Abstract
While high-level evidence is lacking, numerous retrospective studies have depicted the value of supplemental oxygen in idiopathic pulmonary fibrosis (IPF) and other interstitial lung diseases, and its use should be encouraged where necessary. The clinical course and survival of patients with IPF who have been introduced to oxygen therapy is still not fully understood. The objective of this study was to clarify overall survival, factors associated with prognosis, and causes of death in IPF patients after the start of oxygen therapy. This is a prospective cohort multicenter study, enrolling patients with IPF who started oxygen therapy at 19 hospitals with expertise in interstitial lung disease. Baseline clinical data at the start of oxygen therapy and 3-year follow-up data including death and cause of death were assessed. Factors associated with prognosis were analyzed using univariable and multivariable analyses. One hundred forty-seven eligible patients, of whom 86 (59%) were prescribed ambulatory oxygen therapy and 61 (41%) were prescribed long-term oxygen therapy, were recruited. Of them, 111 died (76%) during a median follow-up of 479 days. The median survival from the start of oxygen therapy was 537 ± 74 days. In the univariable analysis, low body mass index (BMI), low forced vital capacity (FVC), low diffusion capacity (DLCO), resting hypoxemia, short 6 min-walk distance, and high COPD assessment test (CAT) score were significantly associated with poor prognosis. Multivariable analysis revealed low BMI, low FVC, low DLCO, low minimum SpO2 on 6MWT, and high CAT score were independent factors for poor prognosis. The overall survival of IPF patients after starting oxygen therapy is about 1.5 years. In addition to pulmonary function tests, 6MWT and patient reported outcomes can be used to predict prognosis more accurately.
Clinical Trial Registration: UMIN000009322.
Similar content being viewed by others
Introduction
IPF is a specific form of chronic, progressive fibrosing interstitial pneumonia of unknown cause occurring in adults. It is characterized by a progressive decline of pulmonary function, worsening dyspnea, impaired health-related quality of life, and poor prognosis with a median untreated survival of 3–5 years from diagnosis1,2. One of the most important non-pharmacologic therapies in IPF is supplemental oxygen therapy. Current guidelines recommend that patients with IPF and clinically significant resting hypoxemia should be treated with long-term oxygen therapy (LTOT), which is based on very low-quality evidence1,3,4,5,6. For adults with interstitial pneumonia who have severe exertional room air hypoxemia without resting hypoxemia, ATS guideline suggests prescribing ambulatory oxygen therapy (AOT), with low-quality evidence7. Frequently, AOT is prescribed for the management of episodic breathlessness and with the expectation of improved exercise capacity3,8,9,10,11,12. There is no guidance on the use of AOT for patients with IPF and data on the proper timing, purpose, type, and prognosis of oxygen therapy in patients with IPF are limited.
In recent years, the importance of discussing end-of-life care for IPF patients has been emphasized. Indeed, the initiation of oxygen therapy is recognized as an appropriate trigger for advance care planning13. In conducting precise advance care planning (ACP) it is important to identify overall survival and prognostic factors for IPF patients after the initiation of oxygen therapy. We think that the prognostic factors at that time may differ depending on the degree of progression of the disease. Therefore, we conducted this cohort study to clarify overall survival, cause of death, and factors associated with the prognosis of IPF patients after starting oxygen therapy.
