Abstract
The COVID-19 pandemic has had a devastating impact on the health and wellbeing of the global population. This paper presents the results of a longitudinal transcultural study that was begun at the peak of the pandemic (in April, 2020). An online survey was used to collect data from English-, Spanish-, and Portuguese-speaking participants. The survey collected information about sociodemographics, lifestyle activities, COVID-19-related circumstances, and drug use (with an emphasis on hallucinogenic drugs), as well as involving psychometric questionnaires. Users of hallucinogenic drugs had higher psychological well-being and lower scores on psychopathology scales, both at baseline and during follow-ups. This difference was larger when users were distinguished by frequency of use, as regular users scored higher on psychological well-being and lower on psychopathology scales. Subjects with more psychological distress had lower scores for all scales of post-traumatic growth, but if they were regular hallucinogens users, they had higher scores for post-traumatic growth. When comparing the results between cultural contexts, heterogeneous results were obtained. There were more English-speaking regular users of hallucinogenic drugs. Further research should analyse the potential role of hallucinogens in large-scale catastrophes, with a special focus on post-traumatic growth.
Similar content being viewed by others
Introduction
The current public health concern brought about by the global COVID-19 crisis is more related with mental health rather than infectious diseases1. This is a consequence of the various challenging situations that populations around the globe are facing: the fear of the virus itself and the adverse health consequences if one is infected, the stigma experienced by certain groups that are in greater contact with the virus, the economic recession and unemployment, the bereavement of people who lost loved ones, and the lockdowns involving long-lasting social isolation, among other challenges.
Some countries duplicated the figures of mental health problems, and the numerous studies that are being published show increased anxiety, depression, post-traumatic stress disorder (PTSD), and general distress in the general population2. For instance, the Organization for Economic Cooperation and Development (OECD) recently reported that, since March 2020, the prevalence of anxiety and depression has increased and, in some countries, doubled. Additionally, the periods when the highest rates of mental distress were reported correlated with periods of marked increases in COVID-19 deaths and strict confinement measures3.
During the last decade, psychedelic drugs have been proposed as safe and efficacious tools for the treatment of mental disorders, including depression, anxiety, and PTSD4,5. There are at least two hallucinogens that are in Phase-III clinical trials for treatment-resistant depression and PTSD: psilocybin (the main alkaloid of Psilocybe cubensis) and 3,4-Methylenedioxymethamphetamine (MDMA), respectively. Certain countries have approved the use of these drugs in the framework of programs supporting compassionate use, including Canada, Israel, and the United States6,7,8,9. Both Australia and United States have allocated public funds to perform clinical trials with hallucinogens10,11. At the same time, a group of leading experts in the field of psychedelic research is recommending the use of such drugs to counter the mental health consequences of the pandemic12,13.
Many studies have been conducted on the effect of attending ceremonies involving psychoactive ethnobotanicals like ayahuasca on mental health14,15. Reported benefits relate to the grieving process16,17, emotional regulation18, mood19, drug use20 and general health21,22. Epidemiological studies about psychedelic use in the general population have also been performed, analysing government databases of health profiles of different populations, with results showing less domestic violence23,24, fewer suicide attempts25,26,27,28,29,30, and better general psychopathology31,32 among psychedelic users. According to the research, it can be hypothesized that psychedelic use may be a protective factor, rather than a risk factor, for mental health problems in the current situation, where a combination of pandemic-related factors threaten mental health13,21.
To date, few studies have been performed regarding the possible role of psychedelic use in preventing/treating mental health issues related to the COVID-19 pandemic. However, there is increasing interest in that regard33. Two retrospective observational studies have been published. The first one found that lifetime use of psychedelics was associated with better mental health during the COVID-19 pandemic34. The other one, a cross-sectional study performed by our group, further supported that finding35. Both studies were retrospective, so a direct causal relation could not be established. The current study includes the follow-ups with our previous sample35 at 2 and 6 months after baseline, aiming to provide a longitudinal assessment in order to determine whether better outcomes among regular users of psychedelics are stable over the long term.
Materials and methods
This study was approved by the Research Ethics Committee of the Universidad Autónoma de Madrid (Autonomous University of Madrid, Spain). All experimental procedures were performed in accordance with the relevant guidelines and regulations, and all respondents provided informed consent.
Sample
This longitudinal study recruited a total of 2971 subjects for the baseline assessment, 1024 subjects for the first follow-up performed two months later, and 455 subjects for the last follow-up, performed six months after the baseline assessment. All participants were asked to complete an online survey specifically developed for this study. The survey was originally developed in Spanish and then translated into Portuguese and English for international dissemination. The first assessment was launched while the populations of most Western countries were confined to their homes (April 7th, 2020), whereas distinct confinement measures were in place in different countries during both follow-ups. Through snowball sampling, researchers from various countries, including mainly Spain and Brazil, spread the questionnaires among direct contacts and through social media. The questionnaire was also shared on the websites of the Mental Health Post-graduate Program of the Ribeirão Preto Medical School at the University of São Paulo, in the scientific journal Archives of Clinical Psychiatry, and on websites offering information about psychedelics and cannabis (Lasdrogas.info, Cannabis Magazine, social media pages of ICEERS and local community websites). It was not mentioned in the instructions nor anywhere else in the survey that the study was investigating relationships between hallucinogenic drug use and other variables.
Psychometric measures
The following validated questionnaires were included in the survey, as described previously in more detail35. First, the General Health Questionnaire (GHQ-12) was used to screen for psychological distress at all time points in its validated Spanish (α = 0.86–0.90)36, English (α = 0.82–0.86)37, and Portuguese (α = 0.83–0.86)38 versions. A higher score represents greater psychological distress.
