Abstract
Metabolic syndrome (MetS) and obesity represent a public health problem worldwide. Bioelectrical impedance analysis (BIA) is a practical and effective way of evaluating body composition, especially abdominal fat. Liraglutide, a GLP-1 analog, reduces body weight and improves cardiometabolic parameters. In this prospective non-randomized intervention study, we evaluated the effect of 6 months of treatment with liraglutide (n = 57) on the clinical, laboratory and BIA findings of adult sex-stratified patients diagnosed with obesity and MetS, compared to a control group receiving sibutramine (n = 46). The groups were statistically similar with regard to the age of females (p = 0.852) and males (p = 0.657). Almost all anthropometric and BIA variables were higher in the treatment group than in the comparative group (p < 0.05). Abdominal circumference (AC) decreased significantly more in the treatment group. In males, body weight and fat mass also decreased (p < 0.05). Liraglutide treatment was associated with a greater reduction in trunk fat mass (FMT) (p < 0.05). AC and FMT were strongly correlated (rho = 0.531, p < 0.001) in the treatment group. In the multiple regression analysis, liraglutide treatment remained independently associated with FMT. Treatment with liraglutide for 6 months promoted weight loss, improved cardiometabolic and inflammatory parameters and led to a significant reduction in FMT correlated with AC in obese MetS patients of both sexes.
Similar content being viewed by others
Introduction
Obesity is a complex and multifactorial chronic disorder frequently refractory to treatment and prediposing towards the development of cardiometabolic conditions, such as cardiovascular disease (CD), type-II diabetes mellitus (DM-II), systemic arterial hypertension (SAH), metabolic syndrome (MetS) and other comorbidities1,2.
MetS, a systemic proinflammatory condition, involves a set of complex metabolic changes, such as insulin resistance, central obesity, SAH, hypertriglyceridemia and reduced HDL cholesterol levels. Due to its close association with CD and DM-II, MetS is considered a major public health problem worldwide3,4,5,6.
Liraglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist 97% similar to native GLP-17 secreted by intestinal L-cells at the level of the distal jejunum, ileum and colon in response to the ingestion of carbohydrates, lipids and mixed food8,9. It reduces blood sugar levels, inhibits glucagon secretion, increases insulin secretion, suppresses the appetite and calorie intake, retards gastric emptying, and enhances sensitivity to insulin10,11.
Due to its direct implication for the metabolism, body composition should be determined before initiating treatment of obesity12. This may be done in the clinical setting by bioelectrical impedance analysis (BIA), a safe and simple procedure which provides timely results based on the measurement of electrical resistance in different body tissues12.
Few studies13,14 have used BIA in patients diagnosed with obesity and MetS, and to our knowledge no previous study has evaluated the effect of liraglutide on BIA parameters in obese patients with MetS. Ozhan et al.13 investigated the diagnostic performance of BIA in MetS and validated the best cut-off in a large adult cohort. The authors found that visceral fat measured with BIA is a useful and easily applicable method for identifying patients with MetS, using as cut-off values > 12% for men and > 9% for women. Likewise, Jeon et al.14 determined whether visceral fat area (VFA) measured by BIA was associated with MetS in subjects with and without obesity and demonstrated that BIA combined with body mass index (BMI) may be a useful target in interventions to improve MetS.
In this study, we evaluated the effect of 6 months of treatment with liraglutide on the clinical, laboratory and BIA parameters of adult patients diagnosed with obesity and MetS, stratified by sex, compared to a control group receiving sibutramine.
Materials and methods
Study approval
This prospective non-randomized intervention study of patient records was conducted at a private clinic in Fortaleza (Northeastern Brazil) from December 2021 to January 2023. The study complied with the tenets of the Declaration of Helsinki15, all activities were conducted in accordance with the approved protocols and guidelines, and all patients gave their informed written consent prior to inclusion in the study protocol. Submitted through an online national research database (Plataforma Brasil), the study protocol was approved by the Research Ethics Committee of University of Fortaleza (Unifor) and filed under entry #64954722.7.0000.5052.
