Abstract
Overweight and obesity rates have increased in recent decades, particularly among the younger population. The long-term consequences of obesity with respect to early venous thromboembolism (VTE) in women have not been established. The aim was to investigate the association between body mass index (BMI) in early pregnancy as a proxy for non-pregnant weight and long-term post-pregnancy risk of VTE in women. This registry-based prospective cohort study analysed data from the Swedish Medical Birth Registry, linked to the National Patient and the National Cause of Death Registries for information on post-pregnancy long-term risk of VTE. Cox proportional hazards model were used to determine the association between BMI at baseline and VTE events during follow-up starting 1 year after baseline. The mean age at registration was 27.5 (standard deviation, 4.9) years. During a median follow-up duration of 12 years (interquartile range, 6–21 years) starting 1 year after the first antenatal visit, 1765 and 2549 women had a deep vein thrombosis and/or pulmonary embolism. The risk of VTE linearly increased with increasing BMI. Compared to women with 20 ≤ BMI < 22.5 kg/m2, women with high normal weight, i.e. with a BMI of 22.5–25.0 kg/m2, had an adjusted hazard ratio (HR) of 1.30 (95% confidence interval [CI] 1.19–1.41), whereas those with a BMI of 30–35 kg/m2 and ≥ 35 kg/m2 (severe obesity) had an adjusted HR of 2.35 (95% CI 2.04–2.70) and 3.47 (95% CI 2.82–4.25, respectively. Using BMI in early pregnancy as a proxy for pre-pregnancy or non-pregnant BMI in young women, we found a significantly increased risk of post-pregnancy long-term risk of VTE even in those with high normal BMI, compared with lean women, whereas those with severe obesity had a markedly high risk.
Similar content being viewed by others
Introduction
Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is the third most common manifestation of acute cardiovascular disease, after myocardial infarction and stroke1. Approximately 10 million cases of VTE are reported to occur annually worldwide, with an annual incidence of 39–115 and 53–162 per 100,000 population for DVT and PE, respectively2. With increasing life expectancy, the number of patients with VTE is expected to increase, and the annual incidence rates may potentially increase to 700 per 100,000 in individuals aged > 70 years3.
The prevalence of overweight, obesity and severe obesity has markedly increased over the last decades, especially among young individuals4. The World Health Organization (WHO) defines underweight as body mass index (BMI) of < 18.5, normal weight as 18.5–24.9, overweight as 25–25.9, obesity as > 30 and severe obesity as > 35.0 kg/m2. According to the WHO, the worldwide prevalence of obesity tripled between 1975 and 2016, with 13% of all adults estimated to be obese in 2016 (15% in women and 11% in men)5.
Overweight and obesity are well-known risk factors for VTE6, 7; however, the 2019 European Society of Cardiology (ESC) Guidelines on VTE considered obesity as a weak risk factor1. Furthermore, most of the cited literature was either dated, included only a limited number of cases, or did not address the risks associated with the highest BMI groups8, 9. Conversely, a recent large-scale study using individual data from 75 predominantly middle-aged population cohorts with > 700,000 participants found that BMI was a strong risk factor for VTE, which was stronger for PE than for DVT10. A strong relationship between overweight and obesity in men during young adulthood and the risk of midlife VTE has also been shown11; however, to which extent this applies to young women has not been established. Given the comparative rarity of VTE in younger women large populations are needed. The Medical Birth registry (MBR) in Sweden with a very high coverage registers weight and height in virtually all women in Sweden who give birth. We used data on BMI assessed in early pregnancy in women and subsequent risk of VTE.
Materials and methods
Study population and design
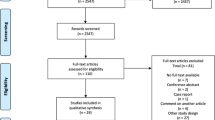
The MBR was used to identify all women in Sweden aged between 18 and 45 years who gave birth to their first child between January 1, 1982, and December 31, 2014. Women were included in the study at the date of their first antenatal visit, usually between 6 and 12 weeks of gestation (90% of women). Women who were first registered with their second child (having given birth abroad or before the start of the registry) were excluded, as were women with BMI < 15 or > 60, inconclusive vital data, those with improbable data on weight and height, women with history of VTE or stroke, and those with < 1 year of follow-up (Fig. 1).
