Abstract
Inappropriate activation of intrarenal renin–angiotensin system (RAS) may contribute to the pathogenesis of cardio-renal syndrome (CRS). We aimed to examine the cross-sectional associations of urinary angiotensinogen (AGT) excretion, a biomarker of intrarenal RAS activity, with central (aortic) and renal hemodynamic parameters in middle-aged and older adults, including patients with chronic kidney disease. Aortic and renal hemodynamic parameters were measured using applanation tonometry and duplex ultrasonography in 282 participants. Urinary AGT, liver-type fatty acid-binding protein (L-FABP), and plasma N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels were measured for each participant. Multiple linear regression analyses demonstrated that urinary AGT levels were associated with aortic blood pressures, pulsatile measures of renal blood flow, plasma NT-proBNP and urinary L-FABP levels after adjusting for potential covariates, including age, sex, body mass index, estimated glomerular filtration rate (GFR), and medication use. Additionally, when classified based on GFR stages and urinary AGT levels, plasma NT-proBNP and urinary L-FABP levels increased in participants with lower GFR and higher AGT groups. Our findings suggest that urinary AGT excretion is a shared determinant of central (aortic) and renal hemodynamics in middle-aged and older adults, providing clinical evidence for the potential role of intrarenal RAS activity in the development of CRS.
Similar content being viewed by others
Introduction
Accumulating clinical evidence indicates that patients with chronic kidney disease (CKD) are at a greater risk of cardiovascular complications1. Conversely, cardiovascular dysfunction (e.g., heart failure) is a well-known risk factor for developing renal dysfunction2. These spectrum disorders involving the heart and kidneys have been widely recognized as a cardio-renal syndrome (CRS), and the complex nature of their treatment and management pose major global public health challenges. With the growing epidemic of CRS, there is an urgent need for further research to explore common predictors in these organs.
The heart and kidneys are affected by humoral, neural, and hemodynamic factors, and abnormal alterations in these factors eventually lead to the development of CRS3,4. Previous studies have shown that elevated renal flow pulsatility—assessed using renal duplex ultrasonography or phase-contrast magnetic resonance imaging—strongly correlates with increased aortic pulse pressure and stiffness in various populations5,6,7. Moreover, increased retrograde flow from the descending thoracic aorta toward the aortic arch has been independently associated with reduced antegrade flow into the kidneys in patients with hypertension8. It has been demonstrated that these hemodynamic alternations, simultaneously observed in the aorta and kidney, could contribute to the pathogenesis of concomitant plasma B-type natriuretic peptide elevation with (micro)albuminuria9. Collectively, these close associations between central (aortic) and renal hemodynamics have been postulated as potential mechanisms that account for the bidirectional nature of CRS.
The renin–angiotensin system (RAS) is an essential hormonal system that regulates blood pressure and fluid/electrolyte homeostasis. In addition to the well-known systemic RAS, growing evidence has demonstrated that a completely functional RAS is present along the nephron, and inappropriate activation of the intrarenal RAS is recognized as the principal pathogenesis of hypertension and CKD10,11,12,13. Basic evidence also indicates that intrarenal RAS activity is a crucial mediator of CRS14. In this context, recent studies have reported that measuring the urinary levels of angiotensinogen (AGT), a substrate for renin, allows for the estimation of intrarenal RAS activity in patients with hypertension15,16 and CKD17,18,19. Moreover, a recent scientific statement from the American Heart Association (AHA) has proposed urinary AGT excretion as a diagnostic and prognostic biomarker of CRS2. However, to date, clinical evidence supporting the use of urinary AGT excretion as a biomarker for CRS has not been fully elucidated.
Based on this background, we hypothesized that augmented intrarenal RAS activity links to both central (aortic) and renal hemodynamic alterations. To test this hypothesis, we investigated the cross-sectional associations of urinary AGT levels with central (aortic) and renal hemodynamic parameters in middle-aged and older adults, including patients with CKD. Clarifying whether urinary AGT excretion is a shared determinant of central (aortic) and renal hemodynamics may lead to a better understanding of the potential role of intrarenal RAS activity in the development of CRS.
