Abstract
To compare outcomes after oblique lateral interbody fusion (OLIF) versus minimally invasive transforaminal lumbar interbody fusion (MISTLIF) with bilateral decompression via unilateral approach for treating mild to moderate symptomatic degenerative lumbar spinal stenosis (DLSS). We retrospectively compared patients who underwent single-level (L4/5) OLIF with an age-, sex-, and segment-matched MISTLIF with bilateral decompression via unilateral approach cohort. Perioperative data were collected for the operative time, intraoperative blood loss, drainage in the first postoperative day, postoperative hospital stay, cost, intraoperative fluoroscopy, and complications. Lumbar radiographs were measured for changes in posterior intervertebral space height (PISH), intervertebral space foramen height (IFH), intervertebral foramen area (IFA), and area of the spinal canal (ASC). Clinical and psychological outcomes included the visual analog scale (VAS), Oswestry Disability Index (ODI), and hospital anxiety and depression scale (HADS). 35 OLIF patients were compared with 35 MISTLIF patients in L4/5 DLSS. The OLIF group had shorter bedtime, postoperative hospital stays, less intraoperative and postoperative blood loss (all P < 0.05), but had more times of intraoperative fluoroscopy, longer operative time, and higher cost (all P < 0.05). The complication rates were equivalent (OLIF vs MISTLIF: 22.86% vs 17.14%). PISH (11.94 ± 1.78 mm vs 9.42 ± 1.94 mm, P < 0.05), IFH (23.87 ± 3.05 mm vs 21.41 ± 2.95 mm, P < 0.05), and IFA (212.14 ± 51.82 mm2 vs 177.07 ± 51.73 mm2, P < 0.05) after surgery were significantly increased in the OLIF group. The ASC was increased significantly after the operation in both groups, but the ASC in the MISTLIF group was increased significantly more than that in the OLIF group (450.04 ± 66.66 mm2 vs 171.41 ± 58.55 mm2, P < 0.05). The lumbar VAS scores at 1 month (1.89 ± 0.87 vs 2.34 ± 0.84, P = 0.028) and 6 months (1.23 ± 0.97 vs 1.80 ± 0.99, P = 0.018) after operation in the OLIF group were significantly lower. There were no significant differences in lower extremity VAS and ODI scores between the two groups. Compared with MISTLIF group, HADS scores on postoperative day 3 (2.91 ± 1.46 vs 4.89 ± 1.78, P < 0.05) and prior to hospital discharge (PTD) (2.54 ± 1.38 vs 3.80 ± 1.78, P = 0.002) in the OLIF group were decreased significantly. OLIF showed more advantages of less surgical invasion, lower incidence of postoperative low back pain, faster postoperative recovery, and less anxiety compared with MISTLIF. Regardless of cost, OLIF seems to be a better option to treat mild to moderate symptomatic DLSS.
Similar content being viewed by others
Introduction
Degenerative lumbar spinal stenosis (DLSS), which mostly occurred in elderly patients over the age of 65 years, is one of the main causes of low back pain and lower extremity dysfunction1. When the conservative treatment is ineffective or the symptoms are further aggravated, decompression and fusion become necessary treatment. The first-hand systematic evidence from the Swedish Lumbar Spine Study Group (SLSSG) suggests that lumbar fusion surgery has better clinical outcomes concerning reducing symptoms and improving limb function than nonsurgical treatment, and the cost is less expensive than conservative treatment in long-term follow-up2,3. Therefore, lumbar interbody fusion is a determined treatment for lumbar degenerative disease4.
Posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF) are common surgical methods for the treatment of lumbar spinal stenosis. Traditional PLIF is limited by causing iatrogenic injury to the paraspinal musculature, over dural extraction, and disruption of the posterior tension band. In recent years, TLIF has been the most commonly used to treat DLSS. TLIF can obtain a good decompression effect and maintain satisfactory spinal stability by resecting the bilateral facet joints and part of the lamina, loosening surrounding fibrous tissue, and implanting pedicle screws and intervertebral cage. TLIF also can be performed via a minimally invasive surgical approach. Although minimally invasive transforaminal lumbar interbody fusion (MISTLIF) can reduce the injury to the posterior branch of the spinal nerve, reduce the denervation of multifidus muscle and reduce the incidence of intramuscular degeneration and necrosis5, patients undergoing MISTLIF often suffer from chronic back pain after surgery, which may be due to the resection of paravertebral muscle and facet joints6. The surgical method that can maximize the preservation of facet joints and reduce paravertebral muscle injury is more helpful to reduce complications. Thus, more and more surgeons have been seeking minimally invasive surgical methods for DLSS. MISTLIF with bilateral decompression via unilateral approach can not only obtain good clinical effect but also preserve the contralateral articular process and reduce the incidence of complications7.
