Abstract
Lumbar spinal stenosis (LSS) can interfere with daily life and quality of life (QOL). Evaluating physical function and QOL and helping patients to improve is the focus of rehabilitation. Phase angle (PhA) assessment is widely used to measure body composition and is considered an indicator of physical function and QOL. This study investigated the relationship between PhA and physical function, physical activity, and QOL in patients with LSS. PhA, handgrip strength, walking speed, Timed Up and Go test (TUG), Life Space Assessment (LSA), Prognostic Nutritional Index (PNI), Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ), and EQ-5D were assessed and statistically analyzed. The study included 133 patients with LSS. Multiple regression analysis of PhA adjusted for age, sex, and body mass index (Model 1) and for Model 1 + PNI (Model 2) showed significant correlations (P < 0.05) with handgrip strength, walking speed, TUG, and LSA. Regarding QOL, PhA was significantly correlated (P < 0.05) with lumbar function in JOABPEQ. PhA was associated with physical function and QOL in patients with LSS and might be a new clinical indicator in this population.
Similar content being viewed by others
Introduction
Lumbar spinal stenosis (LSS) is caused by the narrowing of the spinal canal, impeding the nerves and blood vessels traveling through the lumbar spine. LSS causes pain in the lower back, buttocks, and lower extremities, which can interfere with daily life1. Intermittent claudication is one of the most common symptoms of LSS, severely limiting the patient’s mobility. LSS impairs activities of daily living and may lead to psychosocial problems resulting from depression and isolation due to symptoms such as intermittent claudication, back pain, numbness, and muscle weakness in the lower limbs, leading to a decreased quality of life (QOL)2. Improving QOL is one of the important goals of LSS treatment3, and assessing QOL is important in physical therapy.
In recent years, phase angle (PhA) assessment has been widely used to noninvasively measure body composition and has been reported as a measure of skeletal muscle quality4. A high PhA reflects higher cellularity, cell membrane integrity, and better cell function, whereas a low PhA reflects cell loss and reduced cell membrane integrity5. PhA has been reported to be associated with physical functions such as muscle strength, balance, and walking speed in both community-dwelling elderly individuals and cancer patients6,7. An association between PhA and health-related QOL has been reported in patients on maintenance hemodialysis8,9. Therefore, PhA is an indicator of physical function and QOL and is considered a useful tool for assessing the patient’s condition in clinical practice. However, although PhA is a noninvasive and simple method of measuring body composition, few studies have used PhA in orthopedic diseases, and its relationship with physical function and QOL has not been fully investigated. LSS is often associated with pain and numbness, which may make it difficult to assess physical functions such as muscle strength, balance function, and walking speed. In addition, physical function, activities of daily living, and QOL are interrelated, and PhA, which can be measured noninvasively, may be useful for the indirect assessment of physical function and QOL in patients who are difficult to assess in practice.
Therefore, this study aimed to investigate the relationship between PhA, physical function, and QOL in patients with LSS.
Methods
Ethics
The study protocol conformed to the ethics guidelines of the Declaration of Helsinki, as reflected in the prior approval given by the institutional review board of Kurume University Hospital (approval ID: 22017). This study was retrospective; thus, we provided informed consent forms including the study title, subject, and aim on the web. Informed consent from patients was obtained using an opt-out approach.
Patients
This cross-sectional study included 191 patients (age ≥ 60 years) admitted for surgery for LSS in the orthopedic ward of our hospital between May 2020 and April 2021. Data collection was conducted in May 2022, and no personally identifiable participant information was accessed during the data collection. We excluded patients with pyogenic spondylitis, metastatic bone tumor, history of stroke, difficulty standing due to hemiplegia, difficulty measuring body composition, insertion of a pacemaker, and inability to answer the questionnaire. PhA was measured before admission, and physical function and QOL were assessed before surgery.
