Abstract
We aimed to evaluate the effect of the patient’s clinical and paraclinical condition before and after surgery on short-term mortality and complication and long-term mortality. A retrospective cohort study was conducted and multivariate logistic regression was applied to determine the effect of demographic characteristics (sex, age, AO/OTA classification, height, weight, body mass index), medical history (hypertension, ischemic heart disease, diabetes mellitus, thyroid malfunction, cancer, osteoporosis, smoking) lab data (Complete blood cell, blood sugar, Blood Urea Nitrogen, Creatinine, Na, and K), surgery-related factors (Anesthesia time and type, implant, intraoperative blood transfusion, postoperative blood transfusion, and operation time), duration of admission to surgery and anticoagulant consumption on short-term mortality and complication and long-term mortality. Three hundred ten patients from November 2016 to September 2020 were diagnosed with an intertrochanteric fracture. 3.23% of patients died in hospital, 14.1% of patients confronted in-hospital complications, and 38.3% died after discharge till the study endpoint. ΔNumber of Neutrophiles is the primary determinant for in-hospital mortality in multivariate analysis. Age and blood transfusion are the main determinants of long-term mortality, and Na before surgery is the primary variable associated with postoperative complications. Among different analytical factors Na before surgery as a biomarker presenting dehydration was the main prognostic factor for in hospital complications. In hospital mortality was mainly because of infection and long-term mortality was associated with blood transfusion.
Similar content being viewed by others
Introduction
In an aging population, osteoporotic fractures continue to rise. By the year 2025, there are estimated to be 2.6 million hip fractures, which will increase to 4.5 million by 2050. The changes will be more substantial in Asia, with the percentage of fragility fractures is estimated to increase from 26% of all hip fractures in 1990 to 37% in 2025, and to 45% in 20501. The estimated cost of intertrochanteric hip fractures in the United States healthcare system is $2.63 billion USD per year which represents 44% of all hip fracture costs2. Apart from the economic burden, the risks of subsequent fracture following a hip fracture, mortality, and morbidity including impaired mobility and decreased quality of life remain considerable compared to the general population3.
The 1-year mortality rate for intertrochanteric fractures has decreased from 34 to 23% gradually in the literature4. Still, in-hospital complications and mortality following hip fracture is reported in up to 13% and 5%, respectively5. Associations have been found between the surgical approach6, Charlson Comorbidity Index7, delay from admission to surgery8, body mass index9, anticoagulant consumption10,11,12, type of anesthesia13 and mortality or complications following hip fractures surgery have been previously discussed. Pre-operative factors like anemia14, nutritional parameters15, analytical values16, blood parameters17, and neutrophile to lymphocyte ratio can be measured by a blood test and the prognostic role of these variables is valuable.
We aimed to evaluate the risk factors for morbidity/mortality in patients undergoing surgery for a hip fracture. In particular, we were interested in the association between demographic characteristics, AO/OTA fracture classification, comorbidities, surgical variables, and laboratory tests before and after surgery with in-hospital complications, in-hospital mortality and long-term mortality.
Material and methods
Study population
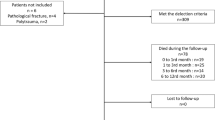
We retrospectively reviewed data from all consecutive patients admitted with intertrochanteric fractures to a trauma referral center Tehran, Iran, from November 2016 to September 2020. Bilateral, high-energy, peri-prosthetic, and pathologic fracture, as well as non-operatively treated patients were excluded. Conservative treatment is only indicated for patients who do not agree to undergo surgery. Institutional IRB approval was obtained prior to data collection. All participants gave informed consent, and the proposal was approved by the Tehran University of Medical Sciences review board. All methods were performed in accordance with the approved guidelines and regulations of Tehran University of Medical Sciences.
Data collection
Charts were reviewed to collect the patients’ demographic information (age, height, weight, body mass index (BMI)), past medical history, medication history, substance use, and family history. Lab results of interest were also collected, including cell count, biochemistry, and metabolic profile. Radiographs at the time of admission were reviewed to classify the fracture type based on the AO/OTA classification. Surgical variables including surgical and anesthesia time, type of surgery and anesthesia, and blood transfusion were also collected.