We also used the Brief Symptom Inventory (BSI) in its validated English (α = 0.87–0.98)39, Portuguese (α = 0.73–0.88)40, and Spanish (α = 0.69–0.85)41 versions. The nine sub-scales (somatization, SOM; obsessive–compulsive, O–C; interpersonal sensitivity, IS; depression, DEP; anxiety, ANX; hostility, HOST; phobic anxiety, PHOB; paranoid ideation, PAR; and psychoticism, PSY) and the General Severity Index (GSI) were used, with higher scores indicating more severe symptoms. A T-score above 70 for each sub-scale and a score of 63 or above for the GSI indicate a clinical case.
Further, we used the Peritraumatic Stress Inventory (PSI) at baseline only. The PSI is a proposed measure of post-traumatic stress disorder (PTSD); that is, it measures symptoms associated with exposure to a potentially traumatic experience. The validated English version (α = 0.75–0.76)42 was used. The questionnaire was translated into Spanish and Portuguese by native Spanish and Portuguese researchers, respectively. Higher scores represent more intense symptoms resulting from exposure to potentially traumatic experiences.
Lastly, the Post-traumatic Growth Inventory (PGI) was also included in the two follow-up questionnaires, in its validated English (α = 0.90)43, Portuguese (α = 0.95)44, and Spanish (α = 0.95)45 versions. This provides a measure of positive changes perceived by the subject following a traumatic event. It contains five sub-scales (relationships, new possibilities, personal change, spiritual change, and life appreciation). Higher scores represent more post-traumatic growth (PTG).
Hallucinogenic drug use
Participants were asked about their use of psychedelic drugs. We included the use of these psychedelic drugs: MDMA, ayahuasca, psilocybin-containing mushrooms, LSD, peyote, San Pedro, Incilius alvarius or 5-MeO-DMT, changa, and other psychedelics, as described previously46. Only at baseline, we categorized participants as (a) regular users (more than once per 6 months), (b) occasional users (tried it, but do not use it regularly), and (c) never-users. At the follow-ups, participants indicated whether they used each drug more often, less often, or the same as before.
At baseline, we also asked for the settings in which participants were using psychedelic drugs: alone, with friends or a partner, at parties or festivals, at rituals or in a therapeutic setting, or microdosing. We only added MDMA to the list of psychedelic drugs when it is used at rituals or in therapeutic settings. Furthermore, we assumed that this context remained the same throughout follow-up.”
Other COVID-19 related indicators
We asked whether persons were diagnosed with COVID-19 or showed COVID-like symptoms, and whether they were still confined. We asked whether participants felt reluctant or afraid to leave their homes and about changes in their relationships, domestic conflicts, and employment/finances.
Additionally, subjects were asked about their lifestyle and the activities they were engaging in during confinement, including aerobic exercise; martial arts; music and singing; playing videogames; watching pornography; reading; watching TV, movies, series, or COVID-19 related news; weightlifting or bending; yoga; Pilates; and meditation. We also assessed changes in health habits since confinement.
We asked about medication use (with and without prescription), the doctors participants had seen during confinement, and whether they started any psychological therapy. We also asked them to rate their psychological well-being and their family environment during confinement on a scale from 1 to 10, with 1 indicating the worst and 10 the best score.
Covariates
We recorded age, gender (male vs. female vs. others), and the language of the participant (Spanish, English, or Portuguese). For each participant, we recorded their partner status (yes/no). We asked for their religion (subsequently classified as atheist, agnostic, or religious) and whether they practice their religion. Each person was asked whether they had any physical or psychological conditions.
At each time point, we defined non-hallucinogenic drugs as alcohol, tobacco, cannabis, cocaine, amphetamines, and MDMA when not used in rituals or therapeutic settings.
Statistical analysis
All variables were described as percentages or means and standard deviations. Sample characteristics are described at baseline, and at 2 and 6 months. We first did this analysis for the sociodemographic factors, religion, health factors, and substance use. Then we did the same for all COVID-19-related factors.
Next, in order to determine longitudinal associations between psychedelic drug users vs. non-users and the psychometric measures, we used generalized estimating equations (GEE) with an exchangeable correlation structure, which takes into account within-person correlations when examining multiple observations per subject and can handle missing values46. As dependent variables, we took these into account: (a) COVID-19-related items regarding psychological wellbeing, the home environment, and information given by politicians or the media, all items are unstandardized and rated on a scale of 1–10; (b) psychological distress (measured by the GHQ); (c) nine BSI scales and the GSI; and (d) five PTG scales. We performed the same analyses at baseline with regular vs. occasional vs. never users of psychedelic drugs as an independent variable, using the same set of psychometric measures as dependent variables. We corrected all these GEE models directly for age, gender, language of questionnaire, religion, practitioner of religion, and alcohol, tobacco, cannabis, cocaine, or amphetamine use, as described previously35.
Subsequently, we performed GEE analyses with peritraumatic stress, the GSI, psychological distress (GHQ), and occasional vs. never and regular vs. never users of psychedelic drugs as independent variables, and the five PTG scores as dependent variables. We corrected for age, gender, language of questionnaire, and religion. Cronbach’s Alpha was calculated for all the questionnaires used.
All analyses were conducted using SPSS version 24.0 (IBM Corp., Armonk, NY, USA). After Bonferroni-correction (p-value of 0.05 divided by 20), we set the significant p-value at 0.003, two-tailed.
