Abstract
To explore the application value of early standardized management in the delivery of neonates of pregnant women with gestational diabetes mellitus (GDM). Parturient diagnosed with GDM and their offspring were selected in our hospital from January 1, 2015 to December 31, 2017 to underwent early standardized management. Non-GDM pregnant women and their offspring were selected as the control group. The growth and development of children aged 0–5 years in the two groups were longitudinally followed up, and the mixed linear model was used to evaluate and compare the growth trajectories. There was no significant difference in height and weight between the two groups at 1 year old (P > 0.05), but the BMI of the GDM group was significantly higher than that in the control group. After 1 year of age, both groups of offspring were similar in height, weight, and BMI, and these similarities persisted at 2, 3, 4, and 5 years of age. After controlling for covariates, the weight, length/height of the two groups of children were slightly different in the growth trajectories between 0–1 years old, 1–2 years old, 2–3 years old, 3–4 years old, and 4–5 years old with no statistical significance (P > 0.05). Although growth differences between the two groups of children were detected within 1 year of age, there were no significant differences in growth trajectories from 1 to 5 years between two groups, which proved that early standardized management has positive significance.
Similar content being viewed by others
Introduction
Gestational diabetes mellitus (GDM) refers to the abnormal glucose metabolism of varying degrees first discovered or occurred during pregnancy, and seriously endangers the health of mothers and babies1,2,3. The incidence of GDM has continued to rise globally over the past few decades4,5. According to the International Diabetes Federation (IDF), approximately 21.3 million live births (16.2%) were affected by some form of hyperglycemia during pregnancy in 20176. About 18.4 million of these cases were due to gestational diabetes mellitus (GDM), accounting for 86.4% of all hyperglycemia in pregnancy. The global incidence of GDM in 2017 was approximately 14%, with the highest primary prevalence of gestational hyperglycemia in Southeast Asia at 26.6% and the lowest in Africa at 9.5%. With economic development and improvement of people's living standards, multiple factors such as unhealthy lifestyles and excessive nutrition, and the improvement and standardization of prenatal screening techniques during pregnancy, the incidence of GDM in China is increasing year by year, which has attracted widespread attention. The prevalence of high-risk pregnant women, such as advanced age, pre-pregnancy overweight or obesity, has risen sharply and is likely to increase further with the implementation of policies to encourage fertility. The high incidence of GDM has brought a huge burden to China's healthcare system. According to the new International Association of Diabetes and Pregnancy Study Groups (IADPSG) criteria, the prevalence of GDM was as high as 19.7% among 15,194 pregnant women in 15 hospitals in Beijing, China in 20137. A recent systematic review and meta-analysis including 25 cross-sectional or retrospective studies and 79,064 Chinese participants showed that the prevalence of GDM in mainland China was 14.8%8. Therefore, enough attention should be paid to GDM and its offspring, and early active intervention should be carried out.
As one of the pregnancy complications that seriously endangers maternal and infant health, a large number of studies have shown that GDM will not only increase the occurrence of maternal and infant perinatal complications (such as preeclampsia, premature birth, polyhydramnios, etc.), but also have long-term effect on obesity, abnormal glucose metabolism, hypertension and other diseases9,10,11,12. At present, offspring of GDM have not shown obvious signs of disease in the early stage, and they have not received enough attention and have entered the children's routine health care system. They have not received timely and effective attention and early intervention. However, interventions after observation of obesity, metabolic syndrome, and abnormal psycho-behavioral development are often ineffective. In addition, there are limited data on the long-term growth and development of GDM offspring with normative management. On the basis of previous research, we aimed to carry out early standardized management of pregnant women with GDM and their offspring, and longitudinally follow-up of the growth and development of GDM offspring aged 0–5 years old in early standardized management. We hypothesize that early standardized management can improve the growth trajectory of GDM offspring aged 0–5 years old.
