Abstract
Current guidelines recommend that cytotoxic chemotherapy be considered first in non-small cell lung cancer (NSCLC) patients with multiple metastases, and whole-brain radiotherapy (WBRT) is not initially recommended even if brain metastases are present. However, cytotoxic chemotherapeutic agents are less effective in brain metastases due to poor blood–brain barrier permeability. We investigated the effect of WBRT in combination with cytotoxic chemotherapy on survival in NSCLC patients who were EGFR, ALK, and PD-L1 negative, had an ECOG PS of 2, and had multiple metastases including brain metastases. From January 2005 to December 2018, histologically confirmed NSCLC patients who were EGFR, ALK, and PD-L1 negative, had an ECOG PS of 2, and had multiple metastases including brain metastases were included in this study. Patients were classified into two groups based on receiving WBRT prior to or concurrently with administration of first-line chemotherapeutic agents or receiving chemotherapy only. We compared intracranial progression-free survival (iPFS) and overall survival (OS). Of the 240 NSCLC patients with brain metastases at diagnosis and an ECOG PS of 2, 67 patients were EGFR, ALK, and PD-L1 negative with multiple metastases including brain metastases. Among those patients, 43 (64.2%) received WBRT prior to or concurrently with platinum-based chemotherapy. Patients who received WBRT prior to or concurrently with chemotherapy had better iPFS (7.7 months [4.8–10.6] vs. 3.5 months [2.1–4.9], p = 0.009) and OS (10.8 months [5.9–15.7] vs. 6.1 months [1.9–10.3], p = 0.038) than those who did not receive WBRT. In multivariate analyses, WBRT was significantly associated with iPFS (HR: 1.94 and 95% CI 1.11–3.40, p = 0.020) and OS (HR: 1.92 and 95% CI 1.08–3.42, p = 0.027). In NSCLC patients who are EGFR, ALK, and PD-L1 negative, have an ECOG PS of 2, and have multiple metastases including brain metastases, WBRT prior to or concurrently with chemotherapy could improve iPFS and OS. Therefore, the combination of WBRT with cytotoxic chemotherapy should be considered in these patients.
Similar content being viewed by others
Introduction
Non-small cell lung cancer (NSCLC) with brain metastases is the most common central nervous system malignancy, accounting for as much as 20% of every brain metastasis case1. Patients with NSCLC with brain metastases often have a poor prognosis, with the median survival ranging between 4 and 6 months2. Whole-brain radiotherapy (WBRT) is often considered for patients in whom surgery or stereotactic radiosurgery is not recommended. However, it is unclear whether WBRT provides clinically significant benefits for NSCLC patients with brain metastases3. Therefore, current guidelines recommend that systemic chemotherapy be considered first in NSCLC patients with multiple metastases, and WBRT is not initially recommended, even if brain metastases are present4.
If tumors are negative for druggable molecular markers and are PD-L1 low (< 1%), systemic chemotherapeutic agents, including cytotoxic agents and immune checkpoint inhibitors (ICI), are considered rather than targeted agents. Specifically, only cytotoxic chemotherapeutic agents are recommended in patients with an Eastern Cooperative Oncology Group performance status (ECOG PS) of 2. However, unlike ICI, cytotoxic chemotherapeutic agents are less effective in brain metastases due to poor blood–brain barrier (BBB) permeability5. Approximately 30–50% of NSCLC patients are PD-L1 low, and half of those patients are epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) negative6,7. Therefore, given the considerable proportion of patients who are recommended to be treated with cytotoxic chemotherapeutic agents alone under the current guidelines, it is necessary to assess whether WBRT can provide a clinically significant benefit for patients with brain metastases.
In this study, we investigated the effect of WBRT in combination with cytotoxic chemotherapy on survival in NSCLC patients who were EGFR, ALK, and PD-L1 negative, had an ECOG PS of 2, and had multiple metastases including brain metastases.
Methods
Study population
A total of 240 patients with histologically confirmed NSCLC who were diagnosed between January 2005 and December 2018 at Inha University Hospital (Incheon, Republic of Korea) were initially considered for this study (Fig. 1). All patients had an ECOG PS of 2 and had brain metastasis at the time of diagnosis. Patients with metastatic lesions confined to the brain and a limited number of brain metastatic lesions (n = 59) were excluded. The limiting number of metastatic lesions was defined as five or less according to the NCCN guidelines4. Patients who did not receive cytotoxic chemotherapy (n = 65) were excluded. Among the remaining patients, those who were positive for EGFR, ALK, or PD-L1 (≥ 1%) (n = 49) were excluded. In total, 67 NSCLC patients who were EGFR, ALK, and PD-L1 negative, had an ECOG PS of 2, and had multiple metastases including brain metastases were included in this study.