Results
Reliability of questionnaires used
GHQ-12 questionnaire showed a Cronbach’s Alpha of 0.87, 0.89, and 0.89 for English, Portuguese, and Spanish versions, respectively. BSI questionnaire showed a Cronbach’s Alpha of 0.96, 0.97, and 0.96 for English, Portuguese, and Spanish versions, respectively. PSI questionnaire showed a Cronbach’s Alpha of 0.89, 0.82, and 0.85 for English, Portuguese, and Spanish versions, respectively. Lastly, PGI showed a Cronbach’s Alpha of 0.95, 0.94, and 0.95 for English, Portuguese, and Spanish versions, respectively.
Sample characteristics and COVID-related items
Table 1 shows the sample characteristics at baseline, and at the 2 and 6-month follow-ups, while Table 2 shows COVID-related items at all time points. According to the epidemiological data, the number of participants who tested COVID-positive increased across the three assessments. Whereas 47% were confined at 2 months, 86% were confined at 6 months. The percentage of the sample in isolation increased as well, from 55.8% at 2 months to 74.1% at 6 months. Regarding personal income, nearly 50% of the sample experienced a reduction in the first weeks of the pandemic, while at 6 months only 33.4% of the sample indicated a reduction in income.
A general increase in the frequency of engaging with different lifestyle activities during confinement can be observed, especially in terms of aerobic exercise, martial arts, music and singing, and reading. There was an increase in watching pornography as well. A general decrease was observed in the case of yoga, Pilates, and meditation.
As can be seen in Fig. 1, at the first follow-up, there was a general and marked increase in alcohol, tobacco, and cannabis use, while the most relevant drug use decrease occurred in the cases of amphetamines, MDMA, and ayahuasca. At the 6-month follow-up, the numbers were very similar, although the alcohol use did not increase as in the previous assessments.
After 2 months, persons with missing values were less often regular psychedelic users (14.9%) than in the persons with recorded data (20.1%), and the drop-outs scored higher on hostility (58.4 vs 57.2), and psychoticism (57.0 vs. 55.7). After 6 months, drop-outs scored lower on psychological well-being (5.8 vs. 5.9).
Hallucinogenic drugs and psychometric measures
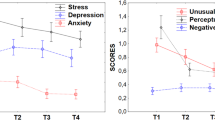
Among the sample, there was a general decrease in BSI scores across the follow-ups (see Supplementary Table 4), suggesting that stress peaked at the beginning of the pandemic and the associated lockdown measures. The use of hallucinogenic drugs over time was significantly associated with higher psychological wellbeing (B = 0.48; SE = 0.10; p < 0.001), and lower rates on the information given by the media (B = − 0.44; SE = 0.10; p < 0.001), as shown in Table 3. Hallucinogenic drug use was also associated with less psychological distress (B = − 0.73; SE = 0.16; p < 0.001), fewer obsessions or compulsions (B = − 1.82; SE = 0.40; p < 0.001), less depression (B = − 1.43; SE = 0.45; p = 0.001), less hostility (B = − 1.13; SE = 0.35; p = 0.001), less phobic anxiety (B = − 1.93; SE = 0.40; p = < 0.001), less paranoid ideation (B = − 1.24; SE = 0.36; p = 0.001), less psychoticism (B = − 1.02; SE = 0.32; p = 0.001), and lower GSI scores (B = − 0.76; SE = 0.22; p = 0.001). Regarding the PTG scores, psychedelic drug use was associated with higher scores on the new possibilities scale (B = 1.79; SE = 0.55; p = 0.001).
When we examined the frequency of hallucinogenic drug use, regular users scored higher in terms of psychological wellbeing, and lower in terms of information given by the media and psychological distress. Regular users of hallucinogens had lower BSI scores, excluding GSI. Regular hallucinogenic drug use was associated with higher scores on the new possibilities and spiritual change scales of PTG.
Stress, psychedelic drugs and posttraumatic growth
Table 4 shows the longitudinal analyses between various psychometric measures, psychedelic drugs, and the five scales of PTG. When entered into a multivariable model, psychological distress was independently associated with lower scores on all five scales, while regular psychedelic use was associated with higher scores on the PTG scales. See Fig. 2 for a graphical representation of the corrected means of the five PTG scores for never, occasional, and regular users of psychedelic drugs.
Means of five scales of posttraumatic growth among hallucinogenic drug users: never users (white) vs. occasional users (grey) vs. regular users (black), while correcting for age, gender, language of questionnaire, religion, peritraumatic stress score, general severity index, and psychological distress scores.
Transcultural comparison
Supplementary Tables 1, 2 and 3 show the differences between the three languages in which the questionnaires were completed. At all three time points, there were significant differences between the English, Spanish, and Portuguese speakers in their rating of the information given by the media and politicians, their stress levels, BSI scores, and the use of psychedelic drugs. Results were heterogeneous, and no clear tendency can be observed.
Discussion
In this manuscript, we explore the relationship between hallucinogen use and different variables, including mental health and well-being, peritraumatic stress, and PTG. This study was initiated during a global pandemic, when many countries were implementing confinement measures.
Results showed that lifetime use of hallucinogens was related to better scores on most of the measures and that regular users had lower scores on each of the psychopathology scales. Regular users of hallucinogens also had higher PTG scores than occasional or never users, even after the multivariate longitudinal analysis corrected for various psychological measures. Within the multivariate model, it can be observed that as scores for psychological distress (GHQ-12) increased, lower scores on PTG were obtained, indicating that as distress reaches higher levels, there is a decrease of growth associated with such distress. It should be noted that both psychological distress and regular use of hallucinogens were independently associated with PTG.