Materials and methods
Subjects
Ninety neonates, whose mothers were diagnosed with GDM, born in our hospital from January 1, 2015 to December 31, 2017 were selected as the GDM group. A total of 90 neonates who were delivered by non-GDM pregnant women who received antenatal care in our hospital during the same period were selected as the control group. The basic information of the offspring since birth was collected, and their growth and development were followed up. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Ethics Review Committee of Wuxi Maternity and Child Health Care Hospital (No: 2021-01-1215-32). Written informed consent was obtained from all subjects and their legal guardian.
GDM group: Inclusion criteria: Healthy before pregnancy, denied family history of hypertension and diabetes, developed gestational diabetes mellitus (GDM) in this pregnancy and regularly participated in pre-pregnancy examinations; The legal guardian of the child voluntarily accepted to enter the health management system. Exclusion criteria: Mothers with the following diseases in addition to GDM: twins and multiple births; thyroid dysfunction; liver and kidney diseases; tuberculosis, HIV and sexually transmitted diseases and other infectious diseases; moderate to severe anemia; chronic intestinal diseases; epilepsy; heart disease, etc.; clinical data is incomplete.
Control group: Inclusion criteria: Neonates born to mothers with normal glucose metabolism during pregnancy; with complete clinical data and informed consent of the guardian. Exclusion criteria: incomplete clinical data; Did not undergo oral glucose tolerance test during pregnancy.
Diagnostic criteria of GDM refer to the "Guidelines for the Diagnosis and Treatment of Diabetes in Pregnancy (2014)" formulated by the Obstetrics Group of the Obstetrics and Gynecology Branch of the Chinese Medical Association and the Gestational Diabetes Collaborative Group of the Perinatal Medicine Branch of the Chinese Medical Association13,14: The 75 g OGTT test was performed at the first visit at 24–28 weeks and after 28 weeks. Before the test, pregnant women were fasted for at least 8 h, and 75 g of glucose was orally administered within 5 min. The limits are: 5.1 mmol/L on an empty stomach, 10.0 mmol/L 1 h after taking sugar, and 8.5 mmol/L 2 h after taking sugar. GDM is diagnosed as any one of the three blood sugar levels that meets or exceeds the above criteria.
Interventions
GDM group: Combined with relevant research consensus, a set of early standardized management and follow-up plans for GDM women and their offspring were formulated. For GDM women: Once diagnosed with GDM, regular follow-up guidance in specialized outpatient clinics were applied, and comprehensive guidance and regular follow-up will be given in terms of diet, exercise, blood sugar monitoring, and insulin treatment during pregnancy. Within 6 months after giving birth, education on exclusive breastfeeding was conducted and breastfeeding was encouraged to 2 years of age. After 6 months of childbirth, mothers were given instruction on the reasonable addition of complementary foods to the test children, and a “Baby Kitchen” complementary food addition course was offered every 1 to 2 months to demonstrate the preparation of complementary foods and guide reasonable food transitions. At the same time, parent schools were held regularly to teach infants and young children the laws of feeding, exercise, and intellectual development, and to guide and train them in terms of exercise, feeding, language, cognition, life, and communication skills.
For offspring, we developed a systematic early comprehensive management program: Follow-up once a month within 1 month after birth, including physical development assessment, newborn hearing screening, developmental screening, glaucoma screening, etc. Follow-up once a month from 1 to 6 months to assess physical growth and development, and provide feeding consultation. Follow-up once every 2 months from 6 to 12 months to conduct motor development assessment and provide parent–child exercise guidance. Follow-up once every 3 months after 1 year of age to assess whether growth and development are normal, and early intervention will be performed in case of abnormalities. Early matching interventions were performed on high-risk children based on screening results.
Control group: Participate in the "Children's Health Management Service for 0–6 Years Old" in accordance with the requirements of the national basic public health service standards.