Oblique lateral interbody fusion (OLIF), another minimally invasive surgery, has recently been adopted by spine surgeons as a minimally invasive and rigid fixation procedure for degenerative disc diseases (DDD). In OLIF surgery, spine surgeons insert a large cage between the vertebrae to achieve indirect decompression through the retroperitoneal space via the interval between the psoas muscle and major vessel assisted by the retractor8. OLIF was reported with satisfactory efficacy in lumbar degenerative diseases in cohort studies9; however, rare studies compared its efficacy with MISTLIF surgery with bilateral decompression via a unilateral approach in DLSS10. The present study evaluates the radiographic and clinical outcomes after OLIF in comparison to an age-, sex-, and segment-matched cohort of patients undergoing bilateral decompression via a unilateral approach MISTLIF for the mild to moderate symptomatic DLSS.
Materials and methods
Ethics statement
This study was approved by the institutional review board of the ethics committee of Qingdao Municipal Hospital and was conducted in accordance with the Declaration of Helsinki. It was a retrospective cohort study comparing patients under-going single-level OLIF versus MISTLIF with bilateral decompression via a unilateral approach at a single center. The 2 cohorts were matched by sex, age, and segment. All the participants gave informed consent before taking part. The datasets analysed during the current study are not publicly available due privacy of the patients but are available from the corresponding author on reasonable request.
Patients
We finally retrospectively compared 35 patients who underwent single-level (L4/5) OLIF with an age-, sex-, and segment-matched MISTLIF with bilateral decompression via unilateral approach cohort from November 2018 to January 2021 (Fig. 1). The main basis for choosing the surgical method is as follows: (1) If the working corridor (distance between aorta and psoas major) allows, we prefer OLIF surgery, and if the working corridor does not allow, we choose MISTLIF. (2) MISTLIF and OLIF were utilized at different times. Early on, MISTLIF was mostly used to treat lumbar degenerative diseases, but OLIF was primarily used to treat them later on. Inclusion criteria: (1) single-level DLSS (L4/5) confirmed by imaging, including spinal stenosis with or without instability and spondylolisthesis (Meyerding grade ≤ II°); (2) mild to moderate symptomatic DLSS (Schizas11: B or C); (3) underwent MISTLIF with bilateral decompression via a unilateral approach (MISTLIF group) or OLIF combined with posterior fixation (OLIF group); (4) failure of conservative treatment. Exclusion criteria: (1) isthmic spondylolisthesis (2) severe symptomatic DLSS (Schizas: D); (3) combined with previous lumbar surgery, fracture, infection, or tumor; (4) osteoporosis; (5) combined with severe heart, lung, and brain diseases, coagulation dysfunction. All the patients were followed up at least for 12 months (ranges: 12 months to 24 months).
Surgical procedure
MISTLIF group
Each patient underwent tracheal intubation under general anesthesia. After the appropriate quadrant expandable channel was installed and the segment was correct, the soft tissue of the lamina and the facet surface were removed. Under the microscope, the unilateral lamina, superior and inferior articular processes, and intervertebral disc were removed, then the unilateral spinal canal was decompressed. After that, an appropriately sized interbody fusion cage was placed. The pedicle screw and the connecting rod were placed on the decompression side. The operating bed was tilted to the opposite side, and the magnification and field of view of the microscope were adjusted. The base of the spinous process and the contralateral part of the lamina was blurred away under the microscope. A laminator was used to dissect the ligament until the contralateral never root was revealed. The pedicle screw was fixed under the channel on the opposite side. Wound drainage was applied in all cases.
OLIF group
The procedure of OLIF was performed as reported by Fan12. In brief, the patient took the right lying position after general anesthesia. A 4-cm long incision was made 3.0–5.0 cm forward of the midpoint of the target intervertebral disc. Then separate the layers of abdominal muscles along the direction of the external oblique, the internal oblique, and the transverse abdominal muscle, respectively, and expose the retroperitoneal space. A working channel was placed and fixed after the correct surgical segment was determined with the guide needle by the C-arm X-ray. The target segment intervertebral disc was removed, then the cartilage endplate was scraped. A cage of appropriate height and length, which was filled with artificial bone, was knocked into the intervertebral space. After the position of the cage was confirmed well by the C-arm, close the incision layer by layer. Adjust the patient to a prone position and perform posterior internal fixation with pedicle screw instrumentation. Whether to place the drainage tube in the surgical area according to the bleeding condition in the operation.
