Abstract
Medial meniscus extrusion (MME) is exacerbated by repeated mechanical stress. Various factors would affect MME; however, there is limited information about the behaviour of the medial meniscus during walking in patients with knee osteoarthritis (KOA). This study aimed to investigate the pattern of MME during walking and its association with limb biomechanics in patients with KOA. Fifty-five patients with KOA and ten older adult volunteers as a control group were involved in this study. The MME and limb biomechanics during walking were evaluated simultaneously by ultrasound and a motion analysis system, respectively. The waveform was constructed from the values of MME, and the point showing the highest value of MME was identified during the gait cycle. According to the peak timing of MME in the waveform, the pattern of the waveform was evaluated and compared to the control group. Lateral thrust, knee adduction moment (KAM), and flexion moment were obtained from motion analysis, and their association with the MME was evaluated. The patients with KOA demonstrated unique peak timing during walking. Compared to the control group, there were three groups of MME waveforms, early (< 59%), normal (60–83%), and late (> 84%) from the peak timing in the gait cycle. The pattern of MME waveform in early, normal, and late groups was correlated with the first KAM and lateral thrust, second KAM, and knee flexion moment, respectively. A unique MME pattern during walking was demonstrated, and these patterns were associated with limb biomechanics in patients with KOA.
Similar content being viewed by others
Introduction
The menisci function as shock absorbers and distribute the mechanical stress of the knee as a hoop function1. However, medial meniscus extrusion (MME) shows meniscal dysfunction and gradually expands2,3,4. The greater MME is associated with the accelerated progression of knee osteoarthritis (KOA) and severe knee pain, leading to poor quality of life5,6,7. Moreover, the greater MME is also a risk factor for a poor clinical score for postoperative patients8,9. The minimisation of MME with appropriate management is required to prevent KOA progression at all stages.
The MME temporarily increases in a weight-bearing situation when compared with non-weight-bearing10,11. It gradually expands by repetitive mechanical stress during daily activities2,3,4. This increase in MME results in unique behaviour during walking, especially as severe extrusion occurs in the late stance phase on the gait cycle, which is associated with limb mechanical stress12,13. However, the lateral thrust and knee adduction moment (KAM) cause repetitive mechanical stress on the medial compartment14,15,16. The association between these mechanical stresses and the behaviour of MME during the gait cycle has not been elucidated yet.
This study aimed to investigate the pattern of meniscal behaviour during walking and its association with limb biomechanics in patients with KOA.
Material and methods
Participants
Ethics Committee of epidemiology of Hiroshima University approved this study (Approval Number: E449-4). This study is in accordance with the principles of the Declaration of Helsinki. All participants gave their informed consent.
From April 2021 to May 2023, 70 patients with KOA and ten healthy older volunteers (control group) participated in this cross-sectional study (mean age, KOA: 62.5 ± 10.6 years, males, n: 35; control: 61.4 ± 8.0 years, males, n: 6), and they were all able to walk smoothly. The patient with KOA in the medial compartment was diagnosed radiographically. The severity of KOA was evaluated with Kellgren–Lawrence (K/L) score using the Rosenberg view. Their knee alignment was evaluated by the hip-knee-ankle angle (HKAA) on the images of the full lower limb. The inclusion criteria were (1): HKAA < 0°, (2): Knee pain and tenderness in the medial joint space, and (3): Awareness of knee pain during activities of daily living, especially loading tasks.
If participants had the following, (1): Pain and tenderness in the lateral compartment, (2): A history of trauma, (3): A neurological disorder, (4): A need for any support due to severe knee pain, which affected the gait form, they were excluded. The final KOA group comprised 55 knees in 55 patients (Table 1).
Gait analyses
The kinematic data were obtained from a three-dimensional motion analysis system (VICON612; Vicon Motion Systems, Oxford, UK) with sixteen cameras (Vicon Motion Systems) at 100 Hz. Moreover, eight force platforms (AMTI, Watertown, Mass) at 1000 Hz were synchronised with the motion analysis system and obtained the kinematical data. In the process, the cameras were calibrated, and passive reflex makers were attached to the participant's lower leg according to the model of the Plug-in-Gait Marker (Plug-in-Gait, Vicon® Peak; Vicon Motion Systems). The participants walked 5 m on a straight course at a comfortable speed. The gait cycle was identified as the heel contact and toe-off using the threshold of vertical ground reaction force 10N and determining the stance phase in the walking cycle as being from heel contact to toe-off. The stance phase's kinetics, kinematic and spatiotemporal data were analysed by the Vicon Nexus (Vicon® Peak; Vicon Motion Systems). The Lateral thrust was calculated as the difference in knee angle between the varus and valgus occurring in the early stance phase of the gait cycle17.