Patients and inclusion and exclusion criteria
The trial enrolled 103 patients of both sexes aged ≥ 21 years, with a BMI (BMI = body mass divided by the square of the body height) of 30 kg/m2 or higher and a diagnosis of MetS based on the “Harmonizing the Metabolic Syndrome” criteria (IDF/NHLBI/AHA/WHO/IAS/IASO) adjusted for South Americans16 and stratified by sex. Over a period of 6 months, 57 eligible patients received liraglutide at 3 mg/day s.c. (treatment group) and 46 eligible patients received sibutramine at 15 mg/day p.o. (control group). Patients were selected by convenience sampling and participants in both groups were aware of the medication received. All patients were submitted to physical examination, BIA and lab testing at baseline and at 6 months, stratified by sex.
Liraglutide is marketed under the trade name Saxenda by Novo Nordisk A/S (Bagsværd, Denmark) and Novo Nordisk Pharmaceutical Industries LP (Clayton, USA). Neither company was involved in this study, or supported it in any manner, or had access to the study data. The compound, a GLP-1 receptor agonist, reduces the appetite and, consequently, reduces food ingestion, promoting weight loss. The drug can cause nausea, vomiting, diarrhea, constipation, loss of appetite, dyspeptic symptoms, sensation of weakness, injection site reactions (hematoma, irritation, rash) and dizziness, among other effects17.
Sibutramine hydrochloride monohydrate is an anti-obesity drug which acts primarily through its active metabolites monodesmethyl (M1) and didesmethyl (M2) by effectively blocking the recapture of serotonin (5-hydroxytryptamine), norepinephrine and dopamine. The compound inhibits the appetite by promoting a sensation of satiety and diminishes weight loss-induced decline in energy expenditure18. The adverse effects include constipation, dry mouth and insomnia (up to 10% of cases), and palpitations, tachycardia, headache, increased blood pressure and sweating (less than 10% of cases). The brand Biomag was used in this study. The manufacturer (Achè Laboratórios Farmacêuticos S.A.) did not support this study in any manner and had no access to the study data.
The general exclusion criteria were age < 21 years, BMI < 30 kg/m2, MetS diagnosed by criteria other than the “Harmonizing the Metabolic Syndrome” criteria adjusted for South Americans16, patients with hypothyroidism, depression, use of antidepressants, obstructive sleep apnea, pregnancy and breastfeeding. Moreover, in the treatment group we also excluded patients with contraindications to liraglutide (history of hypersensitivity to the drug, age > 75 years, pancreatitis, multiple endocrine neoplasia, family history of medullary carcinoma of the thyroid). In the comparative group we excluded patients with contraindications to sibutramine (hypersensitivity to sibutramine, > 65 years of age, history of acute myocardial infarction, congestive heart failure, arrhythmia, peripheral arterial occlusive disease, treatment of psychiatric disorders, poorly controlled hypertension and/or previous cerebrovascular disease).
Study protocol
All patients were submitted to clinical and anthropometric evaluations, including abdominal circumference (AC), arterial pressure and lab tests, at baseline and after 6 months of protocol. Patients in the treatment group were instructed in the proper daily subcutaneous administration of liraglutide (preferably in the morning, in the abdomen or the upper inner arm) at an initial dose of 0.6 mg/day. The dose was raised by 0.6 mg at weekly intervals until reaching 3 mg/day (0.6 → 1.2 → 1.8 → 2.4 → 3 mg/day). The comparative group received sibutramine at 15 mg/day p.o. in the morning. Patients were monitored for pharmacological tolerance, including adverse effects like nausea, vomiting, diarrhea, constipation, loss of appetite, dyspepsia, sensation of weakness, injection site reactions (hematoma, irritation, rash), dizziness or palpitations, tachycardia, headache, and increased blood pressure. All patients were instructed to reduce their calorie ingestion and to perform 150–300 min of moderately intensive or 75–150 min of vigorous physical activity per week, or an equivalent combination thereof19.
Clinical, anthropometric and laboratory evaluations
During the clinical examination, a standardized questionnaire was administered to collect personal information on current health, food habits, physical activity, current and previous treatments, comorbidities, and family history of obesity, diabetes and SAH.