Results
Table 1 summarizes the clinical characteristics classified according to the estimated glomerular filtration rate (GFR). Based on the group comparison of GFR stages, participants in the lower GFR groups (60–89 or < 59 mL/min/1.73 m2) were older; had a lower proportion of females; had a higher percentage of antihypertensive (i.e., renin–angiotensin system inhibitor, calcium channel blocker, diuretic, β-blocker), lipid-lowering, and glucose-lowering medication users; had lower high-density lipoprotein (HDL) cholesterol and low-density lipoprotein (LDL) cholesterol levels; and had higher height, weight, body mass index (BMI), triglyceride, and hemoglobin A1c levels, mean arterial pressure, and brachial systolic blood pressure (SBP) and diastolic blood pressure (DBP).
The central (aortic) and renal characteristics according to GFR stages are shown in Table 2. Compared with the normal GFR group (≥ 90 mL/min/1.73 m2), the lower GFR groups (60 to 89 or < 59 mL/min/1.73 m2) exhibited higher levels of aortic SBP and DBP, carotid-femoral pulse wave velocity (PWV), plasma N-terminal pro-B-type natriuretic peptide (NT-proBNP), renal resistive index (RI) and pulsatility index (PI), serum fibroblast growth factor 23 (FGF23), urinary albumin creatinine ratio (ACR), β2-microglobulin, urinary liver-type fatty acid-binding protein (L-FABP), and urinary AGT excretion.
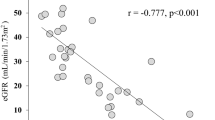
Figure 1 shows the simple correlations of urinary AGT levels with central (aortic) hemodynamic parameters. Positive correlations were observed between urinary AGT levels and aortic SBP (panel A), DBP (panel B), pulse pressure (panel C), augmented pressure (panel D), carotid-femoral PWV (panel E), and plasma NT-proBNP levels (panel F). Figure 2 shows the simple correlations of urinary AGT levels with renal hemodynamic parameters. The results revealed that urinary AGT levels were closely and positively correlated with urinary L-FABP levels (panel A), serum FGF23 levels (panel B), and renal RI (panel C) and PI (panel D) values.
Table S1 presents the simple correlation matrix for urinary AGT and β2-microglobulin levels in individuals with and without albuminuria. Regardless of the presence or absence of albuminuria, we found a positive correlation of urinary AGT and β2-microglobulin levels with plasma NT-proBNP and urinary L-FABP levels, and urinary ACR. Furthermore, in individuals with normoalbuminuria, we observed a positive correlation between urinary AGT levels and aortic SBP and DBP, carotid-femoral PWV, and renal RI and PI. However, we did not find a significant correlation between urinary β2-microglobulin levels and these parameters.
Table S2 presents the simple correlation matrix for urinary AGT and β2-microglobulin levels in individuals with higher and lower plasma NT-proBNP levels. Regardless of the plasma NT-proBNP levels, urinary AGT levels were positively correlated with aortic SBP and DBP, carotid-femoral PWV, urinary L-FABP levels, urinary ACR, renal RI and PI, and serum FGF23 levels.
The multiple adjusted associations of urinary AGT levels with central (aortic) and renal hemodynamic parameters are presented in Tables 3 and 4. Excluding carotid-femoral PWV, the associations between urinary AGT levels and central (aortic) hemodynamic parameters remained significant after adjusting for potential covariates, including age, sex, BMI, estimated GFR, and medication use (Table 3). Similarly, excluding serum FGF23 levels, urinary AGT levels were found to be independent determinants of renal hemodynamic parameters after considering various potentially relevant factors (Table 4).
Figure 3 shows the combined effects of urinary AGT levels and GFR stages on plasma NT-proBNP (panel A) and urinary L-FABP (panel B) levels. In the two-way analysis of covariance, significant main effects of urinary AGT groups were confirmed when participants were classified into six groups according to the three GFR stages and two urinary AGT levels. Moreover, there was a significant interaction effect of GFR stages and urinary AGT groups on urinary L-FABP levels. Increased plasma NT-proBNP and urinary L-FABP levels according to reduced renal function were only observed in the groups with higher urinary AGT levels. The mean plasma NT-proBNP (155 pg/mL) and urinary L-FABP (15.4 μg/g Cr) values were highest in the lower GFR and higher AGT groups.