Phase angle (PhA)
PhA was measured using bioelectrical impedance analysis (BIA). An Inbody 770 BIA unit (Inbody Co., Ltd., Seoul, Korea) was used for the measurements. BIA measures body composition by passing a weak alternating current through the body and taking the impedance or the difference between each tissue. Impedance is a general term for resistance components that interfere with the current, and impedance can be divided into resistance (R) and reactance (Xc). PhA is the value of arctangent, which is Xc divided by R, and is expressed by the following equation5:
Life space assessment (LSA)
LSA is an index that assesses mobility in the spatial extent of an individual’s daily life10. This consists of the range of living space, frequency, presence of assistive devices, and level of independence, and it is a measure that investigates the range of activities in the living space over the past month. The living space from the bedroom at home to outside the town is divided into five levels, and the total score is calculated by multiplying the score of each level by the frequency and degree of independence. The maximum score is 120, with higher scores indicating a higher level of activity. LSA has been used to assess mobility and activities of daily living in a variety of populations, including community-dwelling elderly individuals and stroke patients11,12.
Handgrip strength
Handgrip strength was measured using a Smedley-type grip strength meter (Takei Kiki Kogyo, T.K.K. 5101)13. The subject was instructed, “After the signal, grip the grip strength meter as strongly as possible. Please hold the grip strength meter for 3 s.” The right hand was measured twice, and the maximum value was adopted. Grip strength is used to measure voluntary muscle function as an indicator of muscle strength in patients with LSS14.
Walking speed
A 10-m walk test was conducted to calculate the walking speed. In the 10-m walk test, two marks were placed on the floor so that the distance was 10 m in a straight line, and the time from the leading foot passing the first mark to the moment it stepped on or over the second mark was measured with a stopwatch. To ensure the subject started 1 m before the first mark and passed the second mark by 1 m, the subject was not told about the marks but was shown the direction and instructed, “Walk straight ahead at your normal walking speed15”.
Timed Up and Go test (TUG)
For the TUG, the subject was seated and asked: “Please get up from the chair, walk as fast as you can, walk around the cone 3 m ahead, and sit on the chair again. You may turn in either direction.” The TUG time was measured with a stopwatch from the time the subject’s body began to move till the time they were seated on the chair again. A chair with a height of 42.0 cm and an elbow rest was used16.
Prognostic nutritional index (PNI)
PNI is a simple and reliable assessment of nutritional status17. Consequently, PNI was assessed in this study because it is considered a confounder of nutrition. PNI is a prognostic score that is calculated by reflecting both the inflammatory and nutritional status of the patient. In the current study, it was calculated via the following formula using the preoperative blood test values.
PNI has been reported to be a useful marker of malnutrition18. It has also been reported that a low preoperative PNI indicates a low nutritional status and is associated with postoperative complications in spinal diseases19,20.
Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ)
JOABPEQ is a back-pain disease-specific QOL assessment that combines the Roland-Morris Disability Questionnaire (RDQ) and the Short-Form Health Survey (SF-36) with the Visual Analog Scale (VAS). The assessment consists of 25 items corresponding to five subscales: low back pain (4 items), lumbar function (6 items), walking ability (5 items), social life function (3 items), and mental health (7 items). The score for each subscale ranges from 0 to 100, with higher scores indicating better conditions21.
EuroQOL 5 dimensions 3-level (EQ-5D)
The EQ-5D is a comprehensive QOL scale that can be calculated by answering five questions on three levels: “degree of mobility,” "personal care," "usual activities," "pain/discomfort," and "anxiety/stress.” It has been used to assess health-related QOL in middle-aged and elderly people living at home and for various diseases, including orthopedic diseases22,23.