Some important questions related to clinical and public policy arise from our results. Contrary to the presumptions that justify hallucinogens being scheduled substances (i.e., causing harm to health and having a high abuse potential), our results show that they might offer some kind of protection of mental health when confronting highly stressful situations, like facing a pandemic where most of the world’s population is suffering unprecedented deaths and strict lockdowns. Another retrospective, transversal study (n = 5618), performed at the same time as our study, also found a relationship between lifetime use of hallucinogens and lower scores on dimensions linked to mental health impairment (state/trait anxiety, negative affect), as well as higher scores on dimensions linked to well-being and resilience (mainly positive affect, autonomy, social ties, and wellbeing)34. Other cohort studies have found positive relationships between lifetime use of hallucinogens and mental health27,32,47,48, and negative relationships between hallucinogenic drug use and suicidality26,49 and violence50,51. Additionally, there are numerous published manuscripts reporting the positive effects of hallucinogens on mental health in clinical settings (for reviews, see Goldberg et al.52; Luoma et al.53; and Yu et al.54) and in ceremonies where hallucinogens were administered15,20,55,56,57. Lastly, cross-sectional studies comparing regular hallucinogen users with non-users have found an absence of neuropsychiatric impairments in the former, with users reporting better scores than non-users on some measures31,58,59,60,61.
In a previous manuscript, we hypothesized that regular hallucinogen use could be a protective factor when confronting stressful situations21. The pandemic offered an unfortunate but appropriate scenario in which to test our hypothesis, and the results were in line with it: lifetime hallucinogen use was related longitudinally with positive outcomes in terms of most of the mental health measures. Moreover, regular use of hallucinogenic drugs was specifically associated with higher scores on the PTG scales (relating to others, new possibilities, personal strength, spiritual change, and appreciation of life). In relation to that, another manuscript focused on coping strategies and use of hallucinogens showed that regular users of these drugs are more prone to use adaptive coping strategies62. This is highly relevant in the context of the recently published research on the potential of MDMA for the treatment of PTSD63. PTG reflects an adaptive process of adjustment, and it is positively correlated with resiliency, meaning-making regarding the traumatic event, and functional relationships. Thus, PTG is an indicator of a holistic process of change following a traumatic event54,64. It is worth noting that we should be prevented of labeling the pandemic experience as a traumatic for everyone. Instead, the measure of PTG can be interpreted as an indicator of resilience, or positive-biased personal changes that can occur in generally significant experiences. There are only a couple of research reports that have assessed PTG in the context of MDMA-assisted psychotherapy64,65. Our current results add evidence to these emerging findings, extending from MDMA to the whole class of hallucinogenic drugs, suggesting that the effects of MDMA on PTG may be a non-specific feature of hallucinogenic drugs regarding the treatment of trauma.
The hallucinogenic experience produced by drugs like psilocybin and ayahuasca has been characterized as spiritual and/or mystical66,67. Commonly, the phenomenon so-called “ego dissolution” occurs68, and personal insights can emerge, providing subjects with new perspectives about themselves, their relationships, and the nature of reality69. These features tend to be conceived of as positive, leading to transformative and valuable experiences. However, psychedelic experiences can also be extremely stressful70,71,72,73,74. Despite this, it is common for users to continue taking these drugs after having experienced certain adverse effects, especially in the case of ayahuasca75. It is possible, therefore, that the willingness that users tend to show toward exposing themselves to highly challenging experiences is somehow related to their better PTG scores. In addition, this continuous exposure to challenging experiences could have provided personal resources to deal with pandemic stress, partially explaining the better scores on mental health and well-being they showed in different studies34,62. Previous research has shown different personality traits between hallucinogenic drug users and non-users, especially in the case of ayahuasca, as well as differences between users depending on the environment in which they live31,76. These differences may provide possible explanations for our findings. Taking into account the hierarchical order of psychological variables suggested by some authors34, we observe that personality domains influence on cognitive styles, which are responsible for interpreting and processing reality. These interpretations, in turn, affect emotions, and emotional states contribute to complex self-perceived processes that we conceptualize as well-being or resilience. Therefore, the ability of psychedelics to modulate personality traits, particularly openness and self-transcendence35,75, may be at the core of a "cascade" of subsequent psychological changes that eventually result in protective effects against various stressors, including pandemic-related stress. Further research in that regard is warranted.
Another remarkable result was the association between regular use of hallucinogens and lower psychopathology scores. The public image of hallucinogens has associated their use with madness and bizarre behaviors. In addition, hallucinogenic drugs have been used to mimic psychotic states77. Nevertheless, our results, in concordance with recent research on hallucinogens78, show that the use of these drugs is associated with less psychopathology and with functional behaviors. Many variables could be intertwined with these outcomes. For instance, in the case of the present study, regular users of hallucinogenic drugs also showed an enhanced detachment from the information given by politicians and the media, which has been repeatedly related to higher distress scores during the initial waves of the pandemic79,80. Remarkably, a recently published preclinical study suggested that the use of ayahuasca could have a prophylactic effect in front of depressive symptoms81. Thus, a similar mechanism might be responsible for the present findings.
Due to our social responsibility as scientists, we must emphasize the policy implications of these results. Most classical hallucinogens (LSD, psilocybin, DMT or MDMA) are in the Schedule I of the United Nations (UN) Convention on Psychotropic Drugs of 1971 for their severe health risks. Although drugs included in the Schedule I are only allowed to be used for medical and scientific purposes, their use in non-medical settings has remained highly prevalent in Western countries. Notably, scientists are asking for the reclassification of these substances82,83 given the emerging body of evidence, which the present study strengthens by showing the positive consequences of their use in both informal and experimental settings. A policy that it is not aligned with scientific evidence should be changed for the benefit of society. Good examples of this proposed change include local public policies like the one developed in Alberta (Canada), Oregon (USA) or in Catalonia, where the local government adopted a harm reduction approach regarding the extended use of ayahuasca84.
