Abstract
Particulate matter (PM) is a major air pollutant that has led to global health concerns and can cause and exacerbate chronic obstructive pulmonary disease (COPD). We asked patients with COPD to complete a detailed questionnaire about their lifestyle practices to reduce PM2.5 exposure and analyzed the relationship between ambient PM2.5 concentrations and lifestyle practices. We prospectively enrolled 104 COPD patients from four hospitals in different areas of Korea. They completed detailed questionnaires twice (at enrollment and the end of the study) and Internet of Things-based sensors were installed in their homes to continuously measure PM2.5 for 1 year. The relationship between PM2.5 concentrations, lifestyle practices, and COPD exacerbations were analyzed in each season. The PM2.5 concentration was higher outdoors than indoors in all seasons except summer, and the difference was largest in winter. The six lifestyle practices that significantly lowered the annual indoor PM2.5 concentration compared with the outdoors. The higher the economic status and educational level of patients, the lower the indoor PM2.5 concentration. Some lifestyle practices were associated with reduced small airway resistance, presented as R5–R20 determined by impulse oscillometry, and scores of the St. George’s Respiratory Questionnaire. Some lifestyle practices are associated with reduced indoor PM2.5 concentrations and can even affect clinical outcomes, including small airway resistance and quality of life of COPD patients.
Similar content being viewed by others
Introduction
Air pollution is a major public health threat and is estimated to cause 7 million deaths worldwide each year1,2,3. Due to nationwide efforts of some developed countries, air quality has improved and beneficial effects have been reported4. However, the concentrations of air pollutants far exceed the upper limit defined by the World Health Organization in developing countries2. Moreover, socially vulnerable people are also vulnerable to various air pollutants even in developed countries5. There is no lower limit of air pollution that does not affect our health6. These findings suggest that the lower exposure to air pollution, the better our health, and great efforts should be made to reduce exposure to air pollution.
Identification and control of pollution sources is the best approach to improve air pollution, but this is not easily achieved in most countries. It is particularly complicated to analyze pollution sources in Korea, which is located between Asia, China, and the Pacific Ocean. Due to its location, PM concentrations dynamically change over seasons due to fluctuations in pollutants from domestic and foreign sources according to alterations in the wind direction7. Countries with transboundary air pollution cannot improve air quality solely through domestic regulation. No specific system has been established to share information across jurisdictions between countries in Northeast Asia8, indicating it will be difficult to dramatically reduce ambient pollutants in the near future and that individual efforts to reduce exposure are required.
Patients with chronic respiratory diseases are susceptible to air pollutants. PM with a diameter smaller than 2.5 µm (PM2.5) is associated with hospitalizations and mortality of patients with chronic obstructive pulmonary disease (COPD)9,10 and is even considered a risk factor for this disease11. COPD is neither fully reversible nor medically curable and is a major cause of human mortality. Reduction of outdoor ambient PM2.5 can be advantageous for patients with COPD and can be achieved by nationwide efforts and international collaborations12, but is not easily accomplished as mentioned earlier. A similarly large number of deaths is associated with exposure to indoor air pollution, which can be controlled by individuals, and it takes less time to reduce air pollution indoors than outdoors. In this context, guidance to effectively reduce indoor PM2.5 exposure must be developed. However, most lifestyle guidelines to avoid PM2.5 exposure are based on experts’ opinions without definite evidence. We hypothesized that indoor PM2.5 concentrations are affected by lifestyle behaviors and can be reduced by appropriate lifestyle modifications. To develop an effective strategy and guide patients, we performed a detailed questionnaire survey about daily habits to reduce PM exposure of patients with COPD and measured real-time PM2.5 concentrations in their homes for 1 year. By analyzing lifestyle practices and indoor and outdoor PM2.5 concentrations according to the season in patients with COPD, we aimed to elucidate lifestyle behaviors that improve indoor PM2.5 concentrations and to determine the impact of PM2.5 concentrations on acute COPD exacerbations.