Anthropometric measurements
All subjects included in this study were measured within 24–48 h after birth by trained and qualified researchers using uniform equipment, including height, weight, head circumference, upper arm circumference, biceps, triceps, Skinfold thickness of the subscapular, anterior and upper four parts of the iliac. The weight and length of infants and young children under 2 years of age were measured by infant length–weight scale. The weight reading was accurate to 10 g, and the length reading was accurate to 0.1 cm. Children over 2 years old were measured with a height scale (maximum weighing 120 kg, minimum division 0.5 kg; height measurement range 70–190 cm, division value 0.5 cm). The head circumference, chest circumference, and upper arm circumference were measured with a soft ruler, and the readings were accurate to 0.1 cm. The skinfold thickness was measured using a skinfold thickness gauge, which was calibrated before each measurement, accurate to 0.5 mm, and the pressure was 10 g/mm2. Body fat percentage, body fat content and lean body mass were calculated according to the Weststrate method15. Each index was measured 3 times and the average value was taken.
Baseline information collection
Using a self-made questionnaire, we collected data on the baby's birth status, mother's prenatal conditions, and basic demographic data of the family. This includes baby's gender, birth weight, birth length, mother's weight gain during pregnancy, complications during pregnancy, nutrient intake during pregnancy, parents' age, parents' height, parents' weight, level of education, total monthly family income, type of family, and family economic status, among other statistical data.
Statistical analysis
Data was collected by EpiData for double entry and logical check, and SAS 9.4 (SAS Institute Inc, Cary, NC) was used for statistical analysis. Statistical description of measurement data was carried out by x ± SD, and t-test was used to compare the mean between groups when it obeyed normal distribution or approximately normal distribution and the variance was homogeneous, and t' test was applied when the variance was unequal. Data were statistically described, and statistical analysis was performed using the χ2 test, Fisher's exact test, or the continuity-adjusted χ2 test. The influencing factors of body fat percentage of newborns were analyzed by multiple linear stepwise regression analysis16,17. P < 0.05 was used as the criterion to judge whether the difference was statistically significant. Visual inspection of the histogram and Shapiro–Wilk W test for normality of variable distributions-test. The primary analysis used mixed linear models for offspring height (unnormalized and normalized) and body weight growth trajectories. Different baseline levels between the two groups were included as covariates, including maternal pre-pregnancy BMI, pregnancy weight gain, mode of delivery, and mother's age at delivery. The primary concern was whether the change in outcome over 5 years was significantly different between the two groups, which was assessed by linear comparisons.
Ethics approval and consent to participate
This study was approved by the Ethics Review Committee of Wuxi Maternity and Child Health Care Hospital (No: 2023-06-0804-34), and informed consent was obtained from all subjects and their legal guardian. All methods were carried out in accordance with relevant guidelines and regulations.
Results
Basic information of the mothers
There were no significant differences in maternal age, height, prenatal weight, pregnancy number, parity, mode of delivery, education level and monthly household income between the GDM group and the control group (P > 0.05). The proportions of weight gain during pregnancy and family history of diabetes were higher than those in the control group, and the differences were statistically significant (P < 0.05), see Table 1.
Anthropometric indexes of offspring at birth
Birth weight (3.4 ± 0.5 vs. 3.3 ± 0.4 kg; P = 0.03), chest circumference (33.4 ± 1.5 vs. 32.9 ± 1.3; P = 0.03), and BMI (12.5 ± 1.5 vs. 12.8 ± 1.5 vs. 12.9 ± 1.2 kg /cm2; P = 0.02) of GDM offspring were higher than that in control group. There was no significant difference in birth gestational age, birth length, head circumference and upper arm circumference between the GDM group and the control group (P > 0.05). The skinfold thicknesses of the biceps brachii, triceps brachii, subscapular angle and upper iliac crest in the GDM group were significantly higher than those in the control group (P < 0.01). The weight in the GDM group was 0.1 kg (P = 0.03) and 3.1% higher BF% (P < 0.01), and the delipidated mass in the GDM group was 0.1 kg lower than that in the control group (P = 0.03), see Table 2.
Comparison of growth trajectories between two groups of children aged 0–5 years
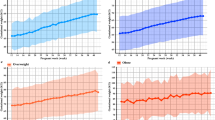
Although there was an initial difference at birth and persisted to about 1 year old, there was no significant difference in height and weight between the two groups at 1 year old, and the BMI of the children in the GDM group was significantly higher than that of the children in the control group (17.65 ± 1.43 vs. 17.14 ± 1.22 kg/cm2, P = 0.01). But after 1 year of age, GDM offspring and control offspring were similar in height, weight, and BMI, which persisted at 2, 3, 4, and 5 years of age (Table 3). From Fig. 1A and B, we can see that the growth trajectories of height and weight for the two groups of children are basically consistent. Figure 1C shows that the BMI of children in the GDM group is higher than that of the control group from birth to 1 year old. From ages 2 to 5, the BMI curves of the two groups tend to converge.