Plasma N-terminal pro-B-type natriuretic peptide (top) and urinary liver-type fatty acid-binding protein (bottom) levels in subgroups classified according to urinary angiotensinogen and estimated glomerular filtration rate levels. P values were calculated by analysis of covariance after adjusting for age, sex, body mass index, renin–angiotensin system inhibitor, calcium channel blocker, diuretics, β-blocker use, lipid-lowering and glucose-lowering use. **P < 0.001, *P < 0.05 vs. estimated GFR ≥ 90 mL/min/1.73 m2 group; ##P < 0.001 vs. estimated GFR 60–80 mL/min/1.73 m2 group; ‡P < 0.001, †P < 0.001 vs. urinary AGT ≤ 12 μg/g Cr group. Multiple pairwise comparisons were corrected by the Bonferroni method.
Discussion
In this study, we examined the cross-sectional associations between urinary AGT levels and several hemodynamic parameters in middle-aged and older adults, including patients with CKD. The main findings of this study were as follows: first, urinary AGT levels positively correlated with aortic blood pressures, aortic PWV, and plasma NT-proBNP levels. Moreover, urinary AGT levels positively correlated with urinary L-FABP and serum FGF23 levels, and pulsatile measures of renal blood flow, as assessed by PI and RI. Second, excluding aortic PWV and serum FGF23 levels, these associations remained significant after adjusting for potential covariates, including age, sex, BMI, estimated GFR, and medication use. Third, when participants were classified based on estimated GFR and urinary AGT levels, plasma NT-proBNP and urinary L-FABP levels increased in the group with a lower GFR and higher urinary AGT levels. Collectively, these findings significantly extend our prior knowledge of intrarenal RAS activity in humans, suggesting that urinary AGT excretion is a shared determinant of central (aortic) and renal hemodynamics.
Evidence that urinary AGT excretion can provide specific information regarding intrarenal RAS activity20, as well as the development of a sensitive and specific quantification system for human AGT using sandwich ELISA21, have contributed to the elucidation of the pathophysiological role of intrarenal RAS activity in humans13. Since then, growing clinical evidence has indicated that urinary AGT levels are associated with several hemodynamic parameters, including clinical blood pressure22,23,24, ambulatory blood pressure25, heart rate26, left ventricular mass index, and intima-media thickness27. However, the relationship between urinary AGT excretion and central and local hemodynamics is not fully understood. Our observations confirm that urinary AGT levels are positively and independently associated with aortic blood pressures and pulsatile measures of renal blood flow. To the best of our knowledge, this is the first study to demonstrate that elevated urinary AGT excretion (i.e., intrarenal RAS activity) may play a key role in regulating hemodynamic alterations in the aorta and kidneys.
Previous studies have reported that urinary AGT levels correlate positively with urinary albumin excretion, and negatively with estimated GFR16,19. Similarly, the present study revealed that urinary AGT levels positively correlated with the log-transformed urinary ACR (r = 0.77) and increased in a stepwise fashion with decline of estimated GFR (Table 2). Although circulating AGT produced and secreted by the liver cannot normally be filtrated across the glomerular basement membrane13, basic research has indicated that glomerular injury leads to the excretion of liver-derived (i.e., circulating) AGT into urine and an increase in intrarenal angiotensin II generation28,29. These results suggest that glomerular injury may be a trigger of intrarenal RAS activation10. However, our stratified analysis based on the presence or absence of albuminuria showed that urinary AGT levels showed a positive correlation with central (aortic) and renal hemodynamic parameters even in individuals with normoalbuminuria (Table S1). Therefore, these findings indicate that elevated urinary AGT may serve as a predicting factor to the alterations in central (aortic) and renal hemodynamics in individuals without glomerular damage.
Urinary L-FABP levels strongly correlated with urinary AGT levels among various parameters (Fig. 2A; Table 4). In addition, the mean urinary L-FABP values increased in the group with lower GFR and higher urinary AGT levels (Fig. 3B). L-FABP is expressed in renal proximal tubular cells and excreted in the urine in response to tubulointerstitial damage30. Also, a previous study showed that urinary L-FABP levels strongly correlated with peritubular capillary blood flow directly assessed in living-related kidney transplantations using intravital video analysis31. Therefore, our findings suggest that augmented intrarenal RAS activity contributes to the pathogenesis of tubular abnormalities and deteriorates the intrarenal microcirculation. In this context, the results of our study are consistent with basic evidence demonstrating that the expression of renal human L-FABP and urinary human L-FABP levels are increased upon intrarenal RAS activation in human L-FABP chromosomal transgenic mice32,33,34.
