, p < 0.001) but attenuated the association between regular transfers and 30-day readmission (OR = 1.01; 95% CI 0.99–1.03, p = 0.22). Removing influential outliers by large values of standardised residuals resulted in 149 observations being dropped from the LOS model, 19 from the mortality model and none from the readmission model but did not meaningfully change the main effects. All sensitivity analyses are presented in Supplementary Tables 6–8.
Reasons underlying atypical transfers
Open coding identified 12 distinct reasons for atypical movements, classified under four main themes: ‘complex clinical journeys’, ‘non-clinical factors’, ‘a need for services and facilities’, and ‘unusual pathways’. The four themes are outlined if the following section. Table 3 details the codes and their descriptions, alongside illustrative quotations from the data.
Complex clinical journeys
Participants highlighted the possibility that some patients have complex clinical journeys, needing input from multiple specialities as their condition evolves. Co-occurring clinical needs could therefore result in transfers across wards with differing but inter-related specialities such as cardiology and renal wards, or stroke and vascular wards. Patients who suffered from unexpected adverse events such as a stroke or a fall may likewise require treatment across differing speciality wards equipped to treat their conditions. Participants also discussed a population of patients whose clinical complexity meant that the most appropriate speciality was unclear, resulting in multiple transfers as patients were assessed and their treatment course decided. This group included patients being transferred from clinical decisions units to in-hospital wards.
Non-clinical factors
A consistent explanation for atypical transfers offered across the data was the possibility that atypical transfers occur for operational reasons. Patients could be outlied across different divisions, such as medicine or surgery to create capacity for incoming patients. It is important to note that these transfers could not always be clearly distinguished from those of patients with complex journeys without additional patient-level information:
Well two things, it could be typical or atypical. Typical if for example a patient is coming with nausea and vomiting, [who] has developed a surgical problem - then that would be a typical transfer, because … it's not a medical problem anymore it's a surgical…However, it becomes atypical if for example we’re inundated with quite a lot of medical patients in A&E… and they [surgical unit] have got something like 10 beds … that they don't need… I would identify patients, with the help of the medical team, to outlie patients into the spaces. It’s because we need to deal with capacity issues and safety of A&E. - Focus group 2, Participant S06
Atypical transfer patients may also be moved within their overarching clinical division to create bed spaces. While such transfers could still be classed as non-clinical, participants typically distinguished these patients, who would remain in an appropriate overarching bed base, from strict outlier patients. One participant highlighted that some speciality wards are not able to admit patients out-of-hours, resulting in an intermediate general ward being used to admit the patient.
A need for services and facilities
Another theme across the data involved atypical transfers to a specific service or facility. These movements were distinct from complex clinical journeys in that they occurred in order for the patient to reach a specific service, equipment or infrastructure, as opposed to more broadly receive input from a second clinical speciality. A common example was the need for rehabilitation services, which were offered on specific wards rather than as a mobile service. In addition, cardiac monitoring was a scarce resource and usually required the patient to be moved to a ward which provided this equipment. Similarly, if a patient became infected on an open bay ward, a transfer would be required to an isolated single side-room, which are only available in a minority of wards.
Unusual pathways
Finally, the ‘unusual pathways’ theme comprises a small number of atypical transfers which participants highlighted as obscure, and possibly due to exceptional reasons. Unusual reasons included major incidents, ward closures, and circumstances such as two individuals being involved in a confrontation being admitted to the same trauma ward.
Discussion
Principal findings
An increasing evidence base associates intrahospital transfers with adverse outcomes. However, our analysis shows that not all ward transfers are equal. In a large-scale retrospective cohort study, we show the feasibility of a novel data-driven approach, which leverages rich EHR data to characterise atypical transfers. We found that among hospitalised patients who undertake at least one transfer during their spell, 12.9% use ‘atypical’ routes between uncommon pairs of wards for their speciality. Such patients experience an approximate 2.8 day increase in LOS, after controlling for regular transfers, site transfers and case-mix variables. The effect size was 0.9 days larger than that of a regular intrahospital transfer to or from any other ward in the hospital (AME = 1.92; 95% CI 1.82–2.03). No relationships between atypical transfers and mortality or 30-day readmission were observed. A secondary finding is that different types of patient movement have differing effects. Transfers between hospital sites within one trust were associated with a 28% reduction in odds of mortality (OR = 0.72; 95% CI 0.64–0.80), and regular transfers with a small increase in odds of readmission (OR = 1.02; 95% CI 1.00–1.04).