AC was measured with a tape positioned horizontally halfway between the iliac crest and the last rib. Height was measured using a digital stadiometer (HM-210 D, Ottoboni®).
Arterial pressure was measured with a previously calibrated sphygmomanometer, using a cuff compatible with the patient’s arm circumference (cuff size 12 × 23 for 25–34 cm; cuff size 16 × 32 for 35–45 cm). After resting for at least 5 min in a quiet room, arterial pressure was measured twice at a minimum interval of 2 min, as proposed by the 2018 ESH/ESC guidelines for the management of SAH20.
Body weight, segmental fat mass and segmental lean mass were quantified for all body segments (arms, legs, trunk) using an InBody 270 tetrapolar bioimpedance device21 manufactured in South Korea and licensed in Brazil by Anvisa under #80051870004. To do so, the patient was positioned on a scale (InBody 270), with electrodes attached to the hands and feet. The results were reported as percentage of body fat (BF%), lean mass, weight, body water and BMI. The test is painless and takes less than 5 min21.
The bioimpedance device features 8 contact points capable of collecting 10 measurements from each body segment (right arm, left arm, right leg, left leg, trunk) using 2 different frequencies (20 kHz and 100 kHz) and a current of 250 µA (Table 1)22. For the best results, patients were recommended to abstain from food and drink 2 h before the evaluation, void the bladder immediately before, not to practice physical activity or use the sauna on the day of the evaluation, and not to be menstruating. Evaluations were conducted at room temperature (20–25 °C).
Blood was collected after 12 h of fasting and 72 h of abstention from alcohol and heavy exercise. The lab parameters included fasting glycemia, insulin, glycated hemoglobin, HOMA-IR, total cholesterol, HDL, LDL, triglycerides, uric acid, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
ESR (mm/hr) was measured in whole blood using the automated Westergreen method. CRP (mg/dL) was measured in serum on nephelometry (Dade-Behring® BNII). Serum levels of glucose (mg/dL) were determined with the glucose-oxidase enzyme method, while serum levels of urea (mg/dL) were estimated with the UV-kinetic method. Using the kinetic method without deproteinization, we quantified serum creatinine (mg/dL), while enzymatic colorimetry was employed to determine the level of triglycerides (mg/dL), total cholesterol (mg/dL) and uric acid (mg/dL). To obtain the lipid profile (mg/dL), we submitted serum samples to calorimetry (Wiener®CMD 800i; Konelab®60i). Serum was also used for the estimation of high-density lipoprotein (HDL) (mg/dL) and low-density lipoproteine (LDL) (mg/dL) on calorimetry (calculated with the Fredwald formula CT = HDL + LDL + TG/5 whenever triglycerides were < 300 mg/dL). Finally, the insulin concentration in whole blood (µU/mL) was estimated on immunofluorometry and insulin resistence was defined by the HOMA-IR index of the top quartile of a non-diabetic population16.
Diagnosis of metabolic syndrome
MetS was classified according to the “Harmonizing the Metabolic Syndrome” statement (IDF/NHLBI/AHA/WHO/IAS/IASO)16, which requires the presence of 3 of the 5 criteria below:
-
Increase in AC using values adjusted for South Americans (≥ 90 for men; ≥ 80 for women)
-
TG ≥ 150 mg/dL, or receiving treatment
-
HDL ≤ 40 mg/dL for men and ≤ 50 mg/dL for women, or receiving treatment
-
Arterial pressure ≥ 130/ ≥ 85 mmHg, or use of antihypertensive medication
-
Fasting glycemia ≥ 100 mg/dL, or diagnosis of DM.
Statistical analysis
Categorical variables were expressed as absolute values and relative frequency (%). The chi-squared test was used to identify associations between categorical variables. The normality of distribution of the continuous variables was verified with the Kolmogorov–Smirnov test. Asymmetry was evaluated based on histograms and Q-Q graphs. Normal data were expressed as means ± standard deviation, while non-normal data were expressed as medians and interquartile range.