It was previously reported that subclinically elevated circulating NT-proBNP levels were associated with an increased risk of developing cardiovascular disease35 and CKD36 in the general population. Thus, circulating NT-proBNP has been recognized as a representative biomarker of CRS in clinical practice2,3. The present study found that increased urinary AGT levels were independent determinants of plasma NT-proBNP levels (Table 3). Moreover, increased plasma NT-proBNP levels associated with reduced renal function were only observed in the group with higher urinary AGT levels (Fig. 3A). A previous study also demonstrated that time course changes in urinary AGT levels on admission and at discharge and readmission were significantly associated with changes in circulating NT-proBNP levels37. Therefore, these findings imply that urinary AGT excretion may serve as a useful biomarker for monitoring CRS2.
Among five known types of CRS, secondary CRS (type 5) reflects a systemic process that causes simultaneous cardiac and renal damage/dysfunction3,4. Several systemic disorders—such as diabetes, amyloidosis, vasculitis, sepsis, and central hemodynamic alterations—have been postulated as potential causes of secondary CRS3,4,9. In this study, we found that urinary AGT excretion was a common determinant of central (aortic) and renal hemodynamic alterations. In addition, the results of a previous study showed that increased urinary AGT levels were associated with the incidence of cardiovascular and renal complications in patients with type 2 diabetes and albuminuria38. Taken together, these findings suggest that increased intrarenal RAS activity may contribute to systemic conditions leading to secondary CRS.
The present study had several limitations; first, this was a cross-sectional investigation with a relatively small sample size. Thus, we could not address the temporal or causal relationships between urinary AGT levels and central (aortic) and renal hemodynamic parameters. In addition, this study is limited to investigating the association between urinary AGT levels and several CRS surrogate markers. Therefore, the long-term prognostic value of urinary AGT in relation to cardiovascular events and its association with changes in estimated GFR slope remains obscure. Future prospective studies are needed to confirm whether increased urinary AGT excretion can lead to changes in central (aortic) and renal hemodynamics. Additionally, these studies should aim to establish the significant relationship between urinary AGT and not only surrogate markers but also clinically relevant outcomes, such as cardiovascular events and changes in estimated GFR slope. Second, we determined the CKD status via a single assessment of the estimated GFR (< 60 mL/min/1.73 m2) and/or urinary ACR (≥ 30 mg/g); however, the diagnosis of CKD usually requires these conditions to have persisted for at least 3 months. Moreover, the etiology of CKD (e.g., glomerulonephritis, diabetic nephropathy, and nephrosclerosis) could not be surveyed in the present study. Third, the association between urinary and plasma AGT concentrations was not investigated in the participants of this study. Previous studies have shown that the level of AGT in renal tissue is significantly lower compared to plasma13. This finding suggests that there may be a discrepancy between urinary and plasma AGT concentrations, particularly in individuals without glomerular damage (i.e., individuals without AGT leakage from the blood). Further analyses using a dataset that includes both plasma and urinary AGT concentrations are necessary. Finally, the hemodynamics of the aorta and kidney was not measured simultaneously; still, they were measured in the resting state on the same day in the morning. Thus, the results of this study should be interpreted with caution and confirmed by other studies. Despite these limitations, this study had several strengths; first, it included a comprehensive dataset of biochemical and hemodynamic measurements that may have affected the relationship between urinary AGT levels and central (aortic) and renal hemodynamic parameters. Second, the analysis included patients both with and without CKD, allowing for the comparison of physiological and pathophysiological differences in urinary AGT within a single study.
In conclusion, this study demonstrates that urinary AGT levels are independently associated with several hemodynamic parameters in the aorta and kidneys. Furthermore, higher urinary AGT levels were found to be associated with increased plasma NT-proBNP and urinary L-FABP levels. Collectively, these findings indicate that urinary AGT excretion is a shared determinant of central (aortic) and renal hemodynamics and may lead to a better understanding of the potential role of intrarenal RAS activity in the development of CRS.