Qualitative focus groups and interviews with experienced site nurse practitioners and bed managers revealed four overarching themes surrounding the decision making underlying atypical transfers: complex patient journeys, meaning the patient did not fit into any common groups of services (theme 1), a lack of capacity resulting in non-clinical transfers within and across overarching major divisions (theme 2), or a particular clinical need triggering a transfer to reach specific services and facilities (theme 3). More exceptionally, some transfers had no clear explanation, and possibly arose because of a rare, unplanned event (theme 4).
Triangulation and interpretation in light of other evidence
While our study did not directly explore the effect of placing patients on clinically inappropriate wards (and excluded patients staying only on one ward), its findings are consistent with several studies on the impact of outlying patients, which report increases in LOS by 0.1–1 days18,19,45. Only one quantitative study has explored the topic of outlying patients using UK hospital data, reporting an increase in LOS but no increased effect on mortality18. The qualitative strand of this study suggests our approach captured ‘partial outliers’ who move between appropriate and inappropriate wards, or vice versa (theme 2). Quantitatively, we found that patients experiencing atypical transfers were more likely to be admitted out-of-hours, which has been associated with outlying status in other studies46. The effect of undergoing an atypical transfer cannot be separated from the subsequent impact of being treated on a potentially inappropriate ward, which may account for increased LOS. However, as clinical factors were also suggested as reasons underlying the transfers, it is not the sole explanation of the effect. Therefore, while atypical transfers have a comparable effect on LOS to outlying patients, they do not necessarily imply that the transfer is clinically inappropriate18.
The qualitative component of the study highlighted two clinical reasons which may lead to atypical transfers. The patient does not equivocally fit into commonly paired wards (theme 1), or the patient needed access to a specific service or facility (theme 3) such as the need for cardiac monitoring paired with an orthopaedic condition, where the nursing skills to look after both factors is seldom co-located in one ward. The quantitative strand of this study also supports these explanations. Patients taking atypical routes were more likely to have multiple primary ICD-10 codes during their spell, potentially reflecting a complex clinical condition and generally experienced more procedures. The need for isolation due to infection was discussed as a reason behind atypical transfers qualitatively, but quantitative findings showed that removing infected patients from the analysis did not attenuate the association with increased LOS, making infection control an unlikely driver of increased LOS. In other literature, cases of population-capacity misalignment comparable to the first theme have been described in qualitative work47,48,49. Kreindler et al., highlight the complexities faced by hospital managers in Canada when patients have significant co-occurring needs, such as dementia and pneumonia50. The patient is then moved, introducing them to a new team and extending their spell. Atypical routes also frequently involved observation units, which have been associated with ad-hoc use where a lack of alternative pathways exist44,51.
An important distinction our study has made to previous literature is that it is exploring the whole patient movement history, rather than a single location. This approach highlights the outcomes of patients who experience transfers. Ward transfers are complex procedures, both in the physical process required to move a patient, which can be destabilising52, and the decision-making processes behind them. Transfers are a vulnerable time for patients and can leave them feeling anxious, disorientated, and ‘forgotten’ by staff53,54, particularly on an inappropriate ward47. Transfers also require cooperation, negotiation, and trust between the sending and receiving clinicians, which is strengthened by familiarity55,56,57. Clinical handovers can be prone to workarounds and communication breakdowns even within one clinical team58, and exacerbated when occurring across units, specialities and physical boundaries59. Patient movement may therefore be a potential additional driver behind increased LOS, which should be considered in studies exploring patient hospital locations.
It is also important to note that among patients with at least one transfer, each additional regular transfer increased LOS by approximately 1.9 days, suggesting that even those undertaking regular transfers experience an associated increase in LOS, after adjusting for case-mix factors. However, this relationship may differ when considering patients unexposed to movement. Others have reported large increases in LOS after intrahospital transfers11,60, highlighting the importance of avoiding transfers where possible. Similarly, while the outcomes of patients following an inter-hospital transfer have been studied61,62, the impact of a transfer to a hospital within a single trust has been unexplored. Our finding that such transfers are associated with a decrease in mortality suggests that localisation of specialist and general hospitals within a trust is a successful model of care, in the context of a large urban hospital trust. Our models controlled for the patient acuity variables available, however it is possible that only patients most likely to survive are transferred between sites, leading to residual confounding. The differences between NHS trusts which co-locate their services in a single site, versus geographically dispersed sites are areas of possible future investigation.