Perioperative parameters
The perioperative clinical data of the patients were recorded, including the operative time, intraoperative blood loss, drainage in the first postoperative day, postoperative bedtime, hospital stay, cost (total cost and high-value medical consumables cost), intraoperative fluoroscopy, and complications. Transient thigh flexion weakness is usually occurred in OLIF surgery and refers to leg weakness or numbness that was only temporary in nature and went away during the first three months, even if surgery was not necessary.
Radiographic parameters
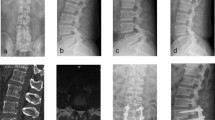
The imaging evaluation was performed using a PAC system. Posterior intervertebral space height (PISH), intervertebral space foramen height (IFH), and intervertebral foramen area (IFA) were collected from X-ray film. The PISH was measured as distance between posterior margin of inferior endplate of the L4 vertebra and posterior margin of superior endplate of the L5 vertebra on lateral radiograph. The IFH was measured as the longest distance between lower margin of the L4 pedicle and the upper margin of L5 pedicle on lateral radiograph. IFA was defined as the region enclosed by the postero-inferior portion of the superior vertebral body, the superior and inferior adjacent vertebral pedicles, the ligamentum flavum surface anteriorly, the postero-superior portion of the inferior vertebral body, the surface of the intervertebral disk posteriorly, and the superior and inferior adjacent vertebral pedicles. The measurement methods of PISH, IFH, and IFA were shown in Fig. 2. The area of the spinal canal (ASC) was calculated from the mean value of the three different slice areas from T2 magnetic resonance imaging (MRI) in the axial view (Fig. 3).
Clinical and psychological outcomes
Clinical outcomes were assessed using the visual analog scale (VAS), and Oswestry Disability Index (ODI) preoperatively, at 1, 6, 12 months, and final follow-up. The hospital anxiety and depression scale (HADS)13 was used to evaluate the psychological outcomes of patients preoperatively, at 3 days after the operation, and prior to hospital discharge (PTD). The final follow-up was defined as the periods between more than 12–24 months.
Statistical methods
Statistical analysis of the data was performed using IBM SPSS 20.0 statistical software (International Business Machines Corporation, Armonk, New York, USA). Continuous or discrete variables are presented as mean ± standard deviation (SD), and categorical variables are expressed as frequency or percentage. Data were screened for abnormalities and normalities using the Shapiro–Wilk test. Levene test was used to check homogeneity of variance. The Student-t test was used for analysis of groups with normally distributed continuous variables. The Mann–Whitney U test was used for analysis of discrete variables, categorical variables, and continuous variables that were not normally distributed. Multiple comparisons between samples on the VAS, ODI and HADS scores were analyzed by analysis of variance (ANOVA). Multiple comparisons between samples on smoking history, diagnosis and neurologic dysfunction was analyzed by the chi-square test. Differences with two-tailed P values < 0.05 were considered statistically significant.
Results
Demographics of patients
According to the inclusion and exclusion criteria, 86 patients were enrolled, and 70 patients achieved at final follow-up. A total of 35 patients who underwent MISTLIF were compared with a matched cohort of 35 patients who underwent OLIF both in the L4/5 segment (Fig. 1). The mean age and gender distributions were expectedly similar between the MISTLIF and OLIF groups. The BMI in the MISTLIF group was also comparable with the OLIF group. There were no significant differences in other baseline demographic characteristics including the history of the disease, smoking history, follow-ups, and neurological function between the 2 cohorts (Table 1).
Perioperative characteristics of patients
OLIF group had significantly shorter bedtime, less postoperative hospital stay, less intraoperative blood loss, and less postoperative drainage, but had more times of intraoperative fluoroscopy, longer operative time, and higher total cost and high-value medical consumables cost than the MISTLIF group (Table 2).