ΔVariable was defined as:
Outcomes
In November 2021, patients were contacted by phone. To determine the outcome, patient or close family were asked whether the patient was alive and, if not, the passing date. Mortality in hospital (post-operative) and complications were obtained from charts. All outcomes are expressed as a binary variable.
Statistical analysis
SPSS version 23 for windows (IBM, Armonk, New York) was used for the statistical analysis Data are presented as the mean and standard deviation or the number of cases and percentages whenever needed. Student’s t test, Pearson, chi-square, and Fisher exact tests were used as appropriate to assess unadjusted associations between variables and outcomes. A p-value of <0.1 was considered significant for univariate analysis. Hosmer-Lemeshow test was performed to evaluate our final regression model. Furthermore, we conducted ROC analysis to develop a screening test. A p-value of <0.05 was considered significant for binary logistic regression, cox regression, and Kaplan-Meier analysis. A p-value of <0.05 was considered significant for ROC analysis and Area under the curve (AUC) > 0.70 was acceptable to achieve a screening test with maximum sensitivity and specificity. The Youden J statistic was applied to determine optimal cutoff points18. Our statistical analysis was carried out in consultation with a statistician.
Ethics approval and consent to participate
The ethics committee of Tehran University of Medical Sciences, Tehran, Iran, has approved. This manuscript. Written informed consent was obtained from patients for publication and all participants gave their consent for participation.
Results
During the study period Three hundred ten patients were diagnosed with an intertrochanteric fracture. 270 patients had full-recorded progress notes in which in hospital complication could be assessed (87%). 67 patients lost to follow-up, which results in a sample size of 243 patients for mortality in long term (81%). All post operative complications are presented on Table 1. The percentage of the female population in those who died in hospital, had complications in hospital, and died in log-term after discharge are as follows: 30%, 34.2%, and 59.1%; Also the mean age of those who died in hospital, had complications in hospital, and died in log-term after discharge is 82.30, 76.37, and 78.55 years respectively. 3.23% of patients died in hospital, 14.1% of patient confront in hospital complication and 38.3% died after discharge till study endpoint. Patients’ data are shown in Table 2.
Patients who died in hospital tend to have higher white blood cells before surgery (p = 0.024), BUN before surgery (p = 0.000), an increased Δ White blood cells (p = 0.033), Δ Cr (mg/dL) (p = 0.077), Δ Neutrophile/Platelet (p = 0.000), Δ Number of Neutrophiles (p = 0.031), and a significant drop in platelet count (p = 0.021).
Patients experiencing postoperative complications in the hospital were more likely to have an increased Δ Cr (p = 0.017), Δ BUN (p = 0.099), and Na before surgery (p = 0.022). Patients who died in the long term were more likely to be female (p=0.013), and those with a lower rate of smoking (p=0.008), a lower Hemoglobin before surgery (p=0.000), a lower drop in hemoglobin (p=0.020), longer Duration of admission to surgery (P=0.004), to have Diabetes Mellitus (p=0.004), BUN before surgery (p=0.000), K before surgery (p=0.076), Δ Na (p=0.064), Δ Neutrophile/Lymphocyte (p=0.072), and Blood sugar baseline (p=0.028). Older age, history of HTN or IHD, blood transfusion (before or after surgery), and higher creatine levels before surgery lead to the worse outcome (in hospital mortality, long-term mortality or in hospital complication).
To develop a regression model for in-hospital mortality as the dependent variable, Δ White blood cell, Δ Cr, and Δ Neutrophile/Platelet were excluded due to high interaction with other variables (The variables which measured the same marker before surgery and is significantly different between groups). The p-value of the Hosmer and Lameshow test is 0.998. Δ Number of Neutrophiles is significant in multivariate analysis. The result is shown in Table 3. ROC analysis was performed for quantitative variables correlated with in-hospital mortality in univariate analysis. The AUC for age (0.721, 95% CI [0.586–0.856]), BUN before surgery (0.770, 95% CI [0.596–0.943]), and Cr before surgery (0.866, 95% CI [0.790–0.941]) were more than 0.70. (Fig. 2). The optimal cut-off values for age, BUN before surgery, and Cr before surgery were 78.5 years (sensitivity = 0.900 and specificity = 0.540), 54.5 mg/dL (sensitivity = 0.800 and specificity = 0.703), and 1.43 mg/dL (sensitivity = 0.800 and specificity = 0.859). Age, HTN, IHD, Cr before surgery, Na before surgery, Δ BUN, and blood transfusion are included in the regression model for in-hospital complications. The p-value of the Hosmer and Lameshow test is 0.117. Na before surgery is the main determinant. The model is explained in Table 4. The AUC for age, Cr before surgery, Na before surgery, Δ BUN were all less than 0.70. The predictive model for long-term mortality was obtained by cox regression and ΔHb is excluded due to interaction with hemoglobin before surgery; ΔNa and Δ Neutrophile/lymphocyte were also excluded to reach the fittest model available. Age and blood transfusion are the main determinants. The model is explained in Table 5. The AUC for age (0.720, 95% CI [0.657–0.783]) and Hemoglobin before surgery (0.718, 95% CI [0.652–0.784] were more than 0.70. the optimal cut-off value for age and Hemoglobin before surgery were 74.5 years (sensitivity = 0.72 and specificity = 0.62) and 11.05 mg/dL (sensitivity = 0.74 and specificity = 0.634) (Fig. 1).