Strengths and limitations
A key strength of our study is the use of a data directed definition of ward specialities and atypical transfers, coupled with a qualitative exploration of their meaning. The data driven definition captures the functional use of wards, rather than a pre-defined, theoretical use. This is an important strength, as the boundaries of a specific service can become blurred in the day-to-day running of a hospital, particularly as bed pools shift over time, leading to possible misclassification of outlying patients63. The task of matching specialities to patient needs is highly complex and organisation dependent, and pre-defining ward specialities may also overlook the fact that staff treating many outliers can become as familiar in caring for them as an inlier patient. With some studies reporting as many as 40% of the patient population to be outliers46, the causal hypothesis that outlier patients have increased adverse outcomes because they are treated by a nursing team which is inexperienced with their condition may not hold. Nevertheless, using a heuristic also draws arbitrary cut off points, and speciality definitions vary depending on the chosen TFC, which can also be subject to recording inconsistencies. While this limitation is mitigated by the large study size, the fact that we removed erroneous spells on several criteria, and that consistent results were obtained when using the first and last patient TFC, inaccuracies and inconsistencies are a known limitation to retrospective EHR data analyses, which should be considered when interpreting results64. Importantly, the qualitative strand of this study addresses some of the weaknesses of the quantitative strand, by verifying ward specialities and explaining the possible purposes underlying atypical transfers. Moreover, our quantitative method can be applied to other routinely collected datasets for validation without the considerable domain knowledge needed to allocate ward specialities manually. It is also possible that atypical transfers are a marker of health system strain akin to outlying patients, leading to residual confounding from broader health system factors such as understaffing, which was not directly adjusted. While it is difficult to attribute causality between this exposure and the environment in which it occurs, adjusting for weekend/out-of-hours admissions when hospitals typically function with reduced staffing, as well as approximate seasonality did not account for the effect on LOS.
It is also important to consider that the specific reasoning behind transfers cannot be systematically analysed without patient notes, and that the qualitative data is limited by a relatively small sample size and homogenous participants, which notably excluded medical doctors. However, the qualitative strand had a narrow aim of understanding the reasons behind atypical transfers, and the participants recruited held a large amount of knowledge and depth of experience relevant to this aim. The principles of information power suggests such a study does not require a large sample size65. Further exploring impact of atypical and other transfers on the workload of other professionals in the hospital, such as doctors and aligned health professionals would be a useful direction for future work. Moreover, while variables such as OPCS-4 and ICD-10 codes found in EHR data could have been used to identify factors reported qualitatively in Table 3, and therefore corroborate the qualitative findings, these data are generally not granular enough to be able to trace their occurrence to one specific ward. Other information sources could be leveraged in future work. For example, others have used incident report systems to understand harmful events and near misses, as well as patient experience66,67. These data could be used to explore associations between patient movement journeys and the themes explored qualitatively. Finally, the generalisability of our findings is unclear. Three other studies have used network analysis to explore patient transfers within hospitals and demonstrated that rare, low frequency transfers also occur in these hospital environments33,68,69. This suggests atypical transfers (with respect to frequency) are not isolated to our setting; however, authors did not link these to patient outcomes.
Implications
Our findings have implications for hospital design and future research. Firstly, we have demonstrated the feasibility of a data-driven method to identify patients which, for any reason, move between uncommon pairs of services using EHR data. These initial findings support further exploration of ward movements, as well as the potential for hospital trusts to leverage their own EHRs for optimising patient pathways in real-time. For example, the identification of complex patients though atypical movements could guide the creation of multi-condition services based on clusters of co-occurring needs50. Models of population segmentation are an important complement to the shift from single conditions to integrated, needs-based care systems70,71, and can be supported by data-driven methods72,73,74. While focus has been given to primary care interventions70, population segmentation interventions in secondary care may improve hospital flow through the introduction of integrated units which have fluid resources and wide eligibility criteria, to better accommodate patients with a ‘shifting fuzzy set of needs’50. Atypical movements can be a potential system focused metric used alongside others to develop segmentation logic. As the UK government looks to expand hospital infrastructure75, such analyses have a place in informing policy on the medical built environment, in combination with knowledge from clinicians, hospital managers and healthcare architects.
Secondly, when patients must be moved due to non-clinical reasons, our analysis also suggests that transfers to wards with a similar speciality profile reduces subsequent LOS. In the highly complex, non-linear hospital system, it is important to consider the downstream effects of policies which aim to rapidly decant the ED76,77. These can result in more patients placed on wards with any available space, increasing atypical transfers78. While our findings show that atypical transfers do not increase mortality or readmission, their relationship to increased LOS suggests that such strategies may exacerbate exit-block in the long-term, as patients remain in hospital for longer. From a systems perspective, minimising atypical transfers helps to sever the cycle of bed-blocking that occurs when patients on the wrong ward spend extra days in hospital, thereby further diminishing access to beds79.