Radiographic results
Lateral X-rays showed that the PISH, IFH, and IFA after surgery were significantly increased in the OLIF group compared with those in the MISTLIF group (P < 0.01, Table 3). But the PISH, IFH, and IFA in the MISTLIF group were not significantly increased after the operation compared with those before the operation (P > 0.05, Table 4). Also, we found that the PISH, IFH, and IFA in the OLIF group were smaller than the MISTLIF group before operation (Table 5). There was no significant difference in ASC before operation between MISTLIF and OLIF group (Table 6). The ASC was increased significantly after the operation in both groups, but the ASC in the MISTLIF group was increased significantly more than the OLIF group (P < 0.05; Table 6).
Clinical and psychological outcomes
No significant differences were found in VAS scores (both lumbar and lower extremity) and ODI scores between the two groups at preoperative, postoperative 12 months, and final follow-up (P < 0.05, Table 7). However, the lumbar VAS scores at 1 month and 6 months after operation in the OLIF group were significantly lower than those in the MISTLIF group (Table 7). So did the ODI (Table 7). There were no significant differences in lower extremity VAS scores between the two groups at any follow-up point (P > 0.05, Table 7). There was no significant difference in HADS score between the MISTLIF and OLIF group preoperatively (8.43 ± 3.42 vs 7.94 ± 2.8, P = 0.519), which indicated that all patients felt anxious preoperatively (Fig. 4). However, the HADS scores on the postoperative day 3 (2.91 ± 1.46 vs 4.89 ± 1.78, P < 0.01) and PTD (2.54 ± 1.38 vs 3.80 ± 1.78, P < 0.01) in the OLIF group decreased significantly compared with those in the MISTLIF group (Fig. 4).
Complications
Considering complications, 8 patients (22.86%, 8/35) were found in the OLIF group, including 7 patients with transient thigh flexion weakness and 1 patient with segmental artery injury. While 6 patients (17.14%, 6/35) with complications were found in the MISTLIF group, including 1 patient with the dural tear, 5 patients with paresthesia or radiculitis. Paresthesia or radiculitis was significantly relieved after treatment with nerve nutrition, dehydration, and hormones.
Discussion
Preserving the soft tissue envelope and understanding the anatomy and biology of the posterior spinal musculature are key concepts in minimally invasive spine surgery14. Based on this concept, the minimally invasive treatment of DLSS is applied. Many scholars have reported that MISTLIF through bilateral decompression via unilateral approach has achieved good results in the treatment of DLSS15,16,17. OLIF is a minimally invasive anterior retroperitoneal approach surgery, which has been very popular in recent years. In OLIF surgery, the surgeon reaches the operative segment through the anatomical space between the abdominal aorta and the psoas muscle via the retroperitoneal space and preserves the integrity of the posterior structure of the spine. In this study, OLIF shows more advantages in the treatment of single-segment lumbar spinal stenosis than MISTLIF.
OLIF had less bleeding and less postoperative drainage than MISTLIF as reported previously18. The possible reasons are as follows: (1) The OLIF passes through the retroperitoneal approach to the disc, with few peripheral vessels, which are easily protected under direct vision. (2) MISTLIF needs to open the spinal canal, which can easily damage the venous plexus and cause bleeding; especially when contralateral decompression is performed, effective hemostasis is difficult. (3) Bony structural damage is avoided since laminectomy is not required in OLIF. The decrease in the incidence of iatrogenic disturbance to the surrounding tissues and nerves ultimately yields better outcomes in surgical bleeding19. The shorter postoperative hospital stay and bedtime in the OLIF group were closely related to less intraoperative injury and less postoperative drainage, which was controversial in previous studies20,21. Pain caused by injury to paravertebral muscles and articular processes in the MISTLIF group was also responsible for increased postoperative hospital stay and bedtime. However, the times of fluoroscopy were significantly increased in the OLIF group than those in the MISTLIF group. Possible reasons are as follows: (1) Repeated fluoroscopy is required to determine the orientation and location of the cage during the OLIF procedure. (2) Spine surgeons are familiar with posterior surgery and unfamiliar with lateral surgery. Therefore, the lack of OLIF surgical experience is also the reason for the increase in fluoroscopy times. In contrast to previous reports22,23, the intraoperative time in the OLIF group was longer than in the MISTLIF group. The possible reasons are as follows: (1) Time of repositioning and disinfection in the OLIF procedure was also included in the intraoperative time in our study. (2) The repeated intraoperative fluoroscopy, surgeon’s expertise, and repertoire were the other related reasons. Therefore, to avoid occupation of time in changing the patient’s position, repreparing and redrapping the surgical field, it has been reported that posterior fixation is performed under the same position. Blizzard reported that the mean operative time of single-position (SP) LLIF (lateral lumbar interbody fusion) or OLIF with bilateral pedicle screw fixation was 87.9 min (range: 49–195 min)24. According to a study comparing single-position versus dual-position (DP) surgery for pedicle screw fixation and lateral interbody fusion, SP surgery could reduce the average surgery time by about 31 min25. A recent meta-analysis also showed that SP surgery in LLIF (including OLIF technique) combined with pedicle screw fixation significantly shortened operative time compared with DP LLIF26. Thus, enhanced the surgeon’s training of posterior fixation in single position can significantly improve surgical efficiency. Higher cost in the OLIF group is mainly related to high-value medical consumables (Cage and artificial bone). This shortcoming may limit the widespread use of OLIF in the treatment of DLSS.