Ethical considerations
The study procedure was approved by the Ethical Committees at the Sahlgrenska Academy at the University of Gothenburg (Dnr:103-15). All personal data were replaced by a code when analyzed (pseudonymized) and therefore informed consent was waived by Ethical Committees at the Sahlgrenska Academy at the University of Gothenburg. The investigation conforms with the principles outlined in the Declaration of Helsinki. All methods were carried out in accordance with relevant guidelines and regulations.
Data sources
Clinical data were extracted from the Swedish MBR and maintained by the Swedish Board of Health and Welfare. The Swedish MBR compiles information on peri- and antenatal factors and their importance for the health of the mother and infant, including data on all pregnancies that resulted in births in Sweden from 1973 and onwards, with a coverage of approximately 99%. Body weight has been registered since 1982 and self-reported height since 1992. Data on height for the period of 1982–1991 were obtained from the records maintained by midwives at the time of delivery. Data were provided by trained healthcare professionals12.
Data on VTE events and deaths were collected from the National Swedish Patient Register (NPR) and Cause of Death Registries. The NPR includes data on inpatient hospital care (85% complete 1980–1986, nationwide coverage from 1987) and specialised hospital-based outpatient clinics (since 2001) but primary care visits are not included13. The Cause of Death Registry includes the date and cause of death for all citizens of Sweden.
Exposure variables and outcomes
Data on the participants’ educational level were obtained from the longitudinal integrated database for health insurance and labour market studies. Educational level was stratified into ≤ 9 years (the compulsory length of education in Sweden), 10–12 years and > 12 years (university or college). Smoking was stratified into 0, 1–9 and ≥ 10 cigarettes per day. Hypertension, congenital heart disease, and diabetes were defined as per the International Classification of Diseases, versions 8, 9 and 10. The prevalence of hypertension and diabetes at baseline was defined using the ICD-code in the NPR and/or self-reported diabetes/hypertension during their first antenatal visit to the MBR.
BMI at the first antenatal visit, the main exposure for the present analyses, was calculated by dividing body weight in kilograms by the square of height in metres (kg/m2). Participants were categorised into seven subgroups based on their BMI: 15– < 18.5 kg/m2, underweight; 18.5– < 20, normal weight (subcategorized into 20– < 22.5 and 22.5– < 25 kg/m2); overweight (subcategorized into 25– < 27.5 and 27.5– < 30 kg/m2); and obese (30– < 35 kg/m2) and severely obese (35– < 55 kg/m2) categories.
Primary and secondary diagnoses are registered in the NPR according to ICD-code (ICD-10 from 1997 and onwards; ICD-9, 1987–1996; and ICD8, 1968–1986). Pulmonary embolism and DVT were defined as a hospital discharge diagnosis or a cause of death according to ICD-8: PE (450), DVT (451); ICD-9: PE (415B, 416W) and DVT (451 except 451A); or ICD-10: PE (I26) and DVT (I80 except 180.0). Individuals were followed from the date of their first antenatal visit until the first diagnosis of PE, DVT, death or until the end of the study in December 31, 2014.
Statistical analyses
The Cox proportional hazards regression models were used to estimate the associations between BMI at the first antenatal visit and VTE risk (PE and DVT) during follow-up, adding potential confounders to the models. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using low normal (20–22.5 kg/m2) BMI as reference values for all analyses. In a separate analysis, women who died of cancer were censored 2 years before death, postulating that malignancy may be a probable cause of VTE in these cases.
The follow-up period started 1 year after the date of the first antenatal visit, and all women were followed until the occurrence of PE, DVT or VTE, death or the end of follow-up (December 31, 2014), whichever occurred first. Only women without a PE or DVT prior to baseline were included in the study.