Pairwise comparisons of continuous variables of independent groups were made with Student’s t test (normal distribution) or the Mann–Whitney test (non-normal distribution). Pairwise comparisons of dependent groups were made with the paired t test (normal distribution) or the Wilcoxon test (non-normal distribution). Finally, quantitative variables were submitted to Spearman’s non-parametric correlation analysis (rho coefficient).
Furthermore, multiple linear regressions were conducted to verify the existence of independent associations between the study variables and reduction in FMT at 6 months (dependent variable), the most significant parameter in the univariate analysis. All parameters significant at the level of 10% (p < 0.10) in the univariate analysis were tested by multivariate analysis. Additionally, sex and age were included as independent variables. Collinearity between quantitative variables was assessed. All the variables selected for the multivariate model were included manually, and a backward stepwise method was used to identify the model which best explained the observed changes in the dependent variable.
All statistical analyses were performed with the software SPSS for Macintosh v. 23 (Armonk, NY: IBM Corp.). The level of statistical significance was set at 5% (p < 0.05).
Results
Our sample of MetS patients (n = 103) was segregated into a treatment group (n = 57, liraglutide 3 mg/day) and a comparative group (n = 46, sibutramine 15 mg/day). The groups were stratified according to sex: females accounted for 26 patients in the comparative group and 24 in the treament group, while males accounted for 20 patients in the comparative group and 33 in the treament group. The groups did not differ statistically with regard to female age (p = 0.852) and male age (p = 0.657). Almost all anthropometric variables were higher in the treatment group than in the comparative group (p < 0.05) regardless of the sex, with the exception of muscle mass (both sexes) and waist-to-hip ratio (males) (Table 2).
Likewise, at baseline all BIA variables in females were significantly higher in the treatment group than in the comparative group (p < 0.05). As for males, many of the BIA variables were statistically similar at baseline, such as lean mass in the right arm (LMA-R) (p = 0.152), lean mass in the left arm (LMA-L) (p = 0.170), lean mass trunk (LMT) (p = 0.228), lean mass in the right leg (LML-R) (p = 0.279) and lean mass in the left leg (LML-L) (p = 0.281).
Among laboratory variables, females treated with liraglutide had higher levels of HDL (p = 0.034) and CRP (p = 0.005) than females treated with sibutramine (Table 2).
Treatment with liraglutide at 3 mg/day for 6 months significantly improved all clinical and anthropometric variables (p < 0.05) and most BIA variables in both sexes. Females treated with liraglutide had a lower body fat percentage (FM%), LMA-R, LMA-L, fat mass in the right arm (FMA-R), fat mass in the left arm (FMA-L), fat mass in the trunk (FMT), fat mass in the right leg (FML-R) and fat mass in the left leg (FML-L) (p < 0.05). In males, the decreased variables included FM%, LMA-R, LMA-L, LML-R, LML-L, FMA-R, FMA-L, FMT, FML-R and FML-L (p < 0.05) (Table 3).
Likewise, most laboratory parameters improved in the treatment group, regardless of the sex, as did the inflammatory parameters ESR (p < 0.05) and CRP (p = 0.05) (Table 4).
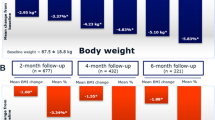
Subsequently, the two groups were compared with regard to changes in clinical, anthropometric, laboratory and BIA parameters, stratified by sex. Weight loss (5% and 10%) was similar in both sexes, but in women AC decreased significantly more in the treatment group than in the comparative group (− 11 [− 14.5; − 8.0] vs − 5 [− 7; − 4] cm, p < 0.001), while in men a decrease was observed in body weight (− 12.6 [− 17.5; − 10] vs − 9.8 [− 14.3; − 6.7] cm, p = 0.037), fat mass (− 10.9 [− 14.8; − 8.5] vs − 8.5 [− 11.1; − 5.45] cm, p = 0.010) and AC (− 14 [− 16; − 11] vs − 7 [− 11.2; − 4] cm, p < 0.001) (Table 5).