Materials and methods
Participants
This prospective panel study recruited patients with COPD from four representative areas of Korea: two metropolitan areas (Seoul, Asan Medical Center and Incheon, Gachon University Gil Medical Center), an industrialized area (Ulsan, Ulsan University Hospital), and a clean rural area (Gangwon province, Gangneung Asan Hospital). The inclusion criteria were (1) adults aged 40 years or older; (2) diagnosis of COPD, defined as post-bronchodilator forced expiratory volume in 1 s (FEV1)/forced vital capacity (FVC) < 0.7; and (3) predicted FEV1 less than 80% of the predicted value at enrollment. The exclusion criteria were (1) patients without respiratory symptoms and (2) patients who could not understand the questionnaires used in the study or instructions about how to use the air sampler device. This study was approved by the Institutional Review Boards of Asan Medical Center (2019-0476), Ulsan University Hospital (2019–07–049), Gangneung Asan Hospital (2019-06-049), and Gil Medical Center (GBirb2019-290). The detailed study design was published previously13.
Study design
Demographic and clinical data, including data about age, sex, current address, concurrent asthma, and history of smoking, were collected at enrollment after obtaining written informed consent. Detailed questionnaire surveys were completed by the participants. Internet of Things (IoT)-based sensors were installed in their homes to measure indoor PM2.5 concentrations. The presence of COPD exacerbations was checked every month. Indoor PM2.5 concentrations were continuously monitored for 1 year. The associations between indoor PM2.5 concentrations and responses to the questionnaires and their impact on COPD exacerbations were analyzed.
Questionnaires about lifestyles, social environment, and clinical data collection
Participants completed questionnaires about their indoor and outdoor environments and lifestyle practices to avoid PM exposure. Questions about the indoor environment asked about the method of indoor ventilation, presence of an indoor ventilating system, whether the kitchen and living room were separated, and use of household appliances such as air filters. Questions about the outdoor environment asked about the distance of their home from the road and traffic volume. The questionnaire about lifestyle practices included 20 practice items for which the response scale ranged from score 0 (have never practiced) to score 7 (practiced every day, Table S1). The questionnaire was formed based on a list of recommended behaviors from our national health department14,15,16 and a list of protective interventions from a literature review17. All questionnaires were completed twice, at enrollment and the end of the study (1 year). Information about educational level and economic status was also collected13. Patients attending Asan Medical Center underwent serial impulse oscillometry. All institutions the subjects’ information was sourced from obtained the informed consent. The data used encrypted identification of the subjects, thus written consent was not required from the patients. All procedures and methods were conducted in accordance Declaration of Helsinki.
Measurements of PM exposure
Indoor PM2.5 concentrations were measured using a sensor-based light scattering measurement device (CP-16-A5; Aircok Inc., Seoul, Korea). The device was located at the center of each participant’s house where they spent most time. The data were sent to a server based on IoT throughout the study period. Before the analysis, data cleaning was performed. Zeroes, frozen concentration values for several hours and extreme peaks were removed from the dataset. We detected outliers using the mean (μ) and standard deviation (σ) normal distribution of the PM2.5 concentrations, set by μ ± 2.97 × σ, including 99.7% of the observations. To correct for possible errors in the light scattering methods, gravimetric measurements using a mini-volume air sampler (Model KMS-4100; KEMIK Corp., Seongnam, Korea) and an accurate aerosol spectrometer (11-D; Grimm, Ainring, Germany) were taken, respectively. Indoor PM2.5 concentrations reported by the IoT showed good linearity (R2 = 0.923) with the GRIMM reference and a moderate correlation (R2 = 0.451) with their co-located mini-volume air samplers. (Figure S1). Information about outdoor PM concentrations relating to the residential address was gathered from Air Korea, a national air pollution information system in South Korea (http://www.airkorea.or.kr).
Statistical analysis
Data are shown as mean ± standard deviation for continuous variables and as number (%) for categorical variables. For non-continuous variables such as practice scores, an analysis of variance was used to confirm the difference between indoor and outdoor PM2.5 concentrations corresponding to the practice scores. In addition, data were compared using the t-test and variation analysis by classifying the frequency with which patients performed the practices into two categories: practiced or not practiced every day. Furthermore, logistic regression analysis was used to determine COPD exacerbations according to the difference between indoor and outdoor PM2.5 concentrations. The statistical significance level was set to p < 0.05, but 0.0125 was considered significant according to Bonferroni correction in the analysis of major outcomes of seasonal lifestyle practices, considering four seasons. All statistical analyses were performed using SPSS software (version 22, IBM Corp., Armonk, NY, USA).