Receiver operating characteristics curves (ROC) for Age (A), BUN before surgery (B), and Cr before surgery (C) while those who die in hospital are considered the positive result of the test. ROC for age (D) Hemoglobin before surgery (E) while those who die in long term and those who remain alive are considered the positive result of the test respectively.
Patients stratified into 4 groups base on blood transfusion status and age. Kaplan–Meier survival curves of four groups are demonstrated. The 54 months survival of total population is 0.51 (SE=0.044) (Fig. 2).
Discussion
The results of our study suggest that a significant rise in number of neutrophile may be associated with in-hospital mortality. Those with increased Na before surgery are more likely to experience in hospital complication. Age is the main determinant of long-term mortality alongside with intra and post-operative blood transfusion.
Post-op neutrophil as a biomarker representing infection was correlated with short-term mortality19. Neutrophile count was positively correlated with size of infarction, and Ischemic and non-ischemic heart failure are associated with increased innate leukocytes, and post-op heart failure has a robust association with mortality after hip fracture19,20,21. After stroke neutrophil start to degrade blood brain barrier and predispose brain to a second injury and by several mechanism worsens outcome22. Furthermore, in acute ischemic strokes, peripheral neutrophil counts are correlated with larger infarct volumes and fatal outcomes23. In hypertensive population neutrophil count increase the risk of first stroke and stroke is one of the post-op comorbidities which increase the risk of mortality in those with hip fracture19,24.
In a cohort study of Asian population, 14,744 elderly patients with hip fracture were followed up for 11 years. 10973 patients included in the transfusion group and the adjusted relative risk of mortality was 1.64, 1.58, 1.43 for 90 days, 180 days, and 1 year respectively25. In our study the adjusted odds ratio of mortality was 1.932 (95% CI [1.023–3.648], p=0.042). It is believed that there might be immunosuppressive consequences with blood transfusion by suppressing CD3 (T-lymphocytes)26. This could result in making patients susceptible to infection which is supported by a meta-analysis of 20 studies which reported an odds ratio of 5.263 (range, 5.03–5.43) for bacterial infection in trauma patients while infection is a risk factor of long-term mortality in the study of Roche et al.19,27,28. A large blood transfusion may lead to fluid overload in elderly who are small and frail. Comorbidities like HTN, chronic kidney disease, and previous heart failure as predisposing factor in combination with large blood transfusion may lead to iatrogenic heart failure and heart failure is the most important risk factor of long-term mortality after hip fracture19,29. To overcome this problem other blood product including iron supplements, Erythropoietin, or anti-fibrinolytics should be considered30,31,32. However, in a meta-analysis of 54 studies in 2015 the results don’t demonstrate an increased risk of long-term mortality in those with blood transfusion after adjusting for all comorbidities33. Further prospective studies with larger sample size are needed to clarify the effect of blood transfusion on long-term mortality. In our study 93 patients (38%) died in long-term and based on Kaplan-Meier analysis the 54-month survival of our patients is 51% and one-year mortality is nearly 15%. Another study by Mehdi Nasab et al. reported a 5-year mortality rate of 37% and a one-year mortality rate of 21%, but this study calculated the mortality rate by dividing the number of deaths in five years by the total population34. A randomized clinical trial by Moradi et al. reported a higher one-year mortality rate of 21% compared to our study35. In a systematic review and meta-analysis by Ma et al. the rate of early mortality following intertrochanteric fracture was 15.1%36. The in-hospital mortality rate reported in the literature ranged from 1.2 to 1.8%, which is lower than the mortality rate of our study (3.23%)8,37,38. It is worth noting that our hospital is a referral center, and our patients mainly come from regions with poor economic and sanitary conditions.