Dynamics of the meniscus and its behaviour of MME during walking
The dynamic meniscus extrusion was obtained by ultrasonography (SNiBLE, KONICA MINOLTA, Japan) and a prototype 3–11 MHz specific liner transducer. The procedure is described in previous studies12,18. Briefly, the longitudinal transducer was placed on the medial joint space where the medial collateral ligament and the triangle meniscus can be seen on the ultrasound images (Fig. 1). Secondly, the transducer was fixed using a flexible band which adapts to knee flexion during walking and allows for natural walking. The participants were asked to walk the 5 m at a comfortable speed. The meniscus movement during walking was recorded using the video mode on the ultrasound with 30 Hz. The external devices recorded the stimulation and synchronised it with the motion analysis system.
The medial meniscus was identified as “The distance from the cortex of the medial tibial plateau to the remotest point of the medial meniscus” based on a previous study19, and the value of MME was calculated using Kinovea software (v0.8.15; Kinovea open source project, www.kinovea.org) (Fig. 1). The ΔMME was calculated as the difference in MME between the maximum and minimum. These processes have been demonstrated to be highly reliable in a previous study12. They continued until around 20 images were obtained, the value of MME in the stance phase of the gait cycle was calculated, and a waveform of MME was made. To compare the different raw data sets on a single stance phase, all data were standardised and time-normalised to the 101 points data (Fig. 2). The behaviour timing was also calculated as the maximum MME in a single stance. Lastly, these processes were repeated three times and the averages were used for statistical analysis.
The ultrasound images and the waveform of meniscus extrusion in the gait cycle. These are four representative images of 20, including the extruded meniscus during walking (A). The constructed waveform from the serial value of meniscus extrusion on 20 images. The stance phase was standardised and time-normalized to the 101 points data (B). The arrow line shows the amount of change in meniscus extrusion (∆MME).
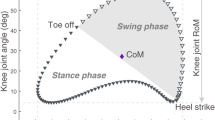
Categorisation of the pattern of meniscal behaviour
According to the range of the behaviour timing in the control group, the KOA patients were divided into three groups, (1) the normal group, which was similar to the control (2) the early group that showed extrusion earlier than the controls, and (3) the late group that demonstrated a later peak time (Fig. 3).
Three patterns of waveforms based on the dynamics of MME and its peak timing. Individual waveforms show the representative patterns of the dynamic meniscus as control (A), early (B), normal (C), and late (D) groups. The peak timings in each group are indicated by an arrow based on the maximum extruded meniscus in the stance phase (E). The distribution of peak timing in each patient from control, early, normal and late groups.
Evaluation of the type of meniscal tear
The meniscus quality was evaluated by magnetic resonance images (MRI), obtained within three months of the first consultation. Two orthopaedic surgeons (M.I. and G.K), each with over ten years of experience, performed the assessments. The type of meniscus tear was identified by the globular or linear signal abnormality within the meniscus that extended to the surface on more than two consecutive images based on previous studies20,21,22,23 and is then divided into horizontal, longitudinal, radial, complex, and degenerative tears. The meniscus tear on the posterior horn of the root was categorised as a medial meniscus posterior root tear (MMPRT) and exhibited the specific radiological signs; the ghost sign or giraffe neck sign24,25.
Statistical analysis
To compare the groups, the demographic data, MME, and ΔMME were analysed using the Wilcoxon signed-rank test. The demographic data, MME, ΔMME, and biomechanical data within the groups were compared using a one-way analysis of variance or the Kruskal–Wallis test. The correlation between ΔMME and biomechanical data was performed by the Pearson or Spearman correlation method. The presence of MMPRT analysed using Chi-squared test and the multiple comparison was demonstrated in each group. These statistical analyses were performed using SPSS (v23, IBM, USA). A P-value of < 0.05 was considered significant.
Results
Demographic data and meniscus quality
The BMI in KOA was higher than that in the control group (p < 0.01). Other parameters were not significantly different between groups (Table 1).
Comparison with the MME and behaviour of timing, and categorised to group
In KOA, the minimum and maximum MME and ΔMME were significantly greater than those in the control group. (ΔMME, KOA: 1.5 ± 0.6 mm, control: 1.0 ± 0.1 mm; p < 0.01). The behaviour timing in KOA patients varied compared to that in the control group (KOA: 69.4 ± 19.2% range: 18–99%, control: 71.3 ± 6.6%, range: 60–83%).