Results
Baseline characteristics of the patients
A total of 110 patients with COPD were enrolled for the panel study. After excluding six patients due to missing data about indoor PM2.5 concentrations, 104 patients were finally enrolled for analysis. The mean age of patients was 67.4 ± 9.8 years, and 94 (90.4%) patients were male. Twenty-three (22.1%) patients were current smokers and 64 (61.5%) patients were ex-smokers with a mean of 33.7 ± 23.3 pack years. Among them, 38 (36.5%) patients had a history of acute exacerbations in the past year. All of them used inhalers. The mean COPD assessment test score was 17.0 ± 8.7. Dyspnea assessed with the modified Medical Research Council scale was relatively mild in a large proportion of patients. More than half (62, 59.6%) of patients had grade 1, but approximately 30% had grade 3 or higher (16 [15.4%] patients had grade 3 and 14 [13.5%] patients had grade 4) at enrollment. The mean total score of the COPD-specific version of the St. George’s Respiratory Questionnaire (SGRQ-C) was 38.43 ± 2.45 and mean R5 (resistance at 5 Hz)–R20 (resistance at 20 Hz) was 0.18 ± 0.03 cmH2O/l/s (Table 1).
PM2.5 concentrations and lifestyle practices to reduce PM exposure
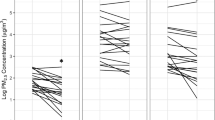
PM2.5 concentrations were lower indoors than outdoors in all seasons except summer. The difference between indoor and outdoor PM2.5 concentrations was greatest in winter (− 4.31 ± 1.02 µg/m3), followed by spring (− 1.87 ± 0.85 µg/m3), fall (− 1.20 ± 0.63 µg/m3), and summer (+ 1.27 ± 0.63 µg/m3, Fig. 1). Among the 20 lifestyle items, those commonly practiced every day included turning on the kitchen ventilation while cooking (49.0%), washing hands after coming home (42.0%), and avoiding secondhand smoke (41.0%). On the contrary, items not commonly practiced were spraying water for cleaning (24.0%), closing windows while driving (11.0%), and being equipped with emergency drugs and using them when necessary (9.0%, Fig. 2).
Mean PM2.5 concentrations by season. (A) Outdoor and indoor PM2.5 concentrations by season. (B) Indoor PM2.5 concentration compared with the outdoor PM2.5 concentration by season. The overall outdoor PM2.5 concentration was higher than the indoor PM2.5 concentration in all seasons except summer. The difference between indoor and outdoor PM2.5 concentrations was greatest in winter.
Lifestyle practices to avoid PM exposure. The 20 lifestyle items are presented according to the proportion (%) of patients. The questionnaire asked questions about how many days per week the patient usually performed the items. During the survey period, the questionnaire was completed twice, and the average scores are expressed.
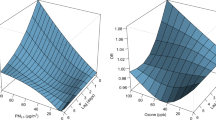
Some everyday lifestyle practices affected the difference between indoor and outdoor PM2.5 concentrations. The PM2.5 concentration was significantly lower indoors than outdoors in spring, summer, and winter when patients used indoor air filters, checked filters of air filters, ventilated the home by opening windows, and closed windows while driving with internal circulation mode. Other lifestyle practices that reduced the indoor PM2.5 concentration compared with the outdoor PM2.5 concentration in specific seasons included mopping indoors (spring and summer), choosing to go out in places with little traffic (spring and winter), and refraining from going out when the outside PM2.5 concentration was high (winter, Fig. 3). No significant association between the difference in indoor and outdoor PM2.5 concentrations and lifestyle practices was found in fall. Detailed seasonal differences are described in the online supplement. The more days air filters were used, the lower the indoor PM2.5 concentration was throughout the year (Fig. 4).