The most relevant limitation of this study was the high drop-out rate during the follow-ups of this study, a limitation that tends to occur in longitudinal studies. Although characteristics like age, gender, and marital status remained the same in each assessment, this drop-out rate might have affected some other characteristics of the sample, giving the longitudinal analyses limited reliability. For instance, the percentage of users of hallucinogenic drugs in the sample dropped considerably across the follow-ups. Nevertheless, in terms of the English version of the questionnaire, the majority of the participants in both follow-ups were users of hallucinogenic drugs, as they were possibly more motivated to answer a survey in which they were asked about their use of hallucinogens. One additional limitation of our study is the comparison of subjects between different language versions of the questionnaire (English, Portuguese, and Spanish), rather than comparing subjects between countries. The latter option would have been challenging due to our sample being provided by individuals from more than 80 countries. However, we opted to group Portuguese-speaking individuals from both Portugal and Brazil, as well as Spanish-speaking individuals from both Spain and South American countries. It is important to note that the reality of the pandemic may have varied substantially in these different regions. Lastly, self-report measures have inherent limitations and may be influenced by biases, such as individuals who already perceive consumption of psychedelic drugs positively. We employed validated assessment tools to minimize subjective interpretation and increase the reliability of our findings, but the results have to be interpreted with caution.
One of the main inspirations for the design of this study was the uncommon scenario of widespread social isolation during confinement measures. While this scenario provided an interesting object of study, it could also be seen as an extraneous variable, since we presume that confinement measures could have affected the number of people who answered the survey. At the baseline assessment, nearly all countries that participants were from were in strict lockdown (97% of the sample were confined), whereas at the second and third assessments, 47% and 85.5% of participants were confined, respectively. Especially during the third assessment, six months after the first (in October, 2020), most countries developed other less strict measures, avoiding complete confinement precisely due to the psychological consequences observed. However, the majority of our sample at this assessment reported being confined (85.5%, which is in line with the high score obtained on the GSI in the last follow-up, as reported in Supplementary Table 4, suggesting that confinement is closely linked with psychological distress). Thus, it is possible that people in confinement were more likely to take 20–30 min to answer an online survey, biasing the results of the study toward confined people.
Conclusions
Users of hallucinogenic drugs scored better on various dimensions that were clearly affected by the recent COVID-19 pandemic, like psychopathology, wellbeing, and post-traumatic growth. This was even clearer in the case of regular users of these drugs. From these results, we can suggest that either these drugs exert certain effects on individuals that protect them against some of the distress of life-changing events, or people who use these drugs do so because they have traits that are related to the better management of stressful events. Overall, these findings have public policy implications that should be addressed. Further research should elucidate the role of hallucinogenic drugs in large-scale catastrophes, such as pandemics and wars.
Data availability
The raw data is available upon request to Dr. JC Bouso, corresponding author.
References
de Vicente, A., Villamarín, S. & Berdullas, S. En Portada: La Nueva Pandemia Psicológica. Infocop. 93, 3–7 (2021).
Rajkumar, R. P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 52, 102066 (2020).
OECD. Tackling the mental health impact of the COVID-19 crisis: An integrated, whole-of-society response. 2021. https://read.oecd-ilibrary.org/view/?ref=1094_1094455-bukuf1f0cm&title=Tackling-the-mental-health-impact-of-the-COVID-19-crisis-An-integrated-whole-of-society-response (accessed 13 June 2022).
Dos Santos, R. G., Bouso, J. C., Alcázar-Córcoles, M. Á. & Hallak, J. E. C. Efficacy, tolerability, and safety of serotonergic psychedelics for the management of mood, anxiety, and substance-use disorders: A systematic review of systematic reviews. Expert Rev. Clin. Pharmacol. 11(9), 889–902 (2018).
Dos Santos, R. G., Bouso, J. C., Rocha, J. M., Rossi, G. N. & Hallak, J. E. The use of classic hallucinogens/psychedelics in a therapeutic context: Healthcare policy opportunities and challenges. Risk Manag. Healthc. Policy. 14, 901–910 (2021).
Efrati, I. Party Drug or Breakthrough Treatment? Israel Approves Compassionate Use of MDMA to Treat PTSD. Haaretz, 2019. https://www.haaretz.com/science-and-health/.premium-israel-s-health-ministry-approves-compassionate-use-of-mdma-to-treat-ptsd-1.6918710 (accessed 13 June 2022).
Greif, A. & Šurkala, M. Compassionate use of psychedelics. Med. Health Care Philos. 23(3), 485–496 (2020).
Jackson, P. Canada approves psilocybin for compassionate use in four patients. The Telegram. August 5, 2020. https://www.saltwire.com/newfoundland-labrador/news/local/canada-approves-psilocybin-for-compassionate-use-in-four-patients-481846/ (accessed 13 June 2022).
MAPS. Expanded Access Program: MDMA-Assisted Therapy for PTSD. 2019. https://maps.org/research/mdma/ptsd/expanded-access (accessed 13 June 2022).
Landis-Hanley, J. Australian government backs psychedelic drug clinical trials to treat mental illness. The Guardian. March 18, 2021. https://www.theguardian.com/australia-news/2021/mar/18/australian-government-backs-psychedelic-drug-clinical-trials-to-treat-mental-illness (accessed 13 June 2022).