Information such as age, gender, smoking history, histology, organs of metastasis, and chemotherapeutic agents were analyzed. The stage of all patients was estimated according to the eighth edition of the TNM classification system8. Volumes of all lesions were calculated using linear dimensions of the tumors (CC, LR, AP) obtained from pretreatment imaging tests. Considering the fact that brain metastases usually have a sphere-like shape, the formula for the volume of a spheroid: 4/3 × π × (CC/2) × (LR/2) × (AP/2) was used to simplify volume assessment9,10. All patients received platinum-based chemotherapy as the first line chemotherapeutic agent up to six cycles unless patients underwent disease progression or death. All information was collected prospectively from electronic medical records of the Lung Cancer Cohort of Inha University Hospital11. This study was approved by the Institutional Review Board of Inha University Hospital. The need for informed consent was waived by Institutional Review Board of Inha University Hospital (IRB number: 2021-07-032).
Brain radiotherapy and response evaluation
Patients were classified into two groups based on whether they received WBRT. WBRT was delivered prior to or concurrently with administration of first-line chemotherapeutic agents. For WBRT, three-dimensional conventional radiotherapy was done by a linear accelerator (RapidArc, Varian/Mevatron, Siemens). Patients were received WBRT dose of 30 Gy in 10 fractions using 4–6 MV X-ray. Each patient was treated in the supine position while wearing a head immobilization mask to ensure that daily positioning was reproducible. The ocular lens was shielded from the direct beam at all times using collimators. Hippocampal sparing was not applied. The planning target volume of WBRT was defined as the whole-brain parenchyma plus 5 mm margins as visualized on the simulator or portal films to account for beam penumbra and day-to-day set-up variation. A dosimetrist optimized the multileaf collimator shape used in the treatment based on the CT image in the treatment planning system of Eclipse.
Chest and abdomen computed tomography (CT), 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) or bone scan, and brain magnetic resonance imaging (MRI) were conducted using standard protocols at the time of diagnosis and approximately every 12 weeks thereafter. The response of intracranial lesions to chemotherapy with or without WBRT was evaluated by brain MRI that was included in the tests for the re-evaluation. In patients received WBRT, brain MRI for the first re-evaluation of intracranial lesion was performed about 1–2 months after completion of WBRT. Responses were evaluated using RECIST (Response Evaluation Criteria in Solid Tumors) 1.1 criteria12. The objective response rate (ORR) of intracranial lesions included the combination of complete response (CR) and partial response (PR), and the disease control rate (DCR) of intracranial lesions included CR, PR, and stable disease (SD).
Statistical analysis
To assess the association between WBRT and clinical variables, Pearson’s chi-square tests were conducted. Mann Whitney U-test was used to compared the number and volume of brain metastases between WBRT group and non-WBRT group. Overall survival (OS) was defined as the time from the start of chemotherapy to death. Intracranial progression-free survival (iPFS) was defined as the time from the start of chemotherapy to radiologically confirmed intracranial progression or death. The Kaplan–Meier method was adopted to estimate OS and iPFS, and survival curves were compared using log-rank tests. To assess the effect of WBRT, we performed univariate and multivariate analyses using the Cox proportional hazards model. Variables that had a value of p ≤ 0.1 in univariate analyses were included in a multivariate Cox proportional hazards model. Statistical significance was considered as two-sided p values ≤ 0.05. All statistical analyses were performed by using a statistical software package (SPSS, version 19.0).
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Inha University Hospital. The need for informed consent was waived by Institutional Review Board of Inha University Hospital (IRB number: 2021-07-032). All methods were performed in accordance with relevant guidelines and regulations.