Methods
Participants
The data in the present study were collected during a voluntary, community-based physical examination conducted in 2018–2019 at the University of Tsukuba. All participants were recruited through local newspaper advertisements, study flyers, homepages, and the Department of Nephrology at the University of Tsukuba Hospital. Two hundred eighty-two participants (66% female) were included in the analysis after excluding participants with young age (< 45 years), missing hemodynamic data, or who did not comply with the study protocol. This study was approved by the Institutional Review Board of the University of Tsukuba and performed in accordance with the guidelines of the Declaration of Helsinki. Written informed consent was obtained from all the participants for study participation.
Biochemical measurements
Each participant abstained from large meals and vigorous exercise a day before the measurements. Antecubital venous blood samples were collected in the morning following overnight fasting to measure the concentrations of HDL and LDL cholesterols, triglyceride, glucose, hemoglobin A1c, NT-proBNP, creatinine, and cystatin C. These parameters were measured at Tsukuba i-Laboratory LLP using certified methods. The serum FGF23 concentrations were measured using a commercial enzyme-linked immunosorbent assay kit (Kainos Laboratories Inc., Tokyo, Japan). The estimated GFR was calculated using Japanese estimated GFR equations based on standardized serum creatinine or cystatin C levels39,40; the average estimated GFRcr and GFRcys values were subsequently used for the analysis.
Urinary concentrations of albumin, β2-microglobulin, L-FABP, AGT, and creatinine were measured using spot urine samples collected in the morning after blood sampling. Among these, the urinary concentrations of albumin and β2-microglobulin were measured using the immunonephelometry and latex agglutination immunoassay methods, respectively. Following the manufacturer’s instructions, urinary L-FABP concentrations were measured using a highly sensitive sandwich enzyme-linked immunosorbent assay (High Sensitivity Human L-FABP ELISA Kit; CMIC Holdings Co., Ltd., Tokyo, Japan)41, while urinary AGT concentrations were determined using a human total AGT assay kit (Immuno-Biological Laboratories, Gunma, Japan)21. All urinary measurements were reported as ratios relative to urinary creatinine concentrations.
Hemodynamic measurements
On the same day as the biochemical assessments, several hemodynamic parameters were measured in an environmentally controlled laboratory after adequate rest. Brachial blood pressure and heart rate were assessed using a semiautomated vascular testing device with an electrocardiogram and oscillometric cuffs (form PWV/ABI: Model BP203RPEII; Colin Medical Technology, Aichi, Japan), and applanation tonometry (TU-100; Colin Medical Technology, Aichi, Japan) was used to record the beat-to-beat carotid pressure waveform, which was converted to an aortic pressure waveform using a validated general transfer function (SphygmoCor version 8.0; AtCor Medical, Sydney, Australia) as described in a previous study42. Subsequently, the aortic pressure waveform was calibrated using the mean arterial pressure and brachial DBP to determine the aortic systolic and pulse pressures. The aortic incident pressure wave height and augmented pressure adjusted for heart rate of 75 bpm were determined as previously described43, and the carotid-femoral (i.e., aortic) PWV—the current gold standard measure of aortic stiffness—was measured using a standard procedure44.
The blood flow velocity profiles in the intrarenal segmental arteries of each kidney were recorded using duplex ultrasonography with a 3.5-MHz convex array probe (Noblus C25; Hitachi Aloka Medical Ltd., Tokyo, Japan). Peak systolic and end-diastolic flow velocities were measured with the focal zone set to the depth of the target artery, and the probe insonation angle to the target artery set to < 60°. The renal PI and RI were calculated from these values, as previously described5.
Statistical analysis
Data were expressed as median with interquartile range for continuous data, or frequencies and percentages for categorical data. Group differences according to estimated GFR levels were compared using Kruskal–Wallis nonparametric tests for continuous variables, and the Chi-squared test for categorical variables. For subsequent statistical analyses, variables with skewed distributions were log-transformed to reduce heteroscedasticity and standardized to a normal distribution. Pearson product–moment correlations and stepwise linear regression analyses were used to determine the association of urinary AGT levels with central (aortic) and renal hemodynamic parameters, with adjustment for potential covariates. In the stepwise models, central (aortic) and renal hemodynamic parameters were entered as the dependent variables, while age, sex, BMI, estimated GFR, and medication use—such as renin–angiotensin system inhibitors, calcium channel blockers, diuretics, β-blockers, lipid-lowering medications, and glucose-lowering medications—were entered as the independent variables. Moreover, two-way analysis of covariance was performed to assess the adjusted effects of combined exposure to urinary AGT (categorized according to the median value) and GFR stages on plasma NT-proBNP and urinary L-FABP levels. In the case of a significant F-test for the group effect, the Bonferroni method was corrected for post hoc pairwise comparisons. All statistical analyses were performed using SPSS Statistics software (version 28.0; IBM Inc., New York, USA), and a P value < 0.05 was considered statistically significant.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available owing to ethical and legal constraints; however, anonymized data are available from the corresponding author upon reasonable request.