Indoor PM2.5 concentrations compared with outdoor PM2.5 concentrations over 1 year by season according to lifestyle practices to reduce PM exposure. (A) In spring, six lifestyle practices were correlated with a significant difference. (B) In summer, five lifestyle practices were correlated with a significant difference. (C) In winter, seven lifestyle practices were correlated with a significant difference.
Indoor and outdoor PM2.5 concentrations according to participants’ social environment
Further analysis was performed of participants’ social environment. The higher the economic status and educational level, the greater the difference between indoor and outdoor PM2.5 concentrations. When economic status was divided into three groups (high, middle, and low), the higher the economic status, the greater the difference between annual indoor and outdoor PM2.5 concentrations (high, − 4.71 ± 1.12 µg/m3; middle, + 0.17 ± 1.40 µg/m3; and low, − 1.93 ± 0.92 µg/m3; p = 0.086, Fig. 5A). These differences as economic levels were even more pronounced on some everyday lifestyle practices, including checking air quality forecasts (p = 0.012), checking filters of air filters (p = 0.023), wearing a mask when going out (p = 0.073), closing windows while driving with internal circulation mode (p = 0.042), and being equipped with emergency drugs and using them when necessary (p = 0.099, Fig. 5A). The difference between indoor and outdoor PM2.5 concentrations also varied according to the educational level, which was divided into three groups (higher than college graduation, high school graduation, and lower than middle school graduation). The higher the educational level, the greater the difference between annual indoor and outdoor PM2.5 concentrations (higher than college graduation, − 6.00 ± 1.14 µg/m3; high school graduation, − 1.98 ± 0.88 µg/m3; and less than middle school graduation, + 0.32 ± 1.40 µg/m3; p = 0.034, Fig. 5B). The difference between indoor and outdoor PM2.5 concentrations was more evident according to some everyday lifestyle practices including operating indoor air filters (p = 0.013), ventilating the home by opening windows (p = 0.005), checking filters of air filters (p = 0.055), mopping indoors (p = 0.075), refraining from going out when the outside PM2.5 concentration was high (p = 0.079), choosing to go out in places with little traffic (p = 0.061), and closing windows while driving with internal circulation mode (p = 0.021, Fig. 5B). Detailed differences are described in the online supplement.
Relationship between indoor PM2.5 concentrations, lifestyle practices, and acute COPD exacerbations
R5–R20 was significantly lower for patients whose everyday lifestyle practices included checking air quality forecasts (0.12 ± 0.02 cmH2O/l/s, p = 0.038) and wearing a mask when going out (0.11 ± 0.03 cmH2O/l/s, p = 0.080, Fig. 6A). The SGRQ-C score was also lower for patients whose everyday lifestyle practices including mopping indoors (29.21 ± 4.29, p = 0.046), choosing to go out in places with little traffic (27.37 ± 3.17, p = 0.004), and dusting clothes when coming home from outside(16.73 ± 2.16, p < 0.001, Fig. 6B).
Discussion
This study shows that PM2.5 concentrations can be affected by lifestyle practices and economic status according to the season. Some lifestyle practices were related with a significantly lower indoor PM2.5 concentration compared with the outdoor PM2.5 concentration in multiple seasons, including operating indoor air filters, ventilating the home by opening windows, checking filters of air filters, and closing windows while driving. Patients with a higher educational level or economic status had lower indoor PM2.5 concentrations. Lifestyle practices related to lower small airway resistance and SGRQ-C scores included checking air quality forecasts and mopping indoors. These results suggest that some lifestyle practices affect PM2.5 exposure and that exposure to PM2.5 can be reduced by adjusting these practices.