The KOA patients were comprised of 14 patients in the early (25%), 25 in the normal (45%), and 16 in the late group (29%) according to the behaviour timing in the control group (Behavior timing: early: < 59%, normal: 60–83% and late: > 84%) (Fig. 3E). The average behaviour timing in maximum MME was 41.8 ± 13.3%, 72.6 ± 5.1%, and 88.4 ± 4.7% in the early, normal, and late groups, respectively.
The KOA patients had varus alignment, and almost all patients had mild to moderate disease (HKAA: -5.2 ± 3.3°) (KL I: 6, II: 28, III: 19, IV: 2). In the group, the diseased knee and knee alignment are shown in Table 2. The HKAA in the early group was lower than that in the late group. The maximum MME in the early group was higher than in the late group. However, other parameters did not differ significantly among the groups. These data are summarised in Table 2.
The comparison with gait parameters and biomechanical data
The gait speeds were 0.8 ± 0.1 m/s, 0.9 ± 0.2 m/s and 0.9 ± 0.1 m/s in the early, normal and late groups, respectively. The gait parameters did not differ among the groups, including gait speed, the first peak angle of flexion and varus, and moments during gait (Table 3).
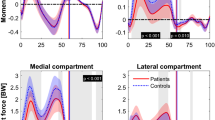
The correlation between meniscal behaviour and biomechanical factors
In the KOA patients, the second KAM tended to correlate positively with ΔMME, but there was no significant correlation (r = 0.21, p = 0.124).
In the early group, the ΔMME was significantly correlated with lateral thrust, first KAM and its impulse. Moreover, the ΔMME was significantly correlated with the second KAM in the normal group, and there were significant correlations with flexion moment and its impulse in the late group (Table 4).
The evaluation of the meniscus quality
The most frequent meniscus pathology included the degenerative tear (42%) in patients with KOA, and a medial meniscus posterior root tear (MMPRT) was found in 17 patients (31%). In the groups, the rate of MMPRT was 12%, 36%, and 56% in the normal, early, and late groups. The presence with and without MMPRT was significantly difference in only normal and late group (p < 0.05). However, there was not difference among groups for other rate of meniscus type (Table 5).
Discussion
Our findings show that patients with KOA have various meniscal behaviour patterns individually associated with limb biomechanics.
Meniscus extrusion is a risk factor for the progression of KOA, knee pain, and poor postoperative clinical outcome6,7,8,9. The increase in extrusion is believed to be due to the greater ΔMME being affected by abnormal mechanical stress. However, each individual with KOA has complex pathology, and the appropriate approach must be based on the knee pathology26. The behaviour of the medial meniscus is shown as an effect of mechanical stress and the key factor associated with the mechano-pathology of KOA progression12,18. Our findings indicated that the pattern of meniscal behaviour varied during walking, and the groups differed regarding the incidence of MMPRT. Moreover, the biomechanical factors associated with the ΔMME changed according to the severity of the posterior portion of the medial meniscus pathology. Thus, it is important to evaluate the mechano-pathology of KOA, emphasising the pattern of meniscal behaviour. Therefore, our findings provide insight into the mechanisms of ΔMME by mechanical stress in individuals with KOA with meniscal pathology of posterior segment and lead to developing the appropriate approach for KOA patients.
In patients with KOA, a variation in behaviour timing of MME was confirmed compared with the control group. Furthermore, the change in extrusion (ΔMME) showed no significant correlation with mechanical stresses. On the other hand, in three groups consisting of subjects with different behaviour timing, the first KAM and lateral thrust in the early group, the second KAM in the normal group, and flexion moment in the late group were significantly correlated with the ΔMME. Thus, these results might show that KOA results in variable behaviour from MME with specific biomechanical stresses. A previous study showed that only the second KAM was correlated with the ΔMME; however, this data came from a small sample and presumably did not investigate the variety of MME patterns in subjects12. To date, the lateral thrust and first KAM are known as the major mechanical stresses on the medial compartment and are known to cause the progression of KOA14,16,27,28. The knee flexion moment is a mechanical stress on the anterior compartment of the knee29. However, a previous study has reported the effect of the combination of KAM and KFM on the prediction of medial contact force and showed a high predictive value when compared with only KAM30. Moreover, the occurring the injury pattern of traumatic MMPRT was investigated and occupied the motion with low knee flexion under loading conditions such as walking and descending actions as the major event31. These facts might support that the late group showed the association between ∆MME and KFM and the highest incidence of MMPRT. Thus, these previous studies indicate that KOA patients have complex mechanical pathology, which may explain the plausible relevance of mechanical loading according to the meniscus dynamics in this study.