Material and methods
Study population and design
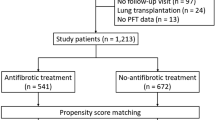
This registry was designed to survey data from patients with IPF who were started on supplemental oxygenation therapy at home (UMIN000009322). Participants were recruited from 19 Japanese hospitals with expertise in interstitial lung disease between December 2012 and November 2015. The inclusion criteria were as follows: a diagnosis of IPF, age > 18 years, and home oxygen therapy being started for the first time. We included not only LTOT but also AOT used only during exertion. We did not include nocturnal only oxygen therapy without daytime use. The diagnoses of IPF were made by the participating investigators based on the 2011 IPF international guidelines1. In Japan, the indications for oxygen therapy for patients with chronic respiratory failure are based on the following criteria: 1) arterial partial pressure of oxygen (PaO2) ≦ 55mmHg (7.3 kPa) or oxygen saturation as measured by pulse oximetry (SpO2) ≦ 88%; 2) PaO2 = 56–59 mmHg (7.5–7.9 kPa) or SpO2 = 89% plus signs of cor pulmonale or pulmonary hypertension. This study included not only patients who necessarily met these inclusion criteria, but also those who did not meet the criteria were included at the discretion of physicians at specialized facilities. The decision to start home oxygen therapy and the type of oxygen therapy depended on each site’s physicians. To exclude reasons for oxygen induction other than IPF, patients whose condition was unstable, or who had a comorbidity likely to affect survival at the start of supplemental oxygenation therapy, such as severe heart failure, recent pulmonary embolism, or advanced malignancy, were excluded.
In this study, LTOT was defined as a prescription of oxygen for ≥ 15 h per day, and AOT was defined as a prescription < 15 h per day.
The clinical data were collected at the time oxygen therapy was started (baseline). The subject baseline characteristics included age, sex, body mass index (BMI), smoking history, experience of surgical lung biopsy, duration of IPF, past history of acute exacerbation, forced vital capacity (FVC), diffusing capacity of the lung for carbon monoxide (DLCO), presence of pulmonary hypertension, resting hypoxemia (oxygen saturation of peripheral blood (SpO2) < 88%), arterial partial pressure of carbon dioxide (PaCO2), 6-min walk test (6MWT) distance, minimum SpO2, modified Medical Research Council Dyspnea (mMRC) scale, and Gender Age and Physiology (GAP) stage14. The diagnosis of pulmonary hypertension in this study was defined as mean pulmonary artery pressure ≥ 25 mmHg measured by right heart catheter, or when the following echocardiography criteria were met. On echocardiography, a diagnosis of pulmonary hypertension was made if the tricuspid regurgitation peak velocity (TRV) was 2.9–3.4 m/s with other signs of pulmonary hypertension or if the TRV was > 3.4 m/s15. Patient reported outcomes were measured by COPD Assessment Test (CAT), which has been successfully used in patients with interstitial lung disease in past studies16,17. Follow-up data (date of death and cause of death) were collected 3 years after the last case enrollment. The cause of death was determined by the investigators at each site after receiving the medical records and death certificate.
Statistical analysis
Data for continuous variables are presented as median (interquartile range) or n (%). Overall survival was analyzed from the time oxygen therapy was started to either death by any cause or lung transplantation. The survival rate was estimated by the Kaplan–Meier method. Univariable Cox proportional regression was used to find prognostic factor candidates. Variables that showed a significant result univariately (p < 0.1) were included in the corresponding multivariable analysis. Given the correlation between mMRC and CAT established in previous studies on COPD18, we prospectively decided not to include mMRC as a variable in the multivariable analysis to avoid potential issues of multicollinearity. In this study, the composite variable, GAP index, was not employed in the multivariate analysis because gender, age, FVC, and DLCO were evaluated as variables. Additionally, as DLCO was often not measurable, we created another model that did not include it as a factor in the multivariate analysis. We planned to accumulate data on 120 deaths to evaluate up to 12 prognostic factors. According to a previous report19, the 3-year mortality rate of IPF patients who were started on oxygen therapy was 80%, and the sample size was calculated to be 150 patients. Independent prognostic factors were identified in the multivariable Cox proportional hazard analysis. To compare AOT and LTOT, survival was assessed using a Cox proportional hazard model with extracted independent prognostic factors as covariates. In all study analyses, p < 0.05 was considered significant. All statistical calculations were performed using SPSS version 25.0 (SPSS Inc., Chicago, IL, USA).