Some lifestyle practices were related with a lower indoor PM2.5 concentration compared with the outdoor PM2.5 concentration in all seasons except fall. Ventilating the home by opening windows was one such lifestyle practice. Many people wonder if regular ventilation through windows is helpful because outdoor PM2.5 concentrations are variable and sometimes higher than indoor PM2.5 concentrations. A previous study showed such ventilation is associated with reduced indoor PM2.5 concentrations even in cold seasons when the mean outdoor PM2.5 concentration is higher than that indoors18. This suggests that regular ventilation through windows does not adversely affect indoor PM2.5 concentrations if it is performed in conjunction with other lifestyle practices19. Many human activities can increase indoor PM2.5 concentrations such as walking, dressing, and cooking20. Even activities beneficial for indoor environments, such as sweeping, can dramatically increase indoor PM2.5 concentrations in the short term21. On the other hand, it would not work where the outdoor concentrations were twice as high as indoor ones22. All these findings suggests that indoor PM2.5 concentrations are variable and that regular ventilation through windows can be helpful depending outdoor conditions21. Meanwhile, the PM2.5 concentration in a vehicle becomes high if the windows are open when the outdoor PM2.5 concentration is high23. Our study found that closing windows while driving when the outdoor PM2.5 concentration was high improved the indoor PM2.5 concentration. Similarly, previous studies showed that driving with windows closed protects against traffic-related PM2.5 exposure24,25. Interestingly, this habit tended to be practiced more as the economic level of patients increased in our study.
Air filters are a well-studied intervention to reduce PM2.5 exposure. In a meta-analysis about air filter interventions for chronic respiratory diseases, air filters consistently improved indoor PM2.5 concentrations26. A recent randomized controlled trial showed that improvements of respiratory symptoms and acute exacerbations by an air filter invention were associated with reduced indoor PM2.5 concentrations27. A classroom-based air filter intervention significantly reduced PM2.5 and black carbon concentrations28. Use of indoor air filters significantly reduced indoor concentrations of PM2.5 and its components such as water soluble organics, NO3–, SO42–, Zn2+, Pb2+, and K+29. In a study of children exposed to secondhand smoke, air filters not only reduced the level of airborne particles but also improved clinical outcomes such as unscheduled hospital visits due to asthma30. A short-term intervention operating indoor air filters improved various cardiovascular biomarkers in college students31. Everyday use of air filters is recommended to significantly improve indoor PM2.5 concentrations, and checking filters is also helpful18,32. In this study, everyday use of air filters reduced indoor PM2.5 concentrations.
Maintenance of a clean indoor environment is another important strategy to reduce indoor air pollution. Interestingly, indoor mopping was significantly associated with a reduced indoor PM2.5 concentration compared with the outdoor PM2.5 concentration in spring and summer. This is consistent with the previous recommendation for wet mopping to lower indoor pollution33. The previous finding that wet sweeping increases PM2.5 concentrations less than dry sweeping supports the recommendation for wet mopping21. Another noteworthy recommendation for the indoor environment is to use a vacuum with a high-efficiency particulate-absorbing (HEPA) filter. Use of a vacuum without an appropriate filter can stir up particles and deep dust, but use of a vacuum with a HEPA filter helps to control asthma by reducing dust exposure34,35.
In contrast with other seasons, we did not find any significant association between lifestyle practices and PM2.5 concentrations in fall. This can be explained by the finding that the difference between indoor and outdoor PM2.5 concentrations was smallest in this season. A national database also showed that the mean outdoor PM2.5 concentration is lower in fall than in other seasons36. By contrast, relatively strong associations were found in winter, during which the difference between indoor and outdoor PM2.5 concentration was largest. There is evidence of seasonal variation in the rate of hospital admissions for COPD, with more exacerbations occurring during winter37,38. Exacerbations are also associated with cooler temperatures39,40. This suggests that lifestyle correction can reduce the risk of COPD more effectively in winter, when patients are usually more vulnerable.
Some other lifestyle practices, such as refraining from going out when the outside PM2.5 concentration was high and choosing to go out in places with little traffic, were also effective, which might not be directly related with indoor PM2.5 concentrations. Consistently, a previous study showed that reducing outdoor physical activities and staying inside on days when outdoor PM concentrations are very high improves indoor PM2.5 concentrations32. The U.S. Air Quality Index recommends to stay indoors in an area with filtered air and to avoid outdoor activities when the outdoor PM concentration is high. With these lifestyle practices, people can refrain from breathing rapidly and deeply, which increases PM2.5 inhalation33. This recommendation also applies to COPD patients41. It is unclear how these lifestyle practices also have beneficial effects on indoor PM2.5 concentrations. It may be because people who perform these lifestyle practices also perform other lifestyles that have significantly beneficial effects on indoor PM2.5 concentrations. In our study, participants who chose to go out in places with little traffic also performed other effective lifestyle practices (Figure S3). A group of participants may perform several lifestyle practices simultaneously to reduce PM exposure.