The most important treatment of DLSS is decompression by increasing the area of the spinal canal. OLIF is an indirect decompression procedure, whereas MISTLIF is a direct decompression procedure. In our study, both achieved effective decompression. In this study, although the preoperative PISH in the OLIF group was smaller than that in the MISTLIF group, the postoperative PISH was found significantly larger in the OLIF group. The effective increment and maintenance of IFH and IFA in the OLIF group were closely related to the increment of PISH. The possible reasons are as follows: (1) The cage, which was inserted into the disc gap through the Kambin triangle in the MISTLIF procedure, is smaller than that in the OLIF procedure. It is reported that the triangle between the exiting and traversing nerve roots above the superior margin of the inferior pedicle is narrow. The triangle area is from 1.83 to 2.19 cm227. If the cage was large in the MISTLIF procedure, the never roots were easy to injure. Thus the cage was confined by the anatomy of the Kambin triangle and the PISH in the MISTLIF group was not larger enough. (2) In MISTILF surgery, only one side of the facet joints was resected while the contralateral side was usually preserved, so the intervertebral space may not be effectively expanded, especially for patients with facet osteophytosis28. Although there was no significant increase in PISH, IFH, and IFA in the MISTLIF group, the postoperative spinal canal area was significantly larger than that in the OLIF group, reflecting the advantage of direct decompression.
Postoperative pain relief and lumbar function recovery were the key focus of both the surgeons and patients. In our study, VAS and ODI scores were significantly decreased, especially in the first 6 months. The symptoms were further improved over time in the follow-up periods and reached a steady state. However, the lumbar VAS and ODI scores at 1 month and 6 months after operation in the OLIF group were significantly lower than those in the MISTLIF group, which was consistent with Kim’s report10. The reasons are as follows: (1) The paraspinal muscles are not separated from the bony structure, and there is no damage to the posterior branch of the nerve, which reduces the denervation or fatty degeneration of the paraspinal muscles, thereby reducing the incidence of lower back pain in the OLIF group5,29. (2) There was little iatrogenic damage to nerves and tissues around the spinal canal in the OLIF group30. Although there was no significant difference in VAS and ODI scores of the lower extremity, we found that there were more patients with transient thigh flexion weakness in the OLIF group. This was likely due to genitofemoral nerve disturbance during the procedure, in which the disturbance is usually temporary and reversible. Both the surgeon's skill and the patient's mental health influence the clinical outcome. The quality of life of patients with lumbar spinal stenosis is closely related to their emotional status31. It is reported that anxiety status after spinal surgery could lead to poor clinical outcomes32. Pain is considered a psychosomatic factor that connects both the physical and psychological domains33. It was reported by the previous studies that poor psychological outcomes were correlated with elevated pain scores and lower physical function34,35. In a recent study, it was reported that the postoperative HADS scores were positively correlated with the low back pain VAS scores36. At the same time, depression can also negatively influence rehabilitation after surgery37. In my opinion, there is a bidirectional relationship between depression and functional disability. In our study, the HADS scores on the postoperative day 3 and PTD in the OLIF group decreased significantly compared with those in the MISTLIF group. This may be related to the lower lumbar VAS scores after operation in the OLIF group. In addition to pain, other factors may also affect the psychological state of patients after surgery, such as early getting out of bed, drainage, etc38. Shorter bedtime and hospital stay after operation, less intraoperative blood loss, and postoperative drainage in the OLIF group would be other reasons.