We next assessed differences in height and weight gain between the two groups after adjusting for different baseline covariates (mother's pre-pregnancy BMI, gestational weight gain, mode of delivery, mother's age at birth, birth weight, and birth length). The results showed that the weight, length/height growth trajectories of the two groups of offspring were slightly different between 0–1 years old, 1–2 years old, 2–3 years old, 3–4 years old, and 4–5 years old with no statistical significance (P > 0.05). See Table 4.
Discussion
With the in-depth study of the theory of Development of Health and Disease (DOHaD), the influence of GDM on the long-term and offspring of pregnant women has attracted more and more attention. GDM not only has adverse effects on the mother and child during the perinatal period, the abnormal intrauterine environment of GDM may also increase the risk of obesity, hypertension, abnormal glucose metabolism, neurological diseases and cardiovascular diseases in the offspring in the long-term18,19. The Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) Follow-up Study Group reported that GDM determined by the IADPSGcriteria after adjustment for maternal BMI was associated with increased body fat content and obesity in offspring aged 10–14 years20. Maternal blood glucose levels were inversely associated with insulin sensitivity and β-cell function, which results in a higher prevalence of impaired glucose tolerance in offspring of GDM mothers16,17. Zhao et al.21 conducted a cross-sectional study of 4740 9–11-year-old children in 12 countries and showed that the risk of obesity in the offspring of GDM was 1.53 times higher than that of non-GDM. A population-based cohort study found that in utero exposure to gestational diabetes was significantly associated with the development of autism spectrum disorder in offspring22. Regardless of glycemic control during pregnancy, the effects of GDM on offspring are not limited to the intrauterine and neonatal periods, and may persist into children, adolescents, and even adults. Therefore, early systematic management of offspring with GDM is of great significance and can affect health status and quality of life throughout life, which is more active, proactive and effective than intervening in adults.
Some studies have pointed out that children are not included in the standardized health management system is one of the main reasons for the deviation of the growth and development of GDM offspring23. The International Federation of Gynecology and Obstetrics (FIGO) proposed in the GDM guidelines issued in 2015 that the follow-up of GDM women and their offspring should be combined with routine physical examination and vaccination of offspring24. Our results showed that the birth weight (3.4 ± 0.5 vs. 3.3 ± 0.4 kg; P = 0.03), BMI (12.5 ± 1.5 vs. 12.8 ± 1.5 vs. 12.9 ± 1.2 kg/cm2; P = 0.02), body fat percentage (BF%; 17.9% vs. 14.8%, P < 0.01), and body fat mass (0.6 kg vs. 0.5 kg; P < 0.01) of GDM offspring were significantly higher than those in the control group, which was consistent with other studies25,26,27. Hyperglycemia that occurs in the second and third trimesters increases maternal blood concentrations of amino acids and fatty acids and transports excess nutrients to the fetus through the placenta28. Excessive nutrient supply stimulates fetal pancreatic β-cells to increase insulin secretion. Fetal hyperinsulinemia can lead to overgrowth of insulin-sensitive tissues such as the liver, adipose tissue, and heart.