Results
Patient characteristics
In total, 67 NSCLC patients who were EGFR, ALK, and PD-L1 negative, had an ECOG PS of 2, and had multiple metastases including brain metastases received a combination of platinum-based chemotherapy as first-line treatment. Among these patients, 43 patients received WBRT prior to or concurrently with administration of first-line chemotherapeutic agents. Of the 43 patients who underwent WBRT, 7 patients (16.3%) received WBRT concurrently with chemotherapy and 36 patients (83.7%) prior to chemotherapy. Table 1 summarizes the baseline characteristics of the study population. The median follow-up time was 7.4 months (range 0.7–69.6 months). The median age of the patients was 65 years (range 34–81 years). Patients in the WBRT group had a statistically significant higher number (median value and interquartile range [IQR], 4 and 1–10 in WBRT group vs. 1 and 1–4 in non-WBRT group, p = 0.014) and larger volume (median value and IQR, 2.3 and 0.3–8.4 in WBRT group vs. 0.2 and 0.1–0.7 in non-WBRT group, p < 0.001) of brain metastases than those in the non-WBRT group. Meanwhile, there was no significant difference in the proportion of patients with neurological symptoms13 between the two groups (25.6% in WBRT group vs. 12.5% in non-WBRT group, p = 0.207). Except for the number and volume of brain metastases, no statistically significant differences were found in the baseline characteristics between the two groups.
Intracranial treatment response
Intracranial responses could be evaluated by brain MRI in 55 patients (82.1%). In the other patients (n = 12), follow-up of intracranial lesions by brain MRI was not performed due to their short OS. Among the 37 patients in the WBRT group, assessment of intracranial lesions indicated that 1 patient (2.7%) had CR, 22 patients (59.5%) had PR, 11 patients (29.7%) had SD, and 3 patients (8.1%) had progressive disease (PD). Whereas 1 patient (5.6%) had PR, 10 patients (55.6%) had SD, and 7 patients (38.9%) had PD among the 18 patients in the non-WBRT group. In the non-WBRT group, 6 of 7 patients with intracranial PD received WBRT after confirmation of intracranial PD. Intracranial ORR was 62.2% for the WBRT group and only 5.6% for the non-WBRT group (p < 0.001). Intracranial DCR was 91.9% for the WBRT group and 61.1% for the non-WBRT group (p = 0.005).
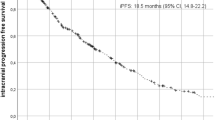
Survival following whole-brain radiotherapy
The median iPFS and OS times were 6.8 months (95% CI 5.1–8.5 months) and 8.2 months (95% CI 6.0–10.4 months). Patients who received WBRT prior to or concurrently with chemotherapy had better iPFS (7.7 months [4.8–10.6] vs. 3.5 months [2.1–4.9], p = 0.009) and OS (10.8 months [5.9–15.7] vs. 6.1 months [1.9–10.3], p = 0.038) than those who did not receive WBRT (Fig. 2). In multivariate analyses, WBRT was significantly associated with iPFS (HR: 1.94 and 95% CI 1.11–3.40, p = 0.020) and OS (HR: 1.92 and 95% CI 1.08–3.42, p = 0.027) (Table 2).
A representative case
A representative case with brain metastases that showed disease progression after receiving only chemotherapy without WBRT is highlighted in Fig. 3. A 75-year-old man was diagnosed with stage IV lung adenocarcinoma with metastasis in the right iliac bone and multiple metastases in the brain. The patient complained of right hemiplegia after 2 cycles of platinum-based chemotherapy. As indicated by imaging examination, the primary tumor decreased in size, and the metastatic lesion in the right iliac bone did not change; however, the metastatic lesions in the brain increased in size and new metastatic lesions developed. The patient died 4 months after lung cancer diagnosis due to rapid deterioration of general health conditions associated with aggravated neurologic symptoms.
A typical case with brain metastases that showed disease progression after receiving only chemotherapy without whole-brain radiotherapy. Compared to the time of lung cancer diagnosis (A), the size of the primary tumor decreased and that of the metastatic lesion in the right iliac bone did not change after two cycles of platinum-based chemotherapy (B). However, the size of metastatic lesions in the brain increased and new metastatic lesions developed.
Discussion
In this study, patients who received WBRT prior to or concurrently with chemotherapy had improved intracranial ORR and intracranial DCR compared to those who did not receive WBRT. In addition, the WBRT group had better iPFS and OS than the non-WBRT group. These results suggest that combining WBRT with cytotoxic chemotherapy could be beneficial for survival in NSCLC patients who are EGFR, ALK, and PD-L1 negative, have an ECOG PS of 2, and have multiple metastases including brain metastases. Patients in the WBRT group showed better iPFS and OS than the those in the non-WBRT group despite the higher number and larger volume of brain metastases at diagnosis. Also, unlike a previous study14, the volume of brain metastases was not significantly associated to iPFS and OS. We suggest that it might be associated to the strong impact of WBRT on survival.