Long-term and constant exposure to high PM2.5 concentrations leads to aggravation of respiratory symptoms and acute exacerbations of COPD via inflammation, oxidative stress, immune dysfunction, and alterations of the airway epithelial structure and microbiome42,43. Therefore, lowering exposure to higher PM2.5 concentrations is a viable approach to reduce acute exacerbations, attenuate COPD progression, and decrease the associated healthcare burden42. In our study, we evaluated whether clinical outcomes were improved by lifestyle practices that reduced PM2.5 concentrations. Checking air quality forecasts (PM2.5 concentrations) daily and wearing a mask when going out correlated with lower R5–R20 levels. In addition, mopping indoors, choosing to go out in places with little traffic, and dusting off clothes after coming home were also associated with lower SGRQ-C total scores. Considering the aforementioned findings, specific lifestyle practices can improve clinical outcomes of COPD patients by reducing PM2.5 exposure.
Several limitations can be suggested in this study. First, the lifestyle questionnaire was based on people’s memories, which can sometimes be biased. This may be why only lifestyle practices performed every day (7 days/week) made a significant difference. Second, the PM2.5 concentrations from IoT-based sensors showed a moderate correlation with their co-located mini-volume air samplers. In this study, the correlation of IoT with the Grimm reference was excellent (R2 = 0.923), but its mean concentrations showed a relatively lower correlation with 24-h volume sampling. This is likely due to different conditions at each deployment site, such as chemical PM2.5 compositions, temperature, relative humidity, and indoor sources. Therefore, it is crucial to develop more accurate real-time monitoring of PM2.5 concentrations since gravimetric monitoring is impractical for long-term home-based cohorts due to noise and device size. Despite this limitation, the findings of the current study are important for several reasons. First, PM has a significant impact on development and progression of COPD, but research about individual management for PM2.5 exposure is lacking. This study reported the detailed lifestyle practices of COPD patients and how they can affect PM2.5 concentrations. It also found a relationship between PM2.5 concentrations and acute COPD exacerbations. Second, IoT-based PM2.5-measuring sensors were installed in patients’ home, and indoor PM concentrations were monitored continuously. This study provides evidence with more accurate data. Third, this study collected data over 1 year and noted dynamic changes in PM2.5 concentrations according to the season. Using this study design, the effect of each lifestyle practice in each season could be determined.
In conclusion, lifestyle practices are associated with indoor PM2.5 concentrations and can even affect clinical outcomes, including small airway resistance and quality of life of COPD patients. Some lifestyle practices such as operating air filters and ventilating the home by opening windows help to reduce PM2.5 concentrations, and these can be included as scientific guidance to reduce exposure of patients with COPD to PM2.5.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- FEV1 :
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- HEPA:
-
High-efficiency particulate-absorbing
- IoT:
-
Internet of Things
- PM:
-
Particulate matter
- PM2.5 :
-
Particulate matter with a diameter smaller than 2.5 µm
- SGRQ-C:
-
COPD-specific version of the St. George’s Respiratory Questionnaire
References
Brook, R. D. et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 121(21), 2331–2378 (2010).
WHO’s global air-quality guidelines. Lancet 368(9544), 1302 (2006).
Wang, Y. et al. Estimating causal effects of long-term PM2.5 exposure on mortality in New Jersey. Environ. Health Perspect. 124, 1182–1188 (2016).
Gauderman, W. J. et al. Association of improved air quality with lung development in children. N. Engl. J. Med. 372(10), 905–913 (2015).
Di, Q. et al. Air Pollution and Mortality in the Medicare Population. N. Engl. J. Med. 376(26), 2513–2522 (2017).
Pope, C. A. 3rd. et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 287(9), 1132–1141 (2002).
Jung, W. Environmental Challenges and Cooperation in Northeast Asia. Institute for Security & Development Policy. 16 March 2016.