This study also has some limitations. First, it is a retrospective cohort study, a multi-center study needs to be considered to decrease the bias. Second, the surgeons and patients had a different understanding of prognosis and treatment, which may affect the evaluation of results and cause bias. Third, the small sample size and short follow-up period may have affected the strength of the statistical analysis. Although OLIF could acquire good indirect decompression efficacy, it is still necessary to extend the follow-up period to confirm this conclusion because the spinal canal could remodel during long-term follow-up after surgery39. A high-quality study of a large sample size and long-term follow-up period is still needed to compare the results of OLIF and MISTLIF.
Conclusion
Both OLIF and MISTLIF with bilateral decompression via unilateral approach are effective treatments for mild to moderate symptomatic DLSS. While both OLIF and MISTLIF provide optimal clinical outcomes, in comparison to an age-, sex-, and segment-matched MISTLIF cohort, OLIF showed the advantages of less surgical invasion, lower incidence of postoperative low back pain, faster postoperative recovery, and less anxiety in single-level DLSS. Regardless of cost, OLIF seems to be a better option to treat mild to moderate symptomatic DLSS in modern days.
Data availability
The datasets analysed during the current study are not publicly available due privacy of the patients but are available from the corresponding author on reasonable request.
References
Wang, J. et al. Changes in kinematics, kinetics, and muscle activity in patients with lumbar spinal stenosis during gait: Systematic review. Spine J. 22(1), 157–167. https://doi.org/10.1016/j.spinee.2021.06.003 (2022).
Fritzell, P., Hägg, O., Wessberg, P., Nordwall, A., Swedish Lumbar Spine Study Group. 2001 Volvo Award Winner in Clinical Studies: Lumbar fusion versus nonsurgical treatment for chronic low back pain: A multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976) 26(23), 2521–2532. https://doi.org/10.1097/00007632-200112010-00002 (2001).
Fritzell, P., Hagg, O., Jonsson, D., Nordwall, A., Swedish Lumbar Spine Study Group. Cost-effectiveness of lumbar fusion and nonsurgical treatment for chronic low back pain in the Swedish Lumbar Spine Study: A multicenter, randomized, controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976) 29, 421–434. https://doi.org/10.1097/01.brs.0000102681.61791.12 (2004).
Mobbs, R. J., Phan, K., Malham, G., Seex, K. & Rao, P. J. Lumbar interbody fusion: Techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J. Spine Surg. 1(1), 2–18. https://doi.org/10.3978/j.issn.2414-469x.2015.10.05 (2015).
Ozgur, B. M., Hughes, S. A., Baird, L. C. & Taylor, W. R. Minimally disruptive decompression and transforaminal lumbar interbody fusion. Spine J. 6(1), 27–33. https://doi.org/10.1016/j.spinee.2005.08.019 (2006).
Min, S. H., Kim, M. H., Seo, J. B., Lee, J. Y. & Lee, D. H. The quantitative analysis of back muscle degeneration after posterior lumbar fusion: Comparison of minimally invasive and conventional open surgery. Asian Spine J. 3(2), 89–95. https://doi.org/10.4184/asj.2009.3.2.89 (2009).
Zhang, Y., Xu, C., Zhou, Y. & Huang, B. Minimally invasive computer navigation-assisted endoscopic transforaminal interbody fusion with bilateral decompression via a unilateral approach: Initial clinical experience at one-year follow-up. World Neurosurg. 106, 291–299. https://doi.org/10.1016/j.wneu.2017.06.174 (2017).
Silvestre, C., Mac-Thiong, J. M., Hilmi, R. & Roussouly, P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: Oblique lumbar interbody fusion in 179 patients. Asian Spine J. 6(2), 89–97. https://doi.org/10.4184/asj.2012.6.2.89 (2012).
Chang, S. Y. et al. Impact of preoperative diagnosis on clinical outcomes of oblique lateral interbody fusion for lumbar degenerative disease in a single-institution prospective cohort. Orthop. Surg. 11(1), 66–74. https://doi.org/10.1111/os.12419 (2019).
Lin, G. X. et al. Clinical and radiologic outcomes of direct versus indirect decompression with lumbar interbody fusion: A matched-pair comparison analysis. World Neurosurg. 119, e898–e909. https://doi.org/10.1016/j.wneu.2018.08.003 (2018).
Schizas, C. et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976) 35(21), 1919–1924. https://doi.org/10.1097/brs.0b013e3181d359bd (2010).