Finally, hospital policies regarding inter-hospital transfers and transfers of critically ill patients are typically more developed than those surrounding intrahospital transfer, despite adult intrahospital transfers also causing safety concerns80,81,82. Our work can help to inform principles underpinning the safety of intrahospital transfers, such as transferring to similar wards where possible. While many hospital policies encourage clinical judgement to be used in the decision to transfer, currently few outline the evidence on potential consequences of transfers, which if provided may help healthcare professionals to understand the risks involved. Future work across multiple hospital centres is needed to understand the generalisability of these findings, given the heterogeneity of ward management practices across organisations, and potentially allow for the creation of national level guidelines for intrahospital moves. A further recommendation for future work is to assess the timing of specific transfers and whether subsequent patient outcomes differ by transfer time-trends. It is also important to consider that a suboptimal patient transfer for one patient may be crucial for the care of the individual taking their bed space. Qualitative exploration to elucidate the challenges that bed managers face, around which literature is limited83. Our analysis therefore provides a starting point for identifying clusters of patients who have moved between unexpected pairs of wards, with a view to optimise pathways for future patients.
Conclusion
Routinely collected EHR data give us the opportunity to examine the true hospital usage and evaluate deviant patient journeys, which may otherwise go undetected. Atypical ward transfers are associated with a significant increase in the patient’s LOS, which is detrimental to both the individual and the wider health system. The physical movement, unfamiliarity between services, and treatment of the patient on a potentially mismatched ward may be factors contributing to this effect. The causes of atypical transfers, and the broader impact of patient movement must be better understood and considered in hospital policy and design. Our work provides an important first step in identifying unusual patient movement and its impacts.
Data availability
Data may be obtained from a third party and are not publicly available. Deidentified patient data cannot be made publicly available due to information governance restrictions. Access to the datasets used in this paper via a secure environment will be reviewed on request by Imperial College Healthcare NHS Trust. Applications for data access can be made to the iCARE team at imperial.dataaccessrequest@nhs.net.
References
‘What’s going on with A&E waiting times? The King’s Fund. https://www.kingsfund.org.uk/projects/urgent-emergency-care/urgent-and-emergency-care-mythbusters. Accessed 24 Jun 2022.
Kreindler, S. A. Planning without action and action without planning? Examining a regional health system’s efforts to improve patient flow, 1998–2013. Int. J. Health Plann. Manage. 33(1), e333–e343. https://doi.org/10.1002/hpm.2481 (2018).
Oredsson, S. et al. A systematic review of triage-related interventions to improve patient flow in emergency departments. Scand. J. Trauma Resusc. Emerg. Med. 19(1), 43. https://doi.org/10.1186/1757-7241-19-43 (2011).
Kreindler, S. A. Six ways not to improve patient flow: A qualitative study. BMJ Qual. Saf. 26(5), 388–394. https://doi.org/10.1136/bmjqs-2016-005438 (2017).
Abuhay, T. M., Mamuye, A., Robinson, S., & Kovalchuk, S. V. ‘Why Machine Learning Integrated Patient Flow Simulation?’ ArXiv210408203 Cs, Apr. 2021 https://doi.org/10.36819/SW21.041
Proudlove, N. C. The 85% bed occupancy fallacy: The use, misuse and insights of queuing theory. Health Serv. Manage. Res. 33(3), 110–121. https://doi.org/10.1177/0951484819870936 (2020).
Tlapa, D. et al. Effects of lean healthcare on patient flow: A systematic review. Value Health 23(2), 260–273. https://doi.org/10.1016/j.jval.2019.11.002 (2020).
Proudlove, N., Boaden, R. & Jorgensen, J. Developing bed managers: The why and the how. J. Nurs. Manag. 15(1), 34–42. https://doi.org/10.1111/j.1365-2934.2006.00632.x (2007).
Bristol, A. A., Schneider, C. E., Lin, S.-Y. & Brody, A. A. A systematic review of clinical outcomes associated with intrahospital transitions. J. Healthc. Qual. https://doi.org/10.1097/JHQ.0000000000000232 (2020).
Blay, N., Roche, M., Duffield, C. & Xu, X. Intrahospital transfers and adverse patient outcomes: An analysis of administrative health data. J. Clin. Nurs. 26(23–24), 4927–4935. https://doi.org/10.1111/jocn.13976 (2017).
Webster, J. et al. Effects of frequent PATient moves on patient outcomes in a large tertiary Hospital (the PATH study): A prospective cohort study. Aust. Health Rev. 40(3), 324–329. https://doi.org/10.1071/AH15095 (2016).