Martinez, M. Johns Hopkins receives first federal grant for psychedelic treatment research in 50 years. Hub. October 20, 2021. https://hub.jhu.edu/2021/10/20/first-nih-grant-for-psychedelics-in-50-years/ (Accessed 13 June 2022).
Daoud, E. Mind Medicine Australia urges psychedelic drugs for mental health treatment during COVID-19. 7News. April 15, 2020. https://7news.com.au/lifestyle/health-wellbeing/mind-medicine-australia-urges-psychedelic-drugs-for-mental-health-treatment-during-covid-19-c-977749 (accessed 13 June 2022).
Kelly, J. R. et al. Psychedelic science in post-COVID-19 psychiatry. Ir. J. Psychol. Med. 38(2), 93–98 (2021).
Dos Santos, R. G., Bouso, J. C. & Hallak, J. E. C. Ayahuasca: What mental health professionals need to know. Arch. Clin. Psychiatry. 44(4), 103–109 (2017).
Jiménez-Garrido, D. F. et al. Effects of ayahuasca on mental health and quality of life in naïve users: A longitudinal and cross-sectional study combination. Sci. Rep. 10(1), 4075 (2020).
González, D. et al. Therapeutic potential of ayahuasca in grief: A prospective, observational study. Psychopharmacology 237(4), 1171–1182 (2020).
González, D., Carvalho, M., Cantillo, J., Aixalá, M. & Farré, M. Potential use of ayahuasca in grief therapy. Omega (Westport). 79(3), 260–285 (2019).
Domínguez-Clavé, E. et al. Ayahuasca improves emotion dysregulation in a community sample and in individuals with borderline-like traits. Psychopharmacology 236(2), 573–580 (2019).
Sarris, J. et al. Ayahuasca use and reported effects on depression and anxiety symptoms: An international cross-sectional study of 11,912 consumers. J. Affect. Dis. Rep. 4, 100098. https://doi.org/10.1016/j.jadr.2021.100098 (2021).
Perkins, D. et al. Influence of context and setting on the mental health and wellbeing outcomes of Ayahuasca drinkers: Results of a large international survey. Front. Pharmacol. 12, 623979 (2021).
Ona, G. et al. Ayahuasca and public health: Health status, psychosocial well-being, lifestyle, and coping strategies in a large sample of ritual Ayahuasca users. J. Psychoactive Drugs. 51(2), 135–145 (2019).
Kohek, M. et al. Ayahuasca and Public Health II: Health status in a large sample of Ayahuasca-ceremony participants in the Netherlands [published online ahead of print, 2022 May 28]. J. Psychoactive Drugs. 55, 1–12 (2022).
Thiessen, M. S., Walsh, Z., Bird, B. M. & Lafrance, A. Psychedelic use and intimate partner violence: The role of emotion regulation. J. Psychopharmacol. 32(7), 749–755 (2018).
Walsh, Z. et al. Hallucinogen use and intimate partner violence: Prospective evidence consistent with protective effects among men with histories of problematic substance use. J. Psychopharmacol. 30(7), 601–607 (2016).
Argento, E., Braschel, M., Walsh, Z., Socias, M. E. & Shannon, K. The moderating effect of psychedelics on the prospective relationship between prescription opioid use and suicide risk among marginalized women. J. Psychopharmacol. 32(12), 1385–1391 (2018).
Hendricks, P. S., Thorne, C. B., Clark, C. B., Coombs, D. W. & Johnson, M. W. Classic psychedelic use is associated with reduced psychological distress and suicidality in the United States adult population. J. Psychopharmacol. 29(3), 280–288 (2015).
Johansen, P. Ø. & Krebs, T. S. Psychedelics not linked to mental health problems or suicidal behavior: A population study. J. Psychopharmacol. 29(3), 270–279 (2015).
Zeifman, R. J. et al. Rapid and sustained decreases in suicidality following a single dose of ayahuasca among individuals with recurrent major depressive disorder: Results from an open-label trial. Psychopharmacology 238(2), 453–459 (2021).
Zeifman, R. J. et al. Post-psychedelic reductions in experiential avoidance are associated with decreases in depression severity and suicidal ideation. Front. Psychiatry. 11, 782 (2020).
Zeifman, R. J. et al. The impact of Ayahuasca on suicidality: Results from a randomized controlled trial. Front. Pharmacol. 10, 1325 (2019).
Bouso, J. C. et al. Personality, psychopathology, life attitudes and neuropsychological performance among ritual users of Ayahuasca: A longitudinal study. PLoS ONE 7(8), e42421 (2012).
Krebs, T. S. & Johansen, P. Ø. Psychedelics and mental health: A population study. PLoS ONE 8(8), e63972 (2013).
Bruno, V., Wiazowski Spelta, L. E., Durão, A. C., Camarini, R. & Marcourakis, T. Psychedelics and mental health: An alternative strategy to treat mental impairments triggered or aggravated by COVID-19. Altern. Ther. Health Med. 28(4), 40–43 (2022).
Cavanna, F. et al. Lifetime use of psychedelics is associated with better mental health indicators during the COVID-19 pandemic. J. Psychedelic Stud. 5(2), 83–93 (2021).
Révész, D. et al. Cross-sectional associations between lifetime use of psychedelic drugs and psychometric measures during the COVID-19 confinement: A transcultural study. Front. Psychiatry. 12, 687546 (2021).
Rocha, K. B. et al. Propiedades psicométricas y valores normativos del General Health Questionnaire (GHQ-12) en población general española. Int. J. Clin. Health Psychol. 11, 125–139 (2011).