The QUARTZ trial showed that WBRT with supportive care does not significantly affect OS compared to supportive care only3. This finding is contrary to the results of our study in that WBRT provided a significant OS benefit. However, in the QUARTZ trial, patients did not receive systemic chemotherapy, so a significant proportion of patients did not live long enough to experience the effects of WBRT unlike in this study; the maximum benefit of WBRT is achieved approximately 6 weeks after the end of treatment15.
The BBB is an obstacle for effective chemotherapies for brain metastases, thus suggesting that brain radiotherapy will continue to play a role in the management of brain metastases16. Furthermore, previous studies have provided evidence that brain radiotherapy disrupts the BBB, allowing chemotherapeutic agents to better reach brain metastases17,18. These findings are supported by our results in that WBRT prior to or concurrently with chemotherapy provides survival benefits.
In previous studies, patients with poor performance, such as those with Karnofsky Performance Scores (KPS) < 70 or ECOG PS ≥ 2, showed no benefit from WBRT3,19,20. Although a significant number of patients were included in the PS = 2 group of the previous studies, the survival benefit of WBRT in patients with PS = 2 was not determined as the patients with PS = 2 were grouped with patients with PS 3 or 421,22. In this study, we considered the clinical significance of patients with PS = 2, and only patients with PS = 2 were included in this study. The significant benefit of WBRT plus cytotoxic chemotherapy was demonstrated in the PS = 2 group.
There are limitations of this study. First, this study was conducted at a single center and external confirmatory studies should be conducted in the future. However, all clinical information was obtained prospectively from the Inha Lung Cancer Cohort. Second, although it is important to consider the quality of life and the toxicity of treatment, these considerations could not be investigated in this study23. Considering that not only WBRT but also chemotherapy can affect cognitive function24,25, it is necessary to investigate changes in cognitive function before and after treatment in the WBRT with chemotherapy group and chemotherapy alone group in the future. Third, because of the small number of patients, it was difficult to conduct a subgroup analysis such as dividing into patients received WBRT concurrently with chemotherapy and those received WBRT prior to with chemotherapy. We believe that a study with a larger number of patients is needed in the future.
Conclusions
WBRT prior to or concurrently with chemotherapy improved iPFS and OS in NSCLC patients who were EGFR, ALK, and PD-L1 negative, had an ECOG PS of 2, and had multiple metastases including brain metastases. Therefore, we suggest that the combination of WBRT with cytotoxic chemotherapy should be considered in these patients. The combination of WBRT with cytotoxic chemotherapy should be carefully individualized for each patient with consideration of each patient’s situation, such as characteristics of metastatic lesions and general health conditions.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- WBRT:
-
Whole-brain radiotherapy
- ECOG PS:
-
Eastern Cooperative Oncology Group performance status
- BBB:
-
Blood–brain barrier
- EGFR:
-
Epidermal growth factor receptor
- ALK:
-
Anaplastic lymphoma kinase
- CT:
-
Computed tomography
- FDG-PET/CT:
-
18F-fluorodeoxyglucose positron emission tomography/computed tomography
- MRI:
-
Magnetic resonance imaging
- RECIST:
-
Response evaluation criteria in solid tumors
- ORR:
-
Objective response rate
- CR:
-
Complete response
- PR:
-
Partial response
- DCR:
-
Disease control rate
- SD:
-
Stable disease
- PD:
-
Progressive disease
- OS:
-
Overall survival
- iPFS:
-
Intracranial progression-free survival
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
References
Barnholtz-Sloan, J. S. et al. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J. Clin. Oncol. 22, 2865–2872 (2004).
Mehta, M. P. et al. Survival and neurologic outcomes in a randomized trial of motexafin gadolinium and whole-brain radiation therapy in brain metastases. J. Clin. Oncol. 21, 2529–2536 (2003).
Mulvenna, P. et al. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): Results from a phase 3, non-inferiority, randomised trial. Lancet 388, 2004–2014 (2016).
Network NCC. NCCN Non-Small Cell Lung Cancer Guidelines, Version 3.2023. April 13, 2023.
Gerstner, E. R. & Fine, R. L. Increased permeability of the blood–brain barrier to chemotherapy in metastatic brain tumors: Establishing a treatment paradigm. J. Clin. Oncol. 25, 2306–2312 (2007).
Aggarwal, C. et al. Prevalence of PD-L1 expression in patients with non-small cell lung cancer screened for enrollment in KEYNOTE-001,-010, and-024. Ann. Oncol. 27, vi363 (2016).
Dietel, M. et al. Real-world prevalence of programmed death ligand 1 expression in locally advanced or metastatic non-small-cell lung cancer: The global, multicenter EXPRESS study. Lung Cancer 134, 174–179 (2019).