Statistical analysis
JMP version 15.0 was used for the statistical analysis, and the significance level was set at 5%. The association between PhA and each measurement item (age, sex, body mass index [BMI], PNI, handgrip strength, walking speed, TUG, LSA, each sub-item of JOABPEQ, and EQ-5D) was investigated using Spearman's rank correlation. PhA is influenced by three main factors: age, sex, and BMI5, and it is considered a useful marker of malnutrition18. In the present study, we focused on the relationship of PhA with physical function and QOL. For this purpose, we created two models, one without adjustment for PNI (Model 1) and the other with adjustment for PNI (Model 2). With each model, we investigated the relationship of PhA with physical function (grip strength, walking speed, TUG), physical activity (LSA), and QOL (JOABPEQ subitems, EQ-5D) using multiple regression analysis, with PhA as the dependent variable. Grip strength, TUG, and 10-m walk tests are easy and practical tools for assessing patients' physical abilities, and these physical assessments have been used in patients with LSS in clinical settings14,24,25. Thus, we applied them in this study.
Results
Patients
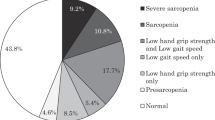
Of the 191 patients who met the eligibility criteria, 133 were analyzed after the exclusion criteria were applied (Fig. 1). The basic attributes of the patients are shown in Table 1.
Correlation between PhA and each measurement item
The results of Spearman's rank correlation analysis of the relationship between PhA and each measurement item are shown in Table 2. PhA was positively correlated with BMI, PNI, handgrip strength, walking speed, and LSA and negatively correlated with age, TUG, and VAS (lower limb pain).
Regarding QOL assessment, PhA was positively correlated with lumbar function, walking ability, social life function, and mental health, which are JOABPEQ subitems, and with EQ-5D.
The results of the Wilcoxon signed-rank test of the relationship between PhA and each measurement item are shown in Table 3. The patients were divided into two groups using a median of PhA. The male/female ratio, hand grip strength, walking speed, TUG, LSA, JOABPPEQ (lower limb pain, mental health), and EQ-5D were significantly higher in the high PhA group than in the low PhA group. Age and VAS score (lower limb pain) were significantly lower in the high PhA group than in the low PhA group.
Multiple regression analysis of confounding-adjusted PhA, physical function, and QOL
Table 4 shows the results of the multiple regression analysis of the relationship of PhA with physical function and physical activity (adjusted for age, sex, and BMI [Model 1] and age, sex, BMI, and PNI [Model 2]). Table 5 shows the results of multiple regression analysis of the relationship between PhA and QOL (Models 1 and 2).
Regarding physical function and physical activity, significant correlations were found between PhA and handgrip strength, walking speed, TUG, and LSA, and for QOL, significant correlations were found between PhA and the lumbar function, walking ability, and mental health subitems of JOABPEQ in both Model 1 and 2. However, no correlation with EQ-5D was observed.
Discussion
This study investigated the relationship between PhA and physical function, physical activity, and QOL in LSS patients admitted for surgery. A significant correlation was found between PhA and physical function and physical activity, and PhA was correlated with the subitems of JOABPEQ, a disease-specific QOL assessment, and EQ-5D, a comprehensive QOL assessment. Furthermore, in the multiple regression analysis, both Model 1 and Model 2 showed that PhA was correlated with the lumbar function subitem of JOABPEQ. PhA may be a useful tool for clinical and perioperative evaluation because it reflects both physical and QOL (Fig. 2).
Relationship between PhA, physical function, and physical activity
In the present study, significant positive correlations were found between the PhA of LSS patients and handgrip strength and walking speed, and significant negative correlations were found with the TUG test. Yamada et al. reported that PhA was significantly correlated with lower limb muscle strength in community-dwelling elderly persons26. Tanaka et al., in their study of the locomotive syndrome (LS) and PhA in community-dwelling elderly persons, found that PhA was significantly correlated with the TUG test and was an independent factor for LS27. In the present study on LSS and in previous studies on other diseases, PhA was significantly higher in patients with higher physical function.
Furthermore, in the present study, a significant positive correlation was found between PhA and LSA, which is an indicator of physical activity. High physical activity is associated with high physical function, and a correlation between physical activity and PhA has been reported in other studies17,28. However, the mechanisms underlying the relationship between physical activity, physical function, and PhA are unknown. Considering the principles of PhA measurement, it is likely that the results of the present study were affected by the decrease in the amount of fat. Fat has high electrical resistance, and physical activity decreases this resistance. Moreover, the increase in the size and mass of cells and the structural integrity of cell membranes increases the reactance (Xc), resulting in a higher PhA5.