Goldberg, D., Williams, P. A User’s Guide to the General Health Questionnaire (NFER-Nelson, 1988).
Gouveia, V. V. et al. Questionário de Saúde Geral (QSG-12): o efeito de itens negativos em sua estrutura fatorial. Cad Saúde Pública. 28, 375–384 (2003).
Derogatis, L. R. Brief Symptom Inventory (Clinical Psychometric Research, 1975).
Laloni, D. T. Escala de Avaliação de Sintomas-90-R. SCL-90-R Adaptação Previsão e Validade. Campinas (Dissertação de mestrado) Instituito de Psicologia e Fonoaudiologia—programa de Pós-Graduação—Psicologia como Profissão e Ciência, Pontifícia Universidade Católica de Campinas (2001).
González de Rivera, J. L., Derogatis, L. R., De las Cuevas, C., Gracia Marco, R., Rodríguez Pulido, F., Henry Benítez, M., Monterrey, A. L. The Spanish Version of the SCL-90-R. Normative Data in the General Population (Clinical Psychometric Research, 1989).
Brunet, A. et al. The Peritraumatic Distress Inventory: A proposed measure of PTSD criterion A2. Am. J. Psychiatry. 158(9), 1480–1485 (2001).
Tedeschi, R. G. & Calhoun, L. G. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J. Trauma Stress. 9(3), 455–471 (1996).
Resende, C., Sendas, S., Maia, A. Estudo das Características Psicométricas do Posttraumatic Growth Inventory—PTGI—(Inventário de Crescimento Pós-Traumático) para a População Portuguesa. In Actas da XIII Conferência Internacional de Avaliação Psicológica: Formas e Contextos (2008).
Costa-Requena, G. & Gil, F. L. Crecimiento postraumático en pacientes oncológicos. Analisis Modificación Conducta. 33(148), 229–250 (2007).
Twisk, J. W. Longitudinal data analysis. A comparison between generalized estimating equations and random coefficient analysis. Eur. J. Epidemiol. 19(8), 769–776 (2004).
Daldegan-Bueno, D., Révész, D., Morais, P. R., Barbosa, P. C. R. & Maia, L. O. Psychosocial and drug use assessment of regular vs non-regular Ayahuasca users in a Brazilian sample: A web-based survey. Subst. Use Misuse. 57(7), 1072–1081 (2022).
Raison, C. L., Jain, R., Penn, A. D., Cole, S. P. & Jain, S. Effects of naturalistic psychedelic use on depression, anxiety, and well-being: Associations with patterns of use, reported harms, and transformative mental states. Front. Psychiatry. 13, 831092 (2022).
Zeifman, R. J. et al. On the relationship between classic psychedelics and suicidality: A systematic review. ACS Pharmacol. Transl. Sci. 4(2), 436–451 (2021).
Hendricks, P. S. et al. The relationships of classic psychedelic use with criminal behavior in the United States adult population. J. Psychopharmacol. 32(1), 37–48 (2018).
Jones, G. M. & Nock, M. K. Psilocybin use is associated with lowered odds of crime arrests in US adults: A replication and extension. J. Psychopharmacol. 36(1), 66–73 (2022).
Goldberg, S. B. et al. Post-acute psychological effects of classical serotonergic psychedelics: A systematic review and meta-analysis. Psychol. Med. 50(16), 2655–2666 (2020).
Luoma, J. B., Chwyl, C., Bathje, G. J., Davis, A. K. & Lancelotta, R. A meta-analysis of placebo-controlled trials of psychedelic-assisted therapy. J. Psychoactive Drugs. 52(4), 289–299 (2020).
Yu, C. L. et al. Trajectory of antidepressant effects after single- or two-dose administration of psilocybin: A systematic review and multivariate meta-analysis. J. Clin. Med. 11(4), 938 (2022).
Domínguez-Clavé, E. et al. Ayahuasca may help to improve self-compassion and self-criticism capacities. Hum. Psychopharmacol. 37(1), e2807 (2022).
O’Shaughnessy, D. M., Berlowitz, I., Rodd, R., Sarnyai, Z. & Quirk, F. Within-treatment changes in a novel addiction treatment program using traditional Amazonian medicine. Ther. Adv. Psychopharmacol. 11, 2045125320986634 (2021).
Perkins, D. et al. Associations between ayahuasca consumption in naturalistic settings and current alcohol and drug use: Results of a large international cross-sectional survey. Drug Alcohol Rev. 41(1), 265–274 (2022).
Barbosa, P. C. et al. Psychological and neuropsychological assessment of regular hoasca users. Compr. Psychiatry. 71, 95–105 (2016).
Bouso, J. C., Fábregas, J. M., Antonijoan, R. M., Rodríguez-Fornells, A. & Riba, J. Acute effects of ayahuasca on neuropsychological performance: Differences in executive function between experienced and occasional users. Psychopharmacology 230(3), 415–424 (2013).
Doering-Silveira, E. et al. Ayahuasca in adolescence: A neuropsychological assessment. J. Psychoactive Drugs. 37(2), 123–128 (2005).
Tucker, T. D. Neuropsychological Effect on Long-Term Ayahuasca Use (Georgia State University, 2018).
Ona, G. et al. Tripping to cope: Coping strategies and use of hallucinogens during the COVID-19 pandemic in three cultural contexts. Psychoactives 1(1), 16–30. https://doi.org/10.3390/psychoactives1010003 (2022).