Our study found that higher levels of Na are associated with an increased risk for complications in hospital. Dehydration caused by water loss is best diagnosed by serum osmolality in older people39. Dehydration is a major problem in the geriatrics with hip fractures. In a retrospective cohort study in 2015 the application of preoperative hemodynamic preconditioning protocol (PHP) results in lower complications for patients with hip fracture. Patients with hip fractures who were deemed at high risk for complications or mortality were treated following the PHP protocol to ensure adequate perfusion and oxygenation and to optimize hemodynamics before surgery40. In the study by Lindholm et al. dehydration was reported as a prognostic factor for pressure ulcers at discharge for those with hip fracture (p=0.005), however, we had only two cases of pressure ulcers41. In a study of 45 patients following hip fracture surgery, dehydration increased the chances of complications by nearly four times (P<0.015); Dehydrated patients presented with confusion, desaturation requiring oxygen treatment, and cardiovascular problems42. Our results are in contrast with a study of 8719 patients with total hip arthroplasty in which dehydration didn’t show any significant relationship with 30-day complications and appears as a protective factor for 30-day readmission (P=0.001). The main difference of last study and our study is the acute setting of present study. Anemia at presentation is risk factor for 30-day readmission and those with dehydration are usually considered as non-anemic group14. One of the reasons could be the blood transfusion in anemic group in the acute setting of hip fracture which increases the infection after surgery while in the elective setting of arthroplasty administration of TXA reduces the risk of readmission14,43.
Several limitations of study should be mentioned. The reliability and accuracy of AO/OTA classification is questionable44. Distribution of cases in subgroups of AO/OTA, type of implant, and type of anesthesia was unbalanced and this leads to random error. The retrospective nature of study which was conducted in one center result in selection bias. Unfortunately, because of recall bias we were not able to analyze the cause of death. The complication was an outcome with high heterogeneity which cannot be sub grouped due to unbalanced distribution of type of complication. Finally, we were not able to introduce a comorbidity index into our analysis.
Conclusion
Among different analytical factors Na before surgery as a biomarker presenting dehydration was the main prognostic factor for in hospital complications. In hospital mortality was mainly because of infection and long-term mortality was associated with blood transfusion.
Data availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- BMI:
-
Body mass index
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the ROC curve
- Cr:
-
Creatine
- BUN:
-
Blood urea nitrogen
- HTN:
-
Hypertension
- IHD:
-
Ischemic heart disease
- Hb:
-
Hemoglobin
- DM:
-
Diabetes mellitus
References
Gullberg, B., Johnell, O. & Kanis, J. A. World-wide projections for hip fracture. Osteoporos. Int. 7(5), 407–13 (1997).
Adeyemi, A. & Delhougne, G. Incidence and economic burden of intertrochanteric fracture: A medicare claims database analysis. JBJS Open Access 4(1), e0045 (2019).
Nazrun, A. S., Tzar, M. N., Mokhtar, S. A. & Mohamed, I. N. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: Morbidity, subsequent fractures, and mortality. Ther. Clin. Risk Manag. 10, 937–48 (2014).
Mundi, S., Pindiprolu, B., Simunovic, N. & Bhandari, M. Similar mortality rates in hip fracture patients over the past 31 years. Acta Orthop. 85(1), 54–9 (2014).
Belmont, P. J. Jr. et al. Risk factors for complications and in-hospital mortality following hip fractures: A study using the National Trauma Data Bank. Arch. Orthop. Trauma Surg. 134(5), 597–604 (2014).
Biçen, Ç. et al. Analysis of risk factors affecting mortality in elderly patients operated on for hip fractures: A retrospective comparative study. Acta Orthop. Traumatol. Turc. 55(6), 493–9 (2021).
Jiang, L. et al. Charlson comorbidity index predicts 5-year survivorship of surgically treated hip fracture patients. Geriatr. Orthop. Surg. Rehabil. 9, 2151459318806442 (2018).