Despite almost no evidence suggesting that routine treatment of GDM affects the long-term outcomes of offspring. In a follow-up study of children (ages 5–10) born to women who participated in a multicenter trial, there was no reduction found in obesity or metabolic dysfunction in the offspring of women who received treatment (diet therapy and insulin if necessary) compared to those with mild untreated GDM29. However, lower fasting blood glucose levels were observed only in female offspring. In this study, although growth differences were detected at birth and persisted up to 1 year of age, we observed similar growth and development trends between 1 and 5 years between offspring of GDM and control group after early standardized management, which suggests that early management should be initiated once a pregnant woman with GDM is identified, and early integrated management of the offspring should be initiated. This is consistent with the results of other studies. Zhou et al. found that the number of blood glucose abnormalities in pregnant women with GDM is directly proportional to the occurrence of neonatal neurological abnormalities, and strengthen prenatal healthcare management for pregnant women could reduce the incidence of abnormal neonatal neurological development30. Although the majority of obesity in adolescents and adults occurs in individuals with normal birth weight, the outcomes of early childhood growth remain clinically relevant because a large proportion of adolescent obesity is established before the age of 5 years. Children who are overweight in kindergarten are four times more likely to become obese by eighth grade than children of normal weight31.
Although this study indicated the importance of early standardized management of GDM offspring, there were still some shortcomings. Selection bias may have arisen because some data were not collected completely or some infants could not be included in this study. In addition, the number of follow-up cases was relatively small, and it was necessary to further expand the sample size and increase the research content, such as children's body composition, in order to better evaluate the physical development level.
Data availability
The dataset generated during and analysed during the current study is available from the corresponding author on reasonable request.
References
Szmuilowicz, E. D., Josefson, J. L. & Metzger, B. E. Gestational diabetes mellitus. Endocrinol. Metab. Clin. North Am. 48(3), 479–493 (2019).
Kim, K. S., Hong, S., Han, K. & Park, C. Y. The clinical characteristics of gestational diabetes mellitus in Korea: A National Health Information Database Study. Endocrinol. Metab. (Seoul) 36(3), 628–636 (2021).
Guariguata, L., Linnenkamp, U., Beagley, J., Whiting, D. R. & Cho, N. H. Global estimates of the prevalence of hyperglycaemia in pregnancy. Diabetes Res. Clin. Pract. 103(2), 176–185 (2014).
Krejci, H. et al. The incidence of gestational diabetes mellitus before and after the introduction of HAPO diagnostic criteria. Ceska Gynekol. 84(6), 404–411 (2019).
Jawad, F. & Ejaz, K. Gestational diabetes mellitus in South Asia: Epidemiology. J .Pak. Med. Assoc. 66(9 Suppl 1), S5–S7 (2016).
Cho, N. H. et al. IDF diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 138, 271–281 (2018).
Zhu, W. W. et al. High prevalence of gestational diabetes mellitus in Beijing: Effect of maternal birth weight and other risk factors. Chin. Med. J. (Engl.) 130(9), 1019–1025 (2017).
Gao, C., Sun, X., Lu, L., Liu, F. & Yuan, J. Prevalence of gestational diabetes mellitus in mainland China: A systematic review and meta-analysis. J. Diabetes Investig. 10(1), 154–162 (2019).
Chung, H. R. et al. Maternal hyperglycemia during pregnancy increases adiposity of offspring. Diabetes Metab. J. 45(5), 730–738 (2021).
Tam, W. H. et al. In utero exposure to maternal hyperglycemia increases childhood cardiometabolic risk in offspring. Diabetes Care 40(5), 679–686 (2017).
Kim, M. H. et al. Pregnancy outcomes of women additionally diagnosed as gestational diabetes by the International Association of the Diabetes and Pregnancy Study Groups Criteria. Diabetes Metab. J. 43(6), 766–775 (2019).
Li, Z. et al. Incidence rate of type 2 diabetes mellitus after gestational diabetes mellitus: A systematic review and meta-analysis of 170,139 women. J. Diabetes Res. 2020, 3076463 (2020).
Moon, J. H. & Jang, H. C. Gestational diabetes mellitus: Diagnostic Approaches and maternal-offspring complications. Diabetes Metab. J. 46(1), 3–14 (2022).
Obstetrics Group of Obstetrics and Gynecology Branch of Chinese Medical Association, Pregnancy-associated Diabetes Collaborative Group of Perinatal Medicine Branch of Chinese Medical Association: Guidelines for Diagnosis and Treatment of Diabetes in Pregnancy (2014). Chin J Obstet Gynecol, 49(08), 561–569 (2014).