FMT in women decreased significantly more in the treatment group than in the comparative group (− 5.85 [− 9.7; − 4.2] vs − 3.15 [− 4.9; − 2.5] kg, p = 0.001). FMT also decreased in males (− 7.8 [− 9.4; − 6.5] vs − 3.85 [− 1.65; − 0.8] kg, p < 0.001), as did FMA-R (− 1.1 [− 1.5; − 0.7] vs − 0.7 [− 1.0; − 0.4] kg, p = 0.024) and FMA-L (− 1.0 [− 1.4; − 0.7] vs − 0.7 [− 1.0; − 0.4] kg, p = 0.049).
Since the reduction in AC and FMT was significantly greater in the treatment group than in the comparative group, we tested for a possible association between the two parameters and found a strong correlation (rho = 0.531; p < 0.001) in the treatment group (Fig. 1).
Finally, the multivariate approach revealed that treatment with liraglutide was independently associated with changes in FMT and BMI (Table 6).
Discussion
Liraglutide at a daily dose of 3 mg was associated with weight loss and considerably improved clinical and laboratory findings in obese MetS pacients of both sexes, confirming the findings of previous trials23,24. BIA parameters (especially FMT) were significantly reduced in our sample of patients stratified by sex, and were correlated with AC. In addition, body weight, fat mass and FMA decreased significantly in males.
The use of an age- and sex-matched comparative group allowed us to reliably establish whether the use of a GLP-1 analog can significantly modify the BIA parameters of obese MetS patients of both sexes. In addition, the overall clinical, laboratory, anthropometric and BIA findings allowed to establish the effect of liraglutide on the cardiometabolic profile with 6 months of follow-up in obese patients with MetS, stratified by sex.
Six months of liraglutide treatment led to reductions in SBP and DBP and in all anthropometric variables in both sexes, matching several other studies23,24,25,26,27,28,29. In support of our findings, a double-blind study involving 3731 patients reported weight loss and a reduction of glycemia and cardiometabolic risk factors after 52 weeks of treatment with liraglutide at 3 mg/day29, suggesting the compound can significantly reduce insulin resistance and glycemia and promote weight loss.
Among the laboratory variables, improvement was observed for fasting glycemia, glycated hemoglobin, insulin resistance, TC, triglycerides and inflammatory markers, indicating a better overall metabolic and inflammatory profile2,25,28,30. Importantly, our findings point to a significantly improved cardiometabolic and inflammatory profile after 6 months of treatment, whereas other studies have generally relied on longer follow-up periods (~ 1 year)28, suggesting the possibility of an earlier onset of the effects of liraglutide, including weight loss and glycemia reduction.
Interestingly, we observed a reduction in anthropometric and BIA variables after 6 months of liraglutide treatment. Moreover, the relationship appeared to be sex-specific (men: BW, FM, AC, FMT, FMA-R and FMA-L; women: AC and FMT). In addition to the well-estabished abdominal adiposity in MetS patients of both sexes, in males BIA arm parameters also seem to reflect response to liraglutide in the cardiometabolic profile. Thus, the assessment of body composition by BIA may be influenced by sex and the subject’s level of hydration and obesity13.
Visceral adipose tissue is now known to be a key component of MetS. AC is therefore an important parameter in the clinical stratification of cardiometabolic risk. However, a high AC value alone is not enough to adequately assess the accumulation of abdominal fat4,31, making it necessary to adopt more accurate methods of quantification, capable of monitoring treatment and preventing cardiac complications.
BIA has been validated for the assessment of body composition32,33,34. The method can evaluate FM in several body compartments and has been shown to perform quite well compared to more costly methods, such as computed tomography35. In this study, BIA was used to assess different body segments, showing truncal fat loss to be correlated with reductions in AC and abdominal fat loss. Interestingly, a Brazilian study evaluated the reliability of BIA and indirect calorimetry in the measurement of the resting metabolic rate of 40 women with MetS over a period of 6 months and concluded that, compared to indirect calorimetry, BIA is a practical and time-saving method which does not require prolonged fasting in order to produce reliable results36.
The observed reduction in AC and FMT in patients treated with liraglutide implies a reduction in visceral fat—the main cardiovascular risk factor in MetS4,31. This is supported by the fact that liraglutide treatment remained independently associated with the BIA parameter FMT in the multiple regression analysis, suggesting BIA is an adequate tool of abdominal fat assessment.