Pinto, I. P. et al. Does early surgical fixation of proximal femoral fractures in elderly patients affect mortality rates?. Rev. Bras. Ortop. (Sao Paulo) 54(4), 392–5 (2019).
Akinleye, S. D., Garofolo, G., Culbertson, M. D., Homel, P. & Erez, O. The role of BMI in hip fracture surgery. Geriatr. Orthop. Surg. Rehabil. 9, 2151458517747414 (2018).
Cha, Y. H., Lee, Y. K., Koo, K. H., Wi, C. & Lee, K. H. Difference in mortality rate by type of anticoagulant in elderly patients with cardiovascular disease after hip fractures. Clin. Orthop. Surg. 11(1), 15–20 (2019).
Harty, J. A., McKenna, P., Moloney, D., D’Souza, L. & Masterson, E. Anti-platelet agents and surgical delay in elderly patients with hip fractures. J. Orthop. Surg. (Hong Kong) 15(3), 270–2 (2007).
Maheshwari, R., Acharya, M., Monda, M. & Pandey, R. Factors influencing mortality in patients on antiplatelet agents presenting with proximal femoral fractures. J. Orthop. Surg. (Hong Kong) 19(3), 314–6 (2011).
Zhao, P. et al. Intertrochanteric hip fracture surgery in Chinese: Risk factors for predicting mortality. Int. J. Clin. Exp. Med. 8(2), 2789–93 (2015).
Ryan, G. et al. Anemia at presentation predicts acute mortality and need for readmission following geriatric hip fracture. JBJS Open Access https://doi.org/10.2106/JBJS.OA.20.00048 (2020).
Lu, J., Chen, Y. Y., Zhang, L., Li, Y. G. & Wang, C. Laboratory nutritional parameters predict one-year mortality in elderly patients with intertrochanteric fracture. Asia Pac. J. Clin. Nutr. 25(3), 457–63 (2016).
Borges, A., Torres, J., São Simão, R., Cabral, A. T. & Pinto, R. Impact of preoperative analytical values on post-operative mortality rate of intertrochanteric fractures. Acta Med. Port. 27(2), 218–22 (2014).
Demirel, E. & Şahin, A. Predictive value of blood parameters and comorbidities on three-month mortality in elderly patients with hip fracture. Cureus 13(10), e18634 (2021).
Youden, W. J. Index for rating diagnostic tests. Cancer 3(1), 32–5 (1950).
Roche, J. J., Wenn, R. T., Sahota, O. & Moran, C. G. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: Prospective observational cohort study. BMJ 331(7529), 1374 (2005).
Kain, V. & Halade, G. V. Role of neutrophils in ischemic heart failure. Pharmacol. Ther. 205, 107424 (2020).
Chia, S. et al. Association of leukocyte and neutrophil counts with infarct size, left ventricular function and outcomes after percutaneous coronary intervention for ST-elevation myocardial infarction. Am. J. Cardiol. 103(3), 333–7 (2009).
Hermann, D. M., Kleinschnitz, C. & Gunzer, M. Implications of polymorphonuclear neutrophils for ischemic stroke and intracerebral hemorrhage: Predictive value, pathophysiological consequences and utility as therapeutic target. J. Neuroimmunol. 321, 138–43 (2018).
Buck, B. H. et al. Early neutrophilia is associated with volume of ischemic tissue in acute stroke. Stroke 39(2), 355–60 (2008).
Zhang, Z. et al. Neutrophil counts and the risk of first stroke in general hypertensive adults. Hypertens. Res. 44(7), 830–9 (2021).
Jang, S. Y. et al. Blood transfusion for elderly patients with hip fracture: A Nationwide Cohort Study. J. Korean Med. Sci. 35(37), e313. https://doi.org/10.3346/jkms.2020.35.e313 (2020).
Sousa, R. et al. Autologous blood transfusion as an immunomodulator in experimental sepsis. Int. J. Surg. Investig. 1(5), 365–71 (2000).
Hill, G. E., Frawley, W. H., Griffith, K. E., Forestner, J. E. & Minei, J. P. Allogeneic blood transfusion increases the risk of postoperative bacterial infection: A meta-analysis. J. Trauma 54(5), 908–14 (2003).
Blumberg, N., Triulzi, D. J. & Heal, J. M. Transfusion-induced immunomodulation and its clinical consequences. Transfus. Med. Rev. 4(4 Suppl 1), 24–35 (1990).