The proportional hazards assumptions were examined using tests based on weighted residuals14. Variables that did not fulfil the assumptions were stratified in the model. The baseline model was adjusted for age, parity and year of pregnancy. The second model was additionally adjusted for hypertension and diabetes, whereas the third model was further adjusted for smoking status and educational level. In the third model analysis, some data were missing, as shown in Table 1. Crude incidence rates and corresponding 95% CIs were calculated for outcomes separately as events per 100,000 person-years using Poisson regression. Baseline characteristics are provided as percentages or as means and standard deviation for continuous variables. All statistical modelling and analyses were performed using R version 3.6.2.
Results
Study population
Of the 1,393,346 women included in the study, 449 were excluded as their reported height was < 140 cm or > 200 cm; 1851 because of prior DVT, 741 because of prior PE, 759 because of a prior stroke at baseline (Fig. 1). Furthermore, 1435 women with a BMI of > 60 kg/m2 or < 15 kg/m2 were excluded. A total of 299,876 women were also excluded as it was not their first pregnancy, 21 women were excluded as they had inconclusive vital data, and 20,174 women was excluded as they had less than 1 year of follow-up time. Finally, the study population included 1,068,040 women. The mean BMI and age of the population were 23.5 kg/m2 and 27.5 years, respectively. Baseline information on age, height, weight, hypertension, diabetes, smoking status and educational level is shown in Table 1. The median follow-up time was 12.9 (interquartile range, 5.9, 21.2) years.
Event rate
During follow-up, 3997 first VTE events were recorded (Table 2). The incidence rate for VTE per 100,000 person-years was 45.7 in women with a BMI of 30–34.9 kg/m2 and 61.1 with a BMI of 35–59.9 kg/m2 compared with 22.1 in women with a BMI of 20–22.4 kg/m2. Women fulfilling the obesity criteria were younger than those with normal weight at the time of VTE diagnosis: the mean age was 35.8 years in women with BMI of 30–35 kg/m2, 35.7 in BMI of 35–59.9 kg/m2 compared with 41.0 years in those with BMI of 20–22.4 kg/m2. Differences in the incidence rate and age at diagnosis for PE and DVT persisted when censoring women who died from cancer (Table 2).
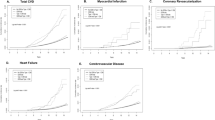
Figure 2 shows a Kaplan–Meier plot for venous thromboembolism by BMI. Survival plot for VTE related to BMI. Survival probability is shown in the Y-axis and time in years in the X-axis. The survival curve showed an exponential increase in risk of VTE with longer follow-up (Fig. 2). Survival probability curves for DVT and PE as separate events can be found in supplementary materials (see Figs. S1 and S2).
Hazard ratios
Women with high normal weight, BMI of 22.5–25.0 kg/m2, had an adjusted HR of 1.30 (95% CI 1.19–1.41) for VTE compared with women with BMI of 20–22.5 kg/m2 (Table 3) after adjusting for age, year of pregnancy, hypertension, diabetes, educational level, parity and smoking status. Corresponding HRs for women with BMI of 30–35 kg/m2 and 35–59.9 kg/m2 were 2.35 (95% CI 2.04–2.70) and 3.47 (95% CI 2.82–4.25). For DVT, the adjusted HR for women with BMI of 30–34.9 kg/m2 was 2.78 (95% CI 2.26–3.41) and for BMI 35–59.9 kg/m2, 4.08 (95% CI 3.00– 5.55). For PE, the adjusted HR for women with BMI of 30–34.9 kg/m2 was 2.20 (95% CI 1.85–2.62) and for BMI of 35–59.9 kg/m2, 3.20 (95% CI 2.48–4.14) compared with women with BMI of 20–22.4 kg/m2 (Table 3).
In a separate analysis, censoring women who died from cancer within 2 years, women with a BMI of 30–34.9 kg/m2 had a HR of 2.20 (95% CI 1.85–2.62) for PE compared with women with a BMI of 20–22.49 kg/m2. The corresponding HR for BMI of 35–59.9 kg/m2 was 3.20 (95% CI 2.48–4.14). For DVT, women with BMI of 30–34.9 kg/m2 had an HR of 2.27 (95% CI 1.89–2.72) and women with BMI of 35–59.9 kg/m2 3.23(95% CI 2.48–4.21) compared with women with BMI of 20–22.49 kg/m2.