Kanak, M. F. et al. The effects of hospitalization on multiple units. Appl. Nurs. Res. 21(1), 15–22. https://doi.org/10.1016/j.apnr.2006.07.001 (2008).
McHaney-Lindstrom, M. et al. Analysis of intra-hospital transfers and hospital-onset Clostridium difficile infection. J. Hosp. Infect. 102(2), 168–169. https://doi.org/10.1016/j.jhin.2018.08.016 (2019).
Boncea, E. E. et al. Association between intrahospital transfer and hospital-acquired infection in the elderly: A retrospective case–control study in a UK hospital network. BMJ Qual. Saf. 30(6), 457–466. https://doi.org/10.1136/bmjqs-2020-012124 (2021).
Tahir, H. et al. Relevance of intra-hospital patient movements for the spread of healthcare-associated infections within hospitals: A mathematical modeling study. PLOS Comput. Biol. 17(2), e1008600. https://doi.org/10.1371/journal.pcbi.1008600 (2021).
Bristol, A. A. et al. Mixed-methods study examining family carers’ perceptions of the relationship between intrahospital transitions and patient readiness for discharge. BMJ Qual. Saf. https://doi.org/10.1136/bmjqs-2022-015120 (2022).
La Regina, M. et al. What quality and safety of care for patients admitted to clinically inappropriate wards: A systematic review. J. Gen. Intern. Med. 34(7), 1314–1321. https://doi.org/10.1007/s11606-019-05008-4 (2019).
Stylianou, N., Fackrell, R. & Vasilakis, C. Are medical outliers associated with worse patient outcomes? A retrospective study within a regional NHS hospital using routine data. BMJ Open 7(5), e015676. https://doi.org/10.1136/bmjopen-2016-015676 (2017).
Kohn, R. et al. Influence of bedspacing on outcomes of hospitalised medicine service patients: A retrospective cohort study. BMJ Qual. Saf. https://doi.org/10.1136/bmjqs-2019-010675 (2020).
Perimal-Lewis, L. et al. The relationship between in-hospital location and outcomes of care in patients diagnosed with dementia and/or delirium diagnoses: Analysis of patient journey. BMC Geriatr. 16(1), 190. https://doi.org/10.1186/s12877-016-0372-5 (2016).
Kreindler, S. A. et al. Working against gravity”: The uphill task of overcapacity management. Health Serv. Insights 13, 1178632920929986. https://doi.org/10.1177/1178632920929986 (2020).
Johnson, S. Emergence: The Connected Lives of Ants, Brains, Cities, and Software. Scribner, 2001.
Kannampallil, T. G., Schauer, G. F., Cohen, T. & Patel, V. L. Considering complexity in healthcare systems. J. Biomed. Inform. 44(6), 943–947. https://doi.org/10.1016/j.jbi.2011.06.006 (2011).
Cresswell, J. & Cresswell, D. Research Design: Qualitative, Quantitative & Mixed Methods Approaches (SAGE edge, 2018).
‘NHS England » NHS provider directory’. https://www.england.nhs.uk/publication/nhs-provider-directory/#i. Accessed 15 Aug 2023.
‘NHS Trust’. https://www.datadictionary.nhs.uk/nhs_business_definitions/nhs_trust.html. Accessed 15 Aug 2023.
Warren, L. R., Clarke, J., Arora, S. and Darzi, A. Improving data sharing between acute hospitals in England: An overview of health record system distribution and retrospective observational analysis of inter-hospital transitions of care’, Open Access, p. 8.
‘Treatment Function and Main Specialty Standard - NHS Digital - Citizen Space’. https://nhs-digital.citizenspace.com/standards-assurance/treatment-function-and-main-specialty-standard/. Accessed 17 Jul 2020.
Rhoades, S. A. Market share inequality, the HHI, and other measures of the firm-composition of a market. Rev. Ind. Organ. 10(6), 657–674. https://doi.org/10.1007/BF01024300 (1995).
Laakso, M. & Taagepera, R. “Effective” number of parties: A measure with application to West Europe. Comp. Polit. Stud. 12(1), 3–27. https://doi.org/10.1177/001041407901200101 (1979).
Yam, C. H., Wong, E. L., Chan, F. W., Wong, Leung, M. C. & Yeoh, E. Review Measuring and preventing potentially avoidable A R T I C L E hospital readmissions: A review of the literature’, p. 7.
VanderWeele, T. J. Principles of confounder selection. Eur. J. Epidemiol. 34(3), 211–219. https://doi.org/10.1007/s10654-019-00494-6 (2019).