Ethics approval
This study was performed in accordance with the Declaration of Helsinki. The study was approved by the human-research review board at Tosei General Hospital (Tosei 301) and each site, and all patients provided written informed consent.
Results
A total 147 IPF patients were included in the study, and the median length of follow-up was 479 days for all patients. Characteristics of the study population at the baseline are summarized in Table 1. The majority of patients were male (80%) with a median duration of IPF before enrollment of 46 months. Twenty-two (15%) patients had hypoxemia (SpO2 < 88%) at rest, and 124 (84%) had hypoxemia (SpO2 < 90%) on exertion. Of the 53 patients diagnosed with pulmonary hypertension, 9 were diagnosed by right heart catheter and the remaining 44 were diagnosed by echocardiography alone. Eighty-six (59%) patients were prescribed AOT and 61 (41%) were prescribed LTOT (Supplementary Table 1).
Eighty-eight (60%) patients met at least one criterion for the introduction of oxygen therapy, while the remaining 59 (40%) did not meet any of the criteria. Patients who did not meet any of the criteria had hypoxemia on exertion and a higher CAT score, as did patients who met the criteria. There was no difference in prognosis between those who met the criterion and those who did not (Table 2).
During the observation period, 113 patients died, and one underwent lung transplantation. Causes of death were chronic respiratory failure in 59 (52%), acute exacerbation in 31 (27%), and lung cancer in 5 (4%). The median survival from the start of oxygen therapy was 537 ± 74 days. Kaplan–Meier survival curves are displayed in Fig. 1.
Factors associated with all-cause mortality
Univariable Cox regression analysis demonstrated that lower FVC (p < 0.001), lower DLCO (p = 0.004), resting hypoxemia (SpO2 < 88%) (p = 0.006), shorter 6MWT distance (p = 0.010), and higher CAT score (p < 0.001), higher mMRC scale (p = 0.006), and higher GAP stage (p < 0.001) were significantly associated with poor prognosis (Table 3). On the other hand, duration of IPF, presence of pulmonary hypertension, and meeting criteria for indication of oxygen therapy were not associated with prognosis. Comorbidities were not associated with prognosis. The study’s criteria, which excluded patients with comorbidities likely to affect survival, may have influenced this result (data not shown). Multivariable analysis revealed that lower BMI (p = 0.008), lower FVC (p = 0.003), lower DLCO (p = 0.030), resting hypoxemia (SpO2 < 88%) (p = 0.034), lower minimum SpO2 on 6MWT (p = 0.004) and higher CAT (p = 0.021) were significantly associated with poor prognosis (Table 3). In the other multivariable model, excluding DLCO, lower BMI (p = 0.028), lower FVC (p < 0.001), shorter 6MWT distance (p = 0.002), lower minimum SpO2 on 6MWT (p < 0.001), and higher CAT (p = 0.009) were significantly associated with poor prognosis (Table 3).
Discussion
This is the first prospective study to investigate the overall survival of patients with IPF after the start of oxygen therapy. In our cohort, the median survival time from the start of oxygen therapy was 17.7 months. Several past retrospective studies reported survival data for patients with interstitial lung disease who started oxygen therapy. Chailleux et al. reported that the prognosis of IPF patients after the start of oxygen therapy was 15–18 months19. In a Swedish nationwide study, the median survival time of patients with interstitial lung disease, not limited to IPF, was 8.4 months after the start of oxygen therapy20. In a Finnish single-center study, the median survival time of the patients with various interstitial lung diseases was 10.8 months21. Previous reports have shown that patients with interstitial lung disease did not survive long after oxygen therapy was initiated, which was also demonstrated in our cohort. In contrast to previous reports, our study is prospective and included only patients with IPF diagnosed according to the 2011 IPF international guidelines. In addition, we excluded patients whose condition was unstable, or who had a comorbidity likely to affect survival at the start of supplemental oxygenation therapy, such as severe heart failure or advanced malignancy.