PhA and JOABPEQ
PhA was correlated with lumbar function in JOABPEQ in both Model 1 and 2. The JOABPEQ items for lumbar function included the following: "I sometimes ask for help when I do something because of my back pain," "I try not to bend my back or kneel because of my back pain," "I have difficulty getting up from a chair because of my back pain," "I have difficulty turning over because of my back pain," "I have difficulty putting on socks or stockings because of my back pain” and "Do you find it difficult to bend forward, kneel, or bend over because of your physical condition?” These questions are related to the flexion, extension, and rotation of the trunk. For preoperative LSS patients with low back pain, trunk flexion, extension, and rotation movements should not be assessed because they are likely to induce pain. Therefore, PhA may be one of the indicators for evaluating lumbar function in patients with LSS because it can be used to estimate lumbar function without actual movements.
PhA and quality of life
There was a significant association between PhA and the lumbar function subitems of JOABPEQ in Models 1 and 2. Machado et al. demonstrated that PhA is associated not only with physical function but also with QOL in patients with idiopathic pulmonary fibrosis29. Azar et al. reported in their study of dialysis patients that PhA is a clinically useful predictive tool because it reflects both physical function and QOL9. To the best of our knowledge, this is the first study to investigate the relationship between PhA and QOL in LSS, with results similar to those of previous studies. JOABPEQ is a lumbar spine disease-specific QOL measure and is a highly responsive outcome measure for assessing changes over time in patients with low back pain21. EQ-5D, on the other hand, is a widely used comprehensive QOL assessment30. The study found that PhA was associated with disease-specific QOL, suggesting that PhA and QOL may be related in patients with LSS. However, a correlation with the EQ-5D, a comprehensive quality of life scale, was found in the bivariate analysis but not in the multiple regression analysis. This may be because the EQ-5D we used was a three-level version, which could provide less information and discrimination than the newly developed five-level version30.
Few studies have investigated both QOL measures, and the results of this study seem to confirm the above findings. Moreover, as mentioned earlier, PhA also reflected the physical function (lumbar spine function) of LSS patients in this study. Evaluating both the physical function and QOL of patients and helping patients improve these parameters is the focus of rehabilitation31. Therefore, PhA may be a useful tool in physical therapy in patients with LSS.
Limitations
Some limitations of this study should be considered. First, it was a cross-sectional study, and the causal relationship was unclear because the broader relationship between disease and factors was not known due to the design. In addition, it was a single-center study with a small number of cases with no direct assessment of lumbar function. Moreover, we demonstrated that PhA is associated with QOL and physical function in patients with LSS in this study. However, we did not include healthy subjects or those with lumbar disc herniation. The dysuria or psychological depression seen in LSS patients was not examined. In this study, only preoperative patients were studied; future studies of patients who are unsuitable for surgery and research involving postoperative patients are necessary.
Conclusion
PhA was associated with physical function and QOL in patients with LSS and may be a useful new tool for preoperative clinical assessment in patients with LSS.
Data availability
The datasets generated and/or analysed during the current study are available in the Harvard Dataverse repository, https://doi.org/10.7910/DVN/REBPZ4.
References
Takenaka, H. et al. Predictors of walking ability after surgery for lumbar spinal canal stenosis: A prospective study. Spine J. 19, 1824–1831. https://doi.org/10.1016/j.spinee.2019.07.002 (2019).
Sobottke, R. et al. Predictors of improvement in quality of life and pain relief in lumbar spinal stenosis relative to patient age: A study based on the Spine Tango registry. Eur. Spine J. 26, 462–472. https://doi.org/10.1007/s00586-015-4078-8 (2017).