Zhang, C., Eken, T., Jørgensen, S. B., Thoresen, M. & Søvik, S. Effects of patient-level risk factors, departmental allocation and seasonality on intrahospital patient transfer patterns: Network analysis applied on a Norwegian single-centre data set. BMJ Open 12(3), e054545. https://doi.org/10.1136/bmjopen-2021-054545 (2022).
Ruiz, M., Bottle, A., Long, S. & Aylin, P. Multi-morbidity in hospitalised older patients: Who are the complex elderly?. PLoS ONE 10(12), e0145372. https://doi.org/10.1371/journal.pone.0145372 (2015).
Abbott, T. E. F. et al. Frequency of surgical treatment and related hospital procedures in the UK: A national ecological study using hospital episode statistics. BJA Br. J. Anaesth. 119(2), 249–257. https://doi.org/10.1093/bja/aex137 (2017).
Agresti, A. & Tarantola, C. Simple ways to interpret effects in modeling ordinal categorical data. Stat. Neerlandica 72(3), 210–223. https://doi.org/10.1111/stan.12130 (2018).
Mize, T. D., Doan, L. & Long, J. S. A general framework for comparing predictions and marginal effects across models. Sociol. Methodol. 49(1), 152–189. https://doi.org/10.1177/0081175019852763 (2019).
‘margins.pdf’. Accessed 25 Apr 2022. [Online]. Available: https://cran.r-project.org/web/packages/margins/margins.pdf.
Mihaylova, B., Briggs, A., O’Hagan, A. & Thompson, S. G. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 20(8), 897–916. https://doi.org/10.1002/hec.1653 (2011).
Moran, J. L. & Solomon, P. J. A review of statistical estimators for risk-adjusted length of stay: Analysis of the Australian and new Zealand intensive care adult patient data-base, 2008–2009. BMC Med. Res. Methodol. https://doi.org/10.1186/1471-2288-12-68 (2012).
Arimie, C. O., Biu, E. O. & Ijomah, M. A. Outlier detection and effects on modeling. OALib 07(09), 1–30. https://doi.org/10.4236/oalib.1106619 (2020).
Gale, N. K., Heath, G., Cameron, E., Rashid, S. & Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 13(1), 117. https://doi.org/10.1186/1471-2288-13-117 (2013).
Doyle, L., McCabe, C., Keogh, B., Brady, A. & McCann, M. An overview of the qualitative descriptive design within nursing research. J. Res. Nurs. 25(5), 443–455. https://doi.org/10.1177/1744987119880234 (2020).
Hassan, T. Clinical decision units in the emergency department: Old concepts, new paradigms, and refined gate keeping. Emerg. Med. J. EMJ 20(2), 123–125. https://doi.org/10.1136/emj.20.2.123 (2003).
Song, H., Tucker, A. L., Graue, R., Moravick, S. & Yang, J. J. Capacity pooling in hospitals: The hidden consequences of off-service placement. Manag. Sci. https://doi.org/10.1287/MNSC.2019.3395 (2020).
Alameda, C. & Suárez, C. Clinical outcomes in medical outliers admitted to hospital with heart failure. Eur. J. Intern. Med. 20(8), 764–767. https://doi.org/10.1016/j.ejim.2009.09.010 (2009).
Goulding, L., Adamson, J., Watt, I. & Wright, J. Lost in hospital: A qualitative interview study that explores the perceptions of NHS inpatients who spent time on clinically inappropriate hospital wards. Health Expect. 18(5), 982–994. https://doi.org/10.1111/hex.12071 (2015).
Caldicott, C. V., Dunn, K. A. & Frankel, R. M. Can patients tell when they are unwanted? “Turfing” in residency training. Patient Educ. Couns. 56(1), 104–111. https://doi.org/10.1016/j.pec.2003.12.014 (2005).
Kreindler, S. A. et al. ‘Can facility-based transitional care improve patient flow? Lessons from four Canadian regions’. Healthc. Manag. Forum. https://doi.org/10.1177/0840470421995934 (2021).
Kreindler, S. et al. ‘How do health systems address patient flow when services are misaligned with population needs? A Qualitative Study. Int. J. Health Policy Manag. https://doi.org/10.34172/ijhpm.2021.36 (2021).
Anwar, M. R. et al. Realist analysis of streaming interventions in emergency departments. BMJ Lead. https://doi.org/10.1136/leader-2020-000369 (2021).
Kulshrestha, A. & Singh, J. Inter-hospital and intra-hospital patient transfer: Recent concepts. Indian J. Anaesth. 60(7), 451–457. https://doi.org/10.4103/0019-5049.186012 (2016).