Tran, P. & Banerjee, P. Iatrogenic decompensated heart failure. Curr. Heart Fail. Rep. 17(2), 21–7 (2020).
Lee, H. & Yuh, Y. A paradigm shift: Perioperative iron and erythropoietin therapy for patient blood management. Hanyang Med. Rev. 38, 16 (2018).
Voorn, V. et al. Erythropoietin to reduce allogeneic red blood cell transfusion in patients undergoing total hip or knee arthroplasty. Vox Sang. 111, 219–225 (2016).
Guzel, Y., Gurcan, O. T., Golge, U. H., Dulgeroglu, T. C. & Metineren, H. Topical tranexamic acid versus autotransfusion after total knee arthroplasty. J. Orthop. Surg. (Hong Kong) 24(2), 179–82 (2016).
Potter, L. J., Doleman, B. & Moppett, I. K. A systematic review of pre-operative anaemia and blood transfusion in patients with fractured hips. Anaesthesia 70(4), 483–500 (2015).
Nasab, S. A. M. & Khorramdin, E. The assessment of mortality and quality of life after intertrochanteric fracture of femur in patients older than 60 at Emam Khomeini Hospital of Ahvaz. Pak. J. Med. Sci. 33(4), 895–898 (2017).
Moradi, A., Moradi, M., Emadzadeh, M. & Bagheri, F. Comparison of the dynamic hip screw with the dynamic hip external fixator for intertrochanteric fractures: Report of a randomized controlled trial. Arch. Bone Jt. Surg. 9(6), 665–676 (2021).
Ma, J. et al. The percutaneous compression plate versus the dynamic hip screw for treatment of intertrochanteric hip fractures: A systematic review and meta-analysis of comparative studies. Orthop. Traumatol. Surg. Res. 98(7), 773–83 (2012).
Kiriakopoulos, E., McCormick, F., Nwachukwu, B. U., Erickson, B. J. & Caravella, J. In-hospital mortality risk of intertrochanteric hip fractures: A comprehensive review of the US Medicare database from 2005 to 2010. Musculoskelet. Surg. 101(3), 213–218 (2017).
McHugh, M. A. et al. Preoperative comorbidities associated with early mortality in hip fracture patients: A multicenter study. J. Am. Acad. Orthop. Surg. 31(2), 81–86 (2023).
Hooper, L., Bunn, D., Jimoh, F. O. & Fairweather-Tait, S. J. Water-loss dehydration and aging. Mech. Ageing Dev. 136–137, 50–8 (2014).
Kusen, J. Q. et al. Does preoperative hemodynamic preconditioning improve morbidity and mortality after traumatic hip fracture in geriatric patients? A retrospective cohort study. Arch. Orthop. Trauma Surg. 141(9), 1491–1497. https://doi.org/10.1007/s00402-020-03601-5 (2021).
Lindholm, C. et al. Hip fracture and pressure ulcers—The Pan-European Pressure Ulcer Study - intrinsic and extrinsic risk factors. Int. Wound J. 5(2), 315–28 (2008).
Ylinenvaara, S. I. et al. Preoperative urine-specific gravity and the incidence of complications after hip fracture surgery: A prospective, observational study. Eur. J. Anaesthesiol. 31(2), 85–90 (2014).
Morrison, R. J. M. et al. Dose optimisation of intravenous tranexamic acid for elective hip and knee arthroplasty: The effectiveness of a single pre-operative dose. Bone Joint Res. 6(8), 499–505 (2017).
Chan, G. et al. Inter- and intra-observer reliability of the new AO/OTA classification of proximal femur fractures. Injury 52(6), 1434–7 (2021).
Funding
The authors received no financial or material support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
M.B. and A.G. contributed to data gathering. M.B. and M.S. contributed to the data analysis. S.B. and S.H.S. contributed to writing the manuscript. All authors have been involved in the writing and revising of the manuscript, and each provide final approval of the version to be published. Written informed consent was obtained from patients for publication and all participants gave their consent for participation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Babagoli, M., Ghaseminejad Raeini, A., Sheykhvatan, M. et al. Influencing factors on morbidity and mortality in intertrochanteric fractures. Sci Rep 13, 12090 (2023). https://doi.org/10.1038/s41598-023-38667-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38667-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.