Discussion
In this large-scale registry-based cohort study, we found a strong, near-linear association between BMI and long-term post-pregnancy risk of VTE, which was already evident at mildly elevated body weight in early pregnancy. Almost a fourfold increase in long-term risk of VTE was found in the severely obese group relative to low normal weight, which is in agreement with other studies in older subjects4, 9, 15; however, adding that the VTE risk associated with obesity among younger women seems to be higher than previously shown.
The study results are comparable to the results of two previous studies on young men11, 16. Conversely, an American population-based, nested case–control study did not identify an elevated BMI as a risk factor for VTE17. However, that study only included 625 participants with several missing data on body weight and height. Compared with findings from the large Emerging Risk Factor Collaboration10 in mainly middle-aged persons, and with a lower number of VTE events than in our study, HRs associated with obesity and severe obesity were lower than in our study. No previous study has assessed long-term VTE risk associated with weight in younger women with a similarly large number of events.
All women included in the study were pregnant at baseline; however, the baseline weight refers to early pregnancy (weeks 8–12), with only marginal weight gain resulting from pregnancy18. However, one problem with only including pregnant women is that they might be healthier than the average woman.
The mechanisms underlying the increased risk of VTE in obesity are not fully understood. A study conducted in 2016 suggested that body weight relates to VTE because of physical factors associated with the blood flow and not the inflammation or hypercoagulability that was proposed to be associated with adiposity19. Conversely, another study found that adipose tissue could play a role in the pro-thrombotic state observed in obesity by affecting coagulation, haemostasis and fibrinolysis20. Moreover, it should be emphasised that the increased VTE risk mediated by overweight and obesity early in life can be reversed by weight reduction21.
The adjustments considered for the models in this study only marginally affected HRs. In sensitivity analyses, we explored the effects of excluding strongly provoked DVT and PE cases (cancer death within 2 years after VTE). These exclusions did not affect the results.
Strengths and limitations
The strengths of this study include the large study population and the near-complete coverage. Another strength is the long-term prospective follow-up. However, it should be noted that the coverage of the inpatient registry was not yet nationwide until 1987, which means that some early VTE events may not have been recorded. Conversely, patients treated on an outpatient basis during the last years of follow-up will not have been included. In addition, the MBR only includes women who gave birth to live babies and those who had pregnancy losses and stillborn children (only 3.5–4 per thousand of all pregnancies in Sweden22 after the third trimester. Consequently, women with pregnancy loss before the third trimester, and women who are voluntarily or involuntarily childless is not included and results from this study may not reflect VTE risk among these women. Involuntary childlessness is more common among women with obesity23, so it is possible that the incidence of VTE may have been underestimated. In addition, we did not take into account subsequent pregnancies during follow-up nor the increased risk each pregnancy entails. However, as about 85% of women in Sweden give birth, with the average number of live births per woman in Sweden below two, it is unlikely that a selective effect of BMI on a first or any further pregnancies will have affected our results.
Other potential limitations include the lack of information on subsequent BMI during follow-up. Given the strong tracking of body weight over lifetime and the likelihood of weight gain during adulthood, it is likely that many women in the normal weight group will have progressed into the overweight or obesity groups later on24. Once established, overweight and obesity are difficult to treat. The extent to which weight loss reduces the excess VTE risk could not be established in the present study.
Another limitation is that the diagnoses were not verified. However, in a Swedish study including nearly 400 VTE cases, where hospital records were retrieved for approximately 80%, the diagnosis was incorrect in only 13 cases (which were excluded) and objectively verified in almost all remaining cases25. Another Swedish cohort study identified 2450 participants with a first-time diagnosis of PE or DVT in the Swedish patient registry26. While the positive predictive value for a diagnosis of PE was 81% for PE, it was only 59% for a DVT. This difference was thought to be due to patients with DVT in a larger proportion being treated as outpatients. Still, findings with respect to BMI and VTE were similar for PE and DVT, and in our analyses we did not include patients treated on an outpatient basis. Further, if misclassification occurs, it may not be random, with obese women potentially underdiagnosed, as well as overdiagnosed with PE or DVT.