Uhrenfeldt, L. et al. A qualitative meta-synthesis of patients’ experiences of intra- and inter-hospital transitions. J. Adv. Nurs. 69(8), 1678–1690. https://doi.org/10.1111/jan.12134 (2013).
Tadd, W. et al. From right place—wrong person, to right place—right person: Dignified care for older people. J. Health Serv. Res. Policy 17(2_suppl), 30–36. https://doi.org/10.1258/jhsrp.2011.011118 (2012).
Abraham, J. & Reddy, M. C. Challenges to inter-departmental coordination of patient transfers: A workflow perspective. Int. J. Med. Inf. 79(2), 112–122. https://doi.org/10.1016/j.ijmedinf.2009.11.001 (2010).
Cleak, H., Osborne, S. R. & de Looze, J. W. M. Exploration of clinicians’ decision-making regarding transfer of patient care from the emergency department to a medical assessment unit: A qualitative study. PLoS ONE 17(2), e0263235. https://doi.org/10.1371/journal.pone.0263235 (2022).
Germack, H. D. et al. Cooperation and conflict in intra-hospital transfers: A qualitative analysis. Nurs. Open 7(2), 634–641. https://doi.org/10.1002/nop2.434 (2020).
Ernst, K. M., McComb, S. A. & Ley, C. Nurse-to-nurse shift handoffs on medical-surgical units: A process within the flow of nursing care. J. Clin. Nurs. 27(5–6), e1189–e1201. https://doi.org/10.1111/jocn.14254 (2018).
Hilligoss, B. & Cohen, M. D. The unappreciated challenges of between-unit handoffs: Negotiating and coordinating across boundaries. Ann. Emerg. Med. 61(2), 155–160. https://doi.org/10.1016/j.annemergmed.2012.04.009 (2013).
Baek, H. et al. Analysis of length of hospital stay using electronic health records: A statistical and data mining approach. PLoS ONE 13(4), e0195901. https://doi.org/10.1371/journal.pone.0195901 (2018).
Fan, R. L., Zhao, M. & Peng, D. X. Differentiating interhospital transfer types: Varied impacts and diverging coordination strategies. Prod. Oper. Manag. 30(10), 3657–3678. https://doi.org/10.1111/poms.13455 (2021).
Mueller, S., Zheng, J., Orav, E. J. & Schnipper, J. L. Inter-hospital transfer and patient outcomes: A retrospective cohort study. BMJ Qual. Saf. 28(11), e1–e1. https://doi.org/10.1136/bmjqs-2018-008087 (2019).
Allen, D. Inside “bed management”: Ethnographic insights from the vantage point of UK hospital nurses. Sociol. Health Illn. 37(3), 370–384. https://doi.org/10.1111/1467-9566.12195 (2015).
Honeyford, K. et al. Challenges and recommendations for high quality research using electronic health records. Front. Digital Health https://doi.org/10.3389/fdgth.2022.940330 (2022).
Malterud, K., Siersma, V. D. & Guassora, A. D. Sample Size in Qualitative interview studies: Guided by information power. Qual. Health Res. 26(13), 1753–1760. https://doi.org/10.1177/1049732315617444 (2016).
Atiomo, W., Weir, P. & Kean, L. Impact of new clinical policies during the COVID-19 pandemic on clinical incidents and complaints at a UK teaching hospital. Int. J. Environ. Res. Public Health 18(8), 3979. https://doi.org/10.3390/ijerph18083979 (2021).
Denning, M. et al. What has been the impact of Covid-19 on safety culture? A case study from a large metropolitan healthcare trust. Int. J. Environ. Res. Public Health 17(19), 7034. https://doi.org/10.3390/ijerph17197034 (2020).
Bean, D. M., Stringer, C., Beeknoo, N., Teo, J., Dobson, R. J. B.‘Network analysis of patient flow in two UK acute care hospitals identifies key sub-networks for A&E performance’, p. 21.
Kohler, K. & Ercole, A. Can network science reveal structure in a complex healthcare system? A network analysis using data from emergency surgical services. BMJ Open 10(2), e034265. https://doi.org/10.1136/bmjopen-2019-034265 (2020).
Chong, J. L., Lim, K. K. & Matchar, D. B. Population segmentation based on healthcare needs: A systematic review. Syst. Rev. 8(1), 202. https://doi.org/10.1186/s13643-019-1105-6 (2019).
Vuik, S. I., Mayer, E. K. & Darzi, A. Patient segmentation analysis offers significant benefits for integrated care and support. Health Aff. 35(5), 769–775. https://doi.org/10.1377/hlthaff.2015.1311 (2016).