Zeng, Z. Y. et al. Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop. Surg. 10(2), 98–106. https://doi.org/10.1111/os.12380 (2018).
Lee, J., Kim, H. S., Shim, K. D. & Park, Y. S. The effect of anxiety, depression, and optimism on postoperative satisfaction and clinical outcomes in lumbar spinal stenosis and degenerative spondylolisthesis patients: Cohort study. Clin. Orthop. Surg. 9(2), 177–183. https://doi.org/10.4055/cios.2017.9.2.177 (2017).
Kim, P. D. & Kim, C. W. Philosophy and Biology of Minimally Invasive Spine Surgery. Minimally Invasive Spine Surgery 15–21 (Springer Science Business Media, 2014).
Min, S. H., Yoo, J. S. & Lee, J. Y. Usefulness of contralateral indirect decompression through minimally invasive unilateral transforaminal lumbar interbody fusion. Asian Spine J. 8, 453–461. https://doi.org/10.4184/asj.2014.8.4.453 (2014).
Kim, M. C. et al. Can unilateral-approach minimally invasive transforaminal lumbar interbody fusion attain indirect contralateral decompression? A preliminary report of 66 MRI analysis. Eur. Spine J. 23, 1144–1149. https://doi.org/10.1007/s00586-014-3192-3 (2014).
Yang, Y. et al. Microendoscopy-assisted minimally invasive transforaminal lumbar interbody fusion for lumbar degenerative disease: Short-term and medium-term outcomes. Int. J. Clin. Exp. Med. 8(11), 21319–21326 (2015).
Hiyama, A. et al. Short-term comparison of preoperative and postoperative pain after indirect decompression surgery and direct decompression surgery in patients with degenerative spondylolisthesis. Sci. Rep. 10(1), 18887. https://doi.org/10.1038/s41598-020-76028-y (2020).
Ye, J. H., Ding, J. L., Xiang, Z. Y. & Zhu, S. P. Minimally invasive anterior oblique lumbar interbody fusion (OLIF) for degenerative lumbar disease. Asian J. Surg. 43(12), 1214–1215. https://doi.org/10.1016/j.asjsur.2020.10.003 (2020).
Li, H. M., Zhang, R. J. & Shen, C. L. Radiographic and clinical outcomes of oblique lateral interbody fusion versus minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar disease. World Neurosurg. 122, e627–e638. https://doi.org/10.1016/j.wneu.2018.10.115 (2019).
Sheng, S. R. et al. Minimally invasive surgery for degenerative spondylolisthesis: Transforaminal or oblique lumbar interbody fusion. J. Comp. Eff. Res. 9(1), 45–51. https://doi.org/10.2217/cer-2019-0055 (2020).
Zhu, H. F. et al. Comparison of oblique lateral interbody fusion (OLIF) and minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) for treatment of lumbar degeneration disease: A prospective cohort study. Spine (Phila Pa 1976) 47(6), E233–E242. https://doi.org/10.1097/brs.0000000000004303 (2022).
Hung, S. F. et al. Comparison of outcomes between indirect decompression of oblique lumbar interbody fusion and MIS-TLIF in one single-level lumbar spondylosis. Sci. Rep. 11(1), 12783. https://doi.org/10.1038/s41598-021-92330-9 (2021).
Blizzard, D. J. & Thomas, J. A. MIS single-position lateral and oblique lateral lumbar interbody fusion and bilateral pedicle screw fixation: Feasibility and perioperative results. Spine 43(6), 440–446. https://doi.org/10.1097/BRS.0000000000002330 (2018).
Hiyama, A. et al. Comparison of radiological changes after single-position versus dual-position for lateral interbody fusion and pedicle screw fixation. BMC Musculoskelet. Disord. 20(1), 601. https://doi.org/10.1186/s12891-019-2992-3 (2019).
Guiroy, A. et al. Single-position surgery versus lateral-then-prone-position circumferential lumbar interbody fusion: A systematic literature review. World Neurosurg. 151, e379–e386. https://doi.org/10.1016/j.wneu.2021.04.039Q (2021).
Hardenbrook, M., Lombardo, S., Wilson, M. C. & Telfeian, A. E. The anatomic rationale for transforaminal endoscopic interbody fusion: A cadaveric analysis. Neurosurg. Focus 40(2), E12. https://doi.org/10.3171/2015.10.focus15389 (2016).