Kobayashi, H. et al. Reference values of the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire in patients with lumbar spinal stenosis and characteristics of deterioration of QOL: Lumbar Spinal Stenosis Diagnosis Support Tool: DISTO project. J. Orthop. Sci. 24, 584–589. https://doi.org/10.1016/j.jos.2018.11.022 (2019).
Abe, T. et al. Impact of phase angle on physical function in patients with acute stroke. J. Stroke Cerebrovasc. Dis. 30, 105941. https://doi.org/10.1016/j.jstrokecerebrovasdis.2021.105941 (2021).
Norman, K., Stobaus, N., Pirlich, M. & Bosy-Westphal, A. Bioelectrical phase angle and impedance vector analysis–clinical relevance and applicability of impedance parameters. Clin. Nutr. 31, 854–861. https://doi.org/10.1016/j.clnu.2012.05.008 (2012).
Matias, C. N. et al. Phase angle predicts physical function in older adults. Arch. Gerontol. Geriatr. 90, 104151. https://doi.org/10.1016/j.archger.2020.104151 (2020).
Matias, C. N. et al. Phase angle as a marker of muscular strength in breast cancer survivors. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17124452 (2020).
Kang, S. H., Do, J. Y. & Kim, J. C. Impedance-derived phase angle is associated with muscle mass, strength, quality of life, and clinical outcomes in maintenance hemodialysis patients. PLoS ONE 17, e0261070. https://doi.org/10.1371/journal.pone.0261070 (2022).
Beberashvili, I. et al. Bioimpedance phase angle predicts muscle function, quality of life and clinical outcome in maintenance hemodialysis patients. Eur. J. Clin. Nutr. 68, 683–689. https://doi.org/10.1038/ejcn.2014.67 (2014).
Peel, C. et al. Assessing mobility in older adults: The UAB Study of Aging Life-Space Assessment. Phys. Ther. 85, 1008–1119 (2005).
Yang, Y. N. et al. Life space assessment in stroke patients. Ann. Rehabil. Med. 41, 761–768. https://doi.org/10.5535/arm.2017.41.5.761 (2017).
Simoes, M., Garcia, I. F., Costa, L. D. C. & Lunardi, A. C. Life-Space Assessment Questionnaire: Novel measurement properties for Brazilian community-dwelling older adults. Geriatr. Gerontol. Int. 18, 783–789. https://doi.org/10.1111/ggi.13263 (2018).
Makizako, H. et al. Associations of social frailty with loss of muscle mass and muscle weakness among community-dwelling older adults. Geriatr. Gerontol. Int. 19, 76–80. https://doi.org/10.1111/ggi.13571 (2019).
Kwon, J. W. et al. Hand grip strength can predict clinical outcomes and risk of falls after decompression and instrumented posterolateral fusion for lumbar spinal stenosis. Spine J. 20, 1960–1967. https://doi.org/10.1016/j.spinee.2020.06.022 (2020).
Peters, D. M., Fritz, S. L. & Krotish, D. E. Assessing the reliability and validity of a shorter walk test compared with the 10-Meter Walk Test for measurements of gait speed in healthy, older adults. J. Geriatr. Phys. Ther. 36, 24–30. https://doi.org/10.1519/JPT.0b013e318248e20d (2013).
Schoene, D. et al. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: Systematic review and meta-analysis. J. Am. Geriatr. Soc. 61, 202–208. https://doi.org/10.1111/jgs.12106 (2013).
Di Vincenzo, O., Marra, M., Di Gregorio, A., Pasanisi, F. & Scalfi, L. Bioelectrical impedance analysis (BIA)-derived phase angle in sarcopenia: A systematic review. Clin. Nutr. 40, 3052–3061. https://doi.org/10.1016/j.clnu.2020.10.048 (2021).
Hirose, S. et al. Phase angle as an indicator of sarcopenia, malnutrition, and cachexia in inpatients with cardiovascular diseases. J. Clin. Med. https://doi.org/10.3390/jcm9082554 (2020).