Aitchison, K. et al. Population child health: Understanding and addressing complex health needs. Arch. Dis. Child. 106(4), 387–391. https://doi.org/10.1136/archdischild-2019-317373 (2021).
Clegg, A. et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 45(3), 353–360. https://doi.org/10.1093/ageing/afw039 (2016).
Vuik, S. I., Mayer, E. & Darzi, A. A quantitative evidence base for population health: Applying utilization-based cluster analysis to segment a patient population. Popul Health Metrics https://doi.org/10.1186/s12963-016-0115-z (2016).
‘Health Infrastructure Plan: A new, strategic approach to improving our hospitals and health infrastructure’, Department of Health and Social Care. [Online]. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/835657/health-infrastructure-plan.pdf
‘A&E: Move patients to wards regardless of bed capacity, to spread risk, says royal college | The BMJ’. https://www.bmj.com/content/379/bmj.o2557?utm_source=etoc&utm_medium=email&utm_campaign=tbmj&utm_content=weekly&utm_term=20221028. Accessed 02 Nov 2022.
‘Should emergency departments move patients to other wards even when there’s no bed space available? The Nuffield Trust, Oct. 13, 2022. https://www.nuffieldtrust.org.uk/news-item/should-emergency-departments-move-patients-to-other-wards-even-when-there-s-no-bed-space-available. Accessed 02 Nov 2022.
Vaughan, L. K. & Bruijns, S. Continuous flow models in urgent and emergency care. BMJ 379, 02751. https://doi.org/10.1136/bmj.o2751 (2022).
McMurdo, M. E. T. & Witham, M. D. Unnecessary ward moves. Age Ageing 42(5), 555–556. https://doi.org/10.1093/ageing/aft079 (2013).
Tolentino, J. C. et al. Adverse events during intrahospital transfers: Focus on patient safety. In Vignettes in Patient Safety—Volume 3 (eds Stawicki, S. P. & Firstenberg, M. S.) (InTech, 2018). https://doi.org/10.5772/intechopen.76777.
Bonnici, K. et al. Learning from critical care: Improving intra- and inter-hospital transfer processes in enhanced care and the ward. Fut. Healthc. J. 7(3), 214–217. https://doi.org/10.7861/fhj.2019-0063 (2020).
Murata, M. et al. Adverse events during intrahospital transport of critically ill patients: A systematic review and meta-analysis. Am. J. Emerg. Med. 52, 13–19. https://doi.org/10.1016/j.ajem.2021.11.021 (2022).
Benjamin, E. Understanding the work and decision-making strategies of bed management nurses: A systematic review. Nurs. Manag. Harrow Lond. Engl. 29(2), 25–31. https://doi.org/10.7748/nm.2021.e2016 (2021).
Acknowledgements
This research has been completed using the National Institute for Health Research Health Informatics Collaborative (NIHR HIC) data resources and supported by the Imperial Clinical Analytics Research and Evaluation (iCARE) team. Data management (and analytical support) was provided by the Big Data and Analytical Unit (BDAU) at the Institute of Global Health Innovation (IGHI). Imperial College London is grateful for the support from the North West London NIHR Applied Research Collaboration. We thank Dr Erik Mayer and Dr Benjamin Post for the helpful discussions on the data analysis and clinical interpretation of the findings.
Disclaimer
This study is partially funded by the NIHR Applied Research Collaboration Northwest London. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Funding
This research was co-funded by the National Institute for Health Research (NIHR) Imperial Biomedical Research Centre (BRC) and the Economic and Social Research Council (ESRC). EM is supported by the ESRC (Grant number ES/P000703/1) as part of the ESRC London Interdisciplinary Social Science Doctoral Training Partnership. PE is partially supported by the National Institute for Health Research (NIHR) Imperial Biomedical Research Centre (BRC) (Grant number NIHR-BRC-P68711). KH is supported by the NIHR [HS&DR] Project: NIHR129082.
Author information
Authors and Affiliations
Contributions
E.M., P.E. and C.C. conceptualised the research question. E.M., overseen by P.E. and C.C., conducted the data analysis. E.M. wrote and revised the manuscript. L.M. conducted the data curation and anonymisation K.H., A.B., R.E.K., provided expert advice and critical review of the paper prior to submission. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mendelsohn, E., Honeyford, K., Brittin, A. et al. The impact of atypical intrahospital transfers on patient outcomes: a mixed methods study. Sci Rep 13, 15417 (2023). https://doi.org/10.1038/s41598-023-41966-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-41966-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.