The meniscal hoop function requires the fixed attachment of the posterior root segment32. However, these often show pathological changes such as stretch and tear on the posterior segment of the medial meniscus, leading to loss of the hoop function33,34. Our findings demonstrate the incidence of MMPRT was higher in the late and early groups than in the normal group. Moreover, these groups were divided based on the dynamics of the meniscus. Thus, the difference in meniscus dynamics waveform might be reflected in the progressive pathological condition of the posterior section of the meniscus. Typically, the meniscal movement during knee flexion translates not only to the posterior but also within the joint on the tibial plate, whereas the MMPRT shows destruction of the general translation35,36,37,38. Walking includes the two flexion points in a single gait cycle's early and late phases in the stance phase. The waveform in the normal group was in line with this movement, which occurs in the middle-to-late phase, excluding the early and late phases. On the other hand, early and late groups were unmatched with normal meniscal movement. Therefore, these results and previous studies might explain the correlation between the dynamics of the meniscus and the absence of hoop function associated with meniscal attachment.
This study has some limitations. First, the study was cross-sectional, so our finding cannot determine whether the biomechanical factor occurs because of the ΔMME. Secondly, the sample size was small, so we cannot compare with bias the K/L stage and knee alignments in the groups. Third, the MMPRT was evaluated only with the MRI images. However, MMPRT has several types with partial or complete tears. Therefore, future studies are needed to add the MMPRT arthroscopy information and assess the correlation between matched K/L and knee alignment in a cohort study.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Aagaard, H. et al. Function of the normal meniscus and consequences of meniscal resection. Scand. J. Med. Sci. Sports. 9, 134–140 (1999).
Furumatsu, T. et al. Medial meniscus extrusion correlates with disease duration of the sudden symptomatic medial meniscus posterior root tear. Orthop. Traumatol. Surg. Res. 103, 1179–1182 (2017).
Furumatsu, T. et al. Meniscal extrusion progresses shortly after the medial meniscus posterior root tear. Knee Surg. Relat. Res. 29, 295–301 (2017).
Ishii, Y. et al. The correlation between osteoarthritis stage and the effect of the lateral wedge insole for 3 months on medial meniscus extrusion in the knee joint. Knee 28, 110–116 (2020).
Berthiaume, M.-J. et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann. Rheum. Dis. 64, 556–563 (2005).
Murakami, T. et al. Useful ultrasonographic evaluation of the medial meniscus as a feature predicting the onset of radiographic knee osteoarthritis. J. Orthop. Sci. 22, 318–324 (2017).
Ishii, Y. et al. Association between medial meniscus extrusion under weight-bearing conditions and pain in early-stage knee osteoarthritis. J. Med. Ultrason. 2001(48), 631–638 (2021).
Xu, T. et al. Large medial meniscus extrusion and varus are poor prognostic factors of arthroscopic partial meniscectomy for degenerative medial meniscus lesions. J. Orthop. Surg. 17, 170 (2022).
Yang, H.-Y. et al. Extent of preoperative medial meniscal extrusion influences intermediate-term outcomes after medial opening-wedge high tibial osteotomy. J. Bone Joint Surg. Am. 104, 316–325 (2022).
Ko, C.-H. et al. H.-L. Sonographic imaging of meniscal subluxation in patients with radiographic knee osteoarthritis. J. Formos. Med. Assoc. Taiwan Yi Zhi 106, 700–707 (2007).
Paparo, F. et al. Extrusion of the medial meniscus in knee osteoarthritis assessed with a rotating clino-orthostatic permanent-magnet MRI scanner. Radiol. Med. (Torino) 120, 329–337 (2015).
Ishii, Y. et al. Knee adduction moment is correlated with the increase in medial meniscus extrusion by dynamic ultrasound in knee osteoarthritis. Knee 38, 82–90 (2022).
Ishii, Y. et al. Dynamic ultrasonography of the medial meniscus during walking in knee osteoarthritis. Knee 27, 1256–1262 (2020).
Chang, A. et al. Thrust during ambulation and the progression of knee osteoarthritis. Arthritis Rheum. 50, 3897–3903 (2004).
Andriacchi, T. P. et al. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr. Opin. Rheumatol. 18, 514–518 (2006).
Ishii, Y. et al. Increase in medial meniscal extrusion in the weight-bearing position observed on ultrasonography correlates with lateral thrust in early-stage knee osteoarthritis. J. Orthop. Sci. 25, 640–646 (2020).