References
Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E. & Hsu, C. Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 351, 1296–1305. https://doi.org/10.1056/NEJMoa041031 (2004).
Rangaswami, J. et al. Cardiorenal syndrome: Classification, pathophysiology, diagnosis, and treatment strategies: A scientific statement from the American Heart Association. Circulation 139, e840–e878. https://doi.org/10.1161/CIR.0000000000000664 (2019).
Ronco, C. et al. Cardio-renal syndromes: Report from the consensus conference of the acute dialysis quality initiative. Eur. Heart J. 31, 703–711. https://doi.org/10.1093/eurheartj/ehp507 (2010).
Ronco, C., Haapio, M., House, A. A., Anavekar, N. & Bellomo, R. Cardiorenal syndrome. J. Am. Coll. Cardiol. 52, 1527–1539. https://doi.org/10.1016/j.jacc.2008.07.051 (2008).
Kosaki, K. et al. Renal hemodynamics across the adult lifespan: Relevance of flow pulsatility to chronic kidney disease. Exp. Gerontol. 152, 111459. https://doi.org/10.1016/j.exger.2021.111459 (2021).
Woodard, T. et al. Mediation analysis of aortic stiffness and renal microvascular function. J. Am. Soc. Nephrol. 26, 1181–1187. https://doi.org/10.1681/ASN.2014050450 (2015).
Hashimoto, J. & Ito, S. Central pulse pressure and aortic stiffness determine renal hemodynamics: Pathophysiological implication for microalbuminuria in hypertension. Hypertension 58, 839–846. https://doi.org/10.1161/HYPERTENSIONAHA.111.177469 (2011).
Hashimoto, J. & Ito, S. Aortic blood flow reversal determines renal function: Potential explanation for renal dysfunction caused by aortic stiffening in hypertension. Hypertension 66, 61–67. https://doi.org/10.1161/HYPERTENSIONAHA.115.05236 (2015).
Hashimoto, J. & Ito, S. Central pulse pressure links microalbuminuria with plasma B-type natriuretic peptide elevation: Causal implication for cardiorenal syndrome in hypertension. J. Hypertens. 32, 1665–1671. https://doi.org/10.1097/HJH.0000000000000242 (2014) (discussion 1671).
Nishiyama, A. & Kobori, H. Independent regulation of renin–angiotensin–aldosterone system in the kidney. Clin. Exp. Nephrol. 22, 1231–1239. https://doi.org/10.1007/s10157-018-1567-1 (2018).
Navar, L. G., Kobori, H., Prieto, M. C. & Gonzalez-Villalobos, R. A. Intratubular renin–angiotensin system in hypertension. Hypertension 57, 355–362. https://doi.org/10.1161/HYPERTENSIONAHA.110.163519 (2011).
Siragy, H. M. & Carey, R. M. Role of the intrarenal renin–angiotensin–aldosterone system in chronic kidney disease. Am. J. Nephrol. 31, 541–550. https://doi.org/10.1159/000313363 (2010).
Kobori, H., Nangaku, M., Navar, L. G. & Nishiyama, A. The intrarenal renin–angiotensin system: From physiology to the pathobiology of hypertension and kidney disease. Pharmacol. Rev. 59, 251–287. https://doi.org/10.1124/pr.59.3.3 (2007).
Rafiq, K. et al. Renal sympathetic denervation suppresses de novo podocyte injury and albuminuria in rats with aortic regurgitation. Circulation 125, 1402–1413. https://doi.org/10.1161/CIRCULATIONAHA.111.064097 (2012).