Other intervening factors that might have affected the relation between BMI and VTE is, for example, hospitalizations, or non-fatal cancers, both potentially more common among obese women, but also rare among these young and predominantly healthy individuals. In ongoing analyses, we found associations between BMI and cancer to be complex and varying by cancer type, and a similar complexity will likely also apply to hospitalizations.
The effects of hormonal treatment, either for contraception or as hormone replacement therapy are well known27; however, potential interactions with obesity remain to be explored28. Furthermore, postmenopausal women who use oestrogen have an increased VTE risk, at least during the first year of treatment29, but this information was not available.
In conclusion, we found that overweight or obese women were at markedly high risk of developing VTE later in life compared with women with normal weight, with risk starting to increase already at normal BMI levels. An important clinical implication of this study is that overweight and obesity are important risk factors for later VTE development among young pregnant women. Women with obesity, particularly those with severe obesity, had a markedly increased risk. Given that obesity and overweight are increasing worldwide, this adds to the numerous reasons to maintain low normal weight throughout adulthood to reduce the risk of VTE and other adverse health outcomes.
Data availability
The data that support the findings of this study are available from the Swedish Medical Birth Registry, the Swedish Inpatient and Outpatient Registry, and the Swedish Cause of Death Registry, held by the Swedish National Board of Health and Welfare, and the LISA registry held by Statistics Sweden. Researchers can apply for these data by contacting these government agencies, fulfilling legal and regulatory requirements, and providing an acceptance letter from the Swedish Ethical Review Authority. For legal reasons, these datasets are not directly available from the corresponding author.
References
Konstantinides, S. V. et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The task force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur. Heart J. 41(4), 543–603 (2019).
Wendelboe, A. M. & Raskob, G. E. Global burden of thrombosis: Epidemiologic aspects. Circ. Res. 118(9), 1340–1347 (2016).
Raskob, G. E. et al. Thrombosis: A major contributor to global disease burden. Arterioscler. Thromb. Vasc. Biol. 34(11), 2363–2371 (2014).
Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390 (10113), 2627–2642 (2017)
WHO. Overweight and obesity 2018. https://www.folkhalsomyndigheten.se/the-public-health-agency-of-sweden/living-conditions-and-lifestyle/obesity/.
Hotoleanu, C. Association between obesity and venous thromboembolism. Med. Pharm. Rep. 93(2), 162–168 (2020).
Puurunen, M. K. et al. Epidemiology of venous thromboembolism in the Framingham heart study. Thromb. Res. 145, 27–33 (2016).
Printen, K. J., Miller, E. V., Mason, E. E. & Barnes, R. W. Venous thromboembolism in the morbidly obese. Surg. Gynecol. Obstet. 147(1), 63–64 (1978).
Kakkar, V. V., Howe, C. T., Nicolaides, A. N., Renney, J. T. & Clarke, M. B. Deep vein thrombosis of the leg. Is there a “high risk” group?. Am. J. Surg. 120(4), 527–530 (1970).
Gregson, J. et al. Cardiovascular risk factors associated with venous thromboembolism. JAMA Cardiol. 4(2), 163–173 (2019).
Glise Sandblad, K. et al. Obesity in adolescent men increases the risk of venous thromboembolism in adult life. J. Intern. Med. 287(6), 734–745 (2020).
Socialstyrelsen. Medicinska födselseregistret 2018. Available from: https://www.socialstyrelsen.se/statistik-och-data/register/alla-register/medicinska-fodelseregistret/.
National bord of health and welfare. The national patients register. 2022. Available from: https://www.socialstyrelsen.se/en/statistics-and-data/registers/national-patient-register/.