OECD. <Policy Brief-NE Asia_Air pollution.pdf>.
Zhu, R. X. et al. Relationship between particulate matter (PM(2.5)) and hospitalizations and mortality of chronic obstructive pulmonary disease patients: A meta-analysis. Am. J. Med. Sci. 359(6), 354–364 (2020).
Li, M. H. et al. Short-term exposure to ambient fine particulate matter increases hospitalizations and mortality in COPD: A systematic review and meta-analysis. Chest 149(2), 447–458 (2016).
Liu, S. et al. Association between exposure to ambient particulate matter and chronic obstructive pulmonary disease: Results from a cross-sectional study in China. Thorax 72(9), 788–795 (2017).
Schraufnagel, D. E. et al. Health benefits of air pollution reduction. Ann Am Thorac Soc. 16(12), 1478–1487 (2019).
Park, S., Ra, S. W., Kang, S. Y., Kim, H.-C. & Lee, S. W. Effect of particulate matter exposure on patients with COPD and risk reduction through behavioural interventions: The protocol of a prospective panel study. BMJ Open 10(11), e039394 (2020).
Asmussen, L. et al. Use of the child health questionnaire in a sample of moderate and low-income inner-city children with asthma. Am. J. Respir. Crit. Care Med. 162(4 Pt 1), 1215–1221 (2000).
Seoul, RoK. Step-by-step health-vulnerable class PM behavior manual. July, 2017.
Jo, H.-J., Park, S.-W., Lee, H.-I. & Lee, S.-W. Health effects caused by particulate matter and guidelines for health care. Wkly. Health Dis. (Korea Centers for Disease Control and Prevention (KCDC) 15, 458–462 (2018).
Xiong, L. et al. Risk reduction behaviors regarding PM(2.5) exposure among outdoor exercisers in the Nanjing Metropolitan area, China. Int J Environ Res Public Health. 15(8), 1728 (2018).
Kim, H. et al. The impact of life behavior and environment on particulate matter in chronic obstructive pulmonary disease. Environ Res. 198, 111265 (2021).
Yang, Z., Shen, J. & Gao, Z. Ventilation and air quality in student dormitories in China: A case study during summer in Nanjing. Int. J. Environ. Res. Public Health 15(7), 1328 (2018).
Zhou, Z. et al. Indoor PM2.5 concentrations in residential buildings during a severely polluted winter: A case study in Tianjin, China. Renew. Sustain. Energy Rev. 64, 372–381 (2016).
Lin, Y., Zou, J., Yang, W. & Li, C.-Q. A review of recent advances in research on PM2.5 in China. Int. J. Environ. Res. Public Health 15(3), 438 (2018).
Wallace, L. A., Zhao, T. & Klepeis, N. E. Indoor contribution to PM(2.5) exposure using all PurpleAir sites in Washington, Oregon, and California. Indoor Air 32(9), e13105 (2022).
Guan, W.-J., Zheng, X.-Y., Chung, K. F. & Zhong, N.-S. Impact of air pollution on the burden of chronic respiratory diseases in China: Time for urgent action. Lancet 388(10054), 1939–1951 (2016).
Chaney, R. A. et al. Personal exposure to fine particulate air pollution while commuting: An examination of six transport modes on an urban arterial roadway. PLoS ONE 12(11), e0188053-e (2017).
Peng, L. et al. Personal exposure to PM2.5 in five commuting modes under hazy and non-hazy conditions. Environ. Pollut. 289, 117823 (2021).
Park, H. J. et al. The effect of particulate matter reduction by indoor air filter use on respiratory symptoms and lung function: A systematic review and meta-analysis. Allergy, Asthma Immunol. Res. 13(5), 719–732 (2021).
Hansel, N. N. et al. Randomized clinical trial of air cleaners to improve indoor air quality and COPD health: Results of the CLEAN AIR study. Am. J. Respir. Crit. Care Med. 205(4), 426 (2021).
Jhun, I. et al. School environmental intervention to reduce particulate pollutant exposures for children with asthma. J. Allergy Clin. Immunol. Pract. 5(1), 154–9.e3 (2017).