The limitations of this study included the short follow-up period (6 months) and the relatively small sample of patients. Also, we did not submit patients to nutritional assessment, and at baseline almost all the anthropometric variables were higher in the treatment group than in the comparative group, suggesting a possible sampling bias. Thus, since it was not possible to reliably establish the difference between treatment and control, we repeated the analysis segregating the patients by sex and ran multiple regressions to confirm the independent association between liraglutide treatment (independent variable) and the reduction in FMT after 6 months (dependent variable).
In conclusion, treatment with liraglutide at 3 mg/day for 6 months promoted weight loss, improved cardiometabolic and inflammatory parameters and led to a significant reduction in FMT correlated with AC in obese MetS patients of both sexes. Studies on larger samples and with longer follow-up periods are necessary to confirm and extrapolate our findings.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request. The data are not publicly available as they contain confidential information that may compromise the privacy/consent of the participants.
References
Garvey, W. T. New tools for weight-loss therapy enable a more robust medical model for obesity treatment: Rationale for a complications-centric approach. Endocr. Pract. 19, 864–874 (2013).
Mancini, M. C. & de Melo, M. E. The burden of obesity in the current world and the new treatments available: Focus on liraglutide 3.0 mg. Diabetol. Metabol. Syndr. 9, 44 (2017).
Neergaard, J. S. et al. Metabolic syndrome and subsequent risk of type 2 diabetes and cardiovascular disease in elderly women. Medicine. 95(36), e4806 (2016).
Després, J. P. et al. Abdominal obesity and the metabolic syndrome: Contribution to global cardiometabolic risk. Arterioscler. Thromb. Vasc. Biol. 28, 1039–1049 (2008).
Vidigal, F. C., Bressan, J., Babio, N. & Salas-Salvadó, J. Prevalence of metabolic syndrome in Brazilian adults: A systematic review. BMC Public Health 13, 1198 (2013).
Anxela, S. R. et al. Metabolic syndrome and visceral fat in women with cardiovascular risk factor. Nutr. Hosp. 34, 863–868 (2017).
Baggio, L. L. & Drucker, D. J. Biology of incretins: GLP-1 and GIP. Gastroenterology 132, 2131–2157 (2007).
Gutzwiller, J. P. et al. Glucagon-like peptide-1 promotes satiety and reduces food intake in patients with diabetes mellitus type 2. Am. J. Physiol. 276, R1541–R1544 (1999).
Keymann, A., Ghatei, M. A. & Williams, G. Glucagon like peptide-1 7–36: A physiological incretin in man. Lancet. 330, 1300–1304 (1987).
MacDonald, P. E. et al. The multiple actions of GLP-1 on the process of glucosestimulated insulin secretion. Diabetes 51, S434–S442 (2002).
Meeran, K. et al. Repeated intracerebroventricular administration of glucagon-like peptide-1-(7–36) amide or exendin-(9–39) alters body weight in the rat. Endocrinology 140, 244–250 (1999).
Jaffrin, M. Y. Body composition determination by bioimpedance: An update. Curr. Opin. Clin. Nutr. Metab. Care 12, 482–486 (2009).
Ozhan, H. et al. Performance of bioelectrical impedance analysis in the diagnosis of metabolic syndrome. J. Investig. Med. 60, 587–591 (2012).
Jeon, H. H. et al. Risk for metabolic syndrome in the population with visceral fat area measured by bioelectrical impedance analysis. Korean J. Intern. Med. 36, 97–105 (2021).
World Medical Association. Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 284, 3043–3045 (2000).
Alberti, K. G. M. M. et al. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International. Circulation 120, 1640–1645 (2009).
Novo Nordisk Inc. Saxenda® (Injeção de liraglutida [origem do DNAr]) Informações completas sobre prescrição. http://www.novo-pi.com/saxenda.pdf.
Luque, C. A. & Rey, J. A. Sibutramine: A serotonine-norepinephrine reuptake-inhibitor for the treatment of obesity. Ann. Pharmacother. 33, 968–978 (1999).