Although many studies on prognostic factors in IPF have been published, there is a lack of prospective studies conducted from the time that oxygen therapy is started. In this prospective study, low BMI, low FVC, low DLCO, low minimum SpO2 on 6MWT, and high CAT score were independently associated factors for poor survival. Some studies have suggested that lower BMI may be associated with poor prognosis in IPF22,23,24,25. This study proved that low BMI is an independent factor for a poor prognosis even in advanced stage IPF. Although FVC is widely recognized as a prognostic factor for IPF, it has not been reported as an independent poor prognostic factor in advanced cases such as those with pulmonary hypertension and those on the waiting list for lung transplantation26,27,28. A possible reason for the discrepancy may be that the FVC percent predicted was about 60% in this study, while it was about 50% in the previously reported advanced cases, indicating that the lung function in our study was still preserved.
In stable IPF, the minimum SpO2 on 6MWT is known to be an independent poor prognostic factor29,30. In this study, the minimum SpO2 on 6MWT was found to be a factor of poor prognosis independent of other poor prognostic factors of poor prognosis including resting hypoxemia. Therefore, the 6-min walk test may be a useful tool to predict prognosis when introducing oxygen therapy to IPF patients.
In this study, we used CAT instead of St. George’s Respiratory Questionnaire (SGRQ) to assess the health status of patients with ILD. The CAT was not developed for patients with IPF, but its scores are strongly correlated with those of the SGRQ, and is a short questionnaire that shows good and valid measurement properties for assessing the health status of patients with ILD17. Several previous studies reported that the SGRQ total score was an independent prognostic factor in patients with mild to moderate IPF31,32. Although we targeted advanced cases, prognostic factors in this cohort were similar to those reported in non-severe cases.
In recent years, there has been growing recognition that advanced care planning and palliative care are important as an integral part of treating patients with IPF21,33. Based on our results, the median survival period after the introduction of oxygen therapy is only about one and a half years, regardless of whether the patient meets the criteria for the introduction of oxygen therapy. Therefore, the initiation of oxygen therapy should be considered a trigger for advance care planning discussions and palliative care consultation, especially in patients with low BMI, low FVC, low DLCO, low minimum SpO2 on 6MWT, or high CAT score.
There are several limitations to our study. First, we did not validate our results in an external cohort, and so we think further studies are needed to confirm these conclusions. Second, in our cohort, all patients were recruited from Japan only. This data may not be applicable to all countries, as different countries have different criteria for introducing oxygen therapy. Third, we were unable to collect information about medication during the follow-up period. Antifibrotic drugs have been shown to reduce the rate of decline in the FVC and improve prognosis of IPF. In the future, it will be necessary to analyze the effects of antifibrotic drug use in patients with advanced IPF.
In conclusion, the median survival of IPF patients after starting oxygen therapy is only about 1.5 years. Multivariable analysis at the time oxygen therapy is started revealed that low BMI, low FVC, low DLCO, low minimum SpO2 on 6MWT, and high CAT score were independent factors for a poor prognosis. In addition to pulmonary function tests, 6MWT and patient reported outcomes can be used to predict prognosis more accurately.
Data availability
The data that support the findings of this study available from the corresponding author upon reasonable request.
Abbreviations
- ACP:
-
Advance care planning
- AOT:
-
Ambulatory oxygen therapy
- BMI:
-
Body mass index
- CAT:
-
COPD assessment test
- DLCO :
-
Diffusion capacity of the lung for carbon monoxide
- FVC:
-
Forced vital capacity
- GAP:
-
Gender, age and physiology
- IPF:
-
Idiopathic pulmonary fibrosis
- IQR:
-
Interquartile range
- LTOT:
-
Long-term oxygen therapy
- mMRC:
-
Modified Medical Research Council Dyspnea
- N/A:
-
Not applicable
- PaCO2 :
-
Arterial partial pressure of carbon dioxide
- PaO2 :
-
Arterial partial pressure of oxygen
- SGRQ:
-
St. George’s respiratory questionnaire
- SpO2 :
-
Oxygen saturation of peripheral blood
- TRV:
-
Tricuspid regurgitation peak velocity
- 6MWT:
-
Six-minute walk test
References
Raghu, G. et al. An official ATS/ERS/JRS/ALAT statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management. Am. J. Respir. Crit. Care Med. 183, 788–824 (2011).