Kobori, H., Urushihara, M., Xu, J. H., Berenson, G. S. & Navar, L. G. Urinary angiotensinogen is correlated with blood pressure in men (Bogalusa Heart Study). J. Hypertens. 28, 1422–1428. https://doi.org/10.1097/HJH.0b013e3283392673 (2010).
Kobori, H. et al. Urinary angiotensinogen as a novel biomarker of the intrarenal renin–angiotensin system status in hypertensive patients. Hypertension 53, 344–350. https://doi.org/10.1161/HYPERTENSIONAHA.108.123802 (2009).
Mills, K. T. et al. Increased urinary excretion of angiotensinogen is associated with risk of chronic kidney disease. Nephrol. Dial. Transplant. 27, 3176–3181. https://doi.org/10.1093/ndt/gfs011 (2012).
Burns, K. D. & Hiremath, S. Urinary angiotensinogen as a biomarker of chronic kidney disease: Ready for prime time?. Nephrol. Dial. Transplant. 27, 3010–3013. https://doi.org/10.1093/ndt/gfs166 (2012).
Kobori, H. et al. Urinary angiotensinogen as a potential biomarker of severity of chronic kidney diseases. J. Am. Soc. Hypertens. 2, 349–354. https://doi.org/10.1016/j.jash.2008.04.008 (2008).
Kobori, H., Harrison-Bernard, L. M. & Navar, L. G. Urinary excretion of angiotensinogen reflects intrarenal angiotensinogen production. Kidney Int. 61, 579–585. https://doi.org/10.1046/j.1523-1755.2002.00155.x (2002).
Katsurada, A. et al. Novel sandwich ELISA for human angiotensinogen. Am. J. Physiol. Renal Physiol. 293, F956-960. https://doi.org/10.1152/ajprenal.00090.2007 (2007).
Kim, H. Y. et al. Effect of urinary angiotensinogen and high-salt diet on blood pressure in patients with chronic kidney disease: Results from the Korean Cohort Study for Outcome in Patients with Chronic Kidney Disease (KNOW-CKD). Korean J. Intern. Med. 36, 659–667. https://doi.org/10.3904/kjim.2020.077 (2021).
Sato, E. et al. Urinary angiotensinogen excretion level is associated with elevated blood pressure in the normotensive general population. Am. J. Hypertens. 31, 742–749. https://doi.org/10.1093/ajh/hpy020 (2018).
Sato, E. et al. Urinary angiotensinogen excretion is associated with blood pressure in obese young adults. Clin. Exp. Hypertens. 38, 203–208. https://doi.org/10.3109/10641963.2015.1081219 (2016).
Zou, J., Li, Y., Li, F. H., Wei, F. F. & Wang, J. G. Urinary angiotensinogen excretion and ambulatory blood pressure. J. Hypertens. 30, 2000–2006. https://doi.org/10.1097/HJH.0b013e3283576928 (2012).
Ohashi, N. et al. Increased heart rate is associated with intrarenal renin–angiotensin system activation in chronic kidney disease patients. Clin. Exp. Nephrol. 23, 1109–1118. https://doi.org/10.1007/s10157-019-01746-1 (2019).
Tiryaki, O. & Usalan, C. Association between urinary angiotensinogen excretion rates and left ventricular mass index and carotid intima-media thickness in hypertensive kidney transplant recipients. Clin. Transplant. 29, 351–358. https://doi.org/10.1111/ctr.12521 (2015).
Matsusaka, T. et al. Podocyte injury enhances filtration of liver-derived angiotensinogen and renal angiotensin II generation. Kidney Int. 85, 1068–1077. https://doi.org/10.1038/ki.2013.453 (2014).
Matsusaka, T. et al. Liver angiotensinogen is the primary source of renal angiotensin II. J. Am. Soc. Nephrol. 23, 1181–1189. https://doi.org/10.1681/ASN.2011121159 (2012).
Noiri, E. et al. Urinary fatty acid-binding protein 1: An early predictive biomarker of kidney injury. Am. J. Physiol. Renal Physiol. 296, F669-679. https://doi.org/10.1152/ajprenal.90513.2008 (2009).
Yamamoto, T. et al. Renal L-type fatty acid-binding protein in acute ischemic injury. J. Am. Soc. Nephrol. 18, 2894–2902. https://doi.org/10.1681/ASN.2007010097 (2007).