Shao, D. et al. Cardiorespiratory responses of air filtration: A randomized crossover intervention trial in seniors living in Beijing: Beijing Indoor Air Purifier StudY, BIAPSY. Sci. Total Environ. 603–604, 541–549 (2017).
Lanphear, B. P. et al. Effects of HEPA air cleaners on unscheduled asthma visits and asthma symptoms for children exposed to secondhand tobacco smoke. Pediatrics 127(1), 93–101 (2011).
Chen, R. et al. Cardiopulmonary benefits of reducing indoor particles of outdoor origin: A randomized, double-blind crossover trial of air purifiers. J. Am. Coll. Cardiol. 65(21), 2279–2287 (2015).
Kate Wolff, MPA. et al. Ventilation in your home. Centers for disease control and prevention.
Michael S. Regan. et al. Extremely high levels of PM2.5: steps to reduce your exposure.
Roberts, J. W. et al. Monitoring and reducing exposure of infants to pollutants in house dust. Rev. Environ. Contam. Toxicol. 201, 1–39 (2009).
Castner, J., Barnett, R., Moskos, L. H., Folz, R. J. & Polivka, B. Home environment allergen exposure scale in older adult cohort with asthma. Can. J. Public Health 112(1), 97–106 (2021).
Airkorea. Monthly/annual report on air conditioning. 2020.
Bryden, C., Bird, W., Titley, H. A., Halpin, D. M. & Levy, M. L. Stratification of COPD patients by previous admission for targeting of preventative care. Respir. Med. 103(4), 558–565 (2009).
Jenkins, C. R. et al. Seasonality and determinants of moderate and severe COPD exacerbations in the TORCH study. Eur. Respir. J. 39(1), 38 (2012).
Dowell, S. F. & Ho, M. S. Seasonality of infectious diseases and severe acute respiratory syndrome-what we don’t know can hurt us. Lancet. Infect. Dis 4(11), 704–708 (2004).
Kim, Y.-M., Kim, J., Cheong, H.-K., Jeon, B.-H. & Ahn, K. Exposure to phthalates aggravates pulmonary function and airway inflammation in asthmatic children. PLoS ONE 13(12), e0208553 (2018).
Choi, J. et al. Harmful impact of air pollution on severe acute exacerbation of chronic obstructive pulmonary disease: Particulate matter is hazardous. Int. J. Chron. Obstruct. Pulmon. Dis. 13, 1053–1059 (2018).
Ni, L., Chuang, C.-C. & Zuo, L. Fine particulate matter in acute exacerbation of COPD. Front. Physiol. 6, 294 (2015).
Hansel, N. N. et al. In-home air pollution is linked to respiratory morbidity in former smokers with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 187(10), 1085–1090 (2013).
Acknowledgements
The authors would like to thank all the members of our research group in University of Ulsan College of Medicine, Asan Medical Center, Gangneung Asan Hospital, Ulsan University Hospital, Gachon University Gil Medical Center and Inha University who contributed to this study, and all the participants involved to support this study.
Funding
This research was supported by the “National Institute of Health” research project (No. 2019ER671100 and 01, and 2021ER120900) and grants from the Korea Research Institute of Bioscience and Biotechnology (KRIBB) Research Initiative Program (KGM5322321), Republic of Korea.
Author information
Authors and Affiliations
Contributions
H.K.: Conceptualization, Formal analysis, Software, Writing—original draft. J.-Y.H.: Formal analysis, Investigation, G.N.: Data collection, Investigation, Formal analysis. S.P.: Investigation, Data curation. S.W.R.: Investigation, Data collection. S.-Y.K.: Investigation, Data collection. H.C.K.: Conceptualization. H.-C.K.: Conceptualization, Investigation, Formal analysis, Data collection. S.W.L.: Conceptualization, Formal analysis, Software, Writing – original draft, Funding acquisition.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, H., Huh, JY., Na, G. et al. Lifestyle practices that reduce seasonal PM2.5 exposure and their impact on COPD. Sci Rep 13, 11822 (2023). https://doi.org/10.1038/s41598-023-38714-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38714-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.