Mura, M. et al. Predicting survival in newly diagnosed idiopathic pulmonary fibrosis: A 3-year prospective study. Eur. Respir. J. 40, 101–109 (2012).
Bell, E. C. et al. Oxygen therapy for interstitial lung disease: A systematic review. Eur. Respir. Rev. 26, 160080 (2017).
Johannson, K. A. et al. Supplemental oxygen in interstitial lung disease: An art in need of science. Ann. Am. Thorac. Soc. 14, 1373–1377 (2017).
Hardinge, M. et al. British Thoracic Society guidelines for home oxygen use in adults. Thorax 70, i1–i43 (2015).
Douglas, W. W., Ryu, J. H. & Schroeder, D. R. Idiopathic pulmonary fibrosis: Impact of oxygen and colchicine, prednisone, or no therapy on survival. Am. J. Respir. Crit. Care Med. 161, 1172–1178 (2000).
Jacobs, S. S. et al. Home oxygen therapy for adults with chronic lung disease. An Official American Thoracic Society clinical practice guideline. Am. J. Respir. Crit. Care Med. 202, e121–e141 (2020).
Sharp, C., Adamali, H. & Millar, A. B. Ambulatory and short-burst oxygen for interstitial lung disease. Cochrane Database Syst. Rev. 7, CD011716 (2016).
Crockett, A. J., Cranston, J. M. & Antic, N. Domiciliary oxygen for interstitial lung disease. Cochrane Database Syst. Rev. 3, CD002883 (2001).
Visca, D. et al. Effect of ambulatory oxygen on quality of life for patients with fibrotic lung disease (AmbOx): A prospective, open-label, mixed-method, crossover randomised controlled trial. Lancet Respir. Med. 6, 759–770 (2018).
Khor, Y. H., Goh, N. S. L., McDonald, C. F. & Holland, A. E. Oxygen therapy for interstitial lung disease. A mismatch between patient expectations and experiences. Ann. Am. Thorac. Soc. 14, 888–95 (2017).
Nishiyama, O. et al. Effect of ambulatory oxygen on exertional dyspnea in IPF patients without resting hypoxemia. Respir. Med. 107, 1241–1246 (2013).
Jabbarian, L. J. et al. Advance care planning for patients with chronic respiratory diseases: A systematic review of preferences and practices. Thorax 73, 222–230 (2018).
Ley, B. et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann. Intern. Med. 156, 684–91 (2012).
Galiè, N. et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur. Heart J. 37, 67–119 (2016).
Matsuda, T. et al. COPD assessment test for measurement of health status in patients with idiopathic pulmonary fibrosis: A cross-sectional study. Respirology 22, 721–727 (2017).
Nagata, K. et al. Evaluation of the chronic obstructive pulmonary disease assessment test for measurement of health-related quality of life in patients with interstitial lung disease. Respirology 17, 506–512 (2012).
Huang, W. C., Wu, M. F., Chen, H. C., Hsu, J. Y., TOLD Group. Features of COPD patients by comparing CAT with mMRC: A retrospective, cross-sectional study. NPJ Prim. Care Respir. Med. 25, 15063 (2015).
Chailleux, E., Fauroux, B., Binet, F., Dautzenberg, B. & Polu, J. M. Predictors of survival in patients receiving domiciliary oxygen therapy or mechanical ventilation. A 10-year analysis of ANTADIR Observatory. Chest 109, 741–9 (1996).