Kosaki, K. et al. Renoprotective effects of voluntary running exercise training on aldosterone-induced renal injury in human L-FABP chromosomal transgenic mice. Hypertens. Res. 42, 1518–1527. https://doi.org/10.1038/s41440-019-0273-z (2019).
Ichikawa, D. et al. Renoprotective effect of renal liver-type fatty acid binding protein and angiotensin II type 1a receptor loss in renal injury caused by RAS activation. Am. J. Physiol. Renal Physiol. 306, F655-663. https://doi.org/10.1152/ajprenal.00460.2013 (2014).
Ichikawa, D. et al. Renal liver-type fatty acid binding protein attenuates angiotensin II-induced renal injury. Hypertension 60, 973–980. https://doi.org/10.1161/HYPERTENSIONAHA.112.199828 (2012).
Doi, Y. et al. N-terminal pro-brain natriuretic peptide and risk of cardiovascular events in a Japanese community: The Hisayama study. Arterioscler. Thromb. Vasc. Biol. 31, 2997–3003. https://doi.org/10.1161/ATVBAHA.111.223669 (2011).
Sasaki, T. et al. N-terminal Pro-B-type natriuretic peptide and incident CKD. Kidney Int. Rep. 6, 976–985. https://doi.org/10.1016/j.ekir.2021.01.006 (2021).
Yokoyama, S. et al. Time course changes in urinary angiotensinogen and circulating N-terminal pro-B-type natriuretic peptide in patients hospitalized with acute heart failure. Intern. Med. 59, 2839–2847. https://doi.org/10.2169/internalmedicine.5212-20 (2020).
Sawaguchi, M. et al. Association between urinary angiotensinogen levels and renal and cardiovascular prognoses in patients with type 2 diabetes mellitus. J. Diabetes Investig. 3, 318–324. https://doi.org/10.1111/j.2040-1124.2011.00172.x (2012).
Horio, M. et al. GFR estimation using standardized serum cystatin C in Japan. Am. J. Kidney Dis. 61, 197–203. https://doi.org/10.1053/j.ajkd.2012.07.007 (2013).
Matsuo, S. et al. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 53, 982–992. https://doi.org/10.1053/j.ajkd.2008.12.034 (2009).
Kosaki, K. et al. Relationship between exercise capacity and urinary liver-type fatty acid-binding protein in middle-aged and older individuals. Clin. Exp. Nephrol. 21, 810–817. https://doi.org/10.1007/s10157-017-1385-x (2017).
Kosaki, K. et al. Urinary liver-type fatty acid-binding protein is associated with subendocardial viability ratio in middle- and older-aged adults. Clin. Exp. Hypertens. 40, 244–250. https://doi.org/10.1080/10641963.2017.1356845 (2018).
Hashimoto, J. & Ito, S. Pulse pressure amplification, arterial stiffness, and peripheral wave reflection determine pulsatile flow waveform of the femoral artery. Hypertension 56, 926–933. https://doi.org/10.1161/HYPERTENSIONAHA.110.159368 (2010).
Kosaki, K. et al. No influence of lower leg heating on central arterial pulse pressure in young men. J. Physiol. Sci. 65, 311–316. https://doi.org/10.1007/s12576-015-0368-5 (2015).
Acknowledgements
The authors are grateful to the members of our laboratory (University of Tsukuba) and Ms. Michiru Hotta for technical assistance.
Funding
This work was partly supported by Grants-in-Aid for Scientific Research KAKENHI from the Ministry of Education, Culture, Sports, Science, and Technology, Japan (Grant numbers: 22H03471) and MEXT Leading Initiative for Excellent Young Researchers (Grant number: JPMXS0320200234).
Author information
Authors and Affiliations
Contributions
K.K. conceived the idea, analyzed the data, and drafted the manuscript. K.K., J.P., and M.M. collected clinical samples. J.P. performed the urinary AGT assays. T.S., M.K., C.S., K.Y., and S.M. contributed to the writing and assisted with the interpretation. All authors have reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kosaki, K., Park, J., Matsui, M. et al. Elevated urinary angiotensinogen excretion links central and renal hemodynamic alterations. Sci Rep 13, 11518 (2023). https://doi.org/10.1038/s41598-023-38507-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38507-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.