Smith, K. W., Sicignano, D. J., Hernandez, A. V. & White, C. M. MDMA-assisted psychotherapy for treatment of posttraumatic stress disorder: A systematic review with meta-analysis. J. Clin. Pharmacol. 62(4), 463–471 (2022).
Wagner, A. C., Liebman, R. E., Mithoefer, A. T., Mithoefer, M. C. & Monson, C. M. Relational and growth outcomes following couples therapy with MDMA for PTSD. Front. Psychiatry. 12, 702838 (2021).
Gorman, I. et al. Posttraumatic growth after MDMA-assisted psychotherapy for posttraumatic stress disorder. J. Trauma Stress. 33(2), 161–170 (2020).
Barrett, F. S. & Griffiths, R. R. Classic hallucinogens and mystical experiences: Phenomenology and neural correlates. Curr. Top. Behav. Neurosci. 36, 393–430 (2018).
Kangaslampi, S., Hausen, A. & Rauteenmaa, T. Mystical experiences in retrospective reports of first times using a psychedelic in Finland. J. Psychoactive Drugs. 52(4), 309–318 (2020).
Nour, M. M., Evans, L., Nutt, D. & Carhart-Harris, R. L. Ego-dissolution and psychedelics: Validation of the ego-dissolution inventory (EDI). Front. Hum. Neurosci. 10, 269 (2016).
Peill, J. M. et al. Validation of the Psychological Insight Scale: A new scale to assess psychological insight following a psychedelic experience. J. Psychopharmacol. 36(1), 31–45 (2022).
Carbonaro, T. M. et al. Survey study of challenging experiences after ingesting psilocybin mushrooms: Acute and enduring positive and negative consequences. J. Psychopharmacol. 30(12), 1268–1278 (2016).
Gómez-Sousa, M. et al. Acute psychological adverse reactions in first-time ritual Ayahuasca users: A prospective case series. J. Clin. Psychopharmacol. 41(2), 163–171 (2021).
Honyiglo, E. et al. Unpredictable behavior under the influence of “magic mushrooms”: A case report and review of the literature. J. Forensic Sci. 64(4), 1266–1270 (2019).
Ona, G. Inside bad trips: Exploring extra-pharmacological factors. J. Psychedelic Stud. 2(1), 53–60 (2018).
Parrott, A. C. et al. MDMA, cortisol, and heightened stress in recreational ecstasy users. Behav. Pharmacol. 25(5–6), 458–472 (2014).
Durante, Í., Dos Santos, R. G., Bouso, J. C. & Hallak, J. E. Risk assessment of ayahuasca use in a religious context: Self-reported risk factors and adverse effects. Braz. J. Psychiatry. 43(4), 362–369 (2021).
Bouso, J. C., Dos Santos, R. G., Alcázar-Córcoles, M. Á. & Hallak, J. E. C. Serotonergic psychedelics and personality: A systematic review of contemporary research. Neurosci. Biobehav. Rev. 87, 118–132 (2018).
Hermle, L., Kraehenmann, R. Experimental psychosis research and schizophrenia—Similarities and dissimilarities in psychopathology In Behavioral Neurobiology of Psychedelic Drugs. Current Topics in Behavioral Neurosciences, vol 36 (eds. Halberstadt, A. L., Vollenweider, F., Nichols, D.) 313–332 (Springer, 2018).
Bouso, J. C. et al. Hallucinations and hallucinogens: Psychopathology or wisdom?. Cult. Med. Psychiatry. 47, 576–604 (2022).
Gómez-Salgado, J. et al. COVID-19 information received by the Peruvian population, during the first phase of the pandemic, and its association with developing psychological distress: Information about COVID-19 and distress in Peru. Medicine (Baltimore) 101(5), e28625 (2022).
Hwang, J., Borah, P., Shah, D. & Brauer, M. The relationship among COVID-19 information seeking, news media use, and emotional distress at the onset of the pandemic. Int. J. Environ. Res. Public Health. 18(24), 13198 (2021).
de Meiroz Grilo, M. L. P. et al. Prophylactic action of ayahuasca in a non-human primate model of depressive-like behavior. Front. Behav. Neurosci. 16, 901425 (2022).
Johnson, M. W., Griffiths, R. R., Hendricks, P. S. & Henningfield, J. E. The abuse potential of medical psilocybin according to the 8 factors of the Controlled Substances Act. Neuropharmacology 142, 143–166 (2018).
Scientific American (Eds.). End the ban on psychoactive drug research. Sci. Am. 310(2), 10 (2014).
GENCAT (Generalitat de Catalunya). Cap a millors pràctiques en l’ús de l’ayahuasca. 2019. https://drogues.gencat.cat/ca/detalls/Noticia/Cap-a-millors-practiques-en-lus-de-layahuasca (accessed 13 June 2022).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
J.C.B., G.O. and M.A.A.C. conceived and designed the study; G.O. developed the questionnaire and database; J.C.B., G.O., G.N.R., J.M.R., and R.G.S. carried out the recruitment; D.R. carried out the statistical analysis and graphic representation; J.C.B., D.R. and G.O. wrote a first draft of the manuscript; J.C.B., D.R., G.O., G.N.R., J.M.R., R.G.S., and M.A.A.C. wrote the final version of the manuscript; J.C.B., J.E.C.H. and M.A.A.C. supervised all the process.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bouso, J.C., Révész, D., Ona, G. et al. Longitudinal and transcultural assessment of the relationship between hallucinogens, well-being, and post-traumatic growth during the COVID-19 pandemic. Sci Rep 13, 14052 (2023). https://doi.org/10.1038/s41598-023-41199-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-41199-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.