Goldstraw, P. et al. The IASLC lung cancer staging project: Proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J. Thorac. Oncol. 11, 39–51 (2016).
Feldman, J. P., Goldwasser, R., Mark, S., Schwartz, J. & Orion, I. A mathematical model for tumor volume evaluation using two-dimensions. J. Appl. Quant. Methods 4, 455–462 (2009).
Mayr, N. A. et al. Method and timing of tumor volume measurement for outcome prediction in cervical cancer using magnetic resonance imaging. Int. J. Radiat. Oncol. Biol. Phys. 52, 14–22 (2002).
Ryu, J.-S. et al. Prognostic impact of minimal pleural effusion in non-small-cell lung cancer. J. Clin. Oncol. 32, 960–967 (2014).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247 (2009).
Patchell, R. A. The management of brain metastases. Cancer Treat. Rev. 29, 533–540 (2003).
Baschnagel, A. M. et al. Tumor volume as a predictor of survival and local control in patients with brain metastases treated with Gamma Knife surgery. J. Neurosurg. 119, 1139–1144 (2013).
Le Pechoux, C., Dhermain, F. & Besse, B. Whole brain radiotherapy in patients with NSCLC and brain metastases. Lancet 388, 1960–1962 (2016).
Suh, J. H. et al. Current approaches to the management of brain metastases. Nat. Rev. Clin. Oncol. 17, 279–299 (2020).
van Vulpen, M., Kal, H. B., Taphoorn, M. J. & El Sharouni, S. Y. Changes in blood–brain barrier permeability induced by radiotherapy: Implications for timing of chemotherapy?. Oncol. Rep. 9, 683–688 (2002).
Blethen, K. E. et al. Modulation of the blood-tumor barrier to enhance drug delivery and efficacy for brain metastases. Neuro-Oncol. Adv. 3, v133–v143 (2021).
Buecker, R. et al. Risk factors to identify patients who may not benefit from whole brain irradiation for brain metastases—a single institution analysis. Radiat. Oncol. 14, 1–6 (2019).
Miyazawa, K. et al. Predicting prognosis of short survival time after palliative whole-brain radiotherapy. J. Radiat. Res. 59, 43–49 (2018).
Kawaguchi, T. et al. Performance status and smoking status are independent favorable prognostic factors for survival in non-small cell lung cancer: A comprehensive analysis of 26,957 patients with NSCLC. J. Thorac. Oncol. 5, 620–630 (2010).
Sehgal, K. et al. Association of performance status with survival in patients with advanced non-small cell lung cancer treated with pembrolizumab monotherapy. JAMA Netw. Open 4, e2037120–e2037120 (2021).
Tallet, A. V. et al. Neurocognitive function impairment after whole brain radiotherapy for brain metastases: Actual assessment. Radiat. Oncol. 7, 1–8 (2012).
Andres, A. L., Gong, X., Di, K. & Bota, D. A. Low-doses of cisplatin injure hippocampal synapses: A mechanism for ‘chemo’brain?. Exp. Neurol. 255, 137–144 (2014).
Kovalchuk, A. & Kolb, B. Chemo brain: From discerning mechanisms to lifting the brain fog—an aging connection. Cell Cycle 16, 1345–1349 (2017).
Funding
This work was supported by an Inha University Research Grant.
Author information
Authors and Affiliations
Contributions
Conceptualization: J.-S.R., J.H.L. Data curation: W.K.R., H.K.C., J.-S.R., J.H.L. Formal analysis: W.K.R., H.K.C., J.-S.R., J.H.L. Investigation: W.K.R., H.K.C., W.K., H.Y.L., H.-J.K., J.-S.R., J.H.L. Methodology: W.K.R., H.K.C., J.-S.R., J.H.L. Project administration: J.-S.R., J.H.L. Supervision: J.-S.R., J.H.L. Validation: W.K.R., H.K.C., J.-S.R., J.H.L. Writing—original draft: W.K.R., H.K.C., W.K., H.Y.L., H.-J.K., J.-S.R., J.H.L. Writing—review and editing: W.K.R., H.K.C., W.K., H.Y.L., H-J.K., J.-S.R., J.H.L.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ryu, W.K., Cha, H.K., Kim, W. et al. Effect of whole-brain radiotherapy with platinum-based chemotherapy in non-small cell lung cancer patients with multiple metastases including brain metastases. Sci Rep 13, 13173 (2023). https://doi.org/10.1038/s41598-023-40235-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40235-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.