Ushirozako, H. et al. Does preoperative prognostic nutrition index predict surgical site infection after spine surgery?. Eur. Spine J. 30, 1765–1773. https://doi.org/10.1007/s00586-020-06622-1 (2021).
Acarbas, A. A novel prognostic marker in patients undergoing spinal surgery: Prognostic Nutritional Index. J. Neurol. Surg. A Cent. Eur. Neurosurg. 80, 470–474. https://doi.org/10.1055/s-0039-1693031 (2019).
Azimi, P., Yazdanian, T. & Benzel, E. C. Determination of minimally clinically important differences for JOABPEQ measure after discectomy in patients with lumbar disc herniation. J. Spine Surg. 4, 102–108. https://doi.org/10.21037/jss.2018.03.11 (2018).
Barzilai, O. et al. Survival, local control, and health-related quality of life in patients with oligometastatic and polymetastatic spinal tumors: A multicenter, international study. Cancer 125, 770–778. https://doi.org/10.1002/cncr.31870 (2019).
van der Vliet, Q. M. J. et al. Long-term outcomes after operative treatment for tibial pilon fractures. OTA Int. 2, e043. https://doi.org/10.1097/OI9.0000000000000043 (2019).
Stienen, M. N. et al. Objective functional assessment using the “Timed Up and Go” test in patients with lumbar spinal stenosis. Neurosurg. Focus 46, E4. https://doi.org/10.3171/2019.2.FOCUS18618 (2019).
Inoue, H. et al. Handgrip strength correlates with walking in lumbar spinal stenosis. Eur. Spine J. 29, 2198–2204. https://doi.org/10.1007/s00586-020-06525-1 (2020).
Yamada, Y. et al. Electrical properties assessed by bioelectrical impedance spectroscopy as biomarkers of age-related loss of skeletal muscle quantity and quality. J. Gerontol. A Biol. Sci. Med. Sci. 72, 1180–1186. https://doi.org/10.1093/gerona/glw225 (2017).
Tanaka, S. et al. The decreasing phase angles of the entire body and trunk during bioelectrical impedance analysis are related to locomotive syndrome. J. Orthop. Sci. 24, 720–724. https://doi.org/10.1016/j.jos.2018.12.016 (2019).
Yamada, Y. et al. Phase angle obtained via bioelectrical impedance analysis and objectively measured physical activity or exercise habits. Sci. Rep. 12, 17274. https://doi.org/10.1038/s41598-022-21095-6 (2022).
Machado, F. V. C. et al. Relationship between body composition, exercise capacity and health-related quality of life in idiopathic pulmonary fibrosis. BMJ Open Respir. Res. https://doi.org/10.1136/bmjresp-2021-001039 (2021).
Thompson, A. J. & Turner, A. J. A comparison of the EQ-5D-3L and EQ-5D-5L. Pharmacoeconomics 38, 575–591. https://doi.org/10.1007/s40273-020-00893-8 (2020).
Rosa Silva, J. P. et al. Quality of life and functional independence in amyotrophic lateral sclerosis: A systematic review. Neurosci. Biobehav. Rev. 111, 1–11. https://doi.org/10.1016/j.neubiorev.2019.12.032 (2020).
Acknowledgements
We would like to thank Mr. Shingo Shimogawa, Ms. Reika Yamaryo, and Ms. Mai Ito for helping with the data acquisition.
Author information
Authors and Affiliations
Contributions
R.O. and R.H. participated in the study conception and design, interpretation of data, and drafting of the manuscript. S.I., K.H., S.K., and Y.T. performed data acquisition. K.M., Y.O., K.Y., T.Y., I.N., T.F., S.M., T.S., K.Y., K.H., K.S., H.M., and N.S. participated in the interpretation of data and critical revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Otsubo, R., Hashida, R., Murotani, K. et al. Phase angle is related to physical function and quality of life in preoperative patients with lumbar spinal stenosis. Sci Rep 13, 13909 (2023). https://doi.org/10.1038/s41598-023-40629-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40629-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.