Robertson, P. A., Armstrong, W. A., Woods, D. L. & Rawlinson, J. J. Lordosis recreation in transforaminal and posterior lumbar interbody fusion: A cadaveric study of the influence of surgical bone resection and cage angle. Spine (Phila Pa 1976) 43(22), E1350–E1357. https://doi.org/10.1097/brs.0000000000002705 (2018).
Fu, C. J., Chen, W. C., Lu, M. L., Cheng, C. H. & Niu, C. C. Comparison of paraspinal muscle degeneration and decompression effect between conventional open and minimal invasive approaches for posterior lumbar spine surgery. Sci. Rep. 10(1), 14635. https://doi.org/10.1038/s41598-020-71515-8 (2020).
Fujibayashi, S. et al. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976) 40(3), E175–E182. https://doi.org/10.1097/brs.0000000000000703 (2015).
Özdemir, E., Paker, N., Bugdayci, D. & Tekdos, D. D. Quality of life and related factors in degenerative lumbar spinal stenosis: A controlled study. J. Back Musculoskelet. Rehabil. 28(4), 749–753. https://doi.org/10.3233/bmr-140578 (2015).
Celestin, J., Edwards, R. R. & Jamison, R. N. Pretreatment psychosocial variables as predictors of outcomes following lumbar surgery and spinal cord stimulation: A systematic review and literature synthesis. Pain Med. 10(4), 639–653. https://doi.org/10.1111/j.1526-4637.2009.00632.x (2009).
Gragnano, A., Villotti, P., Larivière, C., Negrini, A. & Corbière, M. A systematic search and review of questionnaires measuring individual psychosocial factors predicting return to work after musculoskeletal and common mental disorders. J. Occup. Rehabil. 31(3), 491–511. https://doi.org/10.1007/s10926-020-09935-6 (2021).
Hartman, T. J. et al. Poor mental health scores correlate with inferior outcomes following minimally invasive transforaminal lumbar interbody fusion. Acta Neurochir. 165(7), 1931–1942. https://doi.org/10.1007/s00701-023-05557-y (2023).
Burgstaller, J. M. et al. The influence of pre- and postoperative fear avoidance beliefs on postoperative pain and disability in patients with lumbar spinal stenosis: Analysis of the lumbar spinal outcome study (LSOS) data. Spine 42(7), E425–E432. https://doi.org/10.1097/BRS.0000000000001845 (2017).
Yu, B. et al. Psychological and functional comparison between minimally invasive and open transforaminal lumbar interbody fusion for single-level lumbar spinal stenosis. Orthop. Surg. 13(4), 1213–1226. https://doi.org/10.1111/os.12986 (2021).
Ghoneim, M. M. & O’Hara, M. W. Depression and postoperative complications: An overview. BMC Surg. 16, 5. https://doi.org/10.1186/s12893-016-0120-y (2016).
de Groot, K. I. et al. The influence of psychological variables on postoperative anxiety and physical complaints in patients undergoing lumbar surgery. Pain 69(1–2), 19–25. https://doi.org/10.1016/s0304-3959(96)03228-9 (1997).
Ohtori, S. et al. Change of lumbar ligamentum flavum after indirect decompression using anterior lumbar interbody fusion. Asian Spine J. 11(1), 105–112. https://doi.org/10.4184/asj.2017.11.1.105 (2017).
Author information
Authors and Affiliations
Contributions
L.L. and D.W. made contributions to the conception and design of the study. H.X. collected, analyzed, and interpreted the follow-up data with the assistance of Z.H., L.J., and L.C. L.L. drafted the original manuscript and submitted it to D.W. for review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, L., Xue, H., Han, Z. et al. Comparison between OLIF and MISTLIF in degenerative lumbar stenosis: an age-, sex-, and segment-matched cohort study. Sci Rep 13, 13188 (2023). https://doi.org/10.1038/s41598-023-40533-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40533-7
This article is cited by
-
Ultrasonic bone curette-assisted unilateral approach for bilateral decompression with MIS-TLIF for severe lumbar spinal stenosis
BMC Musculoskeletal Disorders (2024)
-
Letter to the editor: efficacy of OLIF combined with pedicle screw internal fixation for lumbar spinal stenosis on spinal canal changes before and after surgery
Journal of Orthopaedic Surgery and Research (2023)
-
Letter to the Editor: Evaluating the efficacy of OLIF combined with pedicle screw internal fixation for lumbar spinal stenosis
Journal of Orthopaedic Surgery and Research (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.