Grambsch, P. M. & Therneau, T. M. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 81(3), 515–526 (1994).
Poston, L. et al. Preconceptional and maternal obesity: Epidemiology and health consequences. Lancet Diabetes Endocrinol. 4(12), 1025–1036 (2016).
Schmidt, M. et al. Obesity in young men, and individual and combined risks of type 2 diabetes, cardiovascular morbidity and death before 55 years of age: A Danish 33-year follow-up study. BMJ Open 3(4), e002698 (2013).
Heit, J. A. et al. Predictors of survival after deep vein thrombosis and pulmonary embolism: A population-based, cohort study. Arch. Intern. Med. 159(5), 445–453 (1999).
Abrams, B., Carmichael, S. & Selvin, S. Factors associated with the pattern of maternal weight gain during pregnancy. Obstet. Gynecol. 86(2), 170–176 (1995).
Cushman, M. et al. Body size measures, hemostatic and inflammatory markers and risk of venous thrombosis: The longitudinal investigation of thromboembolism etiology. Thromb. Res. 144, 127–132 (2016).
Faber, D. R., De Groot, P. G. & Visseren, F. L. J. Role of adipose tissue in haemostasis, coagulation and fibrinolysis. Obes. Rev. 10(5), 554–563 (2009).
Sundbøll, J. et al. Changes in childhood body-mass index and risk of venous thromboembolism in adulthood. J. Am. Heart Assoc. 8(6), e011407 (2019).
Socialstyrelsen. Statistik om graviditeter, förlossningar och nyfödda. 2022. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2022-12-8275.pdf2022.
Rich-Edwards, J. W. et al. Adolescent body mass index and infertility caused by ovulatory disorder. Am. J. Obstet. Gynecol. 171(1), 171–177 (1994).
Tirosh, A. et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N. Engl. J. Med. 364(14), 1315–1325 (2011).
Rosengren, A. et al. Psychosocial factors and venous thromboembolism: A long-term follow-up study of Swedish men. J. Thromb. Haemost. 6(4), 558–564 (2008).
Öhman, L., Johansson, M., Jansson, J. H., Lind, M. & Johansson, L. Positive predictive value and misclassification of diagnosis of pulmonary embolism and deep vein thrombosis in Swedish patient registries. Clin. Epidemiol. 10, 1215–1221 (2018).
Abou-Ismail, M. Y., Citla Sridhar, D. & Nayak, L. Estrogen and thrombosis: A bench to bedside review. Thromb. Res. 192, 40–51 (2020).
Horton, L. G., Simmons, K. B. & Curtis, K. M. Combined hormonal contraceptive use among obese women and risk for cardiovascular events: A systematic review. Contraception 94(6), 590–604 (2016).
Scarabin, P. Y. Hormone therapy and venous thromboembolism among postmenopausal women. Front. Horm. Res. 43, 21–32 (2014).
Acknowledgements
We thank Edanz (www.edanz.com/ac) for editing a draft of this manuscript.
Funding
Open access funding provided by University of Gothenburg. This work was supported by grants from the Swedish state under an agreement concerning research and education of doctors [ALFGBG-966211]; the Swedish Heart and Lung Foundation [2021–0345]; and the Swedish Research Council [2018-02527, VRREG 2019-00193].
Author information
Authors and Affiliations
Contributions
A.R. conceived the idea for the study. A.M., C.E.L., and M.A. performed statistical analysis. AM wrote the first draft of the manuscript. P.O.H., A.R., G.H., and K.G.S. provided clinical input. All authors made important contributions to the study design. All authors were involved in the data interpretation and critical revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
KGS has received speaker’s honoraria from Pfizer, Bristol Myers Squibb, Bayer and Leo Pharma. AM, AR, MA, CEL, GH, and POH report no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahmoud, A., Sandblad, K.G., Lundberg, C.E. et al. Prepregnancy overweight and obesity and long-term risk of venous thromboembolism in women. Sci Rep 13, 14597 (2023). https://doi.org/10.1038/s41598-023-41186-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-41186-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.