Kuroyanagi, Y. et al. A quantitative assessment of varus thrust in patients with medial knee osteoarthritis. Knee 19, 130–134 (2012).
Ishii, Y. et al. Dynamic response of medial meniscus extrusion to the lateral wedge insole is correlated with immediate pain reduction in knee osteoarthritis patients: real-time ultrasonographic study. J. Med. Ultrason. 2001(49), 731–738 (2022).
Ishii, Y. et al. Effects of lateral wedge insole application on medial compartment knee osteoarthritis severity evaluated by ultrasound. Knee 44, 1408–1413 (2017).
Costa, C. R. et al. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear?. AJR Am. J. Roentgenol. 183, 17–23 (2004).
Jee, W.-H. et al. Meniscal tear configurations: categorization with MR imaging. AJR Am. J. Roentgenol. 180, 93–97 (2003).
Howell, R. et al. Degenerative meniscus: Pathogenesis, diagnosis, and treatment options. World J. Orthop. 5, 597–602 (2014).
Low, A. K. et al. Clinical significance of intrasubstance meniscal lesions on MRI. J. Med. Imaging Radiat. Oncol. 52, 227–230 (2008).
Furumatsu, T. et al. A giraffe neck sign of the medial meniscus: A characteristic finding of the medial meniscus posterior root tear on magnetic resonance imaging. J. Orthop. Sci. 22, 731–736 (2017).
Lee, Y. G. et al. Magnetic resonance imaging findings of surgically proven medial meniscus root tear: Tear configuration and associated knee abnormalities. J. Comput. Assist. Tomogr. 32, 452–457 (2008).
Mills, K. et al. Current concepts in joint pain in knee osteoarthritis. Schmerz Berl. Ger. 33, 22–29 (2019).
Miyazaki, T. et al. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann. Rheum. Dis. 61, 617–622 (2002).
Daszkiewicz, K. et al. Biomechanics of the medial meniscus in the osteoarthritic knee joint. PeerJ 9, e12509 (2021).
Teng, H.-L. et al. higher knee flexion moment during the second half of the stance phase of gait is associated with the progression of osteoarthritis of the patellofemoral joint on magnetic resonance imaging. J. Orthop. Sports Phys. Ther. 45, 656–664 (2015).
Walter, J. P. et al. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. J. Orthop. Res. 28, 1348–1354 (2010).
Furumatsu, T. et al. Injury patterns of medial meniscus posterior root tears. Orthop. Traumatol. Surg. Res. 105, 107–111 (2019).
Marzo, J. M. et al. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am. J. Sports Med. 37, 124–129 (2009).
Karpinski, K. et al. No dynamic extrusion of the medial meniscus in ultrasound examination in patients with confirmed root tear lesion. Knee Surg. Sports Traumatol. Arthrosc. (2019).
Lerer, D. B. et al. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 33, 569–574 (2004).
Zhang, X. et al. Medial meniscus posterior root repair reduces the extruded meniscus volume during knee flexion with favorable clinical outcome. Knee Surg. Sports Traumatol. Arthrosc. 29, 4205–4212 (2021).
Okazaki, Y. et al. Medial meniscus posterior root repair restores the intra-articular volume of the medial meniscus by decreasing posteromedial extrusion at knee flexion. Knee Surg. Sports Traumatol. Arthrosc. 28, 3435–3442 (2020).
Liu, T. et al. The MRI-based 3D morphologic changes of knee meniscus under knee weight-bearing and early flexion conditions. Sci. Rep. 11, 22122 (2021).
Shimozaki, K. et al. Usefulness of ultrasonography for dynamic evaluation of medial meniscus hoop function in early knee osteoarthritis. Sci. Rep. 11, 20091 (2021).
Funding
This study was supported by Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (JSPS) (Award Numbers: 21K21218, 21K11191, 23k16541).
Author information
Authors and Affiliations
Contributions
Y.I.: acquisition and analysis of data, conception and design, and drafting the article, Y.N., K.O. and K.T.: image reconstruction, M.I. and G.K.: recruiting participants and interpretation of data, T.H. and S.O.: acquisition and analysis of data, M.T.: interpretation of data and drafting the article, N.A.: final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ishii, Y., Ishikawa, M., Nakashima, Y. et al. Unique patterns of medial meniscus extrusion during walking and its association with limb kinematics in patients with knee osteoarthritis. Sci Rep 13, 12513 (2023). https://doi.org/10.1038/s41598-023-39715-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-39715-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.