Cicek, B. et al. Four-site skinfolds and body fat percentage references in 6-to-17-year old Turkish children and adolescents. J. Pak. Med. Assoc. 64(10), 1154–1161 (2014).
Lowe, W. J. et al. Hyperglycemia and Adverse Pregnancy Outcome Follow-up study (HAPO FUS): Maternal gestational diabetes mellitus and childhood glucose metabolism. Diabetes Care 42(3), 372–380 (2019).
Scholtens, D. M. et al. Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study (HAPO FUS): Maternal glycemia and childhood glucose metabolism. Diabetes Care 42(3), 381–392 (2019).
Chen, S., Zhao, S., Dalman, C., Karlsson, H. & Gardner, R. Association of maternal diabetes with neurodevelopmental disorders: autism spectrum disorders, attention-deficit/hyperactivity disorder and intellectual disability. Int. J. Epidemiol. 50(2), 459–474 (2021).
Tsadok, M. A. et al. Obesity and blood pressure in 17-year-old offspring of mothers with gestational diabetes: Insights from the Jerusalem Perinatal Study. Exp. Diabetes Res. 2011, 906154 (2011).
Lowe, W. J. et al. Maternal glucose levels during pregnancy and childhood adiposity in the Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study. Diabetologia 62(4), 598–610 (2019).
Zhao, P. et al. Maternal gestational diabetes and childhood obesity at age 9–11: Results of a multinational study. Diabetologia 59(11), 2339–2348 (2016).
Nahum, S. K. et al. Prenatal exposure to gestational diabetes mellitus as an independent risk factor for long-term neuropsychiatric morbidity of the offspring. Am. J. Obstet. Gynecol. 215(3), 380–381 (2016).
Gonzalez-Quintero, V. H. et al. The impact of glycemic control on neonatal outcome in singleton pregnancies complicated by gestational diabetes. Diabetes Care 30(3), 467–470 (2007).
Hod, M. et al. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on gestational diabetes mellitus: A pragmatic guide for diagnosis, management, and care. Int. J. Gynaecol. Obstet. 131(Suppl 3), S173–S211 (2015).
Hu, J. et al. Association of gestational diabetes mellitus with offspring weight status across infancy: A prospective birth cohort study in China. BMC Pregnancy Childbirth 21(1), 21 (2021).
Wiechers, C. et al. Body composition in term offspring after maternal gestational diabetes does not predict postnatal hypoglycemia. BMC Pediatr. 21(1), 111 (2021).
Yang, Y. et al. The association of gestational diabetes mellitus with fetal birth weight. J. Diabetes Complicat. 32(7), 635–642 (2018).
Freinkel, N. Banting Lecture 1980. Of pregnancy and progeny. Diabetes 29(12), 1023–1035 (1980).
Goldstein, R., Teede, H. & Thangaratinam, S. Excess gestational weight gain in pregnancy and the role of lifestyle intervention. Semin. Reprod. Med. 34(02), e14–e21 (2016).
Zhou, W., Meng, W. Y. & Su, T. The impact of the number of abnormal glucose values and self-management of gestational diabetes mellitus on the neurodevelopment of newborns. J. Clin. Exp. Med. 21(07), 768–771 (2022).
Cunningham, S. A., Kramer, M. R. & Narayan, K. M. Incidence of childhood obesity in the United States. N Engl. J. Med. 370(17), 1660–1661 (2014).
Funding
The work is supported by the high-level talent training project of Wuxi Taihu Talent Plan (No. HB2020071) and the 21st batch of Wuxi science and technology innovation and entrepreneurship projects (No. Y20212036).
Author information
Authors and Affiliations
Contributions
B.G. conceived the study; B.G., X.J., Y.X. and J.P. performed the survey and summary; B.G. and Y.W. wrote and revised the manuscript. All authors approved the publishment of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guo, B., Pei, J., Xu, Y. et al. Effects of early standardized management on the growth trajectory of offspring with gestational diabetes mellitus at 0–5 years old: a preliminary longitudinal study. Sci Rep 13, 13939 (2023). https://doi.org/10.1038/s41598-023-40928-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40928-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.