Ahmadi, Z. et al. End-of-life care in oxygen-dependent ILD compared with lung cancer: a national population-based study. Thorax 71, 510–516 (2016).
Rantala, H. A., Leivo-Korpela, S., Lehtimäki, L. & Lehto, J. T. Predictors of impaired survival in subjects with long-term oxygen therapy. Respir. Care 64, 1401–1409 (2019).
Kishaba, T., Nagano, H., Nei, Y. & Yamashiro, S. Body mass index-percent forced vital capacity-respiratory hospitalization: New staging for idiopathic pulmonary fibrosis patients. J. Thorac. Dis. 8, 3596–3604 (2016).
Alakhras, M., Decker, P. A., Nadrous, H. F., Collazo-Clavell, M. & Ryu, J. H. Body mass index and mortality in patients with idiopathic pulmonary fibrosis. Chest 131, 1448–1453 (2007).
Nishiyama, O. et al. Fat-free mass index predicts survival in patients with idiopathic pulmonary fibrosis. Respirology 22, 480–485 (2017).
Jouneau, S. et al. Analysis of body mass index, weight loss and progression of idiopathic pulmonary fibrosis. Respir. Res. 21, 312 (2020).
Lettieri, C. J., Nathan, S. D., Barnett, S. D., Ahmad, S. & Shorr, A. F. Prevalence and outcomes of pulmonary arterial hypertension in advanced idiopathic pulmonary fibrosis. Chest 129, 746–752 (2006).
Bennett, D. et al. Mortality on the waiting list for lung transplantation in patients with idiopathic pulmonary fibrosis: A single-centre experience. Lung 193, 677–681 (2015).
Reed, A., Snell, G. I., McLean, C. & Williams, T. J. Outcomes of patients with interstitial lung disease referred for lung transplant assessment. Intern. Med. J. v36, v423-430 (2006).
Lama, V. N. et al. Prognostic value of desaturation during a 6-minute walk test in idiopathic interstitial pneumonia. Am. J. Respir. Crit. Care Med. 168, 1084–1090 (2003).
Vainshelboim, B., Kramer, M. R., Izhakian, S., Lima, R. M. & Oliveira, J. Physical activity and exertional desaturation are associated with mortality in idiopathic pulmonary fibrosis. J. Clin. Med. 18(5), 73 (2016).
Furukawa, T. et al. The St. George’s respiratory questionnaire as a prognostic factor in IPF. Respir. Res. 18, 18 (2017).
Case, A. H. et al. Associations between patient-reported outcomes and death or lung transplant in idiopathic pulmonary fibrosis. Data from the idiopathic pulmonary fibrosis prospective outcomes registry. Ann. Am. Thorac. Soc. 17, 699–705 (2020).
Kreuter, M. et al. Palliative care in interstitial lung disease: Living well. Lancet Respir. Med. 5, 968–980 (2017).
Acknowledgements
This study was partially supported by a grant to the Diffuse Lung Diseases Research Group from the Ministry of Health, Labour and Welfare, Japan.
Author information
Authors and Affiliations
Contributions
K.K., lead author, had full access to all of the data in the study and contributed to the study design, data collection and interpretation, and writing of manuscript. K.O., H.T., T.O., A.M., Y.I., S.A., S.H., T.K., K.S., N.H., K.K., M.N., M.E., N.E., Y.M., K.A., S.I., Y.T., H.I., H.O., and T.S. contributed to data collection and data organization. Y.K. corresponding author, contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript. All authors read and approved the last version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kataoka, K., Oda, K., Takizawa, H. et al. Cohort study to evaluate prognostic factors in idiopathic pulmonary fibrosis patients introduced to oxygen therapy. Sci Rep 13, 13664 (2023). https://doi.org/10.1038/s41598-023-40508-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40508-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.