Bull, F. C. et al. World Health Organization 2020 guidelines on physical activity and sedentary behavior. Br. J. Sports Med. 54, 1451–1462 (2020).
Williams, B. et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens. 36, 1953–2041 (2018).
OTTOBONI. Aparelho de Bioimpedância modelo InBody270. Disponível em: https://ottoboni.com.br/produtos/inbody-270/.
Kyle, U. G. et al. Bioelectrical impedance analysis—Part I: Review of principles and methods. Clin. Nutr. 23, 1226–1243 (2004).
Park, J. S., Kwon, J., Choi, H. J. & Lee, C. Clinical effectiveness of liraglutide on weight loss in South Koreans: First real-world retrospective data on Saxenda in Asia. Medicine 100, e23780 (2021).
Astrup, A. et al. Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int. J. Obes. (Lond.). 36, 843–854 (2012).
Wadden, T. A. et al. Weight maintenance and additional weight loss with liraglutide after low caloric diet induced weight loss: The SCALE maintenance ranzomized study. Int. J. Obes. 37, 1443–1451 (2013).
Peradze, N. et al. Short-term treatment with high dose liraglutide improves lipid and lipoprotein profile and changes hormonal mediators of lipid metabolism in obese patients with no overt type 2 diabetes mellitus: A randomized, placebo-controlled, cross-over, double-blind clinical trial. Cardiovasc. Diabetol. 18, 1–12 (2018).
Wharton, S. et al. Real-world clinical effectiveness of liraglutide 3.0 mg for weight management in Canada. Obesity. 27, 917–924 (2019).
Chou, C. A. & Chuang, S. F. Evaluation of the efficacy of low-dose liraglutide in weight control among Taiwanese non-diabetes patients. J. Diabetes Investig. 11, 1524–1531 (2020).
Pi-Ssunier, X. et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N. Engl. J. Med. 373, 11–22 (2015).
Fujioka, K. et al. Early treatment with liraglutide 3.0 mg predicts weight loss at 1 year and is associated with improvements in clinical markers. Obesity (Silver Spring) 24, 2278–2288 (2016).
Bosello, O. & Vanzo, A. Obesity paradox and aging. Eat Weight Disord. 26, 27–35 (2021).
Lukaski, H. C. Applications of bioelectrical impedance analysis: A critical review. In In Vivo Studies of Body Composition (eds Yasumura, S. et al.) 365–374 (Springer, 1990).
Kyle, U. G. et al. Bioelectrical impedance analysis—Part II: Utilization in clinical practice. Clin. Nutr. 23, 1430–1453 (2004).
Lukaski, H. C., Bolonchuk, W. W., Hall, C. B. & Siders, W. A. Validation of tetrapolar bioelectrical impedance method to assess human body composition. J. Appl. Physiol 60, 1327–32 (1986).
Erickemberg, M., Oliveira, C. C., Roriz, A. K. L. C., Mello, A. L. & Sampaio, L. R. Bioelectrical impedance and visceral fat: A comparison with computed tomography in adults and elderly. Arq. Bras. Endocrinol. Metabol. 57, 27–32 (2013).
Bentes, C. M. et al. Rebiability of BIOIMPEDANCE and indirect calorimetry to evaluate resting metabolic rate in Brazilian women with metabolic syndrome. Diabetes Metab. Syndr. 15, 493–497 (2021).
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. I would like to thanks The Fundação Edson Queiroz for infrastructure and logistical support in the study.
Author information
Authors and Affiliations
Contributions
Conceptualization: F.P.C.F. and C.E.M.R. Analysis: F.P.C.F. and C.E.M.R. Writing/original draft: F.P.C.F. and C.E.M.R. Writing/review and editing: F.P.C.F. and C.E.M.R.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Freitas, F.P.C., Rodrigues, C.E.M. Effect of liraglutide on cardiometabolic profile and on bioelectrical impedance analysis in patients with obesity and metabolic syndrome. Sci Rep 13, 13090 (2023). https://doi.org/10.1038/s41598-023-40366-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40366-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.